Abstract
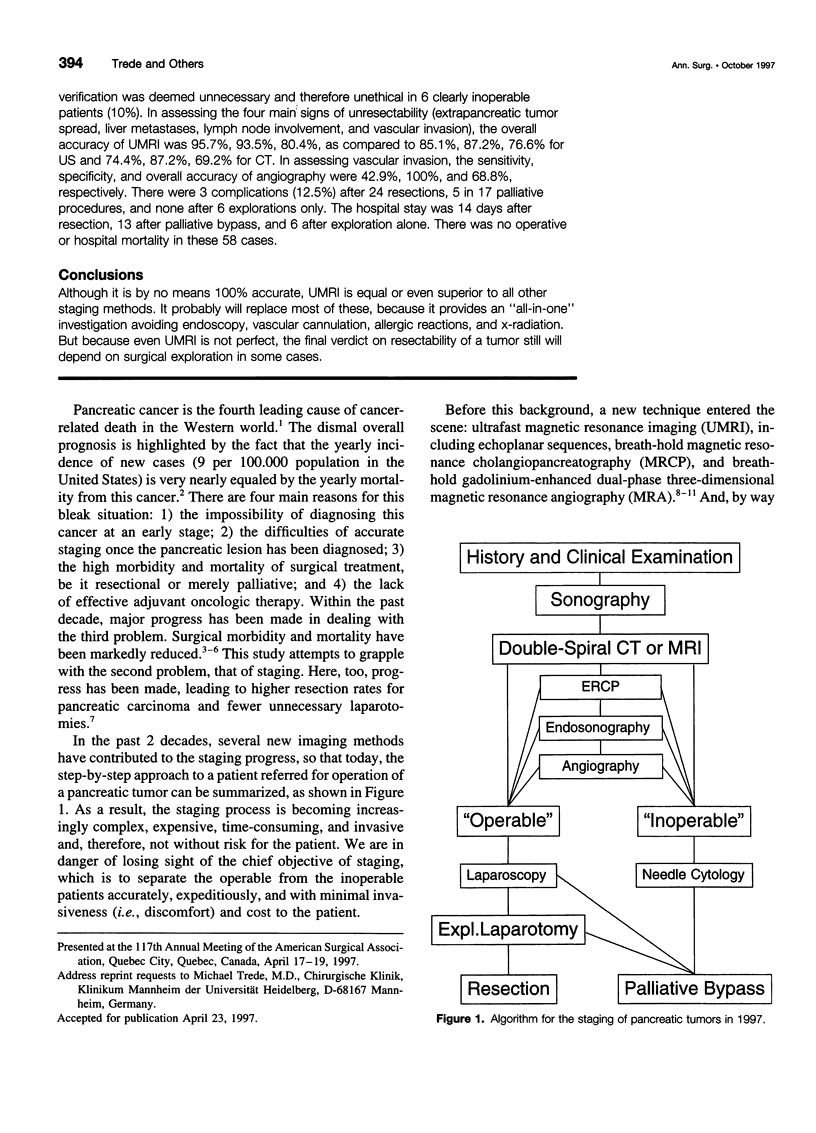
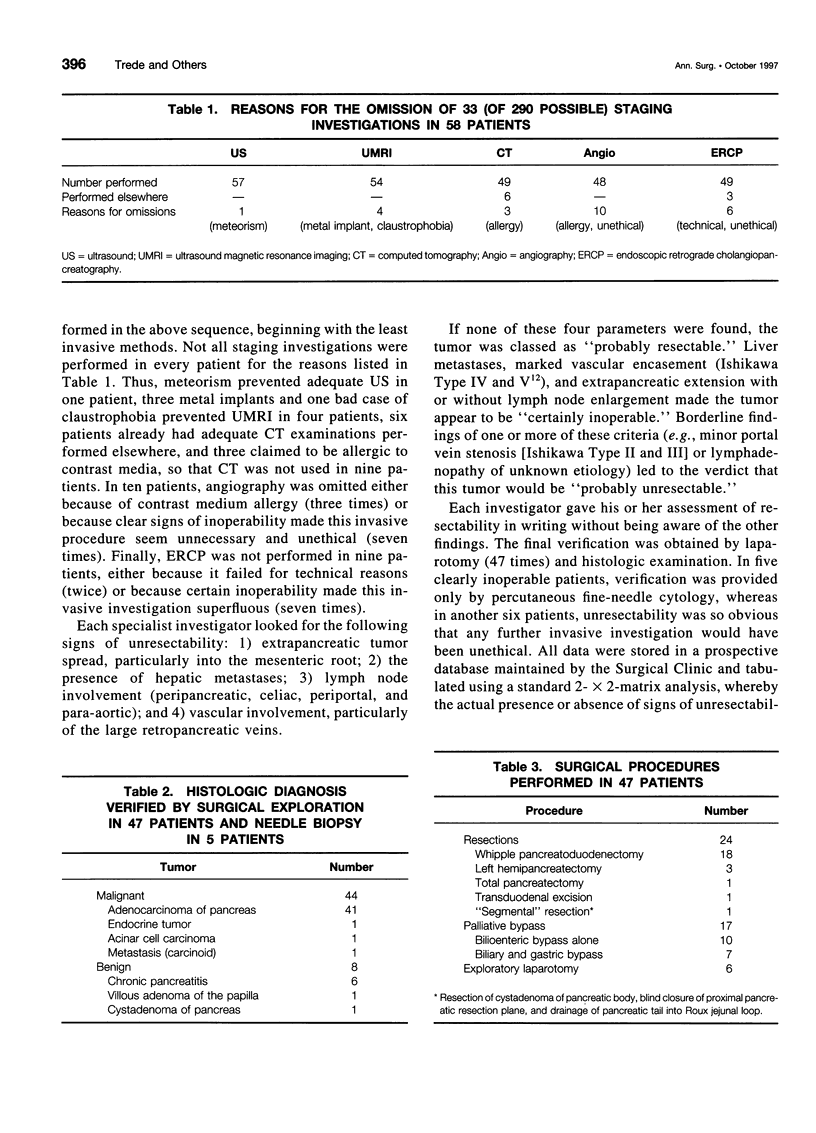
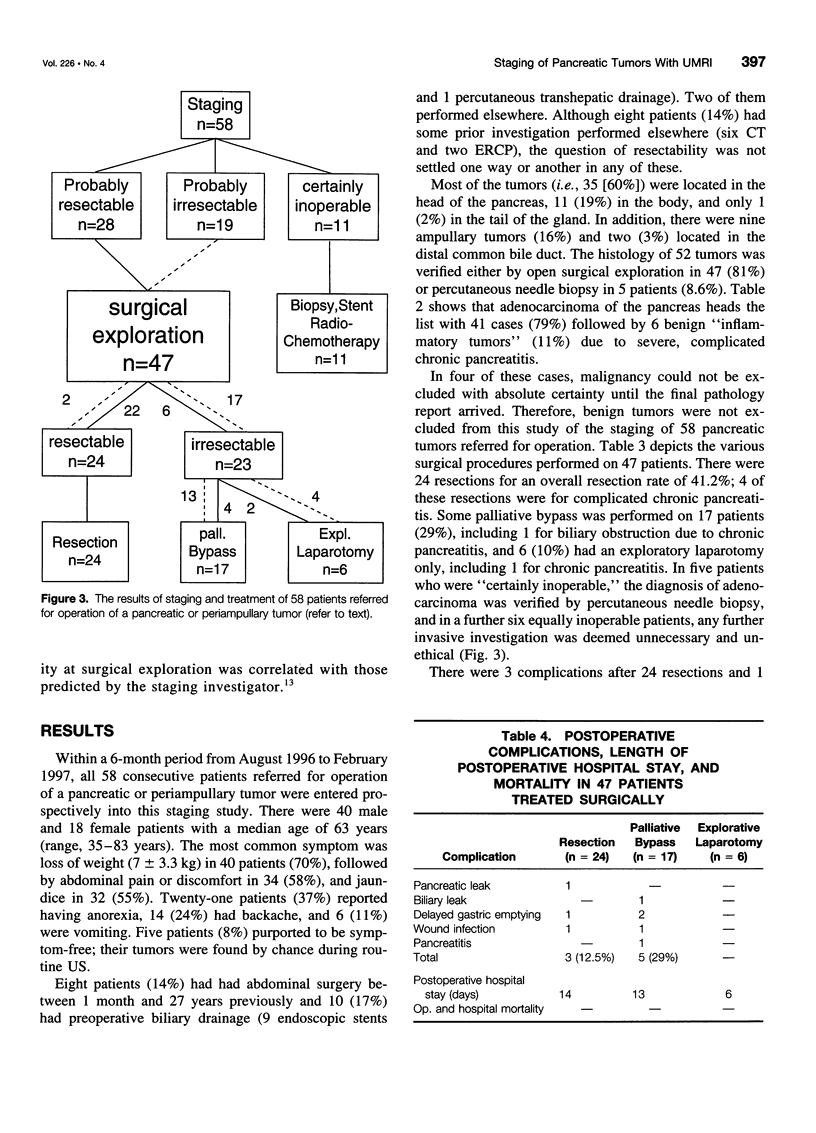
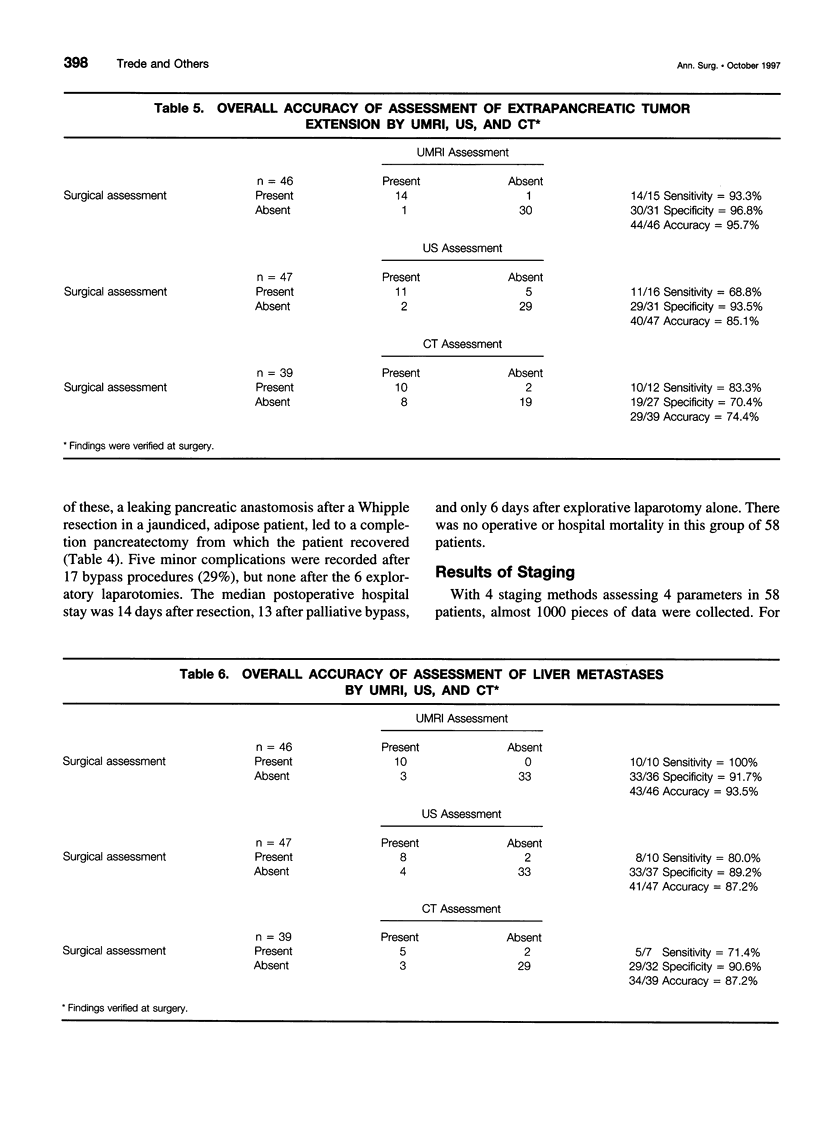
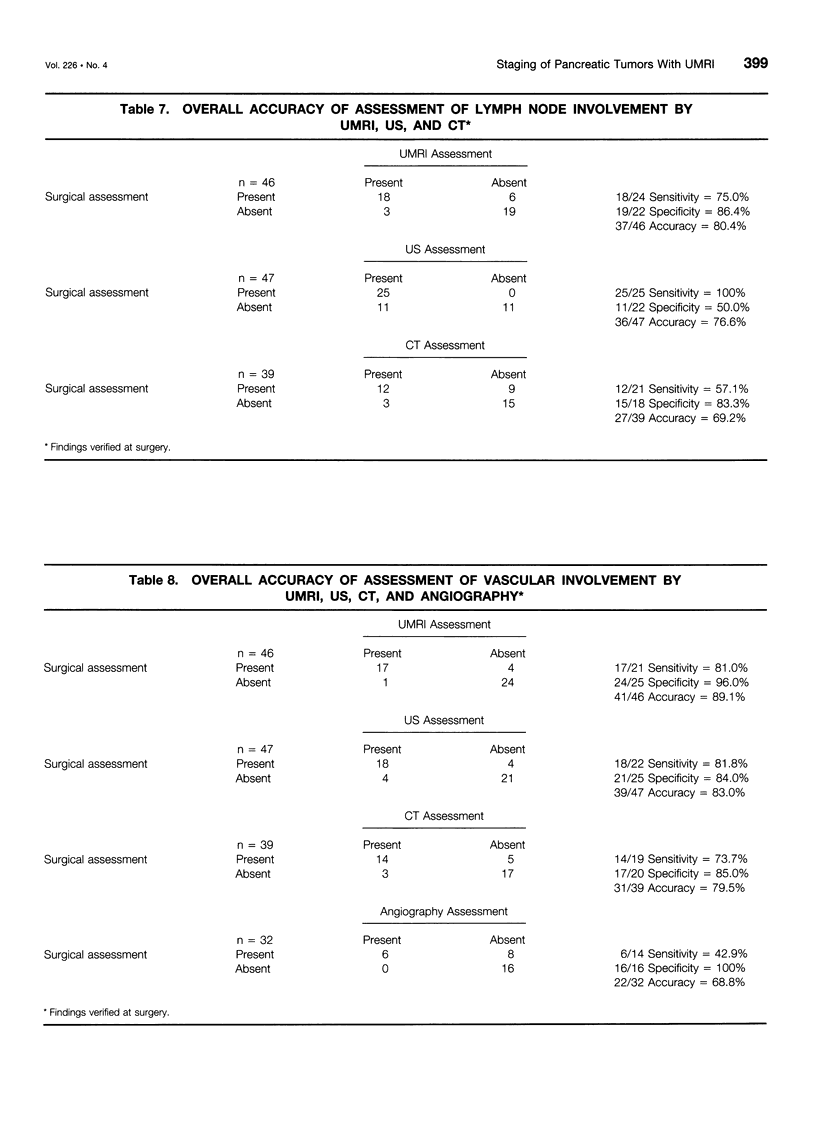
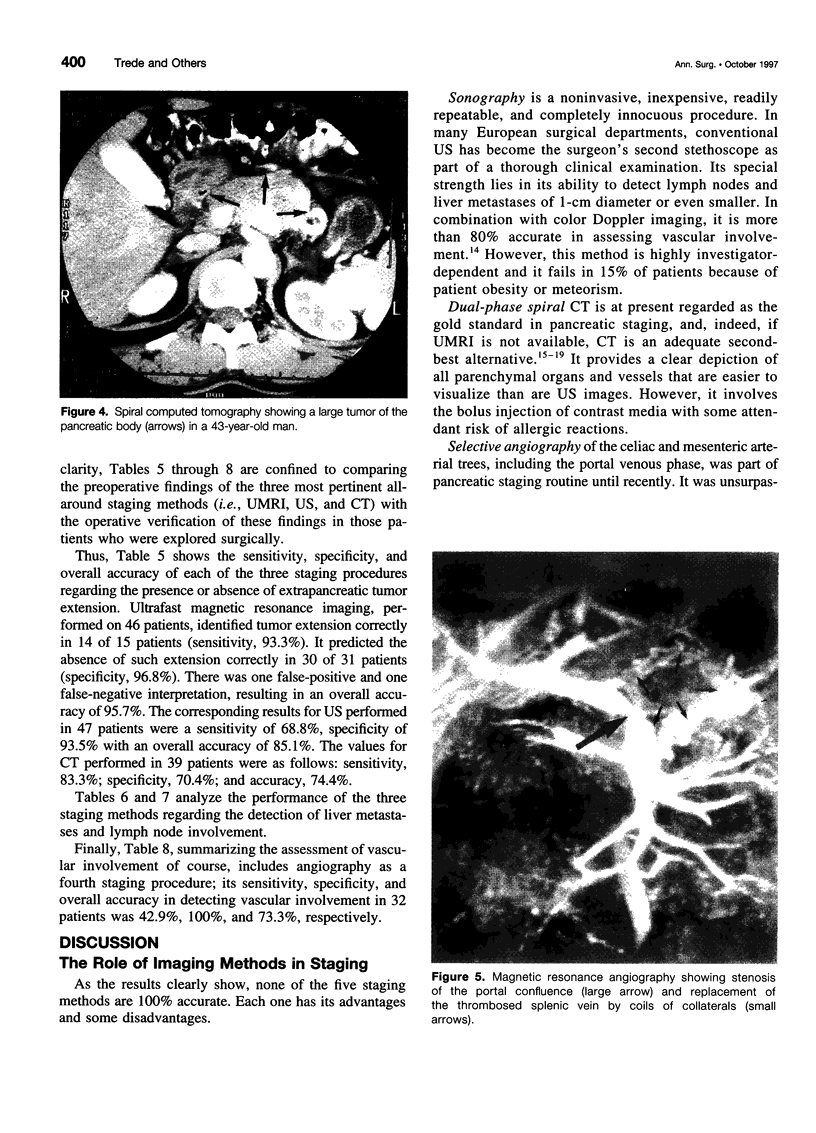
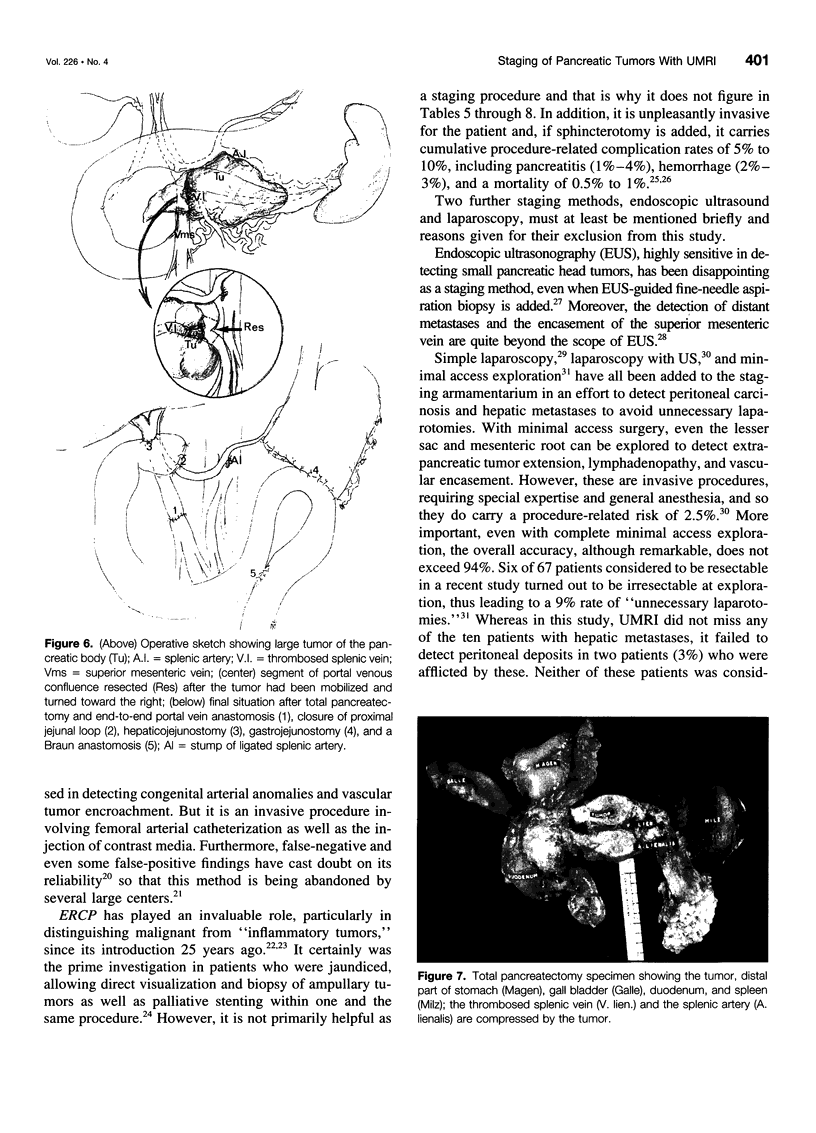
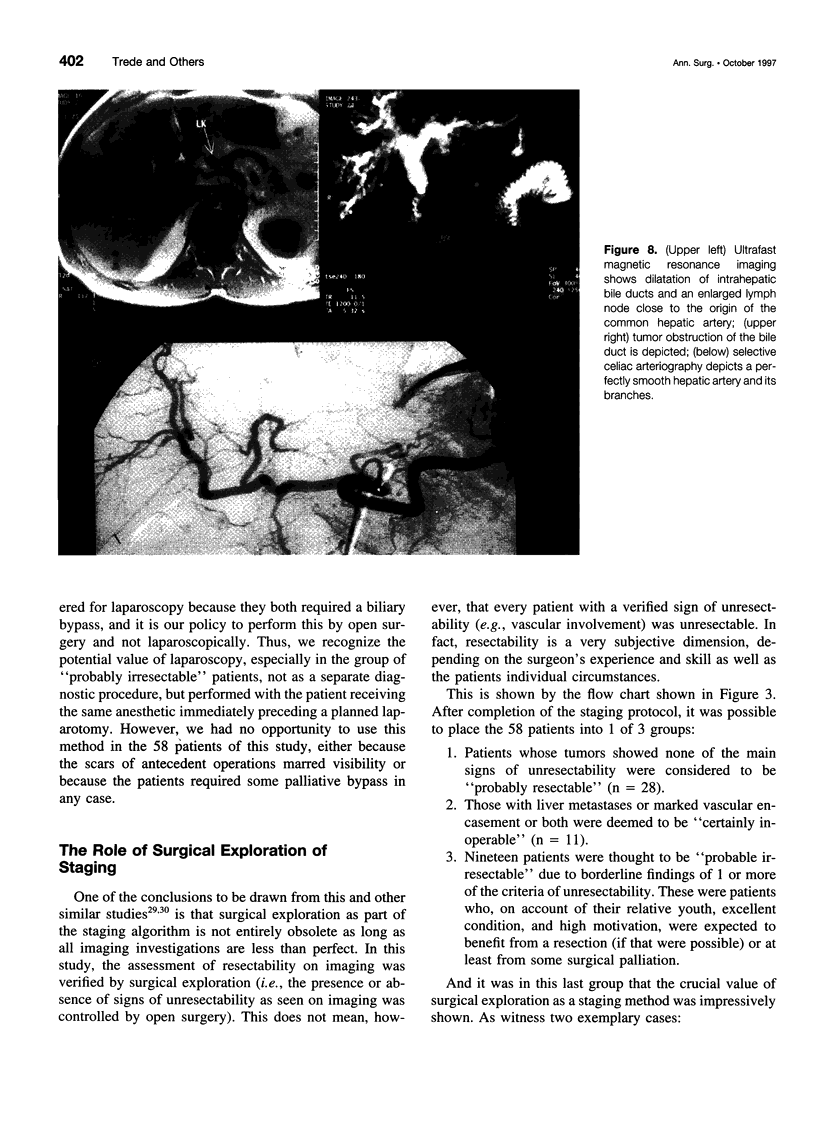
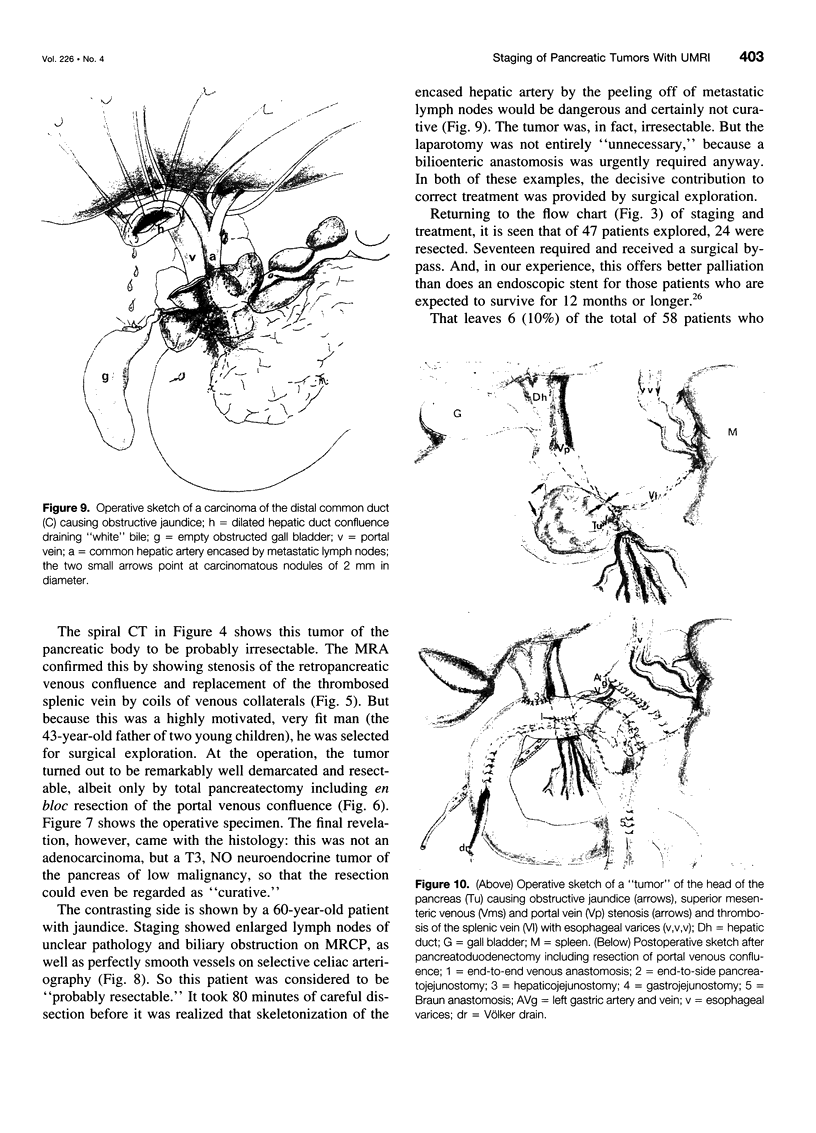
OBJECTIVE: This prospective study was undertaken to evaluate the accuracy of a noninvasive "all-in-one" staging method in predicting surgical resectability in patients with pancreatic or periampullary tumors. SUMMARY BACKGROUND DATA: Despite