Abstract
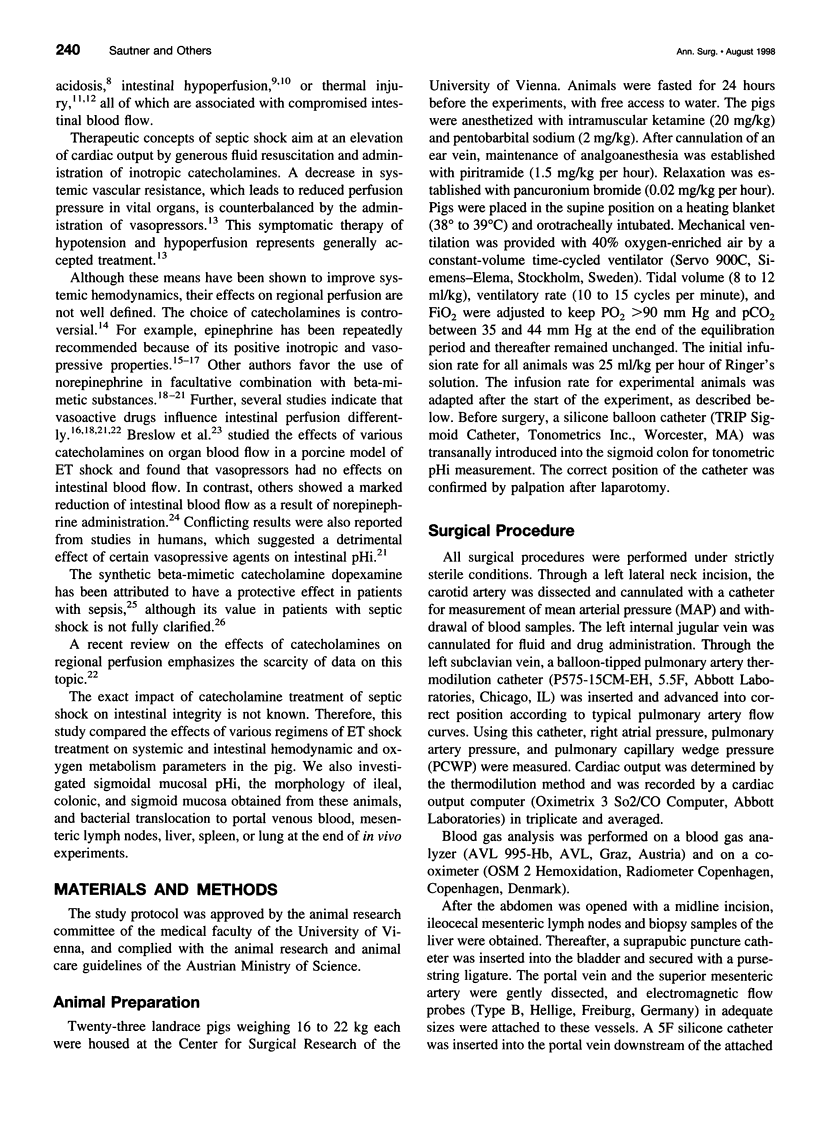
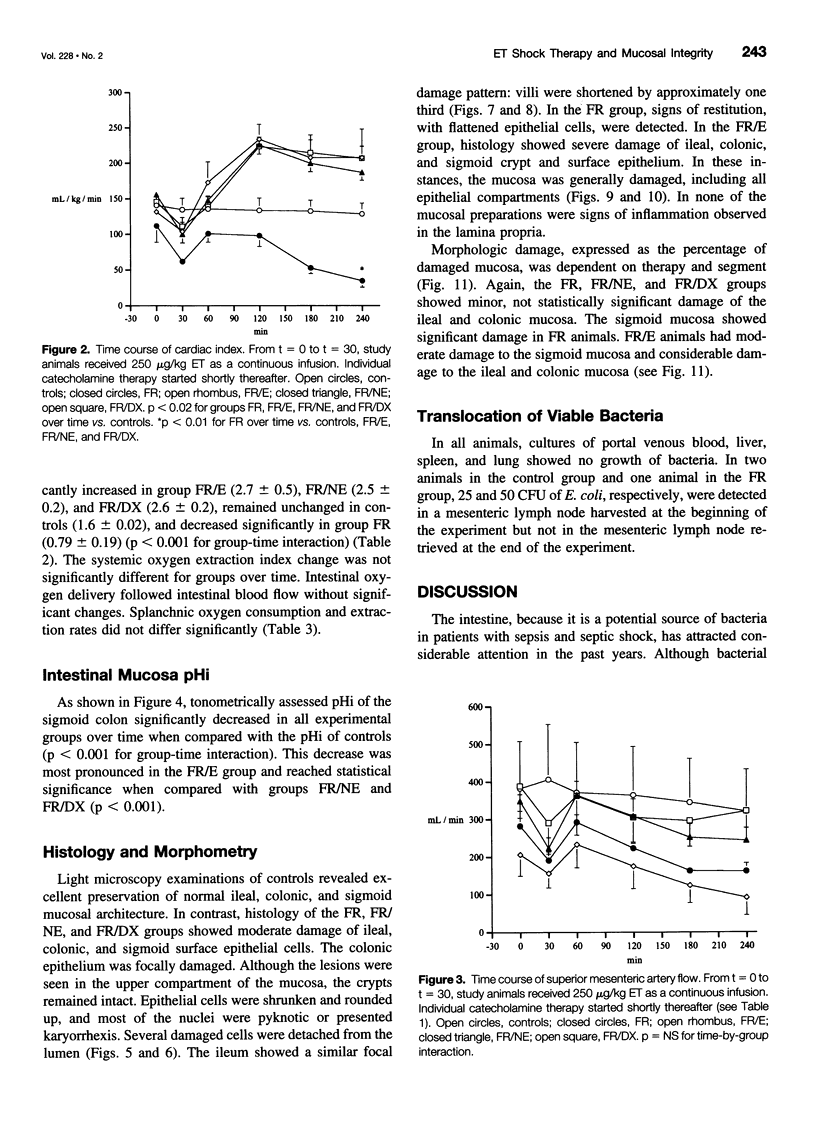
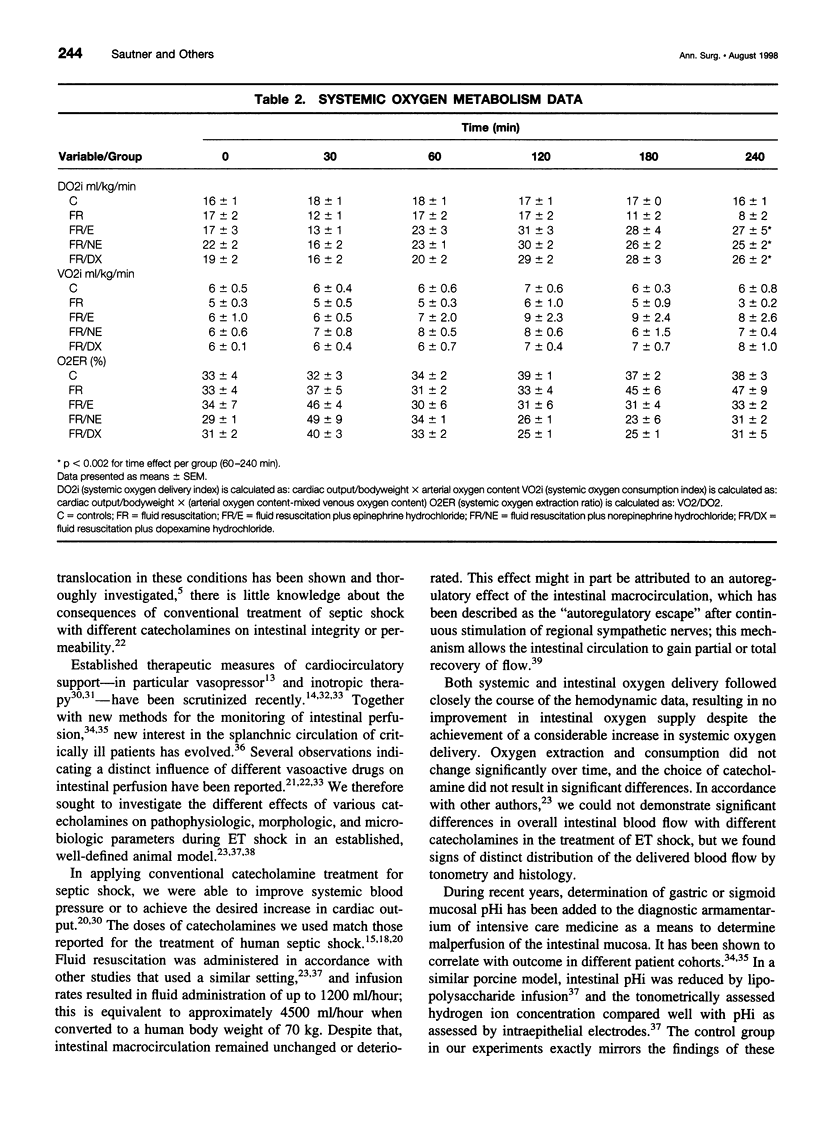
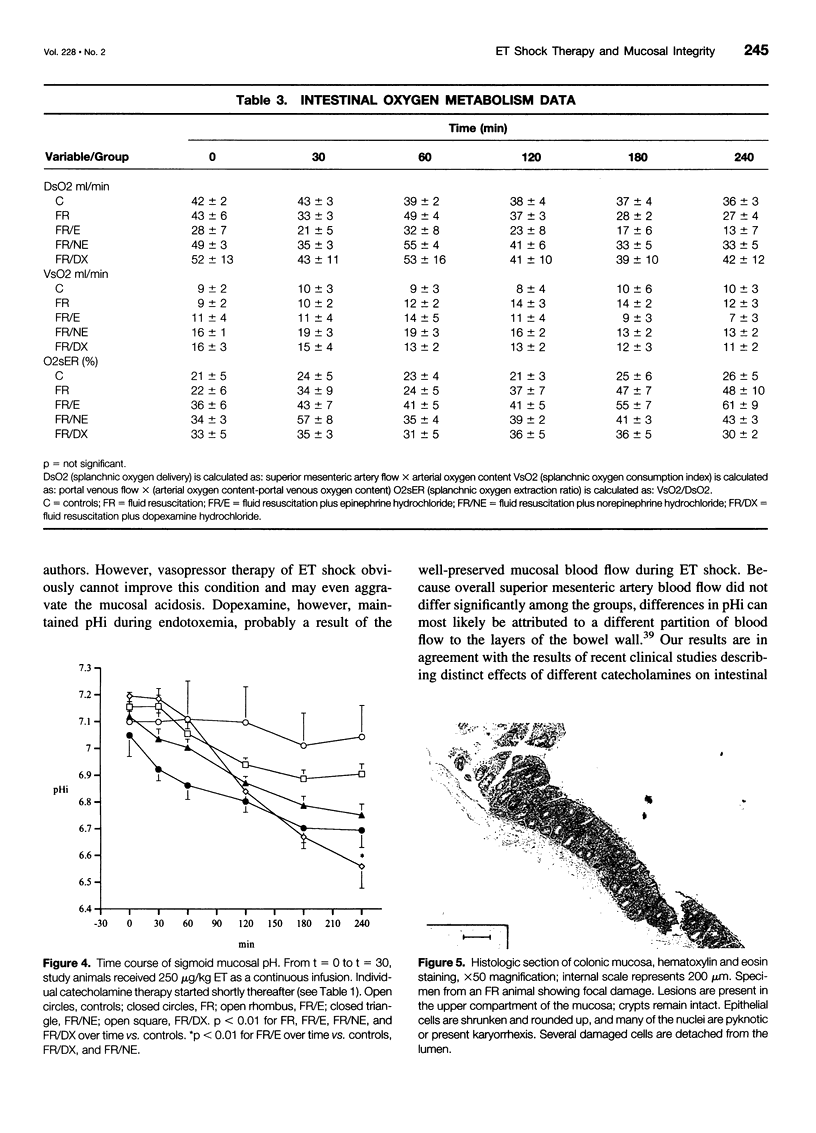
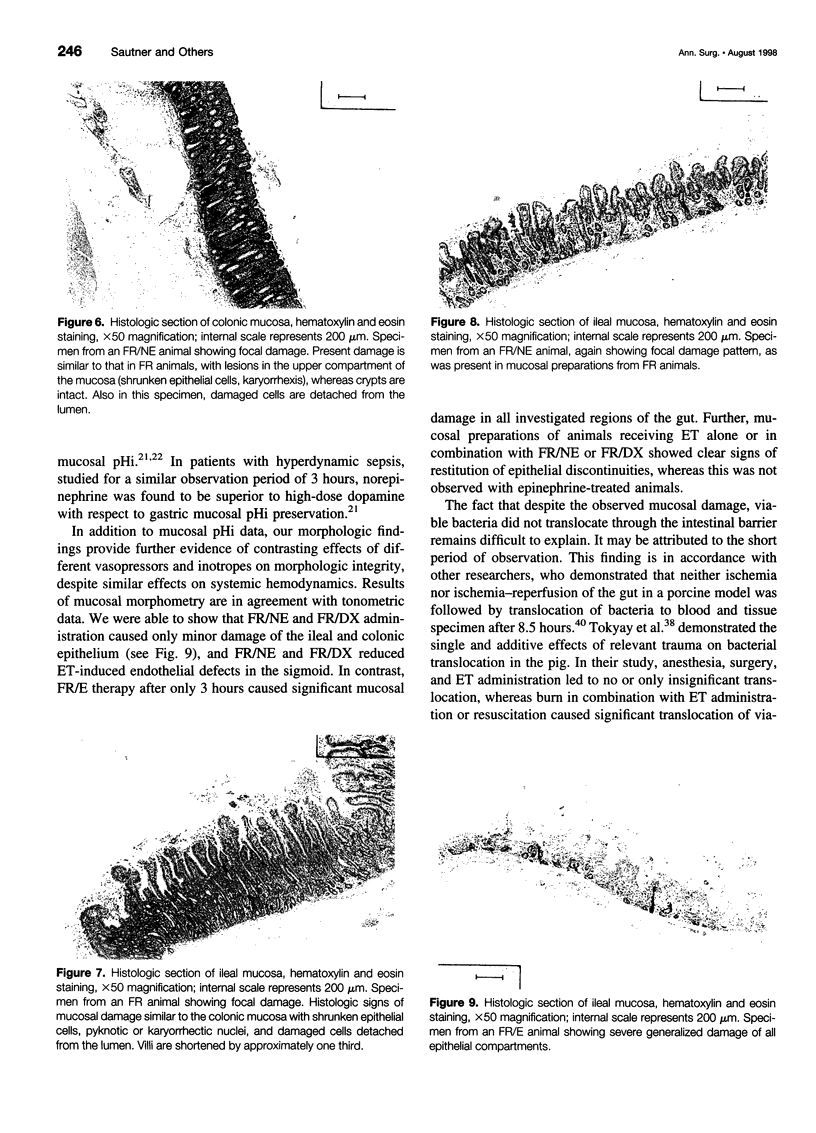
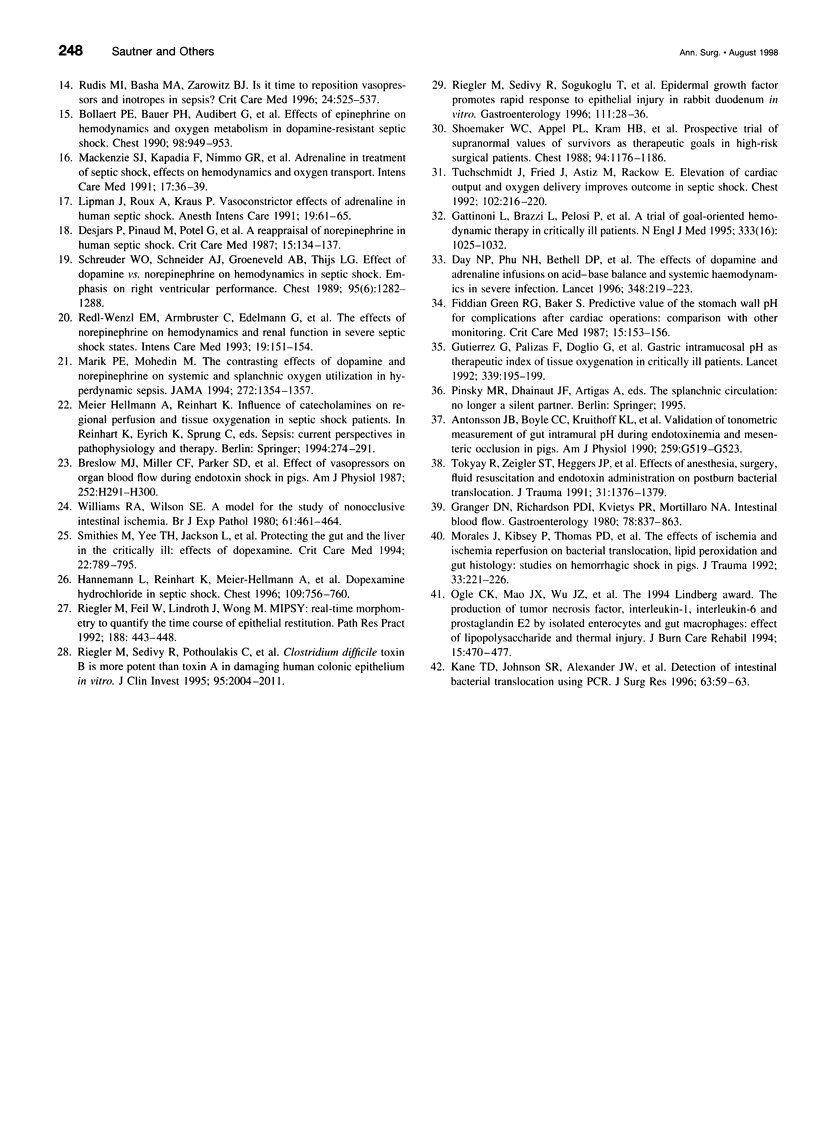
OBJECTIVE: To determine the early effects of therapy of endotoxin (ET) shock with epinephrine, norepinephrine, or dopexamine on splanchnic circulation, oxygen metabolism, sigmoid mucosal pHi, bacterial translocation, and morphologic