Abstract
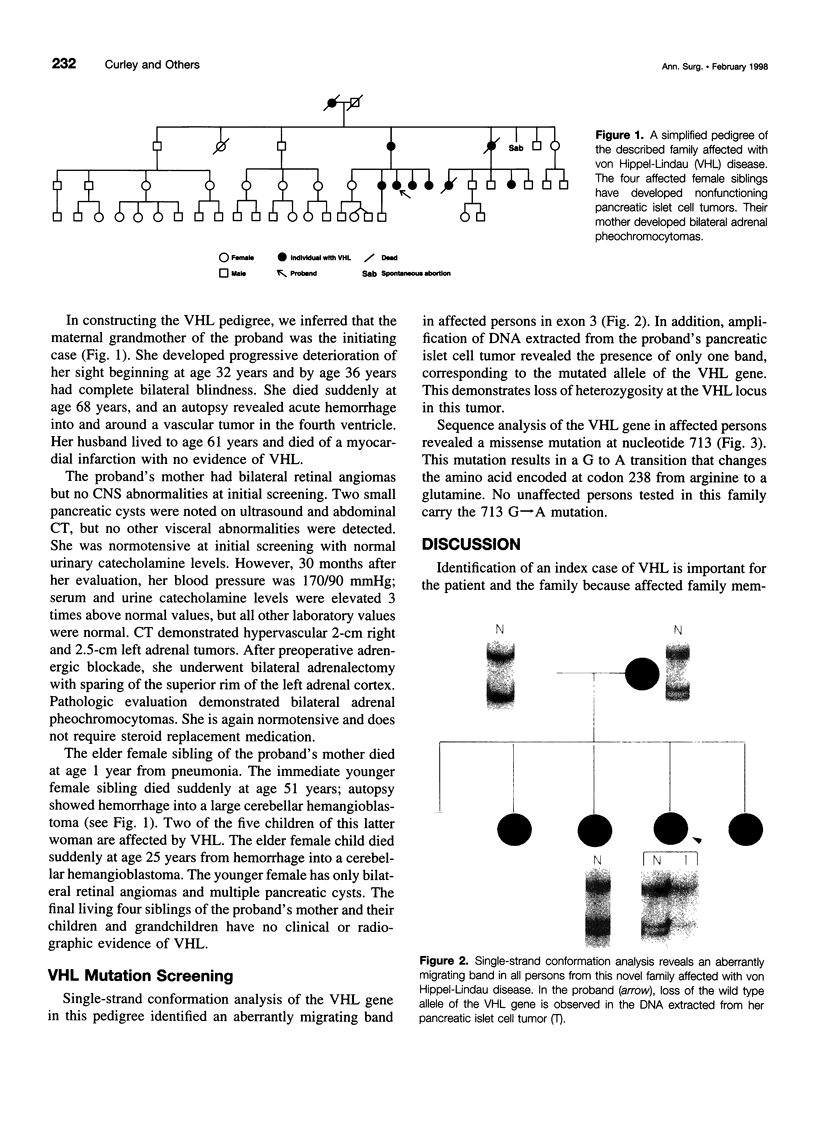
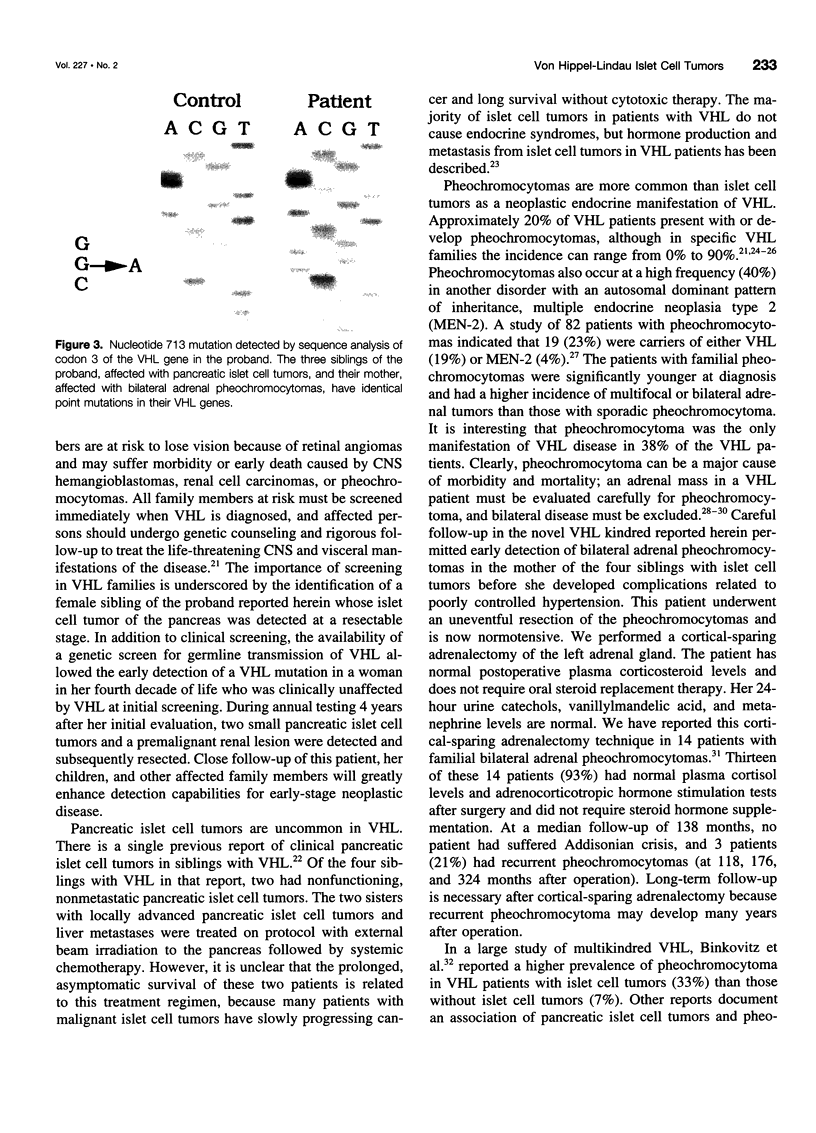
OBJECTIVE: We report a unique, previously undescribed multigeneration kindred with von Hippel-Lindau (VHL) disease in whom clinical or genetic screening led to the detection of surgically resectable neoplastic disease in several family members. SUMMARY BACKGROUND DATA: Patients with VHL disease have a propensity to develop neoplasms of several different organ sites. Retinal angiomas, cerebellar and spinal hemangioblastomas, solid organ cysts, and renal carcinoma are common lesions; pheochromocytomas and pancreatic islet cell tumors occur less frequently but are important causes of morbidity and mortality. METHODS: A detailed pedigree was constructed based on clinical screening and family history that describes the development of pancreatic islet cell tumors in four of five female siblings. VHL mutation analysis was performed in an attempt to determine if genotype-phenotype correlations could be made in this interesting family. RESULTS: The age of onset of VHL-associated neoplasms for three affected siblings was in the third decade of life and in the fourth decade for the fourth sibling. The mother of the four siblings affected with pancreatic tumors developed bilateral pheochromocytomas in the seventh decade of life; she has no pancreatic or kidney tumors. We identified maternal transmission of a missense mutation in codon 238 in exon 3 of the VHL gene in the four affected siblings with pancreatic islet cell tumors. Mutation screening on unaffected family members showed no abnormalities in the VHL gene. Interestingly, one of the four affected siblings had no evidence of VHL on her initial clinical screening evaluation; however, she was followed closely because of her mutated VHL gene. Four years after initial screening, she developed two pancreatic islet cell tumors and a premalignant renal cyst. CONCLUSIONS: Clinical and genetic screening for VHL in this family had a significant impact on surgical management by detecting early-stage islet cell tumors or pheochromocytomas. Furthermore, we conclude that the preponderance of pancreatic islet cell tumors in this family cannot be explained by a strict genotype-phenotype correlation. This suggests that additional genetic abnormalities, possibly on chromosome 3p where the VHL gene is located, may be responsible for the variety of VHL-associated neoplasms.