progress in imaging techniques, accurate staging and correct prediction of resectability remains one of the chief problems in the management of pancreatic tumors. Staging algorithms designed to separate operable from inoperable patients to save the latter an unnecessary laparotomy are becoming increasingly complex, expensive, time-consuming, invasive, and not without risks for the patient. METHODS: Between August 1996 and February 1997, 58 consecutive patients referred for operation of a pancreatic or periampullary tumor were examined clinically and by 5 staging methods: 1) percutaneous ultrasonography (US); 2) ultrafast magnetic resonance imaging (UMRI); 3) dual-phase helical computed tomography (CT); 4) selective visceral angiography; and 5) endoscopic cholangiopancreatography (ERCP). The assessment of resectability by each procedure was verified by surgical exploration and histologic examination. RESULTS: The study comprised 40 male and 18 female patients with a median age of 63 years. Thirty-five lesions were located in the pancreatic head (60%), 11 in the body (19%), and 1 in the tail of the gland (2%); there were 9 tumors of the ampulla (16%) and 2 of the distal common duct (3%). All five staging methods were completed in 36 patients. For reasons ranging from metallic implants to contrast medium allergy or because investigations already had been performed elsewhere, US was completed in 57 (98%), UMRI in 54 (93%), CT in 49 (84%), angiography in 48 (83%), and ERCP in 49 (84%) of these 58 patients. Signs of unresectability found were vascular involvement in 22 (38%), extrapancreatic tumor spread in 16 (26%), liver metastases in 10 (17%), lymph node involvement in 6 (10%), and peritoneal nodules in only 2 patients (3%). These findings were collated with those of surgical exploration in 47 patients (81 %) and percutaneous biopsy in 5 (9%); such invasive verification was deemed unnecessary and therefore unethical in 6 clearly inoperable patients (10%). In assessing the four main signs of unresectability (extrapancreatic tumor spread, liver metastases, lymph node involvement, and vascular invasion), the overall accuracy of UMRI was 95.7%, 93.5%, 80.4%, as compared to 85.1%, 87.2%, 76.6% for US and 74.4%, 87.2%, 69.2% for CT. In assessing vascular invasion, the sensitivity, specificity, and overall accuracy of angiography were 42.9%, 100%, and 68.8%, respectively. There were 3 complications (12.5%) after 24 resections, 5 in 17 palliative procedures, and none after 6 explorations only. The hospital stay was 14 days after resection, 13 after palliative bypass, and 6 after exploration alone. There was no operative or hospital mortality in these 58 cases. CONCLUSIONS: Although it is by no means 100% accurate, UMRI is equal or even superior to all other staging methods. It probably will replace most of these, because it provides an "all-in-one" investigation avoiding endoscopy, vascular cannulation, allergic reactions, and x-radiation. But because even UMRI is not perfect, the final verdict on resectability of a tumor still will depend on surgical exploration in some cases.