integrity of the ileal, colonic, and sigmoid mucosa. SUMMARY BACKGROUND DATA: Conflicting concepts exist concerning the catecholamine therapy of septic shock, but little is known about the effects of catecholamine treatment on splanchnic circulation and mucosal integrity. METHODS: ET shock was induced in pigs by ET infusion over 30 minutes, and animals were studied for 4 hours. All animals were resuscitated with fluid. To mimic the treatment of septic shock in humans, mean arterial pressure was maintained in two groups at >70 mm Hg with the administration of epinephrine or norepinephrine. A third group of animals received dopexamine at 7 microg/kg per minute. Systemic and splanchnic blood flow and oxygen metabolism were studied, sigmoid colon mucosal pHi was obtained tonometrically, and bacterial translocation was determined by culture of portal venous blood, mesenteric lymph nodes, liver, spleen, and lung specimens. Histologic sections of ileal, colonic, and sigmoid mucosa were morphometrically examined for therapy effects. RESULTS: All investigated catecholamines increased cardiac output and systemic oxygen delivery, whereas intestinal blood flow and oxygen delivery remained unchanged. Sigmoid mucosal pHi decreased in all study animals, but the decrease was most pronounced in the epinephrine group. Pigs receiving epinephrine also showed >40% damage of the mucosa of the ileum and colon, whereas animals receiving ET alone, norepinephrine, or dopexamine showed only moderate lesions with signs of restitution. No animal showed bacterial translocation. CONCLUSIONS: Systemic hemodynamics and oxygen metabolism data do not reflect intestinal perfusion. Norepinephrine or dopexamine administration in ET shock causes no additional impairment of intestinal integrity. Epinephrine therapy, in contrast, is associated with a significant reduction of mucosal pHi and considerable early mucosal damage. Its application in septic shock is hazardous.
