Abstract
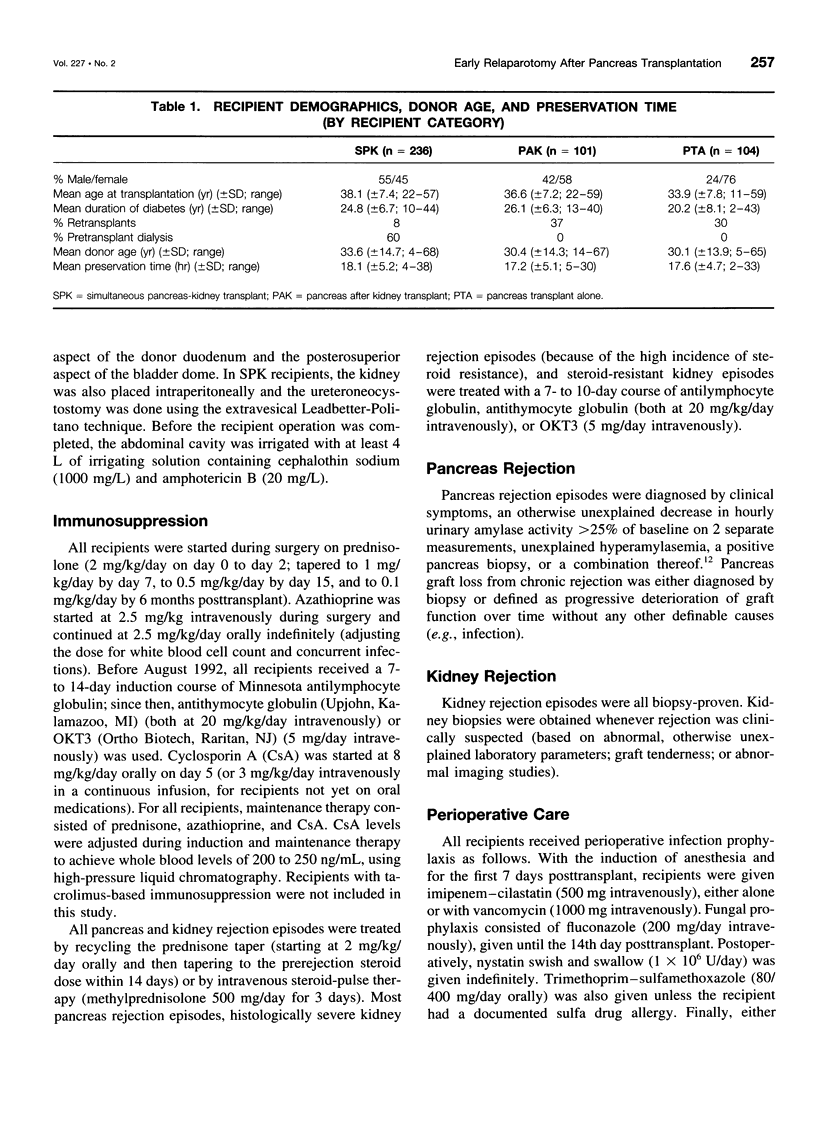
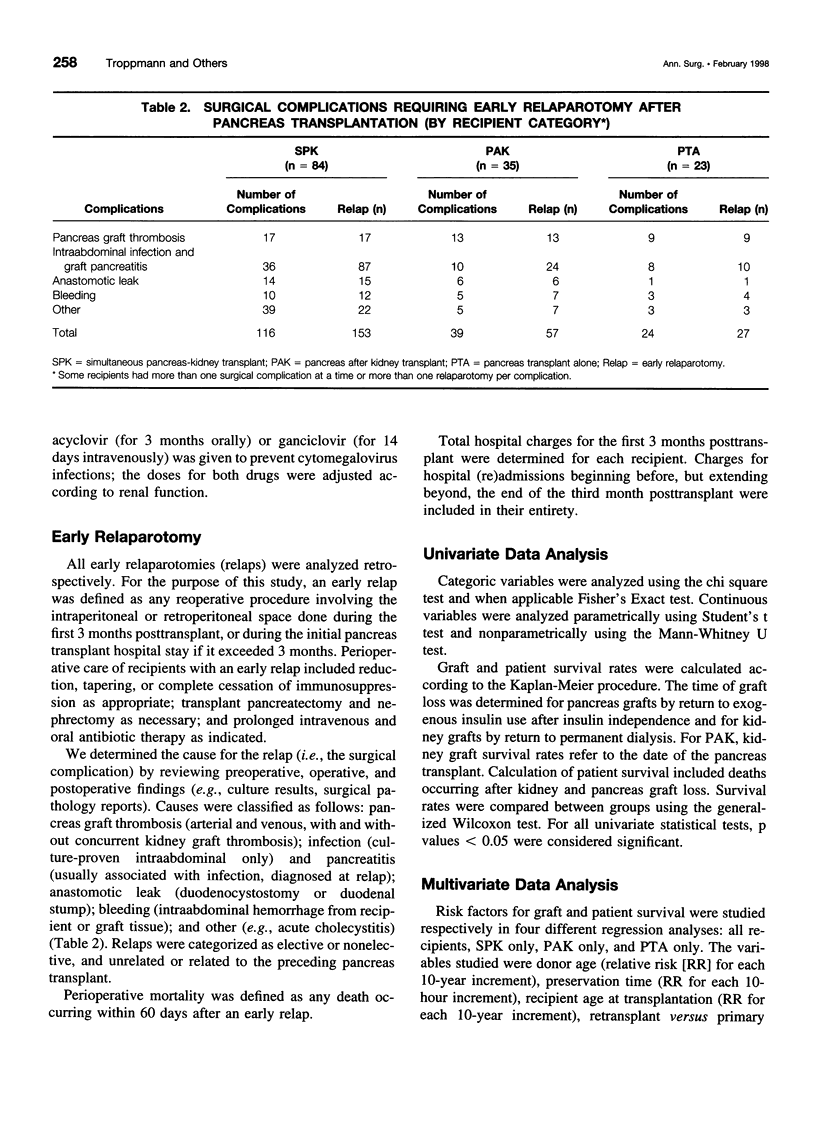
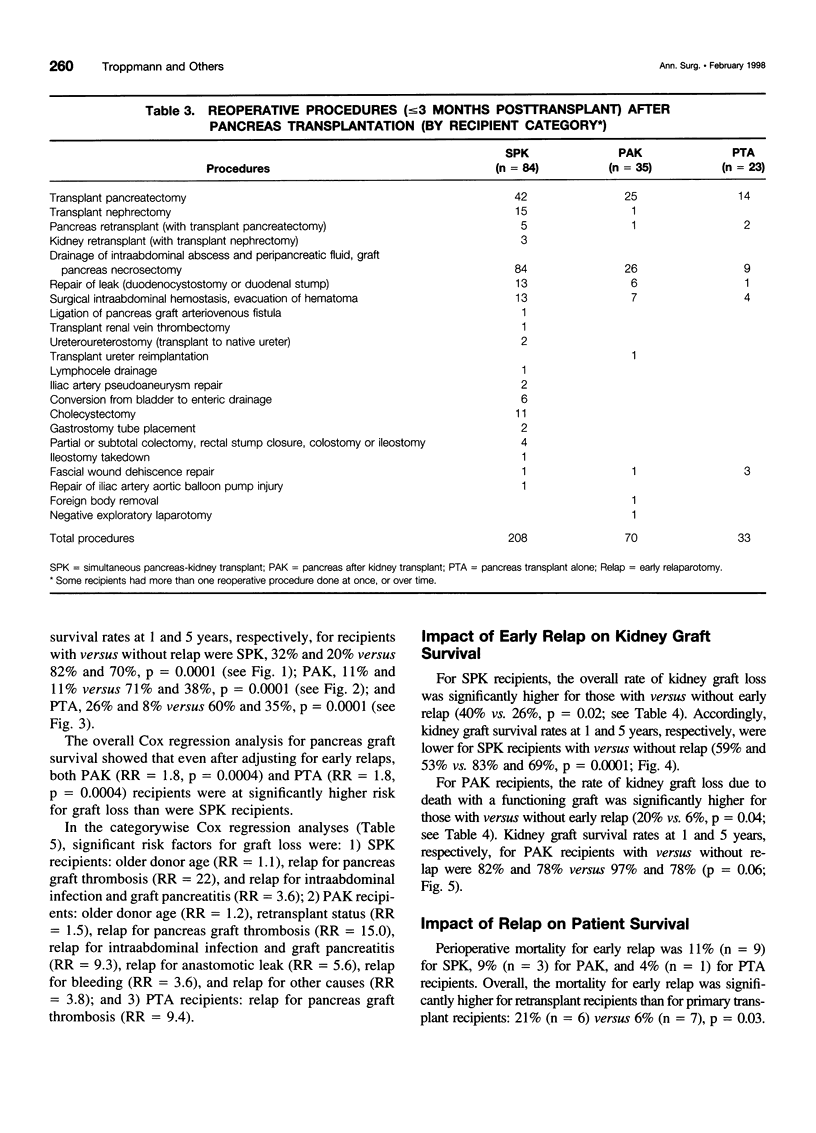
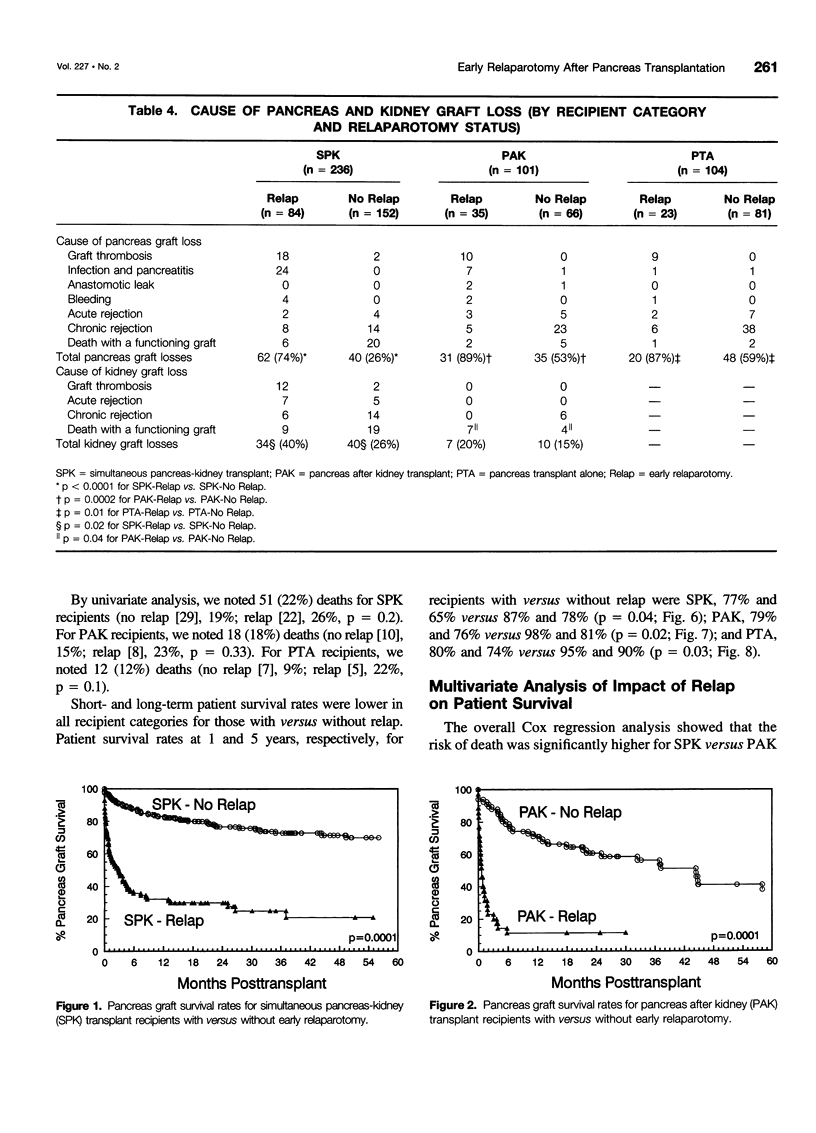
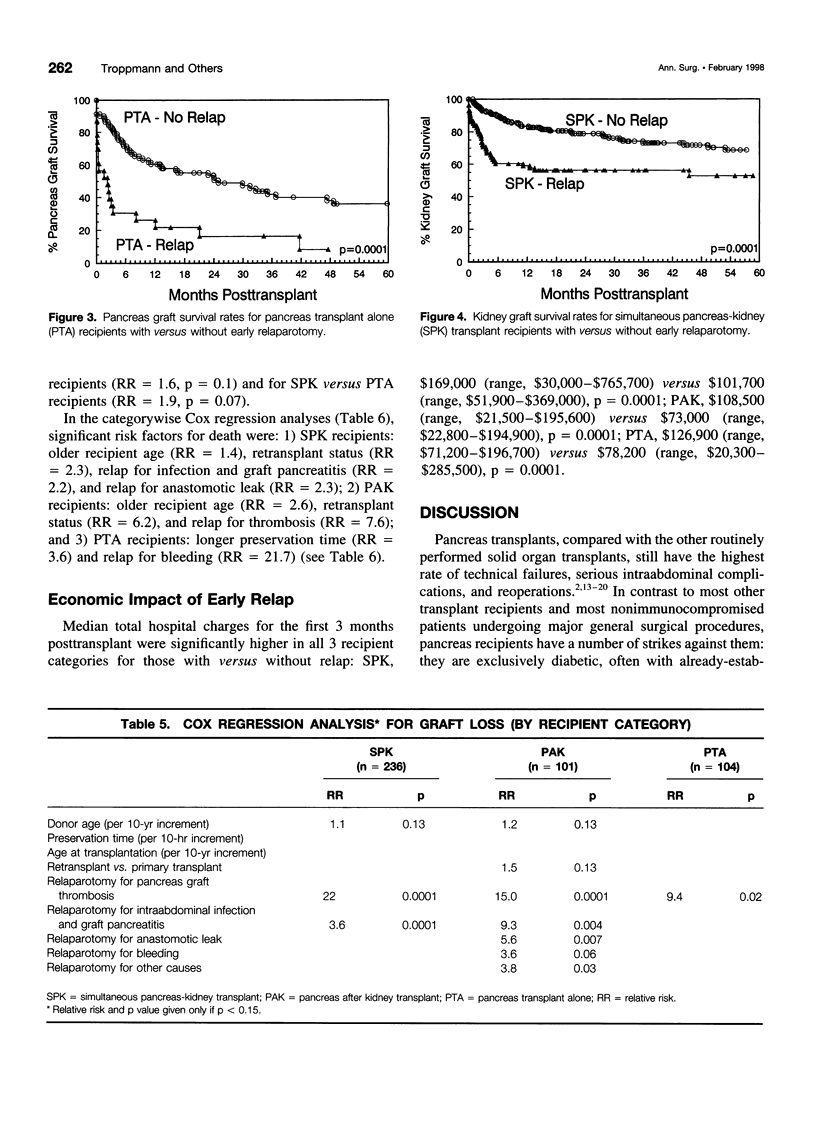
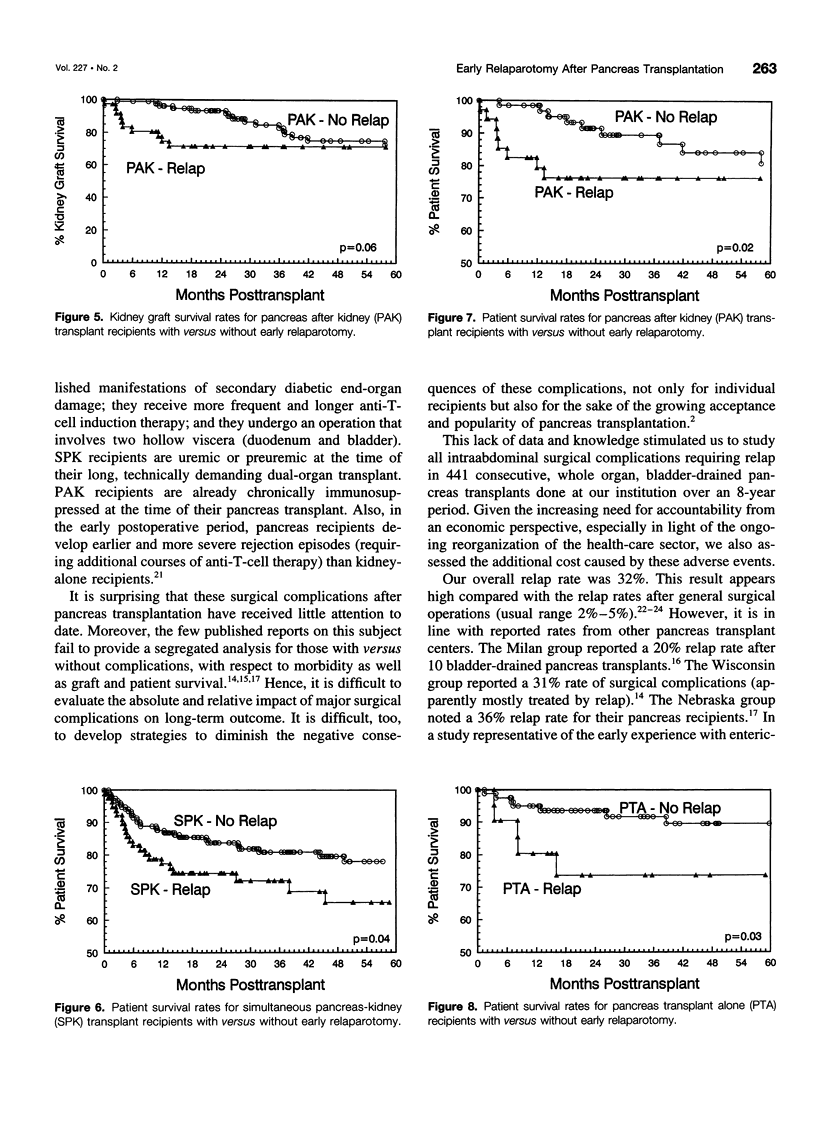
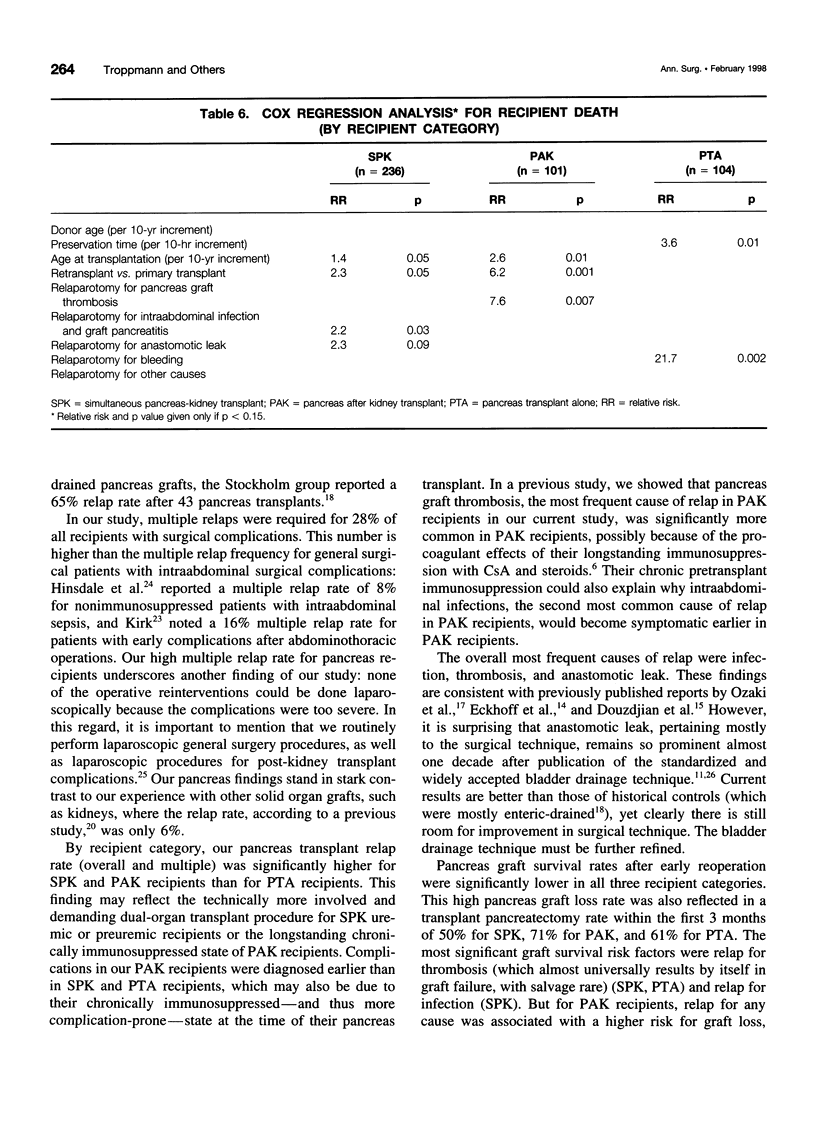
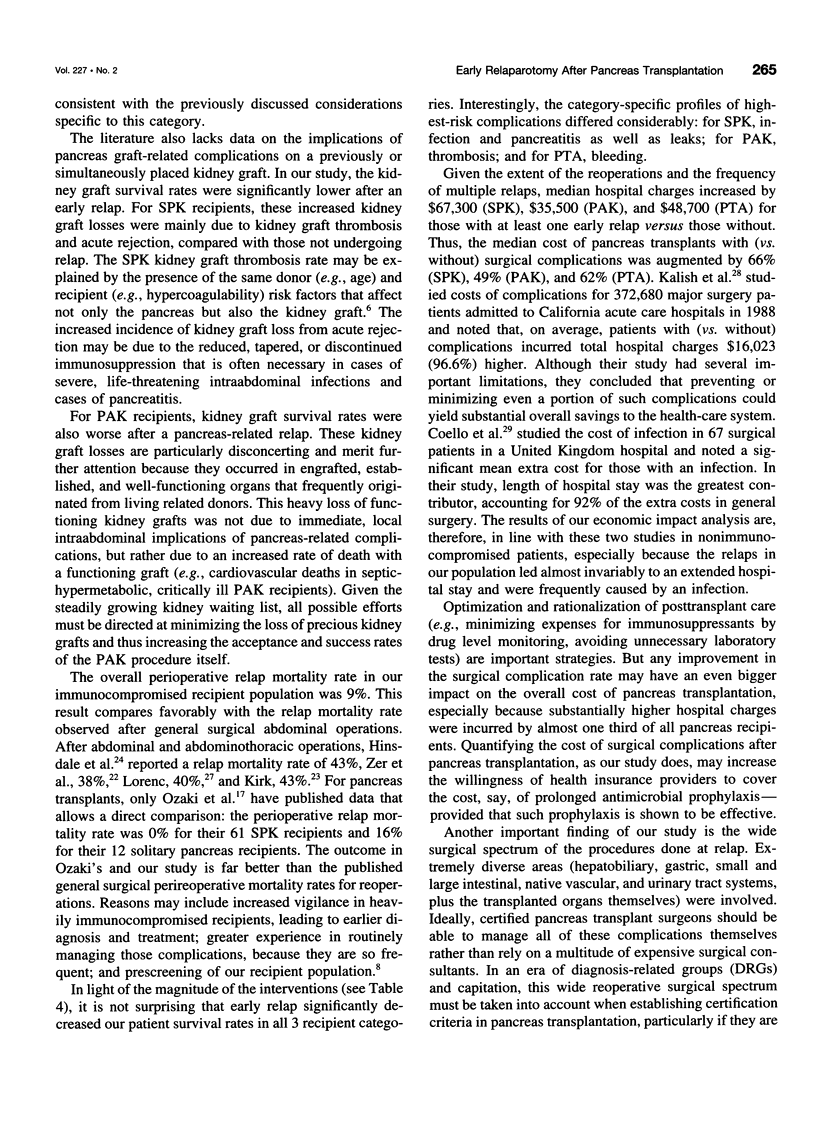
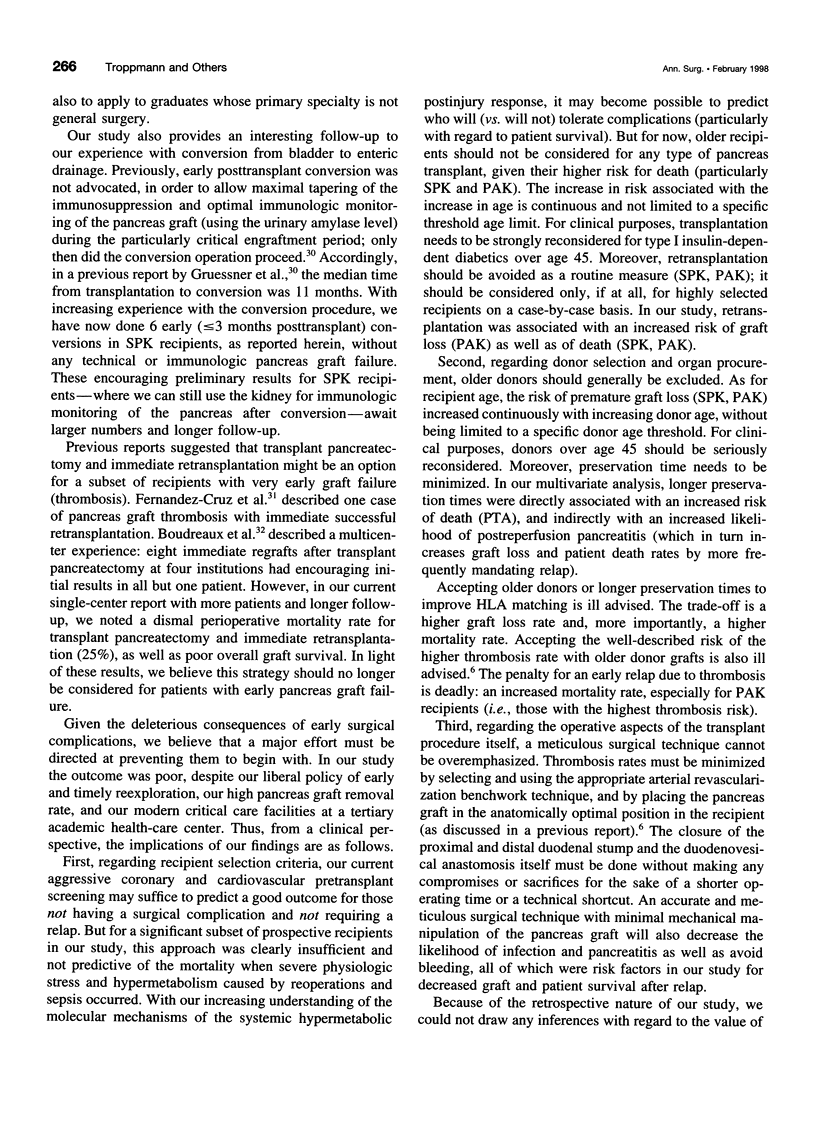
OBJECTIVES: To study significant surgical complications requiring early (< or = 3 months posttransplant) relaparotomy (relap) after pancreas transplants, and to develop clinically relevant surgical and peritransplant decision-making guidelines for preventing and managing such complications. SUMMARY BACKGROUND DATA: Pancreas grafts are still associated with the highest surgical complication rate of all routinely transplanted solid organs. However, the impact of surgical complications on morbidity, hospital costs, and graft and patient survival rates has not been analyzed in detail to date. METHODS: We retrospectively studied surgical complications requiring relap in 441 consecutive cadaver, bladder-drained pancreas transplants (54% simultaneous pancreas and kidney [SPK]; 22% pancreas after kidney [PAK]; 24% pancreas transplant alone [PTA]; 37% retransplant). Outcome and hospital charges were analyzed separately for recipients with versus without reoperation. RESULTS: The overall relap rate was 32% (SPK, 36%; PAK, 25%; PTA, 16%; p = 0.04). The most common causes were intraabdominal infection