Abstract
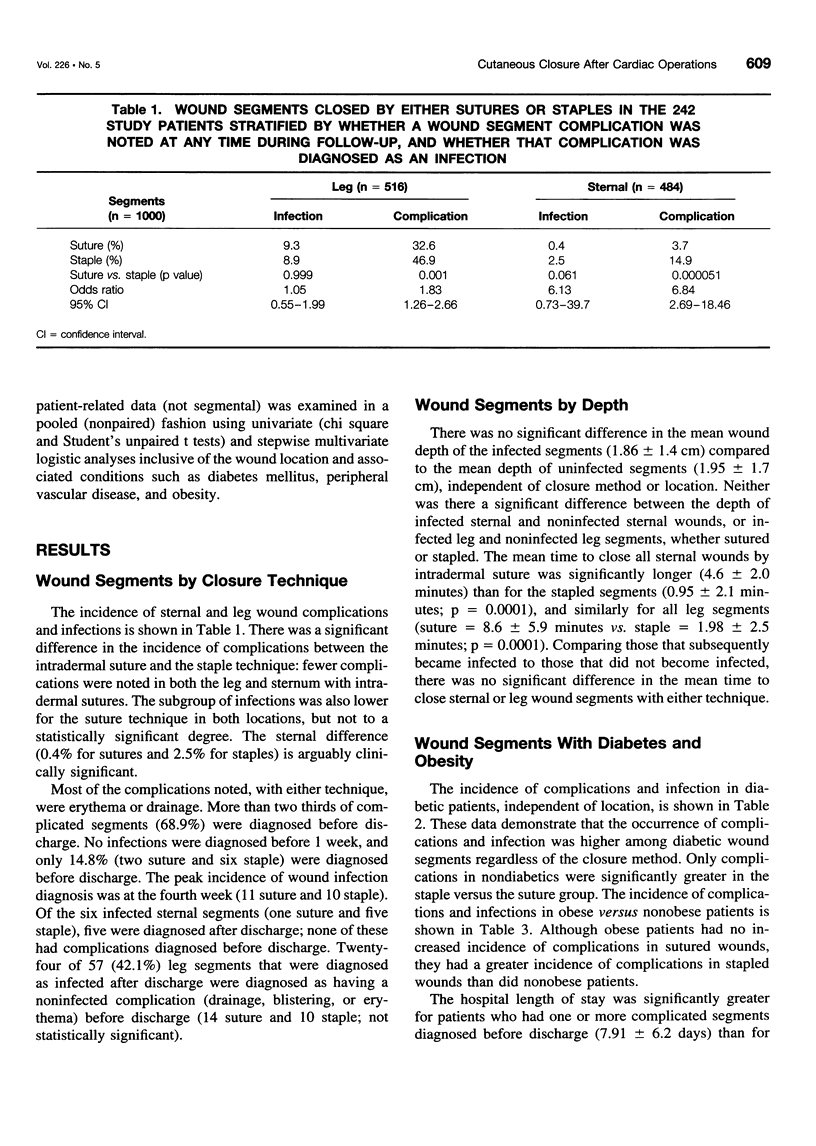
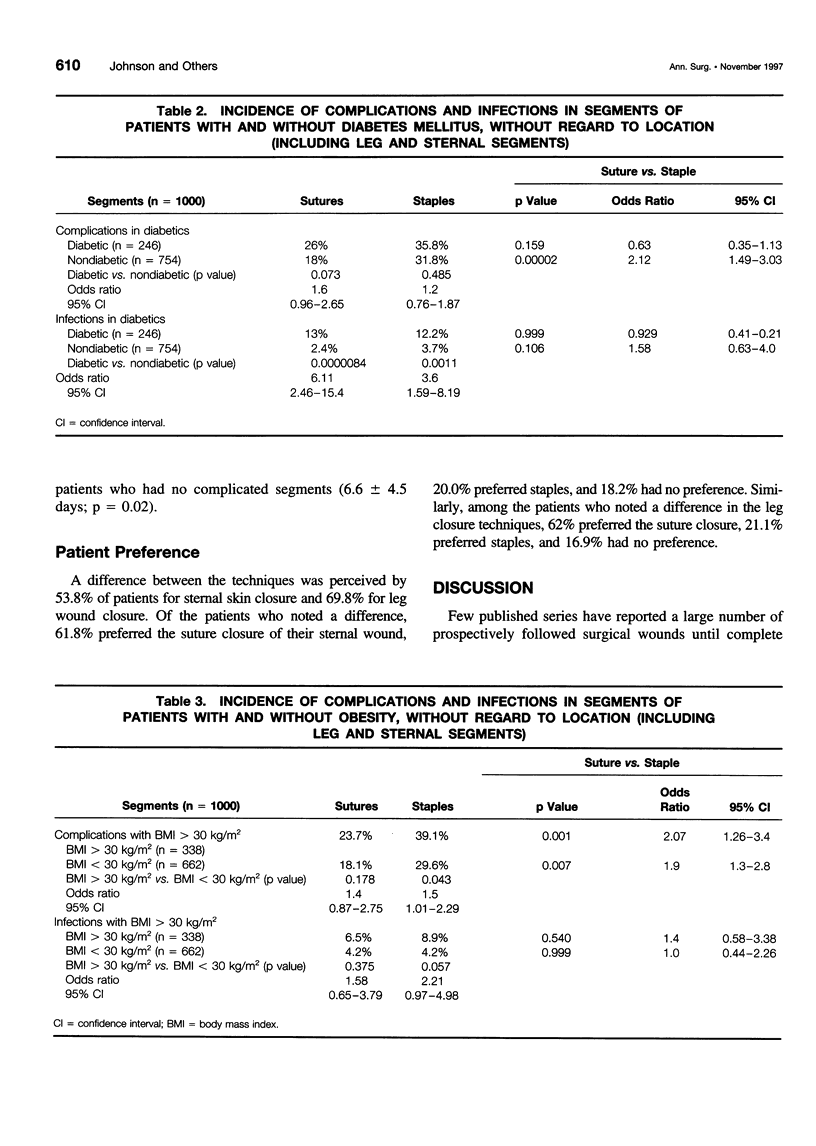
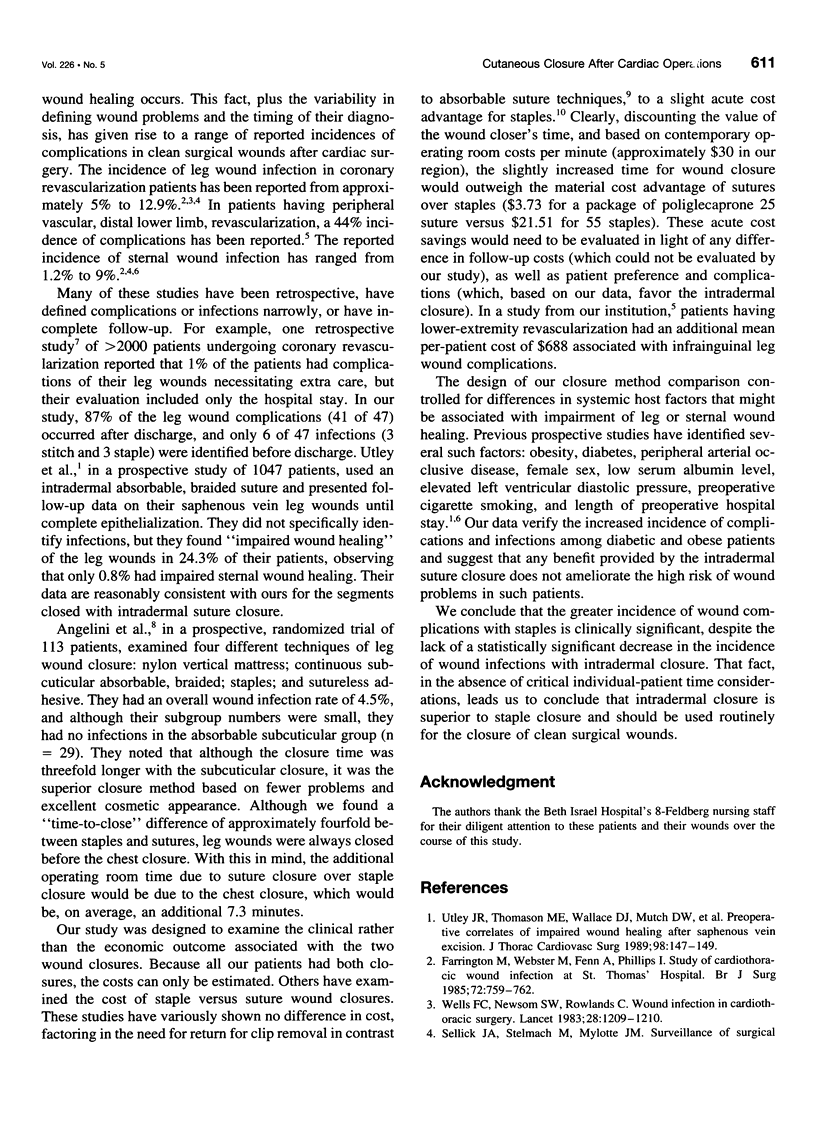
OBJECTIVE: To determine the difference in wound complication and infection rates between suture and staple closure techniques applied to clean incisions in coronary bypass patients. BACKGROUND: The true incidence of postoperative wound complications, and their correlation with closure techniques, has been obscured by study designs incorporating small numbers, retrospective short follow-up, uncontrolled host factors, and narrowly defined complications. METHODS: Sternal and leg wounds were studied prospectively, each patient serving as his or her own control. Two hundred forty-two patients with sternal and saphenous vein harvest wounds had half of each wound closed with staples and the other half with intradermal sutures (484 sternal and 516 leg segments). Wound complications were defined as drainage, erythema, separation, necrosis, seroma, or infection. Infections were identified in the subset having purulent drainage, antibiotic therapy, or debridement. Wounds were examined at discharge, at 1 week after discharge, and at 3 to 4 weeks after operation. Patient preferences for closure type were assessed 3 to 4 weeks after operation. RESULTS: Neither leg nor sternal wounds had a statistically significant difference in infection rate according to closure method (leg sutured = 9.3% vs. leg stapled = 8.9%; p = 0.99, and sternal sutured = 0.4% vs. sternal