Abstract
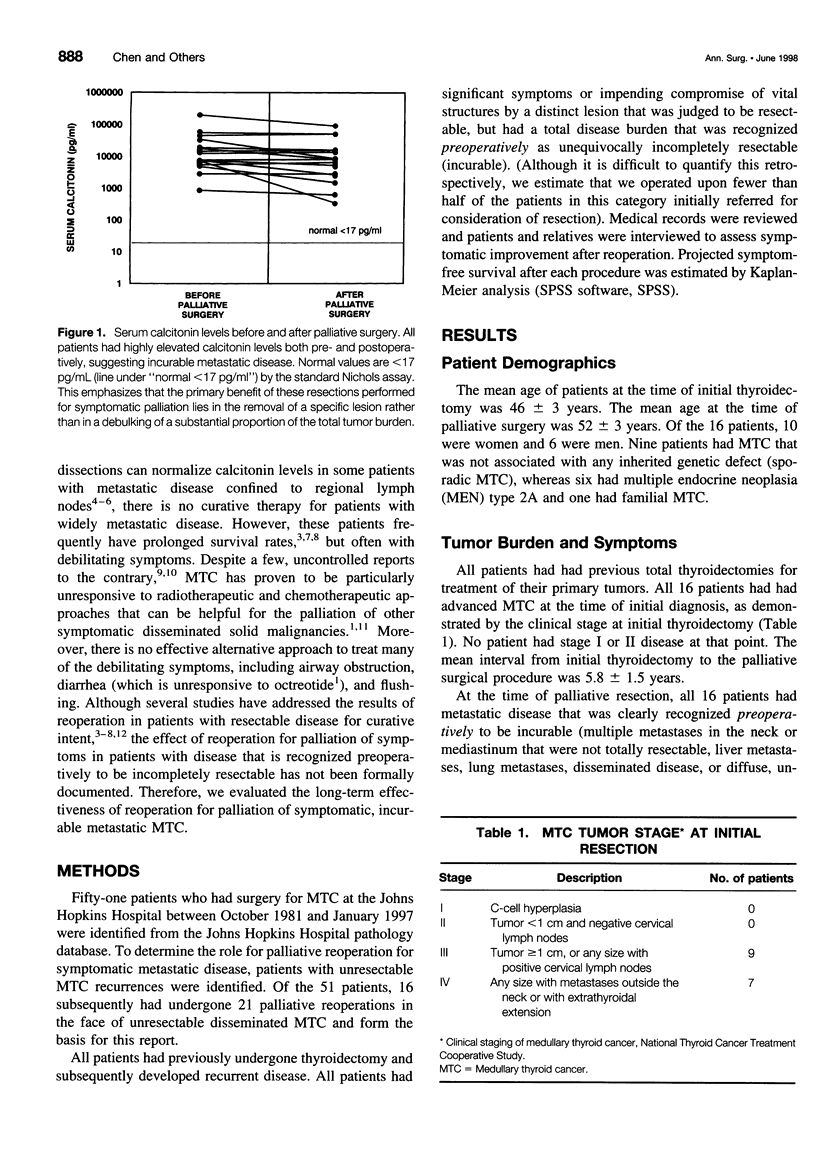
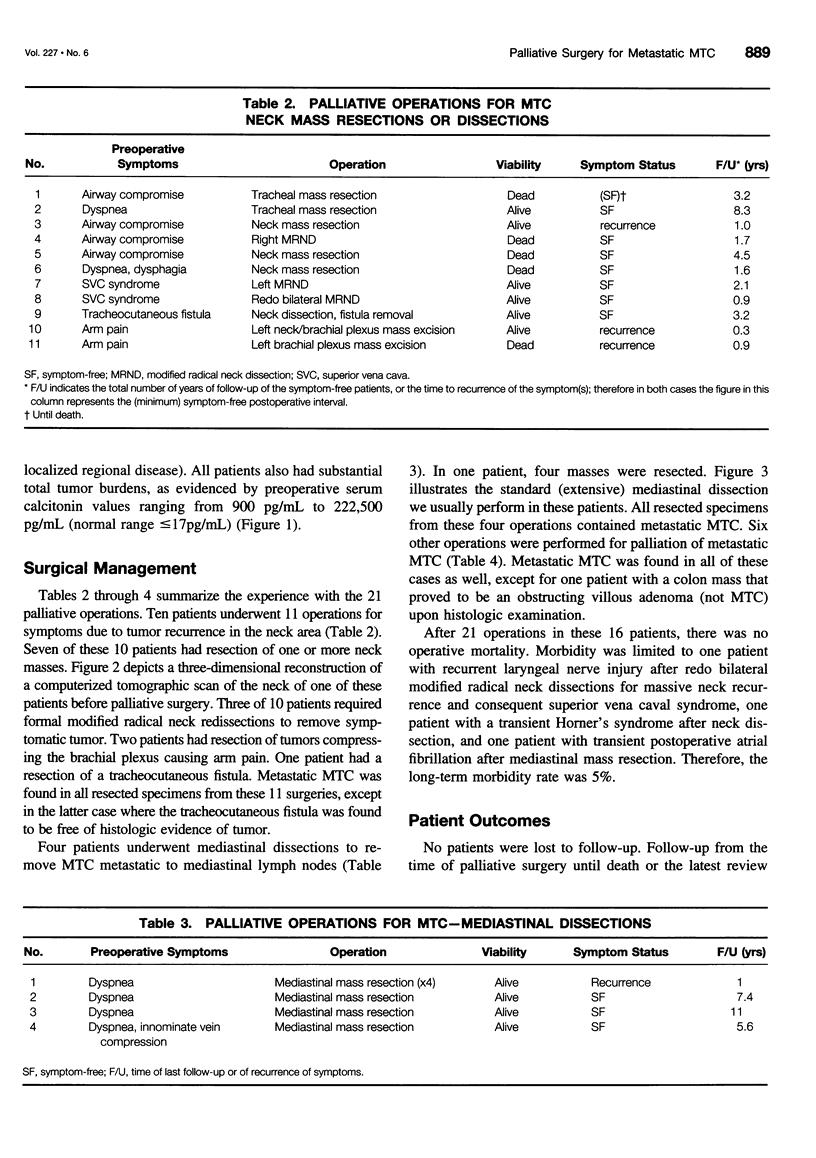
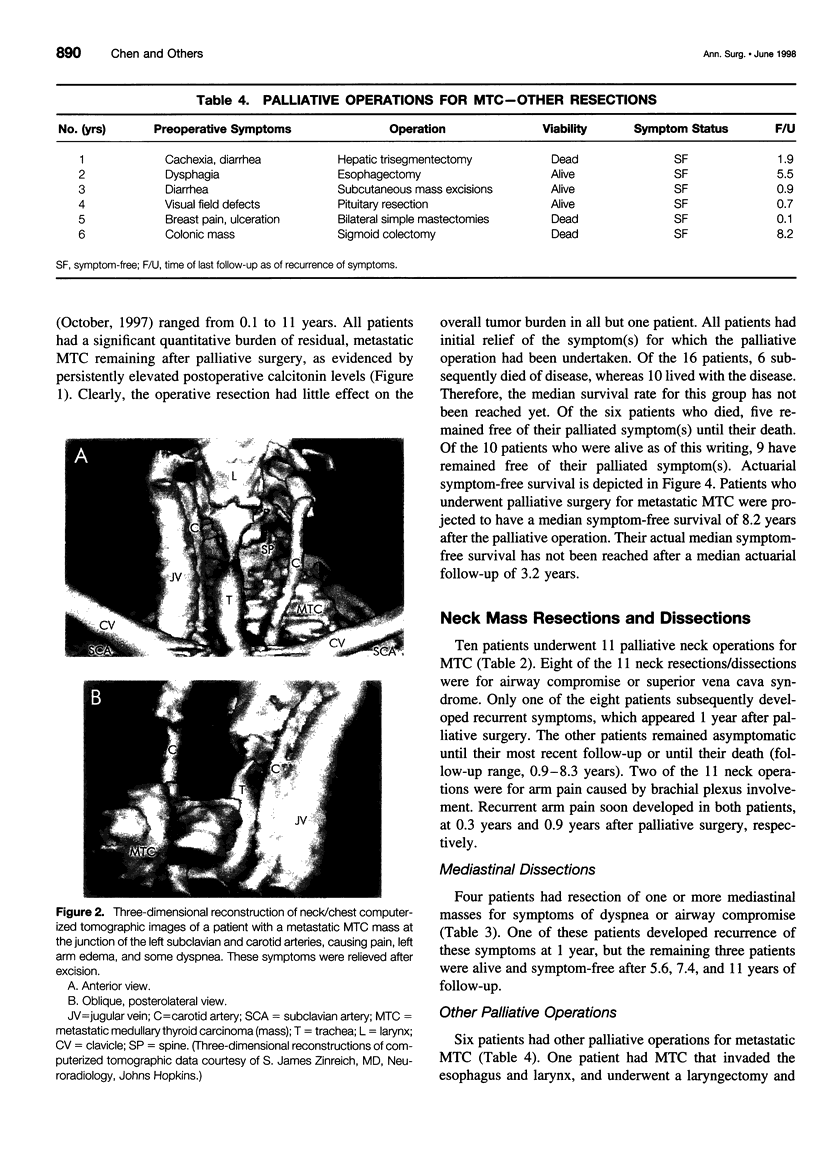
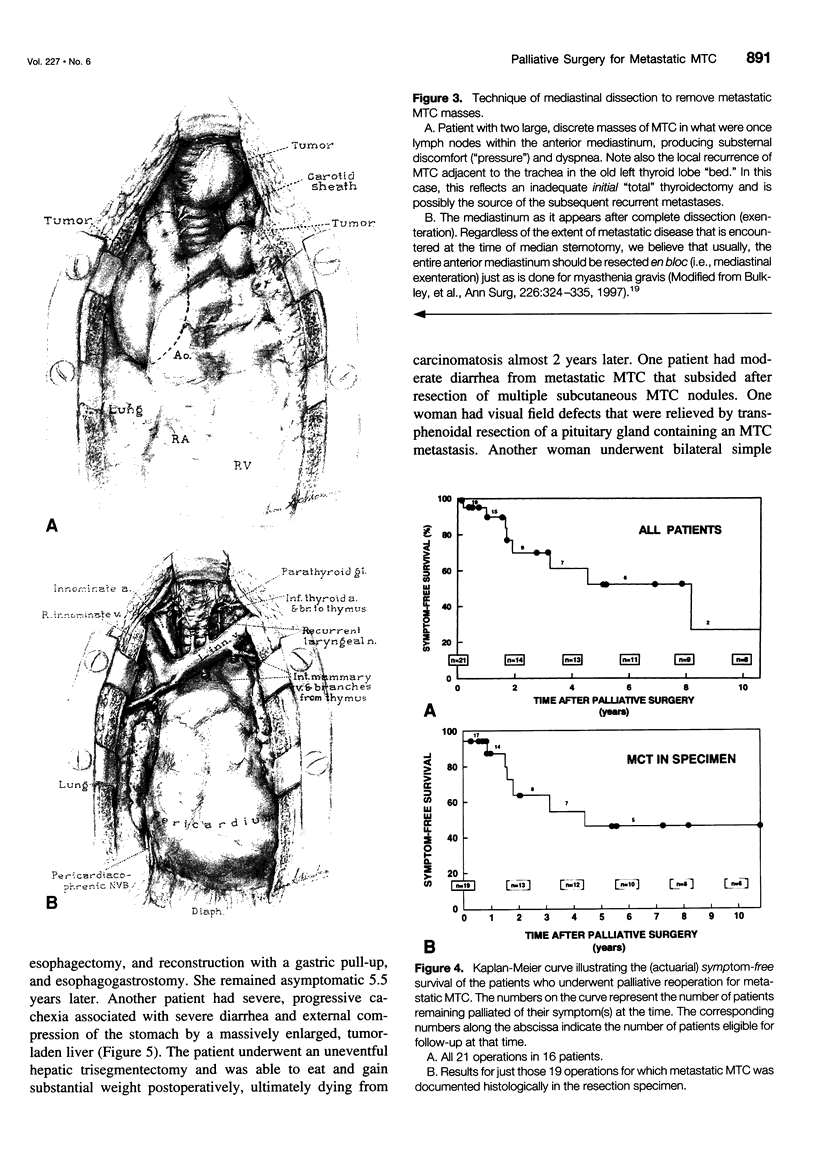
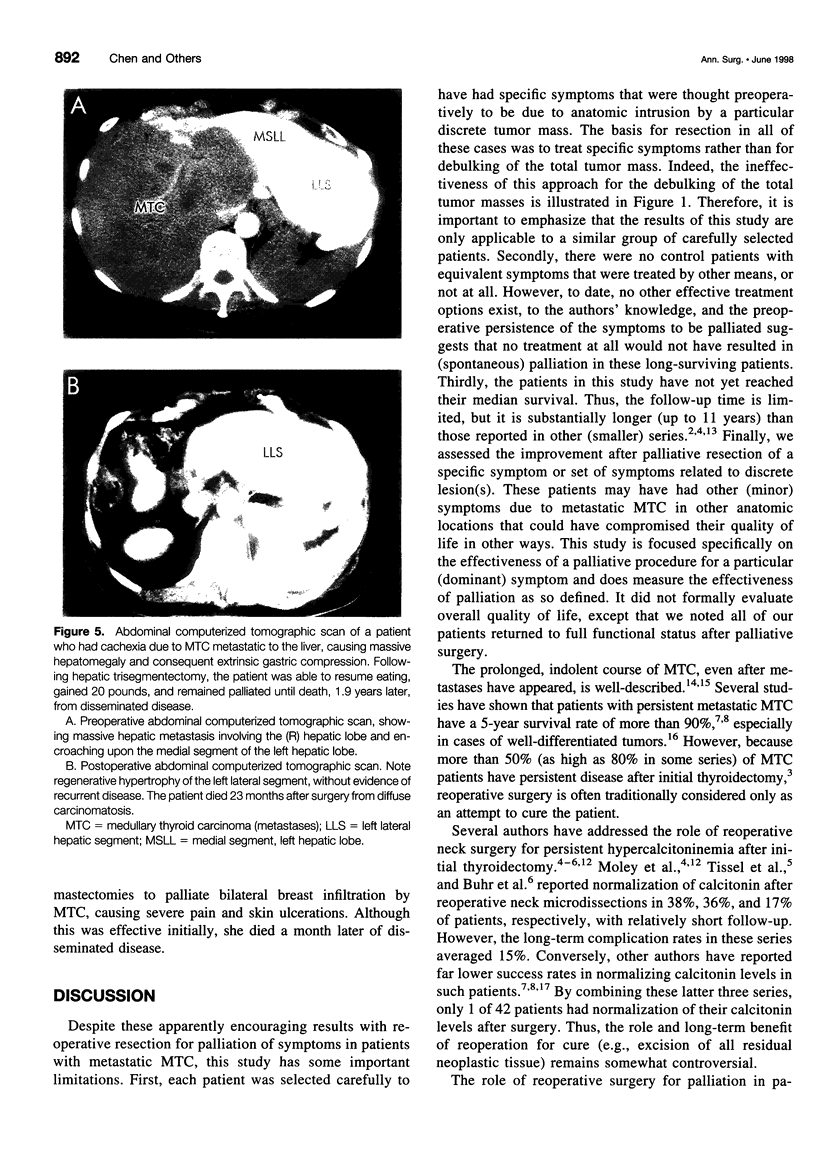
OBJECTIVE: To evaluate the short- and long-term consequences of palliative reresection of specific symptomatic lesions in patients with widely disseminated (incurable) medullary thyroid cancer (MTC). SUMMARY BACKGROUND DATA: Although reoperative neck microdissections can normalize calcitonin levels in patients with metastatic MTC confined to regional lymph nodes, there is no curative therapy for widely metastatic