and graft pancreatitis (38%), pancreas graft thrombosis (27%), and anastomotic leak (15%). Perioperative relap mortality was 9%; transplant pancreatectomy was necessary in 57% of all recipients with one or more relaps. The pancreas graft was lost in 80% of recipients with versus 41% without relap (p < 0.0001). Patient survival rates were significantly lower (p < 0.05) for recipients with versus without relap. By multivariate analysis, significant risk factors for graft loss included older donor age (SPK, PAK), retransplant (PAK), relap for infection (SPK, PAK), and relap for leak or bleeding (PAK). For death, risk factors included older recipient age (SPK, PAK),retransplant (SPK, PAK), relap for thrombosis (PAK), relap for infection or leak (SPK), and relap for bleeding (PTA). CONCLUSIONS: Posttransplant surgical complications requiring relap were frequent, resulted in a high rate of pancreas (SPK, PAK, PTA) and kidney (SPK, PAK) graft loss, and had a major economic impact (p = 0.0001). Complications were associated with substantial perioperative mortality and decreased patient survival rates. The focus must therefore shift from graft salvage to preservation of the recipient's life once a pancreas graft-related complication requiring relap occurs. Thus, the threshold for pancreatectomy should be low. In this context, acceptance of older donors and recipients must be reconsidered.
Full text
PDF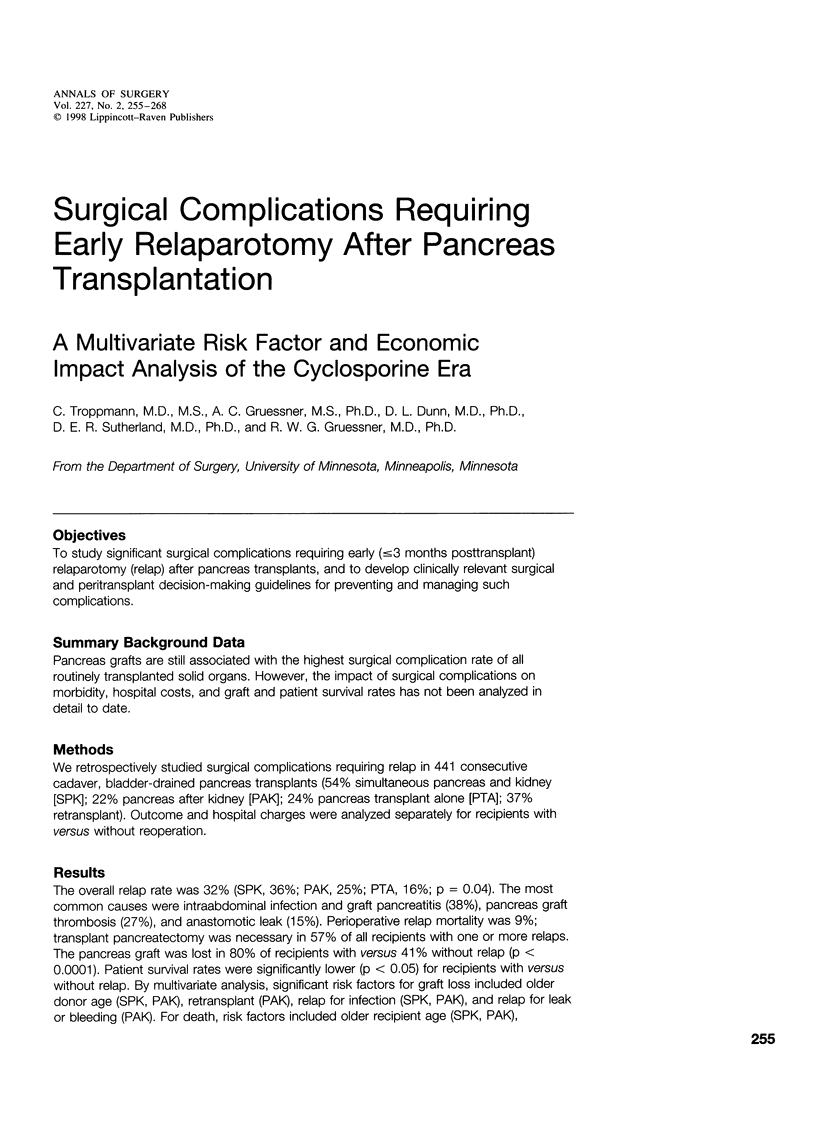
