Abstract
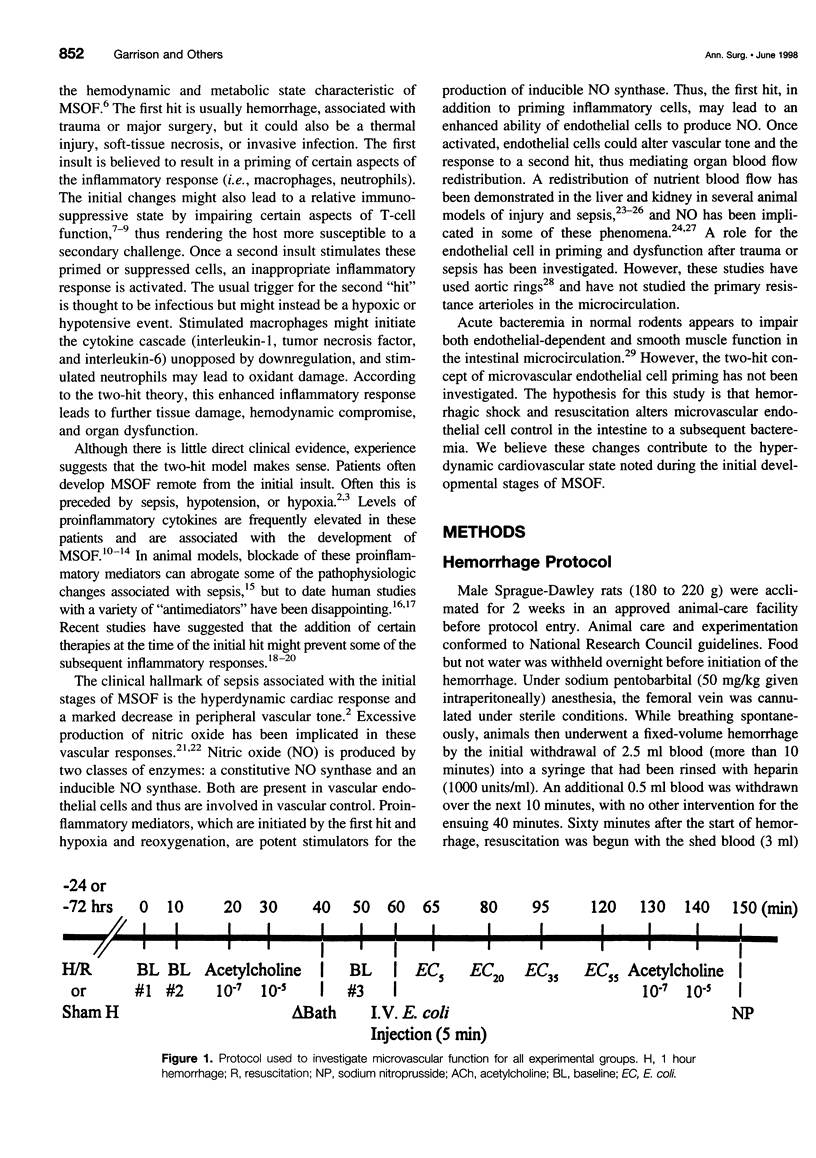
OBJECTIVE: The objective was to determine intestinal microvascular endothelial cell control after sequential hemorrhage and bacteremia. SUMMARY BACKGROUND DATA: Sepsis that follows severe hemorrhagic shock often results in multiple system organ failure (MSOF) and death. The sequential nature of this clinical scenario has led to the idea of a "two-hit" theory for the development of MSOF, the hallmark of which is peripheral vasodilation and acidosis. Acute bacteremia alone results in persistent intestinal vasoconstriction and mucosal hypoperfusion. Little experimental data exist to support the pathogenesis of vascular dysregulation during sequential physiologic insults. We postulate that hemorrhagic shock followed by bacteremia results in altered microvascular endothelial cell control of dilation and blood flow. METHODS: Rats underwent volume hemorrhage and resuscitation. A sham group underwent the vascular cannulation without hemorrhage and resuscitation, and controls had no surgical manipulation. After 24 and 72 hours, the small intestine microcirculation was visualized by in vivo videomicroscopy. Mean arterial pressure, heart rate, arteriolar diameters, and A1 flow by Doppler velocimetry were measured. Endothelial-dependent dilator function was determined by the topical application of acetylcholine (ACh). After 1 hour of Escherichia coil bacteremia, ACh dose responses were again measured. Topical nitroprusside was then applied to assess direct smooth muscle dilation (endothelial-independent dilator function) in all groups. Vascular reactivity to ACh was compared among the groups. RESULTS: Acute bacteremia, with or without prior hemorrhage, caused significant large-caliber A1 arteriolar constriction with a concomitant decrease in blood flow. This constriction was blunted at 24 hours after hemorrhage but was restored to control values by 72 hours. There was a reversal of the response to bacteremia in the premucosal A3 vessels, with a marked dilation both at 24 and 72 hours. The sequence of hemorrhage and E. coli resulted in a progressive enhanced reactivity to the endothelial-dependent stimulus of ACh in the A3 vessels at 24 and 72 hours. Reactivity to endothelial-independent smooth muscle relaxation and subsequent vessel dilation was similar for all groups. CONCLUSIONS: These data indicate that there is altered endothelial control of the intestinal microvasculature after hemorrhage in favor of enhanced dilator mechanisms in premucosal vessels with enhanced constrictor forces in inflow vessels. This enhanced dilator sensitivity is most evident in small premucosal vessels. This experimental finding supports the premise that an initial pathophysiologic stress alters the subsequent microvascular blood flow responses to systemic inflammation. These changes in the intestinal microcirculation are in concert with the "two-hit" theory for MSOF.
