Abstract
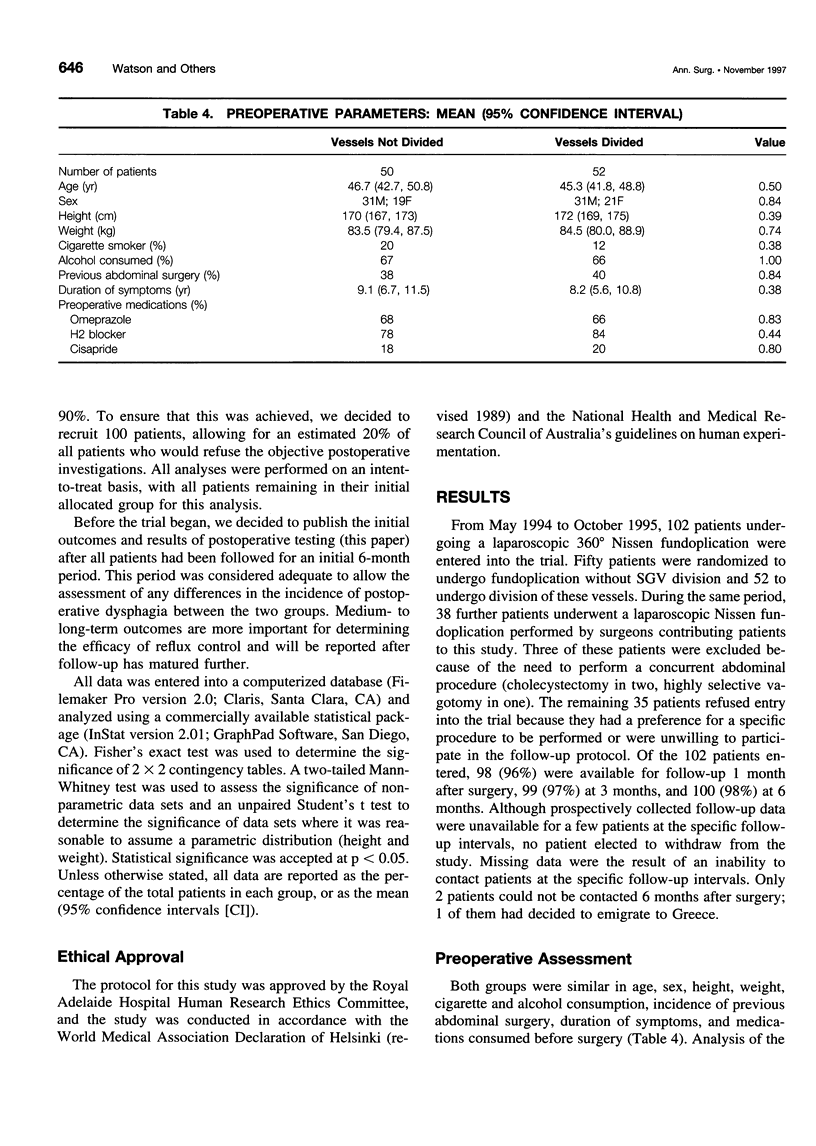
OBJECTIVE: To determine whether division of the short gastric vessels (SGVs) and full mobilization of the gastric fundus is necessary to reduce the incidence of postoperative dysphagia and other adverse sequelae of laparoscopic Nissen fundoplication. SUMMARY BACKGROUND DATA: Based on historical and uncontrolled studies, division of the SGVs has been advocated during laparoscopic Nissen fundoplication to improve postoperative clinical outcomes. However, this modification has not been evaluated in a large prospective randomized trial. METHODS: One hundred two patients with proven gastroesophageal reflux disease presenting for laparoscopic Nissen fundoplication were prospectively randomized to undergo fundoplication with (52 patients) or without (50 patients) division of the SGVs. Patients with esophageal motility disorders, patients requiring a concurrent abdominal procedure, and patients who had undergone previous antireflux surgery were excluded. Patients were blinded to the postoperative status of their SGVs. Clinical assessment was performed by a blinded independent investigator who used multiple standardized clinical grading systems to assess dysphagia, heartburn, and patient satisfaction 1, 3, and 6 months after surgery. Objective measurement of lower esophageal sphincter pressure, esophageal emptying time, and distal esophageal acid exposure and radiologic assessment of postoperative anatomy were also performed. RESULTS: Operating time was increased by 40 minutes (median 65 vs. 105) by vessel division. Perioperative outcomes and complications, postoperative dysphagia, relief of heartburn, and overall satisfaction were not improved by dividing the SGVs. Lower esophageal sphincter pressure, acid exposure, and esophageal emptying times were similar for the two groups. CONCLUSION: Division of the SGVs during laparoscopic Nissen fundoplication did not improve any clinical or objective postoperative outcome.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anvari M., Allen C., Borm A. Laparoscopic Nissen fundoplication is a satisfactory alternative to long-term omeprazole therapy. Br J Surg. 1995 Jul;82(7):938–942. doi: 10.1002/bjs.1800820728. [DOI] [PubMed] [Google Scholar]
- Dakkak M., Bennett J. R. A new dysphagia score with objective validation. J Clin Gastroenterol. 1992 Mar;14(2):99–100. doi: 10.1097/00004836-199203000-00004. [DOI] [PubMed] [Google Scholar]
- Dallemagne B., Weerts J. M., Jehaes C., Markiewicz S. Causes of failures of laparoscopic antireflux operations. Surg Endosc. 1996 Mar;10(3):305–310. doi: 10.1007/BF00187377. [DOI] [PubMed] [Google Scholar]
- DeMeester T. R., Bonavina L., Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg. 1986 Jul;204(1):9–20. doi: 10.1097/00000658-198607000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., Stein H. J. Minimizing the side effects of antireflux surgery. World J Surg. 1992 Mar-Apr;16(2):335–336. doi: 10.1007/BF02071542. [DOI] [PubMed] [Google Scholar]