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Benedetti E., Gruessner A. C., Troppmann C., Papalois B. E., Sutherland D. E., Dunn D. L., Gruessner R. W. Intra-abdominal fungal infections after pancreatic transplantation: incidence, treatment, and outcome. J Am Coll Surg. 1996 Oct;183(4):307–316. [PubMed] [Google Scholar]
- Benedetti E., Najarian J. S., Gruessner A. C., Nakhleh R. E., Troppmann C., Hakim N. S., Pirenne J., Sutherland D. E., Gruessner R. W. Correlation between cystoscopic biopsy results and hypoamylasuria in bladder-drained pancreas transplants. Surgery. 1995 Nov;118(5):864–872. doi: 10.1016/s0039-6060(05)80277-6. [DOI] [PubMed] [Google Scholar]
- Boudreaux J. P., Corry R. J., Dickerman R., Sutherland D. E. Combined experience with immediate pancreas retransplantation. Transplant Proc. 1991 Feb;23(1 Pt 2):1628–1629. [PubMed] [Google Scholar]
- Castoldi R., Staudacher C., Ferrari G., Cristallo M., Carlucci M., La Rocca E., Secchi A., Pozza G., Di Carlo V. Early postoperative surgical complications: comparison of segmental duct-injected versus whole bladder-drained pancreas transplantation. Transplant Proc. 1992 Jun;24(3):817–820. [PubMed] [Google Scholar]
- Cheung A. H., Sutherland D. E., Gillingham K. J., McHugh L. E., Moudry-Munns K. C., Dunn D. L., Najarian J. S., Matas A. J. Simultaneous pancreas-kidney transplant versus kidney transplant alone in diabetic patients. Kidney Int. 1992 Apr;41(4):924–929. doi: 10.1038/ki.1992.141. [DOI] [PubMed] [Google Scholar]