stapled = 2.5%; p = 0.128). There was, however, a greater complication rate in stapled segments (leg stapled = 46.9% vs. leg sutured = 32.6%; p = 0.001, and sternal stapled = 14.9% vs. sternal sutured = 3.7%; p = 0.00005). Sutures were favored over staples among patients who expressed a preference (sternal = 75.6%, leg = 74.6%). CONCLUSIONS: With the host factors controlled by pairing staples and sutures in each patient, we demonstrated a similar incidence of infection but a significantly lower incidence of total wound complications with intradermal suture closure than with staple closure.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Angelini G. D., Butchart E. G., Armistead S. H., Breckenridge I. M. Comparative study of leg wound skin closure in coronary artery bypass graft operations. Thorax. 1984 Dec;39(12):942–945. doi: 10.1136/thx.39.12.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLaria G. A., Hunter J. A., Goldin M. D., Serry C., Javid H., Najafi H. Leg wound complications associated with coronary revascularization. J Thorac Cardiovasc Surg. 1981 Mar;81(3):403–407. [PubMed] [Google Scholar]
- Farrington M., Webster M., Fenn A., Phillips I. Study of cardiothoracic wound infection at St. Thomas' Hospital. Br J Surg. 1985 Sep;72(9):759–762. doi: 10.1002/bjs.1800720932. [DOI] [PubMed] [Google Scholar]