disease. However, these patients frequently have prolonged survival, but often with debilitating symptoms. METHODS: Between October 1981 and January 1997, 16 patients (mean age, 46 +/- 3 years; 10/16 female) underwent 21 palliative reoperations for unresectable MTC at the Johns Hopkins Hospital. All patients had significant symptom(s) or impending compromise of vital structures by a discrete lesion and had unequivocal preoperative evidence of a total disease burden that was unresectable. RESULTS: The mean interval from initial thyroidectomy to palliative surgery was 5.8 +/- 1.5 years. All patients had significant tumor burdens as evidenced by preoperative calcitonin values ranging from 900 to 222,500 pg/mL (nL < or = 17 pg/mL). The palliative operations consisted of reoperative neck dissection/mass excision (11), mediastinal mass resection (4), esophagectomy (1), liver trisegmentectomy (1), sigmoidectomy (1), bilateral simple mastectomies (1), pituitary resection (1), and subcutaneous mass excisions (1). All but two of the operative specimens contained MTC. There was no perioperative mortality. The long-term morbidity rate was limited to one recurrent laryngeal nerve injury. All patients had initial relief of the index symptom(s) after the palliative surgery, followed by a median actuarial symptom-free survival rate of 8.2 years. CONCLUSIONS: Patients with widely metastatic MTC often live for years, but many develop symptoms secondary to tumor persistence or progression. Judicious palliative, reoperative resection of discrete, symptomatic lesions can provide significant long-term relief of symptoms with minimal operative mortality and morbidity. In selected patients with metastatic MTC lesions causing significant symptoms or physical compromise, palliative reoperative resection should be considered despite the presence of widespread incurable metastatic disease.
Full text
PDF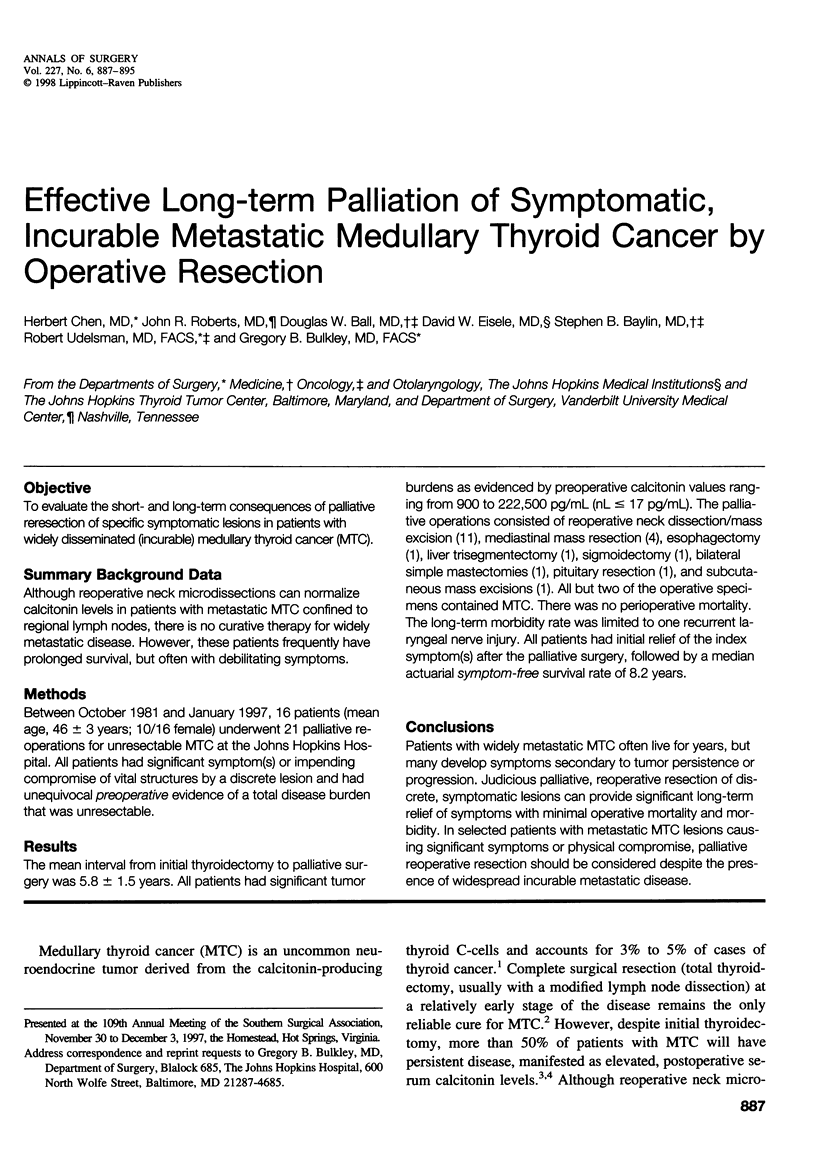
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bergholm U., Adami H. O., Auer G., Bergström R., Bäckdahl M., Grimelius L., Hansson G., Ljungberg O., Wilander E. Histopathologic characteristics and nuclear DNA content as prognostic factors in medullary thyroid carcinoma. A nationwide study in Sweden. The Swedish MTC Study Group. Cancer. 1989 Jul 1;64(1):135–142. doi: 10.1002/1097-0142(19890701)64:1<135::aid-cncr2820640123>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Bergholm U., Bergström R., Ekbom A. Long-term follow-up of patients with medullary carcinoma of the thyroid. Cancer. 1997 Jan 1;79(1):132–138. doi: 10.1002/(sici)1097-0142(19970101)79:1<132::aid-cncr19>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Buhr H. J., Kallinowski F., Raue F., Frank-Raue K., Herfarth C. Microsurgical neck dissection for occultly metastasizing medullary thyroid carcinoma. Three-year results. Cancer. 1993 Dec 15;72(12):3685–3693. doi: 10.1002/1097-0142(19931215)72:12<3685::aid-cncr2820721221>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Bulkley G. B., Bass K. N., Stephenson G. R., Diener-West M., George S., Reilly P. A., Baker R. R., Drachman D. B. Extended cervicomediastinal thymectomy in the integrated management of myasthenia gravis. Ann Surg. 1997 Sep;226(3):324–335. doi: 10.1097/00000658-199709000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Carson-Walter E. B., Baylin S. B., Nelkin B. D., Ball D. W. Differentiation of medullary thyroid cancer by C-Raf-1 silences expression of the neural transcription factor human achaete-scute homolog-1. Surgery. 1996 Aug;120(2):168–173. doi: 10.1016/s0039-6060(96)80284-4. [DOI] [PubMed] [Google Scholar]
- Ellenhorn J. D., Shah J. P., Brennan M. F. Impact of therapeutic regional lymph node dissection for medullary carcinoma of the thyroid gland. Surgery. 1993 Dec;114(6):1078–1082. [PubMed] [Google Scholar]
- Marzano L. A., Porcelli A., Biondi B., Lupoli G., Delrio P., Lombardi G., Zarrilli L. Surgical management and follow-up of medullary thyroid carcinoma. J Surg Oncol. 1995 Jul;59(3):162–168. doi: 10.1002/jso.2930590306. [DOI] [PubMed] [Google Scholar]