- Coello R., Glenister H., Fereres J., Bartlett C., Leigh D., Sedgwick J., Cooke E. M. The cost of infection in surgical patients: a case-control study. J Hosp Infect. 1993 Dec;25(4):239–250. doi: 10.1016/0195-6701(93)90110-l. [DOI] [PubMed] [Google Scholar]
- Douzdjian V., Abecassis M. M., Cooper J. L., Smith J. L., Corry R. J. Incidence, management and significance of surgical complications after pancreatic transplantation. Surg Gynecol Obstet. 1993 Nov;177(5):451–456. [PubMed] [Google Scholar]
- Eckhoff D. E., Sollinger H. W. Surgical complications after simultaneous pancreas-kidney transplant with bladder drainage. Clin Transpl. 1993:185–191. [PubMed] [Google Scholar]
- Grewal H. P., Garland L., Novak K., Gaber L., Tolley E. A., Gaber A. O. Risk factors for postimplantation pancreatitis and pancreatic thrombosis in pancreas transplant recipients. Transplantation. 1993 Sep;56(3):609–612. doi: 10.1097/00007890-199309000-00021. [DOI] [PubMed] [Google Scholar]
- Gruessner R. W., Dunn D. L., Gruessner A. C., Matas A. J., Najarian J. S., Sutherland D. E. Recipient risk factors have an impact on technical failure and patient and graft survival rates in bladder-drained pancreas transplants. Transplantation. 1994 Jun 15;57(11):1598–1606. [PubMed] [Google Scholar]
- Gruessner R. W., Fasola C., Benedetti E., Foshager M. C., Gruessner A. C., Matas A. J., Najarian J. S., Goodale R. L. Laparoscopic drainage of lymphoceles after kidney transplantation: indications and limitations. Surgery. 1995 Mar;117(3):288–295. doi: 10.1016/s0039-6060(05)80204-1. [DOI] [PubMed] [Google Scholar]
