Abstract
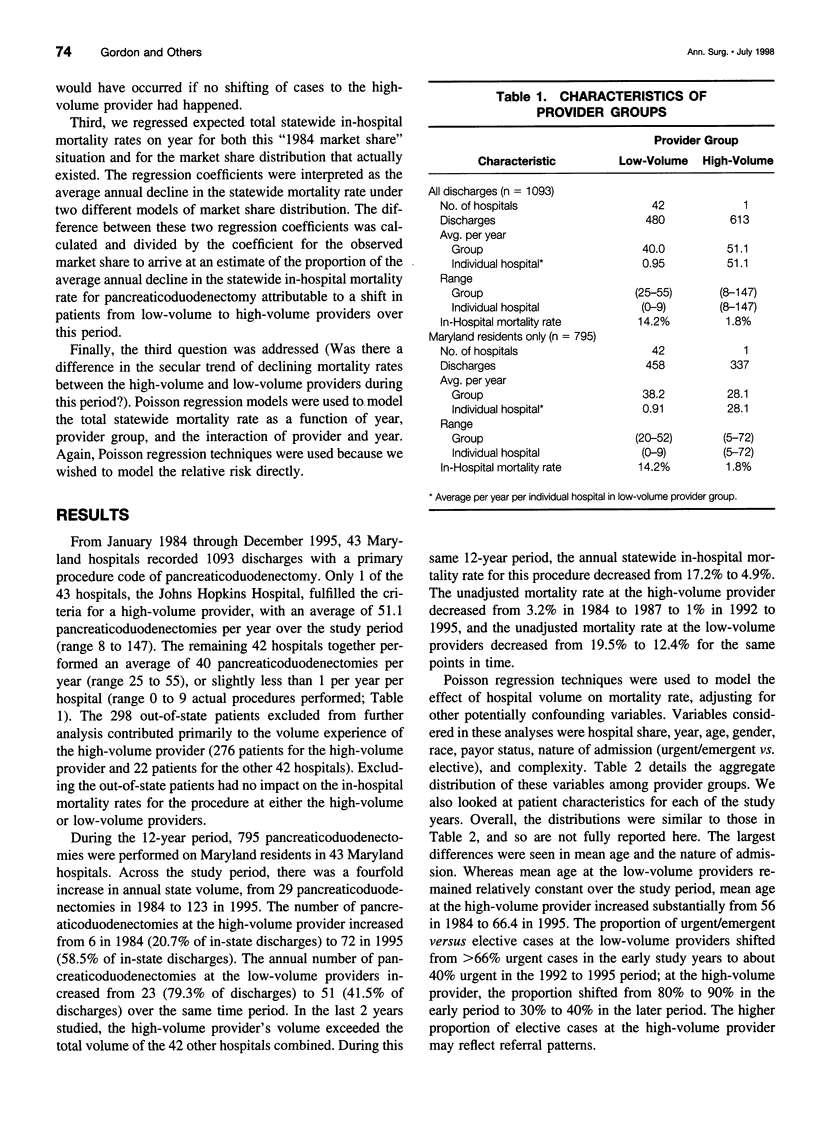
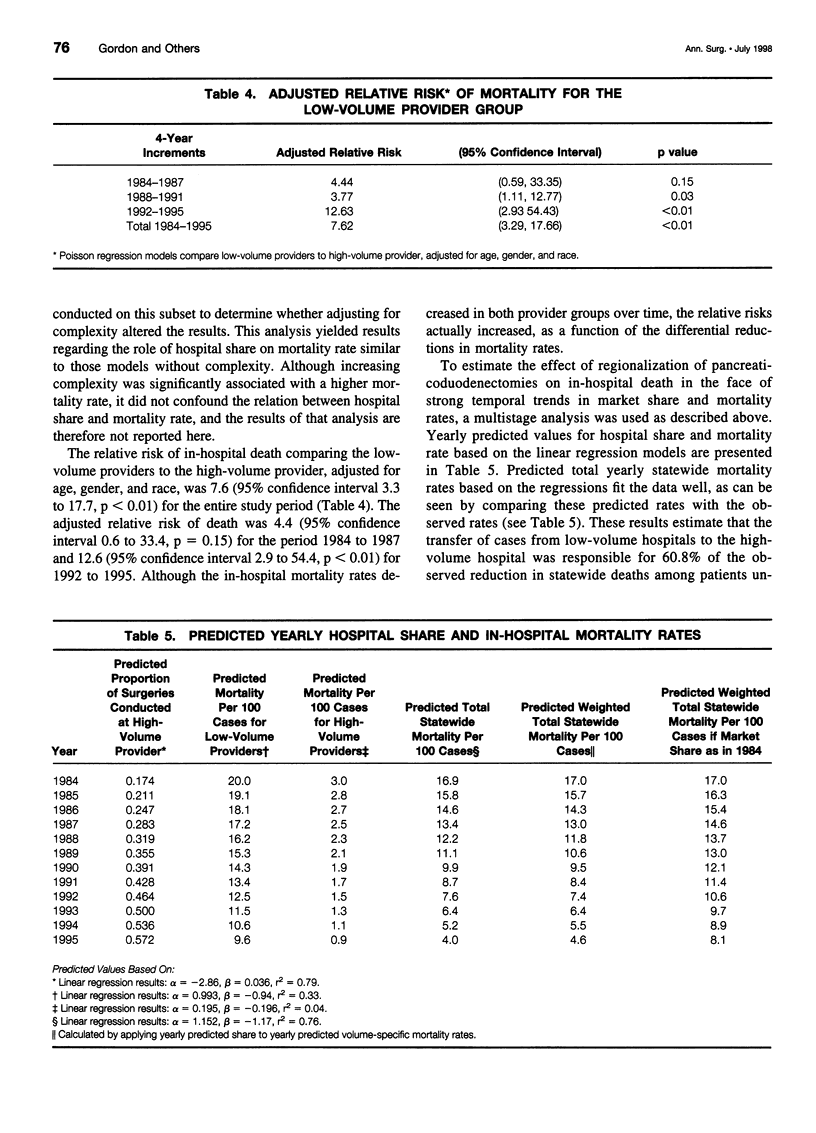
OBJECTIVE: This study examined a statewide trend in Maryland toward regionalization of pancreaticoduodenectomy over a 12-year period and its effect on statewide in-hospital mortality rates for this procedure. SUMMARY BACKGROUND DATA: Previous studies have demonstrated that the best outcomes are achieved in centers performing large numbers of pancreaticoduodenectomies, which suggests that regionalization could lower the overall in-hospital mortality rate for this procedure. METHODS: Maryland state hospital discharge data were used to select records of patients undergoing a pancreaticoduodenectomy between 1984 and 1995. Hospitals were classified into high-volume and low-volume provider groups. Trends in surgical volume and mortality rates were examined by provider group and for the entire state. Regression analyses were used to examine whether hospital share of pancreaticoduodenectomies was a significant predictor of the in-hospital mortality rate, adjusting for study year and patient characteristics. The portion of the decline in the statewide in-hospital mortality rate for this procedure attributable to the high-volume provider's increasing share was determined. RESULTS: A total of 795 pancreaticoduodenectomies were performed in Maryland at 43 hospitals from 1984 to 1995 (Maryland residents only). During this period, one institution increased its yearly share of pancreaticoduodenectomies from 20.7% to 58.5%, and the statewide in-hospital mortality rate for the procedure decreased from 17.2% to 4.9%. After adjustment for patient characteristics and study year, hospital share remained a significant predictor of mortality. An estimated 61% of the decline in the statewide in-hospital mortality rate for the procedure was attributable to the increase in share of discharges at the high-volume provider. CONCLUSIONS: A trend toward regionalization of pancreaticoduodenectomy over a 12-year period in Maryland was associated with a significant decrease in the statewide in-hospital mortality rate for this procedure, demonstrating the effectiveness of regionalization for high-risk surgery.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dragalin D., Perkins D., Plocher D. W. Institutes of Quality: Prudential's approach to outcomes management for specialty procedures. QRB Qual Rev Bull. 1990 Mar;16(3):111–115. doi: 10.1016/s0097-5990(16)30345-1. [DOI] [PubMed] [Google Scholar]