Full text
PDF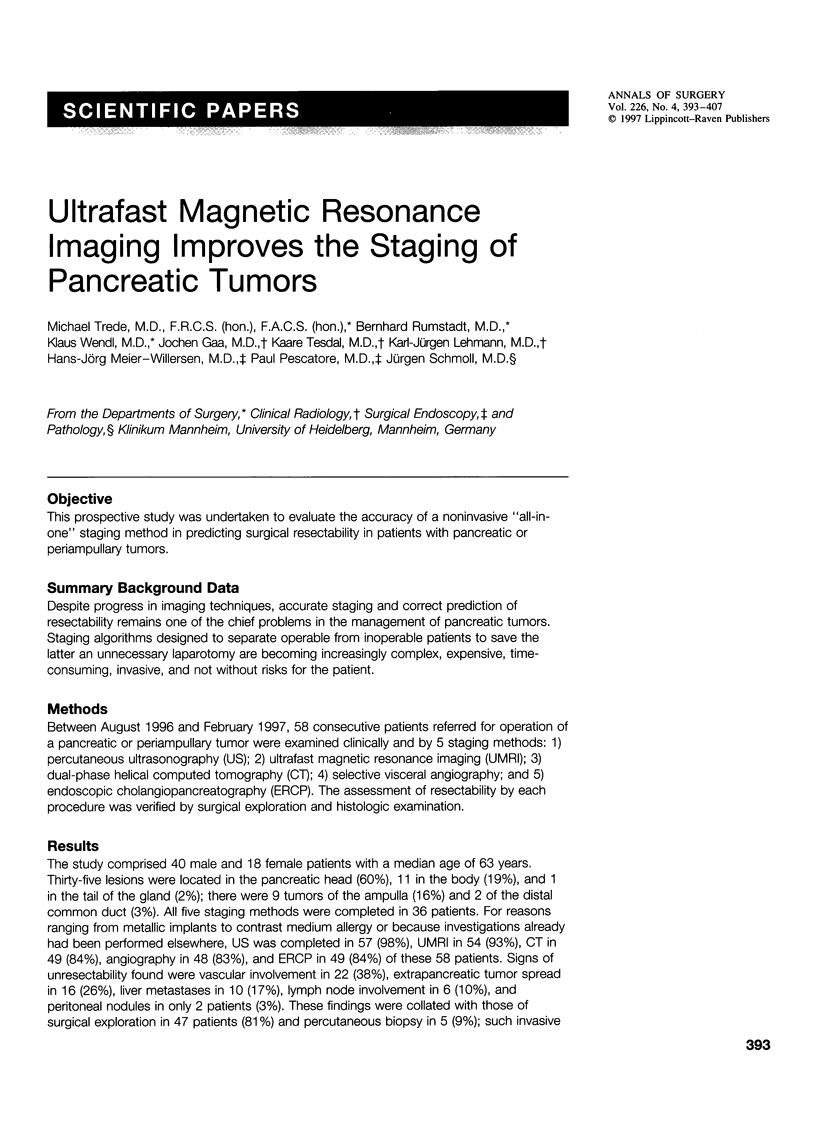

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aliperti G. Complications related to diagnostic and therapeutic endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 1996 Apr;6(2):379–407. [PubMed] [Google Scholar]
- Bluemke D. A., Cameron J. L., Hruban R. H., Pitt H. A., Siegelman S. S., Soyer P., Fishman E. K. Potentially resectable pancreatic adenocarcinoma: spiral CT assessment with surgical and pathologic correlation. Radiology. 1995 Nov;197(2):381–385. doi: 10.1148/radiology.197.2.7480681. [DOI] [PubMed] [Google Scholar]
- Cameron J. L., Pitt H. A., Yeo C. J., Lillemoe K. D., Kaufman H. S., Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993 May;217(5):430–438. doi: 10.1097/00000658-199305010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlon K. C., Dougherty E., Klimstra D. S., Coit D. G., Turnbull A. D., Brennan M. F. The value of minimal access surgery in the staging of patients with potentially resectable peripancreatic malignancy. Ann Surg. 1996 Feb;223(2):134–140. doi: 10.1097/00000658-199602000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-del Castillo C., Rattner D. W., Warshaw A. L. Standards for pancreatic resection in the 1990s. Arch Surg. 1995 Mar;130(3):295–300. doi: 10.1001/archsurg.1995.01430030065013. [DOI] [PubMed] [Google Scholar]
- Freeman M. L., Nelson D. B., Sherman S., Haber G. B., Herman M. E., Dorsher P. J., Moore J. P., Fennerty M. B., Ryan M. E., Shaw M. J. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996 Sep 26;335(13):909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- Gaa J., Fischer H., Laub G., Georgi M. Breath-hold MR imaging of focal liver lesions: comparison of fast and ultrasound techniques. Eur Radiol. 1996;6(6):838–843. doi: 10.1007/BF00240685. [DOI] [PubMed] [Google Scholar]
- Ishikawa O., Ohigashi H., Imaoka S., Furukawa H., Sasaki Y., Fujita M., Kuroda C., Iwanaga T. Preoperative indications for extended pancreatectomy for locally advanced pancreas cancer involving the portal vein. Ann Surg. 1992 Mar;215(3):231–236. doi: 10.1097/00000658-199203000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janes R. H., Jr, Niederhuber J. E., Chmiel J. S., Winchester D. P., Ocwieja K. C., Karnell J. H., Clive R. E., Menck H. R. National patterns of care for pancreatic cancer. Results of a survey by the Commission on Cancer. Ann Surg. 1996 Mar;223(3):261–272. doi: 10.1097/00000658-199603000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John T. G., Greig J. D., Carter D. C., Garden O. J. Carcinoma of the pancreatic head and periampullary region. Tumor staging with laparoscopy and laparoscopic ultrasonography. Ann Surg. 1995 Feb;221(2):156–164. doi: 10.1097/00000658-199502000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lentschig M. G., Reimer P., Rummeny E., Grenzheuser C., Daldrup H. E., Berns T., Dinse P., Sulkowski U., Peters P. E. Die Wertigkeit der 3-Phasen-Spiral-CT und der Magnetresonanztomographie in der präoperativen Diagnostik des Pankreaskarzinoms. Radiologe. 1996 May;36(5):406–412. doi: 10.1007/s001170050089. [DOI] [PubMed] [Google Scholar]