- Kent K. C., Bartek S., Kuntz K. M., Anninos E., Skillman J. J. Prospective study of wound complications in continuous infrainguinal incisions after lower limb arterial reconstruction: incidence, risk factors, and cost. Surgery. 1996 Apr;119(4):378–383. doi: 10.1016/s0039-6060(96)80135-8. [DOI] [PubMed] [Google Scholar]
- Nagachinta T., Stephens M., Reitz B., Polk B. F. Risk factors for surgical-wound infection following cardiac surgery. J Infect Dis. 1987 Dec;156(6):967–973. doi: 10.1093/infdis/156.6.967. [DOI] [PubMed] [Google Scholar]
- Orlinsky M., Goldberg R. M., Chan L., Puertos A., Slajer H. L. Cost analysis of stapling versus suturing for skin closure. Am J Emerg Med. 1995 Jan;13(1):77–81. doi: 10.1016/0735-6757(95)90248-1. [DOI] [PubMed] [Google Scholar]
- Ranaboldo C. J., Rowe-Jones D. C. Closure of laparotomy wounds: skin staples versus sutures. Br J Surg. 1992 Nov;79(11):1172–1173. doi: 10.1002/bjs.1800791122. [DOI] [PubMed] [Google Scholar]
- Sellick J. A., Jr, Stelmach M., Mylotte J. M. Surveillance of surgical wound infections following open heart surgery. Infect Control Hosp Epidemiol. 1991 Oct;12(10):591–596. doi: 10.1086/646247. [DOI] [PubMed] [Google Scholar]
- Utley J. R., Thomason M. E., Wallace D. J., Mutch D. W., Staton L., Brown V., Wilde C. M., Bell M. S. Preoperative correlates of impaired wound healing after saphenous vein excision. J Thorac Cardiovasc Surg. 1989 Jul;98(1):147–149. [PubMed] [Google Scholar]
- Wells F. C., Newsom S. W., Rowlands C. Wound infection in cardiothoracic surgery. Lancet. 1983 May 28;1(8335):1209–1210. doi: 10.1016/s0140-6736(83)92479-0. [DOI] [PubMed] [Google Scholar]