Full text
PDF







Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson B. O., Harken A. H. Multiple organ failure: inflammatory priming and activation sequences promote autologous tissue injury. J Trauma. 1990 Dec;30(12 Suppl):S44–S49. [PubMed] [Google Scholar]
- Baue A. E. Multiple, progressive, or sequential systems failure. A syndrome of the 1970s. Arch Surg. 1975 Jul;110(7):779–781. doi: 10.1001/archsurg.1975.01360130011001. [DOI] [PubMed] [Google Scholar]
- Bohlen H. G., Gore R. W. Preparation of rat intestinal muscle and mucosa for quantitative microcirculatory studies. Microvasc Res. 1976 Jan;11(1):103–110. doi: 10.1016/0026-2862(76)90081-9. [DOI] [PubMed] [Google Scholar]
- Botha A. J., Moore F. A., Moore E. E., Sauaia A., Banerjee A., Peterson V. M. Early neutrophil sequestration after injury: a pathogenic mechanism for multiple organ failure. J Trauma. 1995 Sep;39(3):411–417. doi: 10.1097/00005373-199509000-00003. [DOI] [PubMed] [Google Scholar]
- Carrico C. J., Meakins J. L., Marshall J. C., Fry D., Maier R. V. Multiple-organ-failure syndrome. Arch Surg. 1986 Feb;121(2):196–208. doi: 10.1001/archsurg.1986.01400020082010. [DOI] [PubMed] [Google Scholar]
- Chaudry I. H., Ayala A., Ertel W., Stephan R. N. Hemorrhage and resuscitation: immunological aspects. Am J Physiol. 1990 Oct;259(4 Pt 2):R663–R678. doi: 10.1152/ajpregu.1990.259.4.R663. [DOI] [PubMed] [Google Scholar]
- Coimbra R., Hoyt D. B., Junger W. G., Angle N., Wolf P., Loomis W., Evers M. F. Hypertonic saline resuscitation decreases susceptibility to sepsis after hemorrhagic shock. J Trauma. 1997 Apr;42(4):602–607. doi: 10.1097/00005373-199704000-00004. [DOI] [PubMed] [Google Scholar]
- Deitch E. A. Multiple organ failure. Pathophysiology and potential future therapy. Ann Surg. 1992 Aug;216(2):117–134. doi: 10.1097/00000658-199208000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douzinas E. E., Tsidemiadou P. D., Pitaridis M. T., Andrianakis I., Bobota-Chloraki A., Katsouyanni K., Sfyras D., Malagari K., Roussos C. The regional production of cytokines and lactate in sepsis-related multiple organ failure. Am J Respir Crit Care Med. 1997 Jan;155(1):53–59. doi: 10.1164/ajrccm.155.1.9001289. [DOI] [PubMed] [Google Scholar]
- Fisher C. J., Jr, Opal S. M., Dhainaut J. F., Stephens S., Zimmerman J. L., Nightingale P., Harris S. J., Schein R. M., Panacek E. A., Vincent J. L. Influence of an anti-tumor necrosis factor monoclonal antibody on cytokine levels in patients with sepsis. The CB0006 Sepsis Syndrome Study Group. Crit Care Med. 1993 Mar;21(3):318–327. doi: 10.1097/00003246-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Flynn W. J., Cryer H. G., Garrison R. N. Pentoxifylline restores intestinal microvascular blood flow during resuscitated hemorrhagic shock. Surgery. 1991 Aug;110(2):350–356. [PubMed] [Google Scholar]