- Moley J. F., Dilley W. G., DeBenedetti M. K. Improved results of cervical reoperation for medullary thyroid carcinoma. Ann Surg. 1997 Jun;225(6):734–743. doi: 10.1097/00000658-199706000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moley J. F. Medullary thyroid cancer. Surg Clin North Am. 1995 Jun;75(3):405–420. doi: 10.1016/s0039-6109(16)46630-2. [DOI] [PubMed] [Google Scholar]
- Moley J. F., Wells S. A., Dilley W. G., Tisell L. E. Reoperation for recurrent or persistent medullary thyroid cancer. Surgery. 1993 Dec;114(6):1090–1096. [PubMed] [Google Scholar]
- Porter A. T., Ostrowski M. J. Medullary carcinoma of the thyroid treated by low-dose adriamycin. Br J Clin Pract. 1990 Nov;44(11):517–518. [PubMed] [Google Scholar]
- Saad M. F., Guido J. J., Samaan N. A. Radioactive iodine in the treatment of medullary carcinoma of the thyroid. J Clin Endocrinol Metab. 1983 Jul;57(1):124–128. doi: 10.1210/jcem-57-1-124. [DOI] [PubMed] [Google Scholar]
- Scherübl H., Raue F., Ziegler R. Combination chemotherapy of advanced medullary and differentiated thyroid cancer. Phase II study. J Cancer Res Clin Oncol. 1990;116(1):21–23. doi: 10.1007/BF01612635. [DOI] [PubMed] [Google Scholar]
- Tiede D. J., Tefferi A., Kochhar R., Thompson G. B., Hay I. D. Paraneoplastic cholestasis and hypercoagulability associated with medullary thyroid carcinoma. Resolution with tumor debulking. Cancer. 1994 Feb 1;73(3):702–705. doi: 10.1002/1097-0142(19940201)73:3<702::aid-cncr2820730333>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Tisell L. E., Hansson G., Jansson S., Salander H. Reoperation in the treatment of asymptomatic metastasizing medullary thyroid carcinoma. Surgery. 1986 Jan;99(1):60–66. [PubMed] [Google Scholar]
- Wells S. A., Jr, Dilley W. G., Farndon J. A., Leight G. S., Baylin S. B. Early diagnosis and treatment of medullary thyroid carcinoma. Arch Intern Med. 1985 Jul;145(7):1248–1252. [PubMed] [Google Scholar]
- van Heerden J. A., Grant C. S., Gharib H., Hay I. D., Ilstrup D. M. Long-term course of patients with persistent hypercalcitoninemia after apparent curative primary surgery for medullary thyroid carcinoma. Ann Surg. 1990 Oct;212(4):395–401. doi: 10.1097/00000658-199010000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]