Full text
PDF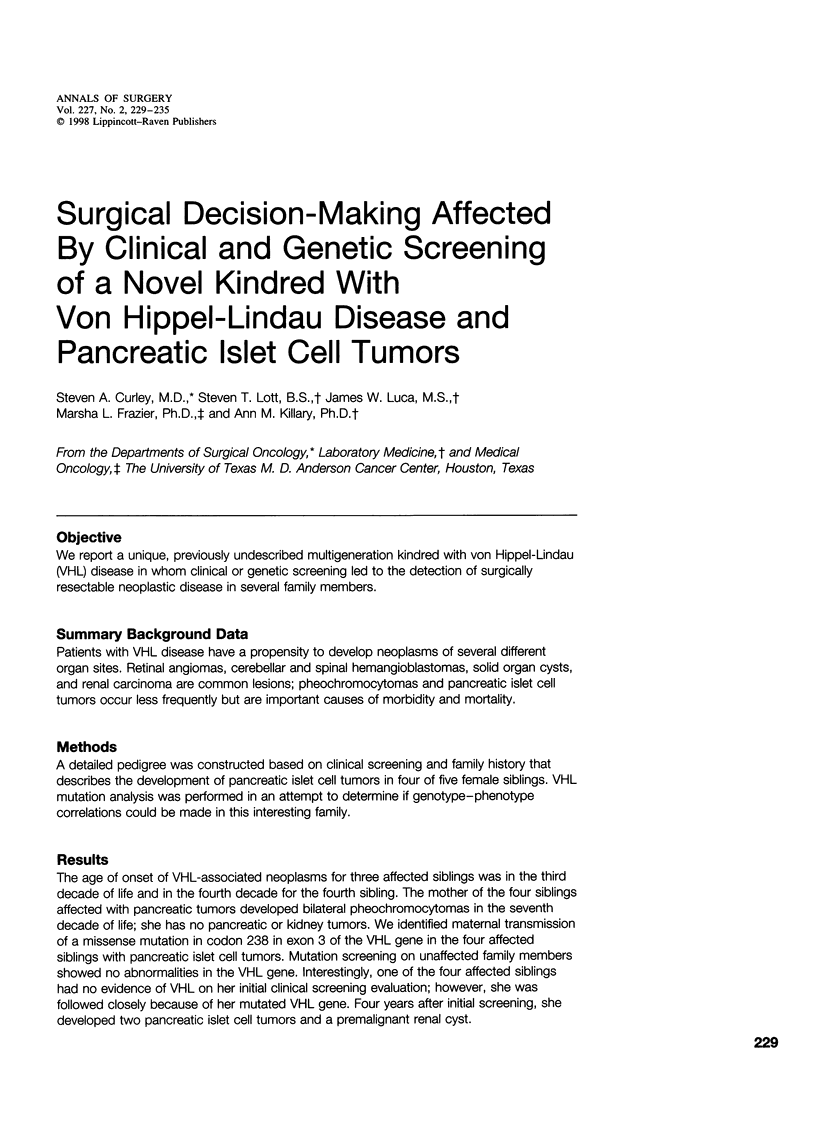


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aprill B. S., Drake A. J., 3rd, Lasseter D. H., Shakir K. M. Silent adrenal nodules in von Hippel-Lindau disease suggest pheochromocytoma. Ann Intern Med. 1994 Mar 15;120(6):485–487. doi: 10.7326/0003-4819-120-6-199403150-00006. [DOI] [PubMed] [Google Scholar]
- Atuk N. O., McDonald T., Wood T., Carpenter J. T., Walzak M. P., Donaldson M., Gillenwater J. Y. Familial pheochromocytoma, hypercalcemia, and von Hippel-Lindau disease. A ten year study of a large family. Medicine (Baltimore) 1979 May;58(3):209–218. doi: 10.1097/00005792-197905000-00001. [DOI] [PubMed] [Google Scholar]
- Binkovitz L. A., Johnson C. D., Stephens D. H. Islet cell tumors in von Hippel-Lindau disease: increased prevalence and relationship to the multiple endocrine neoplasias. AJR Am J Roentgenol. 1990 Sep;155(3):501–505. doi: 10.2214/ajr.155.3.1974734. [DOI] [PubMed] [Google Scholar]
- Chew S. L., Dacie J. E., Reznek R. H., Newbould E. C., Sheaves R., Trainer P. J., Lowe D. G., Shand W. S., Hungerford J., Besser G. M. Bilateral phaeochromocytomas in von Hippel-Lindau disease: diagnosis by adrenal vein sampling and catecholamine assay. Q J Med. 1994 Jan;87(1):49–54. [PubMed] [Google Scholar]
- Cohen A. J., Li F. P., Berg S., Marchetto D. J., Tsai S., Jacobs S. C., Brown R. S. Hereditary renal-cell carcinoma associated with a chromosomal translocation. N Engl J Med. 1979 Sep 13;301(11):592–595. doi: 10.1056/NEJM197909133011107. [DOI] [PubMed] [Google Scholar]
- Cornish D., Pont A., Minor D., Coombs J. L., Bennington J. Metastatic islet cell tumor in von Hippel-Lindau disease. Am J Med. 1984 Jul;77(1):147–150. doi: 10.1016/0002-9343(84)90450-9. [DOI] [PubMed] [Google Scholar]
- Crossey P. A., Foster K., Richards F. M., Phipps M. E., Latif F., Tory K., Jones M. H., Bentley E., Kumar R., Lerman M. I. Molecular genetic investigations of the mechanism of tumourigenesis in von Hippel-Lindau disease: analysis of allele loss in VHL tumours. Hum Genet. 1994 Jan;93(1):53–58. doi: 10.1007/BF00218913. [DOI] [PubMed] [Google Scholar]
- Gnarra J. R., Tory K., Weng Y., Schmidt L., Wei M. H., Li H., Latif F., Liu S., Chen F., Duh F. M. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994 May;7(1):85–90. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- Gnarra J. R., Tory K., Weng Y., Schmidt L., Wei M. H., Li H., Latif F., Liu S., Chen F., Duh F. M. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994 May;7(1):85–90. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- Hough D. M., Stephens D. H., Johnson C. D., Binkovitz L. A. Pancreatic lesions in von Hippel-Lindau disease: prevalence, clinical significance, and CT findings. AJR Am J Roentgenol. 1994 May;162(5):1091–1094. doi: 10.2214/ajr.162.5.8165988. [DOI] [PubMed] [Google Scholar]
- Hull M. T., Warfel K. A., Muller J., Higgins J. T. Familial islet cell tumors in Von Hippel-Lindau's disease. Cancer. 1979 Oct;44(4):1523–1526. doi: 10.1002/1097-0142(197910)44:4<1523::aid-cncr2820440452>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Huson S. M., Harper P. S., Hourihan M. D., Cole G., Weeks R. D., Compston D. A. Cerebellar haemangioblastoma and von Hippel-Lindau disease. Brain. 1986 Dec;109(Pt 6):1297–1310. doi: 10.1093/brain/109.6.1297. [DOI] [PubMed] [Google Scholar]
- Jennings A. M., Smith C., Cole D. R., Jennings C., Shortland J. R., Williams J. L., Brown C. B. Von Hippel-Lindau disease in a large British family: clinicopathological features and recommendations for screening and follow-up. Q J Med. 1988 Mar;66(251):233–249. [PubMed] [Google Scholar]
- Jennings C. M., Gaines P. A. The abdominal manifestation of von Hippel-Lindau disease and a radiological screening protocol for an affected family. Clin Radiol. 1988 Jul;39(4):363–367. doi: 10.1016/s0009-9260(88)80266-6. [DOI] [PubMed] [Google Scholar]
- Kanno H., Kondo K., Ito S., Yamamoto I., Fujii S., Torigoe S., Sakai N., Hosaka M., Shuin T., Yao M. Somatic mutations of the von Hippel-Lindau tumor suppressor gene in sporadic central nervous system hemangioblastomas. Cancer Res. 1994 Sep 15;54(18):4845–4847. [PubMed] [Google Scholar]
- Knudson A. G., Jr Genetics of human cancer. Annu Rev Genet. 1986;20:231–251. doi: 10.1146/annurev.ge.20.120186.001311. [DOI] [PubMed] [Google Scholar]
- Kovacs G., Emanuel A., Neumann H. P., Kung H. F. Cytogenetics of renal cell carcinomas associated with von Hippel-Lindau disease. Genes Chromosomes Cancer. 1991 Jul;3(4):256–262. doi: 10.1002/gcc.2870030404. [DOI] [PubMed] [Google Scholar]
- Lamiell J. M., Salazar F. G., Hsia Y. E. von Hippel-Lindau disease affecting 43 members of a single kindred. Medicine (Baltimore) 1989 Jan;68(1):1–29. doi: 10.1097/00005792-198901000-00001. [DOI] [PubMed] [Google Scholar]
- Latif F., Tory K., Gnarra J., Yao M., Duh F. M., Orcutt M. L., Stackhouse T., Kuzmin I., Modi W., Geil L. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993 May 28;260(5112):1317–1320. doi: 10.1126/science.8493574. [DOI] [PubMed] [Google Scholar]
- Lee J. E., Curley S. A., Gagel R. F., Evans D. B., Hickey R. C. Cortical-sparing adrenalectomy for patients with bilateral pheochromocytoma. Surgery. 1996 Dec;120(6):1064–1071. doi: 10.1016/s0039-6060(96)80056-0. [DOI] [PubMed] [Google Scholar]
- MELMON K. L., ROSEN S. W. LINDAU'S DISEASE. REVIEW OF THE LITERATURE AND STUDY OF A LARGE KINDRED. Am J Med. 1964 Apr;36:595–617. doi: 10.1016/0002-9343(64)90107-x. [DOI] [PubMed] [Google Scholar]
- Maher E. R., Iselius L., Yates J. R., Littler M., Benjamin C., Harris R., Sampson J., Williams A., Ferguson-Smith M. A., Morton N. Von Hippel-Lindau disease: a genetic study. J Med Genet. 1991 Jul;28(7):443–447. doi: 10.1136/jmg.28.7.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann H. P. Basic criteria for clinical diagnosis and genetic counselling in von Hippel-Lindau syndrome. Vasa. 1987;16(3):220–226. [PubMed] [Google Scholar]