- Gruessner R. W., Stephanian E., Dunn D. L., Gruessner A. C., Najarian J. S., Sutherland D. E. Cystoenteric conversion after whole pancreaticoduodenal transplantation: indications, risk factors, and outcome. Transplant Proc. 1993 Feb;25(1 Pt 2):1179–1181. [PubMed] [Google Scholar]
- Gruessner R. W. Tacrolimus in pancreas transplantation: a multicenter analysis. Tacrolimus Pancreas Transplant Study Group. Clin Transplant. 1997 Aug;11(4):299–312. [PubMed] [Google Scholar]
- Gruessner R. W., Troppmann C., Barrou B., Dunn D. L., Moudry-Munns K. C., Najarian J. S., Sutherland D. E., Gruessner A. C. Assessment of donor and recipient risk factors on pancreas transplant outcome. Transplant Proc. 1994 Apr;26(2):437–438. [PubMed] [Google Scholar]
- Hinsdale J. G., Jaffe B. M. Re-operation for intra-abdominal sepsis. Indications and results in modern critical care setting. Ann Surg. 1984 Jan;199(1):31–36. doi: 10.1097/00000658-198401000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalish R. L., Daley J., Duncan C. C., Davis R. B., Coffman G. A., Iezzoni L. I. Costs of potential complications of care for major surgery patients. Am J Med Qual. 1995 Spring;10(1):48–54. doi: 10.1177/0885713X9501000108. [DOI] [PubMed] [Google Scholar]