Full text
PDF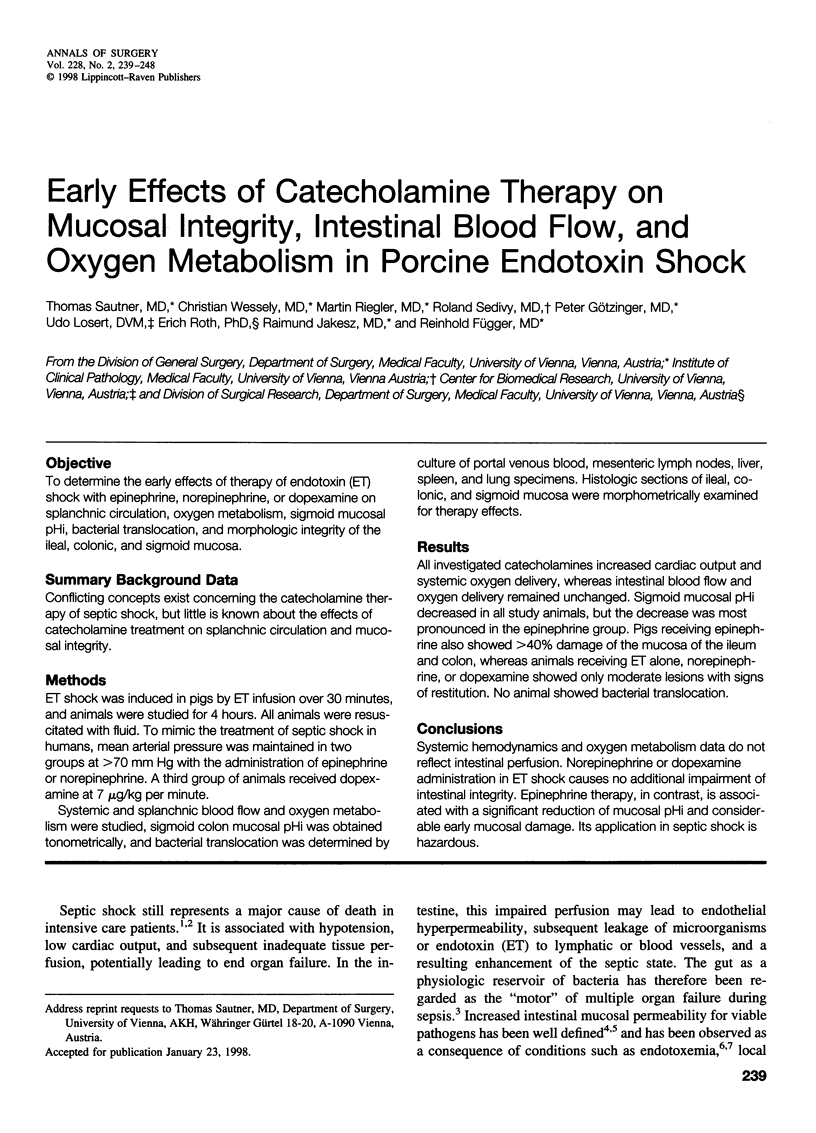
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander J. W., Boyce S. T., Babcock G. F., Gianotti L., Peck M. D., Dunn D. L., Pyles T., Childress C. P., Ash S. K. The process of microbial translocation. Ann Surg. 1990 Oct;212(4):496–512. doi: 10.1097/00000658-199010000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonsson J. B., Boyle C. C., 3rd, Kruithoff K. L., Wang H. L., Sacristan E., Rothschild H. R., Fink M. P. Validation of tonometric measurement of gut intramural pH during endotoxemia and mesenteric occlusion in pigs. Am J Physiol. 1990 Oct;259(4 Pt 1):G519–G523. doi: 10.1152/ajpgi.1990.259.4.G519. [DOI] [PubMed] [Google Scholar]
- Baue A. E. Multiple organ failure, multiple organ dysfunction syndrome, and the systemic inflammatory response syndrome-where do we stand? Shock. 1994 Dec;2(6):385–397. doi: 10.1097/00024382-199412000-00001. [DOI] [PubMed] [Google Scholar]
- Bollaert P. E., Bauer P., Audibert G., Lambert H., Larcan A. Effects of epinephrine on hemodynamics and oxygen metabolism in dopamine-resistant septic shock. Chest. 1990 Oct;98(4):949–953. doi: 10.1378/chest.98.4.949. [DOI] [PubMed] [Google Scholar]
- Breslow M. J., Miller C. F., Parker S. D., Walman A. T., Traystman R. J. Effect of vasopressors on organ blood flow during endotoxin shock in pigs. Am J Physiol. 1987 Feb;252(2 Pt 2):H291–H300. doi: 10.1152/ajpheart.1987.252.2.H291. [DOI] [PubMed] [Google Scholar]
- Brun-Buisson C., Doyon F., Carlet J., Dellamonica P., Gouin F., Lepoutre A., Mercier J. C., Offenstadt G., Régnier B. Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. French ICU Group for Severe Sepsis. JAMA. 1995 Sep 27;274(12):968–974. [PubMed] [Google Scholar]
- Day N. P., Phu N. H., Bethell D. P., Mai N. T., Chau T. T., Hien T. T., White N. J. The effects of dopamine and adrenaline infusions on acid-base balance and systemic haemodynamics in severe infection. Lancet. 1996 Jul 27;348(9022):219–223. doi: 10.1016/s0140-6736(96)09096-4. [DOI] [PubMed] [Google Scholar]
- Deitch E. A., Ma W. J., Ma L., Berg R., Specian R. D. Endotoxin-induced bacterial translocation: a study of mechanisms. Surgery. 1989 Aug;106(2):292–300. [PubMed] [Google Scholar]
- Desjars P., Pinaud M., Potel G., Tasseau F., Touze M. D. A reappraisal of norepinephrine therapy in human septic shock. Crit Care Med. 1987 Feb;15(2):134–137. doi: 10.1097/00003246-198702000-00011. [DOI] [PubMed] [Google Scholar]
- Fiddian-Green R. G., Baker S. Predictive value of the stomach wall pH for complications after cardiac operations: comparison with other monitoring. Crit Care Med. 1987 Feb;15(2):153–156. doi: 10.1097/00003246-198702000-00015. [DOI] [PubMed] [Google Scholar]
- Gattinoni L., Brazzi L., Pelosi P., Latini R., Tognoni G., Pesenti A., Fumagalli R. A trial of goal-oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995 Oct 19;333(16):1025–1032. doi: 10.1056/NEJM199510193331601. [DOI] [PubMed] [Google Scholar]