- Gold E. B. Epidemiology of and risk factors for pancreatic cancer. Surg Clin North Am. 1995 Oct;75(5):819–843. doi: 10.1016/s0039-6109(16)46730-7. [DOI] [PubMed] [Google Scholar]
- Gordon T. A., Burleyson G. P., Tielsch J. M., Cameron J. L. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg. 1995 Jan;221(1):43–49. doi: 10.1097/00000658-199501000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi L. C. Life, money, quality: the impact of regionalization on perinatal/neonatal intensive care. Neonatal Netw. 1988 Feb;6(4):53–59. [PubMed] [Google Scholar]
- Grumbach K., Anderson G. M., Luft H. S., Roos L. L., Brook R. Regionalization of cardiac surgery in the United States and Canada. Geographic access, choice, and outcomes. JAMA. 1995 Oct 25;274(16):1282–1288. [PubMed] [Google Scholar]
- Lieberman M. D., Kilburn H., Lindsey M., Brennan M. F. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg. 1995 Nov;222(5):638–645. doi: 10.1097/00000658-199511000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luft H. S., Bunker J. P., Enthoven A. C. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med. 1979 Dec 20;301(25):1364–1369. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- Maerki S. C., Luft H. S., Hunt S. S. Selecting categories of patients for regionalization. Implications of the relationship between volume and outcome. Med Care. 1986 Feb;24(2):148–158. doi: 10.1097/00005650-198602000-00006. [DOI] [PubMed] [Google Scholar]
- Renlund D. G., Bristow M. R., Lybbert M. R., O'Connell J. B., Gay W. A., Jr Medicare-designated centers for cardiac transplantation. N Engl J Med. 1987 Apr 2;316(14):873–876. doi: 10.1056/NEJM198704023161411. [DOI] [PubMed] [Google Scholar]
- Shackford S. R., Mackersie R. C., Hoyt D. B., Baxt W. G., Eastman A. B., Hammill F. N., Knotts F. B., Virgilio R. W. Impact of a trauma system on outcome of severely injured patients. Arch Surg. 1987 May;122(5):523–527. doi: 10.1001/archsurg.1987.01400170029003. [DOI] [PubMed] [Google Scholar]