- Neumann H. P., Berger D. P., Sigmund G., Blum U., Schmidt D., Parmer R. J., Volk B., Kirste G. Pheochromocytomas, multiple endocrine neoplasia type 2, and von Hippel-Lindau disease. N Engl J Med. 1993 Nov 18;329(21):1531–1538. doi: 10.1056/NEJM199311183292103. [DOI] [PubMed] [Google Scholar]
- Neumann H. P., Dinkel E., Brambs H., Wimmer B., Friedburg H., Volk B., Sigmund G., Riegler P., Haag K., Schollmeyer P. Pancreatic lesions in the von Hippel-Lindau syndrome. Gastroenterology. 1991 Aug;101(2):465–471. doi: 10.1016/0016-5085(91)90026-h. [DOI] [PubMed] [Google Scholar]
- Pathak S., Strong L. C., Ferrell R. E., Trindade A. Familial renal cell carcinoma with a 3;11 chromosome translocation limited to tumor cells. Science. 1982 Sep 3;217(4563):939–941. doi: 10.1126/science.7112106. [DOI] [PubMed] [Google Scholar]
- Phipps M. E., Maher E. R., Affara N. A., Latif F., Leversha M. A., Ferguson-Smith M. E., Nakamura Y., Lerman M., Zbar B., Ferguson-Smith M. A. Physical mapping of chromosome 3p25-p26 by fluorescence in situ hybridisation (FISH). Hum Genet. 1993 Aug;92(1):18–22. doi: 10.1007/BF00216139. [DOI] [PubMed] [Google Scholar]
- Sanchez Y., el-Naggar A., Pathak S., Killary A. M. A tumor suppressor locus within 3p14-p12 mediates rapid cell death of renal cell carcinoma in vivo. Proc Natl Acad Sci U S A. 1994 Apr 12;91(8):3383–3387. doi: 10.1073/pnas.91.8.3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz C. E., Ulmer J., Brown A., Pancoast I., Goodman H. O., Stevenson R. E. Allan-Herndon syndrome. II. Linkage to DNA markers in Xq21. Am J Hum Genet. 1990 Sep;47(3):454–458. [PMC free article] [PubMed] [Google Scholar]
- Seizinger B. R., Rouleau G. A., Ozelius L. J., Lane A. H., Farmer G. E., Lamiell J. M., Haines J., Yuen J. W., Collins D., Majoor-Krakauer D. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature. 1988 Mar 17;332(6161):268–269. doi: 10.1038/332268a0. [DOI] [PubMed] [Google Scholar]
- Sekido Y., Bader S., Latif F., Gnarra J. R., Gazdar A. F., Linehan W. M., Zbar B., Lerman M. I., Minna J. D. Molecular analysis of the von Hippel-Lindau disease tumor suppressor gene in human lung cancer cell lines. Oncogene. 1994 Jun;9(6):1599–1604. [PubMed] [Google Scholar]
- Tisherman S. E., Tisherman B. G., Tisherman S. A., Dunmire S., Levey G. S., Mulvihill J. J. Three-decade investigation of familial pheochromocytoma. An allele of von Hippel-Lindau disease? Arch Intern Med. 1993 Nov 22;153(22):2550–2556. [PubMed] [Google Scholar]
- Tsuchiya H., Iseda T., Hino O. Identification of a novel protein (VBP-1) binding to the von Hippel-Lindau (VHL) tumor suppressor gene product. Cancer Res. 1996 Jul 1;56(13):2881–2885. [PubMed] [Google Scholar]
- Yamakawa K., Takahashi E., Murata M., Okui K., Yokoyama S., Nakamura Y. Detailed mapping around the breakpoint of (3;8) translocation in familial renal cell carcinoma and FRA3B. Genomics. 1992 Oct;14(2):412–416. doi: 10.1016/s0888-7543(05)80234-4. [DOI] [PubMed] [Google Scholar]