- Kirk R. M. Reoperative surgery for early complications following abdominal and abdominothoracic operations. J R Soc Med. 1988 Jan;81(1):7–9. doi: 10.1177/014107688808100105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamberts S. W., van der Lely A. J., de Herder W. W., Hofland L. J. Octreotide. N Engl J Med. 1996 Jan 25;334(4):246–254. doi: 10.1056/NEJM199601253340408. [DOI] [PubMed] [Google Scholar]
- Lorenc J. Early urgent relaparotomy in abdominal surgery. Int Surg. 1969 May;51(5):433–437. [PubMed] [Google Scholar]
- Manske C. L., Thomas W., Wang Y., Wilson R. F. Screening diabetic transplant candidates for coronary artery disease: identification of a low risk subgroup. Kidney Int. 1993 Sep;44(3):617–621. doi: 10.1038/ki.1993.289. [DOI] [PubMed] [Google Scholar]
- Manske C. L., Wang Y., Rector T., Wilson R. F., White C. W. Coronary revascularisation in insulin-dependent diabetic patients with chronic renal failure. Lancet. 1992 Oct 24;340(8826):998–1002. doi: 10.1016/0140-6736(92)93010-k. [DOI] [PubMed] [Google Scholar]
- Morel P., Goetz F. C., Moudry-Munns K., Freier E., Sutherland D. E. Long-term glucose control in patients with pancreatic transplants. Ann Intern Med. 1991 Nov 1;115(9):694–699. doi: 10.7326/0003-4819-115-9-694. [DOI] [PubMed] [Google Scholar]
- Nghiem D. D., Corry R. J. Technique of simultaneous renal pancreatoduodenal transplantation with urinary drainage of pancreatic secretion. Am J Surg. 1987 Apr;153(4):405–406. doi: 10.1016/0002-9610(87)90588-5. [DOI] [PubMed] [Google Scholar]
- Nicholson C. P., Barr D., Oeltjen M. R., Munn S. R., DiMagno E. P., Carpenter H. A., Sarr M. G., Perkins J. D. The effect of somatostatin 201-995 on the early course of porcine pancreaticoduodenal allotransplantation. Transplantation. 1991 Jan;51(1):31–36. doi: 10.1097/00007890-199101000-00004. [DOI] [PubMed] [Google Scholar]
- Ozaki C. F., Stratta R. J., Taylor R. J., Langnas A. N., Bynon J. S., Shaw B. W., Jr Surgical complications in solitary pancreas and combined pancreas-kidney transplantations. Am J Surg. 1992 Nov;164(5):546–551. doi: 10.1016/s0002-9610(05)81198-5. [DOI] [PubMed] [Google Scholar]
- Pescovitz M. D., Dunn D. L., Sutherland D. E. Use of the circular stapler in construction of the duodenoneocystostomy for drainage into the bladder in transplants involving the whole pancreas. Surg Gynecol Obstet. 1989 Aug;169(2):169–171. [PubMed] [Google Scholar]
- Reichlin S. Neuroendocrine-immune interactions. N Engl J Med. 1993 Oct 21;329(17):1246–1253. doi: 10.1056/NEJM199310213291708. [DOI] [PubMed] [Google Scholar]
- Stratta R. J., Taylor R. J., Lowell J. A., Bynon J. S., Cattral M. S., Frisbie K., Brennan D. C. Randomized trial of Sandostatin prophylaxis for preservation injury after pancreas transplantation. Transplant Proc. 1993 Dec;25(6):3190–3192. [PubMed] [Google Scholar]
- Stratta R. J., Taylor R. J., Ozaki C. F., Bynon J. S., Miller S. A., Knight T. F., Fischer J. L., Neumann T. V., Wahl T. O., Duckworth W. C. A comparative analysis of results and morbidity in type I diabetics undergoing preemptive versus postdialysis combined pancreas-kidney transplantation. Transplantation. 1993 May;55(5):1097–1103. doi: 10.1097/00007890-199305000-00031. [DOI] [PubMed] [Google Scholar]