- Donahue P. E., Samelson S., Nyhus L. M., Bombeck C. T. The floppy Nissen fundoplication. Effective long-term control of pathologic reflux. Arch Surg. 1985 Jun;120(6):663–668. doi: 10.1001/archsurg.1985.01390300013002. [DOI] [PubMed] [Google Scholar]
- Geagea T. Laparoscopic Nissen-Rossetti fundoplication. Surg Endosc. 1994 Sep;8(9):1080–1084. doi: 10.1007/BF00705724. [DOI] [PubMed] [Google Scholar]
- Hinder R. A., Filipi C. J., Wetscher G., Neary P., DeMeester T. R., Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994 Oct;220(4):472–483. doi: 10.1097/00000658-199410000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson G. G., Watson D. I., Britten-Jones R., Mitchell P. C., Anvari M. Laparoscopic Nissen fundoplication. Ann Surg. 1994 Aug;220(2):137–145. doi: 10.1097/00000658-199408000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laycock W. S., Trus T. L., Hunter J. G. New technology for the division of short gastric vessels during laparoscopic Nissen fundoplication. A prospective randomized trial. Surg Endosc. 1996 Jan;10(1):71–73. doi: 10.1007/s004649910019. [DOI] [PubMed] [Google Scholar]
- Leonardi H. K., Crozier R. E., Ellis F. H., Jr Reoperation for complications of the Nissen fundoplication. J Thorac Cardiovasc Surg. 1981 Jan;81(1):50–56. [PubMed] [Google Scholar]
- Lundell L., Myers J. C., Jamieson G. G. The effect of antireflux operations on lower oesophageal sphincter tone and postprandial symptoms. Scand J Gastroenterol. 1993 Aug;28(8):725–731. doi: 10.3109/00365529309098281. [DOI] [PubMed] [Google Scholar]
- McKernan J. B., Champion J. K. Laparoscopic antireflux surgery. Am Surg. 1995 Jun;61(6):530–536. [PubMed] [Google Scholar]
- Peters J. H., Heimbucher J., Kauer W. K., Incarbone R., Bremner C. G., DeMeester T. R. Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg. 1995 Apr;180(4):385–393. [PubMed] [Google Scholar]
- Rieger N. A., Jamieson G. G., Britten-Jones R., Tew S. Reoperation after failed antireflux surgery. Br J Surg. 1994 Aug;81(8):1159–1161. doi: 10.1002/bjs.1800810825. [DOI] [PubMed] [Google Scholar]
- Rossetti M., Hell K. Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg. 1977 Jul;1(4):439–443. doi: 10.1007/BF01565907. [DOI] [PubMed] [Google Scholar]
- Swanstrom L. L., Pennings J. L. Laparoscopic control of short gastric vessels. J Am Coll Surg. 1995 Oct;181(4):347–351. [PubMed] [Google Scholar]
- Watson A., Jenkinson L. R., Ball C. S., Barlow A. P., Norris T. L. A more physiological alternative to total fundoplication for the surgical correction of resistant gastro-oesophageal reflux. Br J Surg. 1991 Sep;78(9):1088–1094. doi: 10.1002/bjs.1800780918. [DOI] [PubMed] [Google Scholar]
- Watson D. I., Jamieson G. G., Devitt P. G., Matthew G., Britten-Jones R. E., Game P. A., Williams R. S. Changing strategies in the performance of laparoscopic Nissen fundoplication as a result of experience with 230 operations. Surg Endosc. 1995 Sep;9(9):961–966. doi: 10.1007/BF00188451. [DOI] [PubMed] [Google Scholar]