- Granger D. N., Richardson P. D., Kvietys P. R., Mortillaro N. A. Intestinal blood flow. Gastroenterology. 1980 Apr;78(4):837–863. [PubMed] [Google Scholar]
- Gutierrez G., Palizas F., Doglio G., Wainsztein N., Gallesio A., Pacin J., Dubin A., Schiavi E., Jorge M., Pusajo J. Gastric intramucosal pH as a therapeutic index of tissue oxygenation in critically ill patients. Lancet. 1992 Jan 25;339(8787):195–199. doi: 10.1016/0140-6736(92)90002-k. [DOI] [PubMed] [Google Scholar]
- Hannemann L., Reinhart K., Meier-Hellmann A., Wallenfang G., Bredle D. L. Dopexamine hydrochloride in septic shock. Chest. 1996 Mar;109(3):756–760. doi: 10.1378/chest.109.3.756. [DOI] [PubMed] [Google Scholar]
- Herndon D. N., Zeigler S. T. Bacterial translocation after thermal injury. Crit Care Med. 1993 Feb;21(2 Suppl):S50–S54. doi: 10.1097/00003246-199302001-00010. [DOI] [PubMed] [Google Scholar]
- Horton J. W. Alterations in intestinal permeability and blood flow in a new model of mesenteric ischemia. Circ Shock. 1992 Feb;36(2):134–139. [PubMed] [Google Scholar]
- Inoue S., Wirman J. A., Alexander J. W., Trocki O., Cardell R. R. Candida albicans translocation across the gut mucosa following burn injury. J Surg Res. 1988 May;44(5):479–492. doi: 10.1016/0022-4804(88)90152-7. [DOI] [PubMed] [Google Scholar]
- Kane T. D., Johnson S. R., Alexander J. W., Babcock G. F., Ogle C. K. Detection of intestinal bacterial translocation using PCR. J Surg Res. 1996 Jun;63(1):59–63. doi: 10.1006/jsre.1996.0223. [DOI] [PubMed] [Google Scholar]
- Krause W., Matheis H., Wulf K. Fungaemia and funguria after oral administration of Candida albicans. Lancet. 1969 Mar 22;1(7595):598–599. doi: 10.1016/s0140-6736(69)91534-7. [DOI] [PubMed] [Google Scholar]
- Lipman J., Roux A., Kraus P. Vasoconstrictor effects of adrenaline in human septic shock. Anaesth Intensive Care. 1991 Feb;19(1):61–65. doi: 10.1177/0310057X9101900111. [DOI] [PubMed] [Google Scholar]
- Mackenzie S. J., Kapadia F., Nimmo G. R., Armstrong I. R., Grant I. S. Adrenaline in treatment of septic shock: effects on haemodynamics and oxygen transport. Intensive Care Med. 1991;17(1):36–39. doi: 10.1007/BF01708407. [DOI] [PubMed] [Google Scholar]
- Marik P. E., Mohedin M. The contrasting effects of dopamine and norepinephrine on systemic and splanchnic oxygen utilization in hyperdynamic sepsis. JAMA. 1994 Nov 2;272(17):1354–1357. [PubMed] [Google Scholar]
- Morales J., Kibsey P., Thomas P. D., Poznansky M. J., Hamilton S. M. The effects of ischemia and ischemia-reperfusion on bacterial translocation, lipid peroxidation, and gut histology: studies on hemorrhagic shock in pigs. J Trauma. 1992 Aug;33(2):221–227. doi: 10.1097/00005373-199208000-00010. [DOI] [PubMed] [Google Scholar]
- Navaratnam R. L., Morris S. E., Traber D. L., Flynn J., Woodson L., Linares H., Herndon D. N. Endotoxin (LPS) increases mesenteric vascular resistance (MVR) and bacterial translocation (BT). J Trauma. 1990 Sep;30(9):1104–1115. doi: 10.1097/00005373-199009000-00006. [DOI] [PubMed] [Google Scholar]