- Flynn W. J., Cryer H. G., Garrison R. N. Pentoxifylline restores intestinal microvascular blood flow during resuscitated hemorrhagic shock. Surgery. 1991 Aug;110(2):350–356. [PubMed] [Google Scholar]
- Garrison R. N., Ratcliffe D. J., Fry D. E. Hepatocellular function and nutrient blood flow in experimental peritonitis. Surgery. 1982 Oct;92(4):713–719. [PubMed] [Google Scholar]
- Garrison R. N., Wilson M. A., Matheson P. J., Spain D. A. Nitric oxide mediates redistribution of intrarenal blood flow during bacteremia. J Trauma. 1995 Jul;39(1):90–97. doi: 10.1097/00005373-199507000-00012. [DOI] [PubMed] [Google Scholar]
- Gavin T. J., Fabian T. C., Wilson J. D., Trenthem L. L., Pritchard F. E., Croce M. A., Stewart R. M., Proctor K. G. Splanchnic and systemic hemodynamic responses to portal vein endotoxin after resuscitation from hemorrhagic shock. Surgery. 1994 Mar;115(3):310–324. [PubMed] [Google Scholar]
- Goris R. J., te Boekhorst T. P., Nuytinck J. K., Gimbrère J. S. Multiple-organ failure. Generalized autodestructive inflammation? Arch Surg. 1985 Oct;120(10):1109–1115. doi: 10.1001/archsurg.1985.01390340007001. [DOI] [PubMed] [Google Scholar]
- Gosche J. R., Spain D. A., Garrison R. N., Lübbe A. S., Cryer H. G. Differential microvascular response to cyclooxygenase blockade in the rat small intestine during acute bacteremia. Shock. 1994 Dec;2(6):408–412. doi: 10.1097/00024382-199412000-00004. [DOI] [PubMed] [Google Scholar]
- Isoyama T., Sato T., Tanaka J., Shatney C. H. Measurement of cardiac output in small animals by aortic thermodilution. J Surg Res. 1982 Aug;33(2):170–176. doi: 10.1016/0022-4804(82)90025-7. [DOI] [PubMed] [Google Scholar]
- Livingston D. H., Malangoni M. A. An experimental study of susceptibility to infection after hemorrhagic shock. Surg Gynecol Obstet. 1989 Feb;168(2):138–142. [PubMed] [Google Scholar]
- Livingston D. H., Mosenthal A. C., Deitch E. A. Sepsis and multiple organ dysfunction syndrome: a clinical-mechanistic overview. New Horiz. 1995 May;3(2):257–266. [PubMed] [Google Scholar]
- Lübbe A. S., Garrison R. N., Cryer H. M., Alsip N. L., Harris P. D. EDRF as a possible mediator of sepsis-induced arteriolar dilation in skeletal muscle. Am J Physiol. 1992 Mar;262(3 Pt 2):H880–H887. doi: 10.1152/ajpheart.1992.262.3.H880. [DOI] [PubMed] [Google Scholar]
- Lübbe A. S., Garrison R. N., Harris P. D., Cryer H. M. Hypertension alters microvascular responses in skeletal muscle to hyperdynamic bacteremia and hypodynamic Escherichia coli sepsis. J Surg Res. 1989 Feb;46(2):108–117. doi: 10.1016/0022-4804(89)90212-6. [DOI] [PubMed] [Google Scholar]
- Marano M. A., Fong Y., Moldawer L. L., Wei H., Calvano S. E., Tracey K. J., Barie P. S., Manogue K., Cerami A., Shires G. T. Serum cachectin/tumor necrosis factor in critically ill patients with burns correlates with infection and mortality. Surg Gynecol Obstet. 1990 Jan;170(1):32–38. [PubMed] [Google Scholar]
- Martin C., Saux P., Mege J. L., Perrin G., Papazian L., Gouin F. Prognostic values of serum cytokines in septic shock. Intensive Care Med. 1994;20(4):272–277. doi: 10.1007/BF01708964. [DOI] [PubMed] [Google Scholar]
- Matheson P. J., Wilson M. A., Spain D. A., Harris P. D., Anderson G. L., Garrison R. N. Glucose-induced intestinal hyperemia is mediated by nitric oxide. J Surg Res. 1997 Oct;72(2):146–154. doi: 10.1006/jsre.1997.5176. [DOI] [PubMed] [Google Scholar]
- Meldrum D. R., Ayala A., Perrin M. M., Ertel W., Chaudry I. H. Diltiazem restores IL-2, IL-3, IL-6, and IFN-gamma synthesis and decreases host susceptibility to sepsis following hemorrhage. J Surg Res. 1991 Aug;51(2):158–164. doi: 10.1016/0022-4804(91)90088-4. [DOI] [PubMed] [Google Scholar]
- Moore F. A., Sauaia A., Moore E. E., Haenel J. B., Burch J. M., Lezotte D. C. Postinjury multiple organ failure: a bimodal phenomenon. J Trauma. 1996 Apr;40(4):501–512. doi: 10.1097/00005373-199604000-00001. [DOI] [PubMed] [Google Scholar]
- Pinsky M. R., Vincent J. L., Deviere J., Alegre M., Kahn R. J., Dupont E. Serum cytokine levels in human septic shock. Relation to multiple-system organ failure and mortality. Chest. 1993 Feb;103(2):565–575. doi: 10.1378/chest.103.2.565. [DOI] [PubMed] [Google Scholar]
- Polk H. C., Jr, George C. D., Wellhausen S. R., Cost K., Davidson P. R., Regan M. P., Borzotta A. P. A systematic study of host defense processes in badly injured patients. Ann Surg. 1986 Sep;204(3):282–299. [PMC free article] [PubMed] [Google Scholar]
- Roumen R. M., Hendriks T., van der Ven-Jongekrijg J., Nieuwenhuijzen G. A., Sauerwein R. W., van der Meer J. W., Goris R. J. Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult respiratory distress syndrome and multiple organ failure. Ann Surg. 1993 Dec;218(6):769–776. doi: 10.1097/00000658-199312000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schirmer W. J., Schirmer J. M., Naff G. B., Fry D. E. Complement activation in peritonitis. Association with hepatic and renal perfusion abnormalities. First place winner: Conrad Jobst award. Am Surg. 1987 Dec;53(12):683–687. [PubMed] [Google Scholar]
- Spain D. A., Wilson M. A., Bar-Natan M. F., Garrison R. N. Role of nitric oxide in the small intestinal microcirculation during bacteremia. Shock. 1994 Jul;2(1):41–46. doi: 10.1097/00024382-199407000-00009. [DOI] [PubMed] [Google Scholar]
- Spain D. A., Wilson M. A., Bloom I. T., Garrison R. N. Renal microvascular responses to sepsis are dependent on nitric oxide. J Surg Res. 1994 Jun;56(6):524–529. doi: 10.1006/jsre.1994.1084. [DOI] [PubMed] [Google Scholar]
- Spain D. A., Wilson M. A., Krysztopik R. J., Matheson P. J., Garrison R. N. Differential intestinal microvascular dysfunction occurs during bacteremia. J Surg Res. 1997 Jan;67(1):67–71. doi: 10.1006/jsre.1996.4947. [DOI] [PubMed] [Google Scholar]
- Steeb G. D., Wilson M. A., Garrison R. N. Pentoxifylline preserves small-intestine microvascular blood flow during bacteremia. Surgery. 1992 Oct;112(4):756–764. [PubMed] [Google Scholar]