- Manegold B. C. Möglichkeiten und Grenzen der diagnostischen und therapeutischen ERCP beim Verschlussikterus. Chirurg. 1981 Jul;52(7):423–432. [PubMed] [Google Scholar]
- Murugiah M., Windsor J. A., Redhead D. N., O'Neill J. S., Suc B., Garden O. J., Carter D. C. The role of selective visceral angiography in the management of pancreatic and periampullary cancer. World J Surg. 1993 Nov-Dec;17(6):796–800. doi: 10.1007/BF01659101. [DOI] [PubMed] [Google Scholar]
- Müller M. F., Meyenberger C., Bertschinger P., Schaer R., Marincek B. Pancreatic tumors: evaluation with endoscopic US, CT, and MR imaging. Radiology. 1994 Mar;190(3):745–751. doi: 10.1148/radiology.190.3.8115622. [DOI] [PubMed] [Google Scholar]
- Prince M. R. Gadolinium-enhanced MR aortography. Radiology. 1994 Apr;191(1):155–164. doi: 10.1148/radiology.191.1.8134563. [DOI] [PubMed] [Google Scholar]
- Reinhold C., Bret P. M. Current status of MR cholangiopancreatography. AJR Am J Roentgenol. 1996 Jun;166(6):1285–1295. doi: 10.2214/ajr.166.6.8633434. [DOI] [PubMed] [Google Scholar]
- Richter G. M., Simon C., Hoffmann V., DeBernardinis M., Seelos R., Senninger N., Kauffmann G. W. Hydrospiral-CT des Pankreas in Dünnschichttechnik. Radiologe. 1996 May;36(5):397–405. doi: 10.1007/s001170050088. [DOI] [PubMed] [Google Scholar]
- Sironi S., De Cobelli F., Zerbi A., Balzano G., Di Carlo V., DelMaschio A. Pancreatic carcinoma: MR assessment of tumor invasion of the peripancreatic vessels. J Comput Assist Tomogr. 1995 Sep-Oct;19(5):739–744. [PubMed] [Google Scholar]
- Tomiyama T., Ueno N., Tano S., Wada S., Kimura K. Assessment of arterial invasion in pancreatic cancer using color Doppler ultrasonography. Am J Gastroenterol. 1996 Jul;91(7):1410–1416. [PubMed] [Google Scholar]
- Trede M., Schwall G., Saeger H. D. Survival after pancreatoduodenectomy. 118 consecutive resections without an operative mortality. Ann Surg. 1990 Apr;211(4):447–458. doi: 10.1097/00000658-199004000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hoe L., Gryspeerdt S., Marchal G., Baert A. L., Mertens L. Helical CT for the preoperative localization of islet cell tumors of the pancreas: value of arterial and parenchymal phase images. AJR Am J Roentgenol. 1995 Dec;165(6):1437–1439. doi: 10.2214/ajr.165.6.7484581. [DOI] [PubMed] [Google Scholar]
- Warshaw A. L., Fernández-del Castillo C. Pancreatic carcinoma. N Engl J Med. 1992 Feb 13;326(7):455–465. doi: 10.1056/NEJM199202133260706. [DOI] [PubMed] [Google Scholar]
- Warshaw A. L., Gu Z. Y., Wittenberg J., Waltman A. C. Preoperative staging and assessment of resectability of pancreatic cancer. Arch Surg. 1990 Feb;125(2):230–233. doi: 10.1001/archsurg.1990.01410140108018. [DOI] [PubMed] [Google Scholar]
- de Rooij P. D., Rogatko A., Brennan M. F. Evaluation of palliative surgical procedures in unresectable pancreatic cancer. Br J Surg. 1991 Sep;78(9):1053–1058. doi: 10.1002/bjs.1800780909. [DOI] [PubMed] [Google Scholar]