- Ogle C. K., Mao J. X., Wu J. Z., Ogle J. D., Alexander J. W. The 1994 Lindberg Award. The production of tumor necrosis factor, interleukin-1, interleukin-6, and prostaglandin E2 by isolated enterocytes and gut macrophages: effect of lipopolysaccharide and thermal injury. J Burn Care Rehabil. 1994 Nov-Dec;15(6):470–477. [PubMed] [Google Scholar]
- Redl-Wenzl E. M., Armbruster C., Edelmann G., Fischl E., Kolacny M., Wechsler-Fördös A., Sporn P. The effects of norepinephrine on hemodynamics and renal function in severe septic shock states. Intensive Care Med. 1993;19(3):151–154. doi: 10.1007/BF01720530. [DOI] [PubMed] [Google Scholar]
- Riegler M., Feil W., Lindroth J., Wong M. MIPSY: real-time morphometry to quantify the time course of rapid epithelial restitution. Pathol Res Pract. 1992 Jun;188(4-5):443–448. doi: 10.1016/S0344-0338(11)80035-X. [DOI] [PubMed] [Google Scholar]
- Riegler M., Sedivy R., Pothoulakis C., Hamilton G., Zacherl J., Bischof G., Cosentini E., Feil W., Schiessel R., LaMont J. T. Clostridium difficile toxin B is more potent than toxin A in damaging human colonic epithelium in vitro. J Clin Invest. 1995 May;95(5):2004–2011. doi: 10.1172/JCI117885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegler M., Sedivy R., Sogukoglu T., Cosentini E., Bischof G., Teleky B., Feil W., Schiessel R., Hamilton G., Wenzl E. Epidermal growth factor promotes rapid response to epithelial injury in rabbit duodenum in vitro. Gastroenterology. 1996 Jul;111(1):28–36. doi: 10.1053/gast.1996.v111.pm8698221. [DOI] [PubMed] [Google Scholar]
- Rudis M. I., Basha M. A., Zarowitz B. J. Is it time to reposition vasopressors and inotropes in sepsis? Crit Care Med. 1996 Mar;24(3):525–537. doi: 10.1097/00003246-199603000-00026. [DOI] [PubMed] [Google Scholar]
- Salzman A. L., Wang H., Wollert P. S., Vandermeer T. J., Compton C. C., Denenberg A. G., Fink M. P. Endotoxin-induced ileal mucosal hyperpermeability in pigs: role of tissue acidosis. Am J Physiol. 1994 Apr;266(4 Pt 1):G633–G646. doi: 10.1152/ajpgi.1994.266.4.G633. [DOI] [PubMed] [Google Scholar]
- Saydjari R., Beerthuizen G. I., Townsend C. M., Jr, Herndon D. N., Thompson J. C. Bacterial translocation and its relationship to visceral blood flow, gut mucosal ornithine decarboxylase activity, and DNA in pigs. J Trauma. 1991 May;31(5):639–644. doi: 10.1097/00005373-199105000-00007. [DOI] [PubMed] [Google Scholar]
- Schreuder W. O., Schneider A. J., Groeneveld A. B., Thijs L. G. Effect of dopamine vs norepinephrine on hemodynamics in septic shock. Emphasis on right ventricular performance. Chest. 1989 Jun;95(6):1282–1288. doi: 10.1378/chest.95.6.1282. [DOI] [PubMed] [Google Scholar]
- Shoemaker W. C., Appel P. L., Kram H. B., Waxman K., Lee T. S. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988 Dec;94(6):1176–1186. doi: 10.1378/chest.94.6.1176. [DOI] [PubMed] [Google Scholar]
- Smithies M., