Abstract
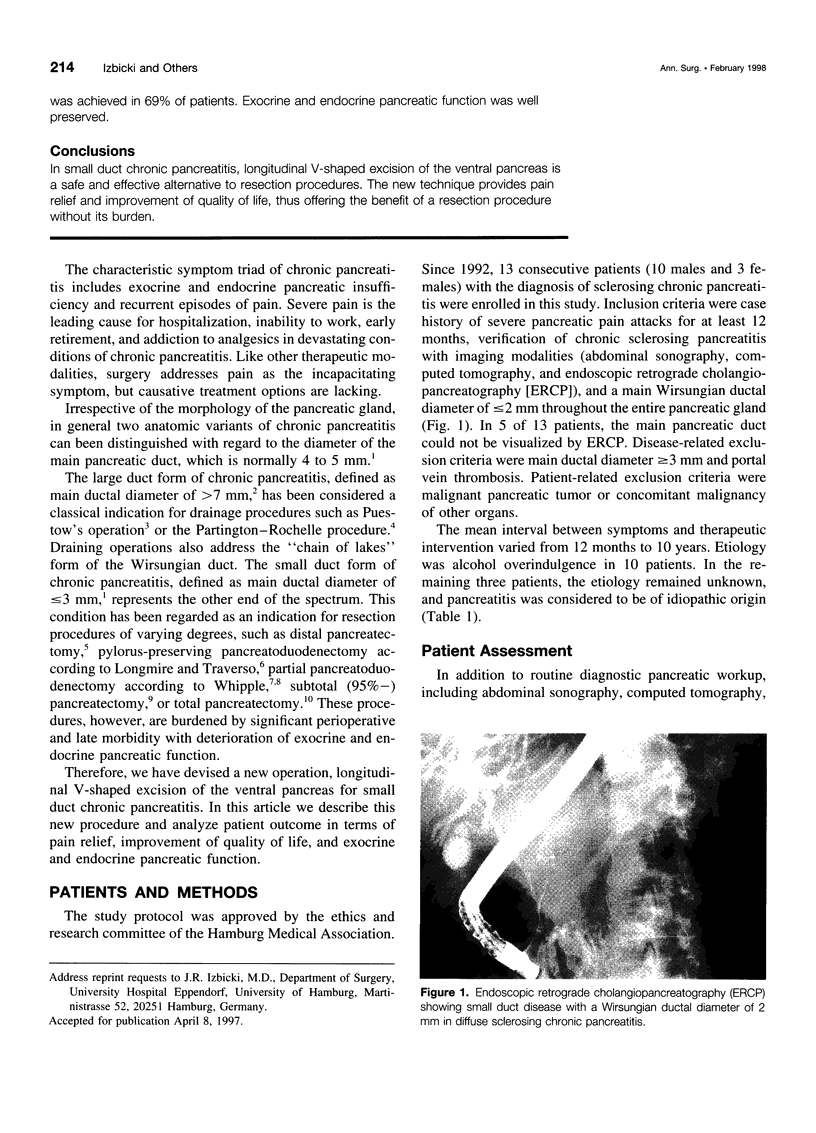
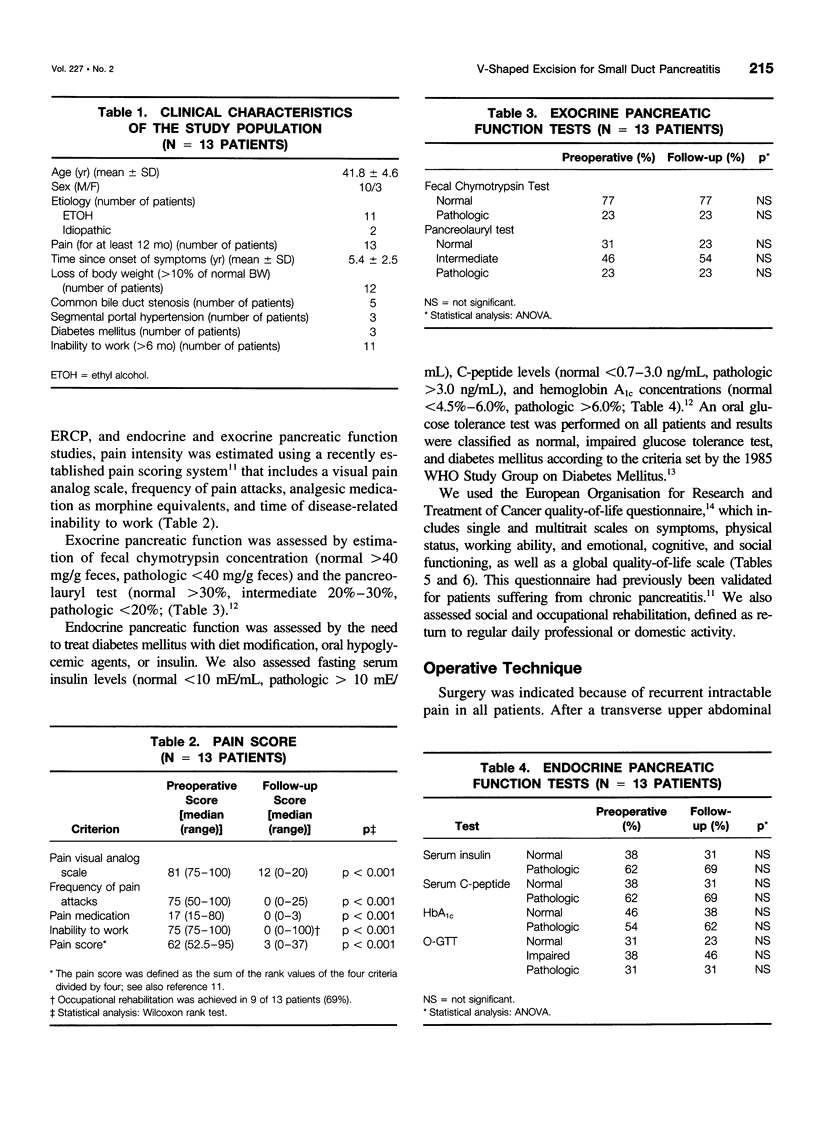
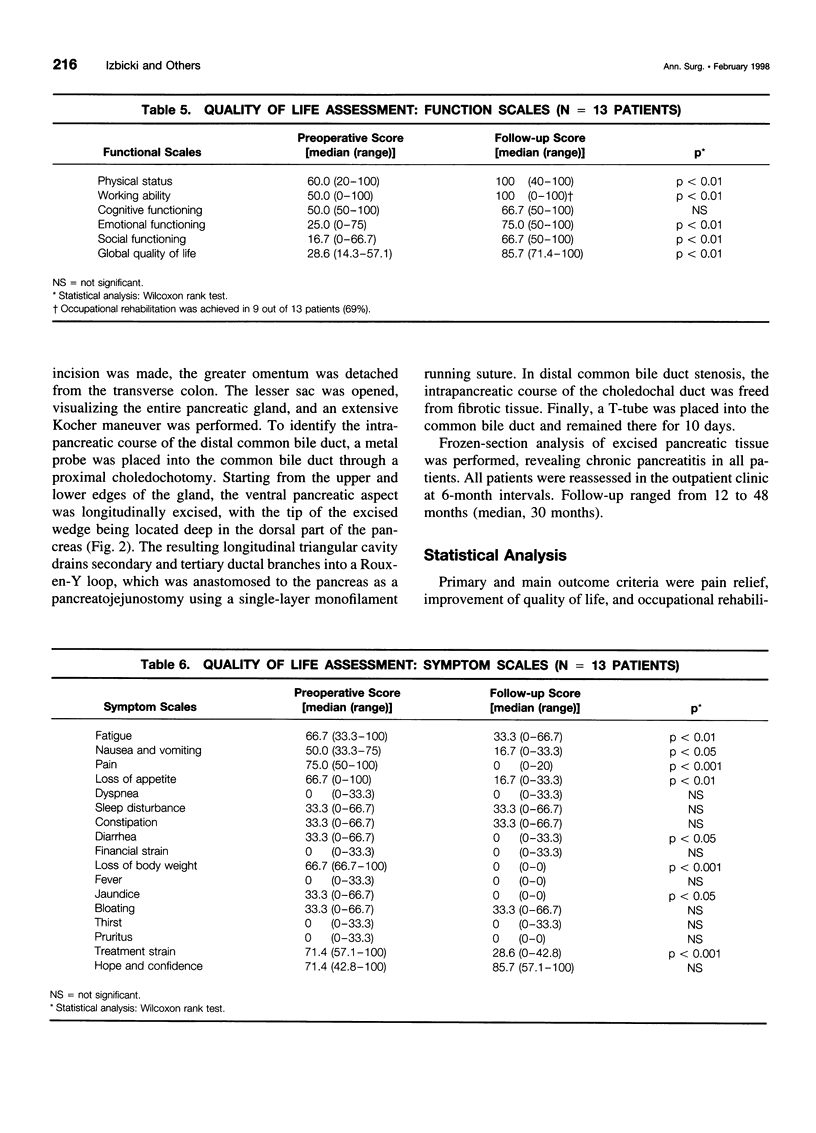
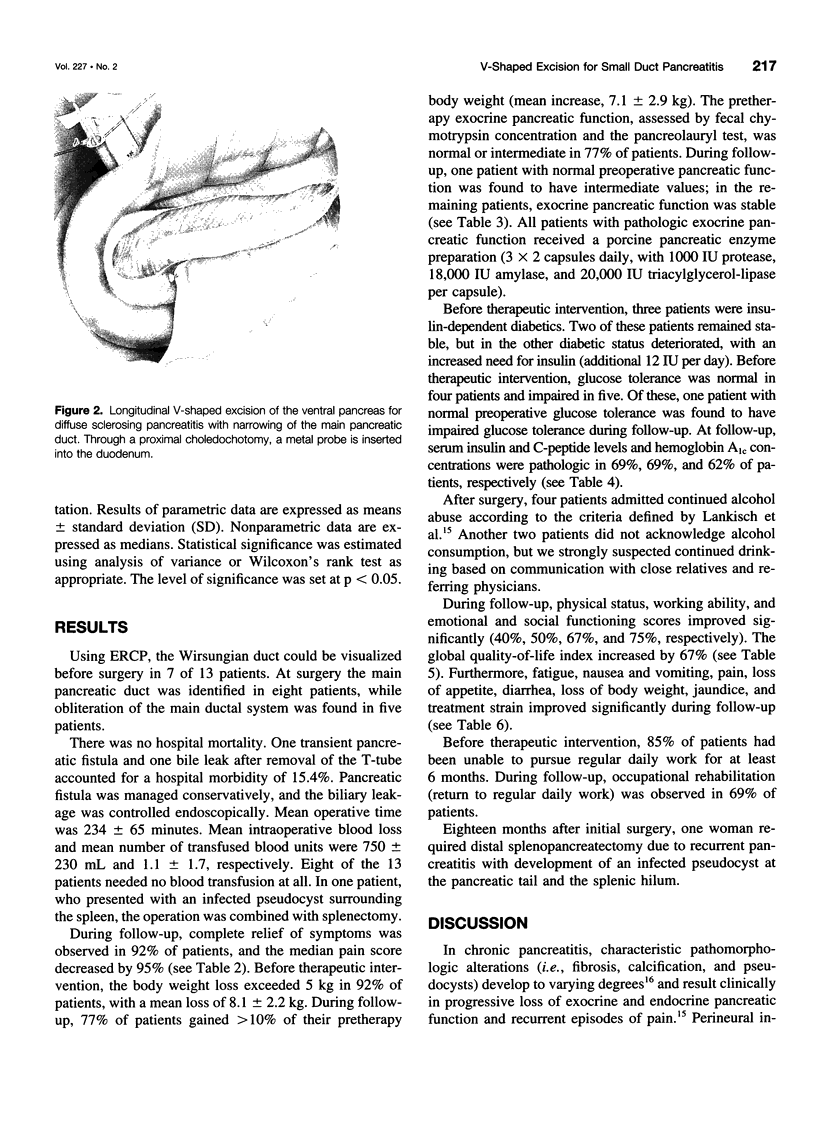
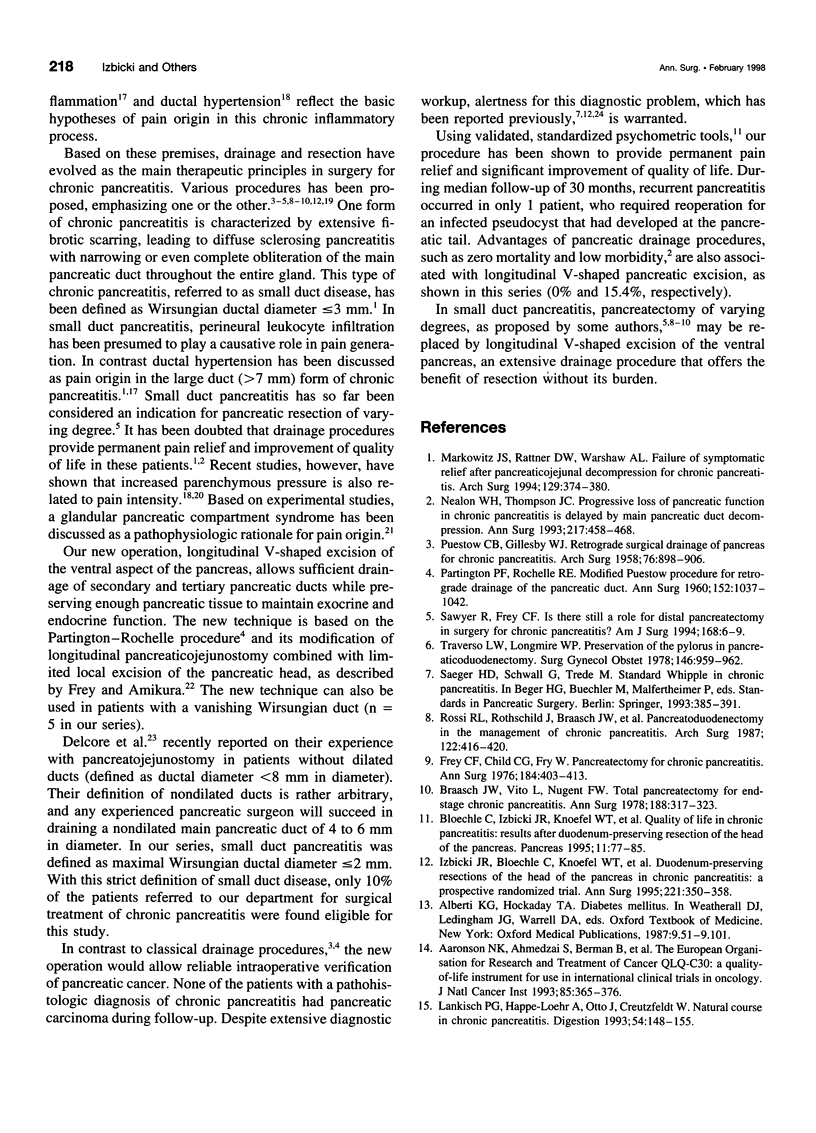
OBJECTIVE: The technique of longitudinal V-shaped excision of the ventral pancreas for small duct chronic pancreatitis is presented and its efficacy in terms of pain relief and improvement of quality of life is evaluated. SUMMARY BACKGROUND DATA: Small duct chronic pancreatitis has been regarded as a classical indication for more or less extensive resection, in which the therapeutic success of pain relief is offset by the considerable risk of significant perioperative mortality and morbidity and the burden of substantial loss of pancreatic function. METHODS: Thirteen patients with severe pain who were diagnosed with small duct pancreatitis (defined as maximal Wirsungian ductal diameter of 2 mm) underwent longitudinal V-shaped excision of the ventral pancreas. In addition to routine pancreatic workup, a multidimensional psychometric quality-of-life questionnaire and a pain score were used. Assessment of exocrine and endocrine function included fecal chymotrypsin and the pancreolauryl test as well as oral glucose tolerance, serum concentrations of insulin, C-peptide, and hemoglobin A1c. The interval between symptoms and surgery ranged from 12 months to 10 years (mean, 5.4 years). Median follow-up was 30 months (range, 12-48 months). RESULTS: There were no deaths. Overall morbidity was 15.4%. In 92% of patients, complete relief of symptoms was obtained. Median pain score decreased by 95%. Physical status, working ability, and emotional and social functioning scores improved by 40%, 50%, 67%,, and 75%, respectively. Global quality-of-life index increased by 67%. Occupational rehabilitation was achieved in 69% of patients. Exocrine and endocrine pancreatic function was well preserved. CONCLUSIONS: In small duct chronic pancreatitis, longitudinal V-shaped excision of the ventral pancreas is a safe and effective alternative to resection procedures. The new technique provides pain relief and improvement of quality of life, thus offering the benefit of a resection procedure without its burden.