- Tibell A., Tydén G., Brattström C., Mainetti L., Groth C. G. Surgical complications after segmental pancreatic transplantation with enteric exocrine diversion. Transplant Proc. 1989 Feb;21(1 Pt 3):2801–2802. [PubMed] [Google Scholar]
- Troppmann C., Gruessner A. C., Benedetti E., Papalois B. E., Dunn D. L., Najarian J. S., Sutherland D. E., Gruessner R. W. Vascular graft thrombosis after pancreatic transplantation: univariate and multivariate operative and nonoperative risk factor analysis. J Am Coll Surg. 1996 Apr;182(4):285–316. [PubMed] [Google Scholar]
- Troppmann C., Gruessner A. C., Benedetti E., Papalois B. E., Sutherland D. E., Gruessner R. W. Positive duodenal segment cultures are not associated with increased surgical complications after whole organ, bladder-drained pancreas transplantation in three recipient categories. Transplant Proc. 1995 Dec;27(6):3101–3103. [PubMed] [Google Scholar]
- Troppmann C., Gruessner A. C., Papalois B. E., Sutherland D. E., Matas A. J., Benedetti E., Gruessner R. W. Delayed endocrine pancreas graft function after simultaneous pancreas-kidney transplantation. Incidence, risk factors, and impact on long-term outcome. Transplantation. 1996 May 15;61(9):1323–1330. doi: 10.1097/00007890-199605150-00007. [DOI] [PubMed] [Google Scholar]