- Stephan R. N., Kupper T. S., Geha A. S., Baue A. E., Chaudry I. H. Hemorrhage without tissue trauma produces immunosuppression and enhances susceptibility to sepsis. Arch Surg. 1987 Jan;122(1):62–68. doi: 10.1001/archsurg.1987.01400130068010. [DOI] [PubMed] [Google Scholar]
- Theuer C. J., Wilson M. A., Spain D. A., Edwards M. J., Garrison R. N. Alpha-adrenergic receptor antagonism prevents intestinal vasoconstriction but not hypoperfusion following resuscitated hemorrhage. J Surg Res. 1995 Aug;59(2):292–298. doi: 10.1006/jsre.1995.1167. [DOI] [PubMed] [Google Scholar]
- Tracey K. J., Fong Y., Hesse D. G., Manogue K. R., Lee A. T., Kuo G. C., Lowry S. F., Cerami A. Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987 Dec 17;330(6149):662–664. doi: 10.1038/330662a0. [DOI] [PubMed] [Google Scholar]
- Wang P., Ba Z. F., Chaudry I. H. Endothelium-dependent relaxation is depressed at the macro- and microcirculatory levels during sepsis. Am J Physiol. 1995 Nov;269(5 Pt 2):R988–R994. doi: 10.1152/ajpregu.1995.269.5.R988. [DOI] [PubMed] [Google Scholar]
- Wang P., Ba Z. F., Zhou M., Tait S. M., Chaudry I. H. Pentoxifylline restores cardiac output and tissue perfusion after trauma-hemorrhage and decreases susceptibility to sepsis. Surgery. 1993 Aug;114(2):352–359. [PubMed] [Google Scholar]
- Wang X., Andersson R. The role of endothelial cells in the systemic inflammatory response syndrome and multiple system organ failure. Eur J Surg. 1995 Oct;161(10):703–713. [PubMed] [Google Scholar]
- Whitworth P. W., Cryer H. M., Garrison R. N., Baumgarten T. E., Harris P. D. Hypoperfusion of the intestinal microcirculation without decreased cardiac output during live Escherichia coli sepsis in rats. Circ Shock. 1989 Feb;27(2):111–122. [PubMed] [Google Scholar]
- Wickel D. J., Cheadle W. G., Mercer-Jones M. A., Garrison R. N. Poor outcome from peritonitis is caused by disease acuity and organ failure, not recurrent peritoneal infection. Ann Surg. 1997 Jun;225(6):744–756. doi: 10.1097/00000658-199706000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zervos E. E., Norman J. G., Denham D. W., Carey L. C., Livingston D., Rosemurgy A. S. Cytokine activation through sublethal hemorrhage is protective against early lethal endotoxic challenge. Arch Surg. 1997 Nov;132(11):1216–1221. doi: 10.1001/archsurg.1997.01430350066011. [DOI] [PubMed] [Google Scholar]
- Ziegler E. J., Fisher C. J., Jr, Sprung C. L., Straube R. C., Sadoff J. C., Foulke G. E., Wortel C. H., Fink M. P., Dellinger R. P., Teng N. N. Treatment of gram-negative bacteremia and septic shock with HA-1A human monoclonal antibody against endotoxin. A randomized, double-blind, placebo-controlled trial. The HA-1A Sepsis Study Group. N Engl J Med. 1991 Feb 14;324(7):429–436. doi: 10.1056/NEJM199102143240701. [DOI] [PubMed] [Google Scholar]