Full text
PDF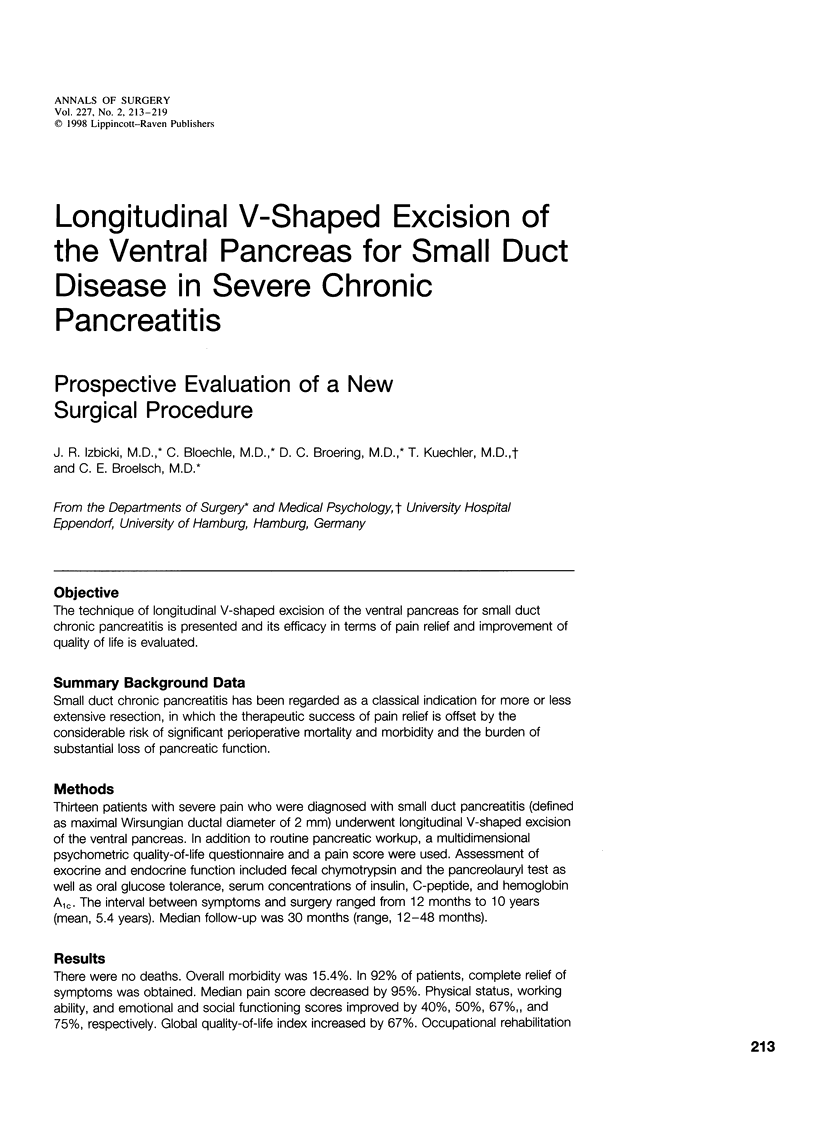

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aaronson N. K., Ahmedzai S., Bergman B., Bullinger M., Cull A., Duez N. J., Filiberti A., Flechtner H., Fleishman S. B., de Haes J. C. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993 Mar 3;85(5):365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- Bloechle C., Izbicki J. R., Knoefel W. T., Kuechler T., Broelsch C. E. Quality of life in chronic pancreatitis--results after duodenum-preserving resection of the head of the pancreas. Pancreas. 1995 Jul;11(1):77–85. doi: 10.1097/00006676-199507000-00008. [DOI] [PubMed] [Google Scholar]
- Bockman D. E., Buchler M., Malfertheiner P., Beger H. G. Analysis of nerves in chronic pancreatitis. Gastroenterology. 1988 Jun;94(6):1459–1469. doi: 10.1016/0016-5085(88)90687-7. [DOI] [PubMed] [Google Scholar]
- Braasch J. W., Vito L., Nugent F. W. Total pancreatectomy of end-stage chronic pancreatitis. Ann Surg. 1978 Sep;188(3):317–322. doi: 10.1097/00000658-197809000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delcore R., Rodriguez F. J., Thomas J. H., Forster J., Hermreck A. S. The role of pancreatojejunostomy in patients without dilated pancreatic ducts. Am J Surg. 1994 Dec;168(6):598–602. doi: 10.1016/s0002-9610(05)80129-1. [DOI] [PubMed] [Google Scholar]
- Ebbehøj N., Svendsen L. B., Madsen P. Pancreatic tissue pressure: techniques and pathophysiological aspects. Scand J Gastroenterol. 1984 Nov;19(8):1066–1068. [PubMed] [Google Scholar]
- Frey C. F., Amikura K. Local resection of the head of the pancreas combined with longitudinal pancreaticojejunostomy in the management of patients with chronic pancreatitis. Ann Surg. 1994 Oct;220(4):492–507. doi: 10.1007/BF02348284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey C. F., Child C. G., Fry W. Pancreatectomy for chronic pancreatitis. Ann Surg. 1976 Oct;184(4):403–413. doi: 10.1097/00000658-197610000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izbicki J. R., Bloechle C., Knoefel W. T., Kuechler T., Binmoeller K. F., Broelsch C. E. Duodenum-preserving resection of the head of the pancreas in chronic pancreatitis. A prospective, randomized trial. Ann Surg. 1995 Apr;221(4):350–358. doi: 10.1097/00000658-199504000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karanjia N. D., Widdison A. L., Leung F., Alvarez C., Lutrin F. J., Reber H. A. Compartment syndrome in experimental chronic obstructive pancreatitis: effect of decompressing the main pancreatic duct. Br J Surg. 1994 Feb;81(2):259–264. doi: 10.1002/bjs.1800810236. [DOI] [PubMed] [Google Scholar]
- Klöppel G., Maillet B. Pathology of acute and chronic pancreatitis. Pancreas. 1993 Nov;8(6):659–670. doi: 10.1097/00006676-199311000-00001. [DOI] [PubMed] [Google Scholar]
- Lankisch P. G., Löhr-Happe A., Otto J., Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion. 1993;54(3):148–155. doi: 10.1159/000201029. [DOI] [PubMed] [Google Scholar]
- Markowitz J. S., Rattner D. W., Warshaw A. L. Failure of symptomatic relief after pancreaticojejunal decompression for chronic pancreatitis. Strategies for salvage. Arch Surg. 1994 Apr;129(4):374–380. doi: 10.1001/archsurg.1994.01420280044006. [DOI] [PubMed] [Google Scholar]
- Nealon W. H., Thompson J. C. Progressive loss of pancreatic function in chronic pancreatitis is delayed by main pancreatic duct decompression. A longitudinal prospective analysis of the modified puestow procedure. Ann Surg. 1993 May;217(5):458–468. doi: 10.1097/00000658-199305010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PARTINGTON P. F., ROCHELLE R. E. Modified Puestow procedure for retrograde drainage of the pancreatic duct. Ann Surg. 1960 Dec;152:1037–1043. doi: 10.1097/00000658-196012000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PUESTOW C. B., GILLESBY W. J. Retrograde surgical drainage of pancreas for chronic relapsing pancreatitis. AMA Arch Surg. 1958 Jun;76(6):898–907. doi: 10.1001/archsurg.1958.01280240056009. [DOI] [PubMed] [Google Scholar]
- Rossi R. L., Rothschild J., Braasch J. W., Munson J. L., ReMine S. G. Pancreatoduodenectomy in the management of chronic pancreatitis. Arch Surg. 1987 Apr;122(4):416–420. doi: 10.1001/archsurg.1987.01400160042004. [DOI] [PubMed] [Google Scholar]
- Sawyer R., Frey C. F. Is there still a role for distal pancreatectomy in surgery for chronic pancreatitis? Am J Surg. 1994 Jul;168(1):6–9. doi: 10.1016/s0002-9610(05)80061-3. [DOI] [PubMed] [Google Scholar]
- Traverso L. W., Longmire W. P., Jr Preservation of the pylorus in pancreaticoduodenectomy. Surg Gynecol Obstet. 1978 Jun;146(6):959–962. [PubMed] [Google Scholar]
- Whipple A. O. Radical Surgery for Certain Cases of Pancreatic Fibrosis associated with Calcareous Deposits. Ann Surg. 1946 Dec;124(6):991–1006. [PMC free article] [PubMed] [Google Scholar]
- White T. T., Hart M. J. Pancreaticojejunostomy versus resection in the treatment of chronic pancreatitis. Am J Surg. 1979 Jul;138(1):129–134. doi: 10.1016/0002-9610(79)90252-6. [DOI] [PubMed] [Google Scholar]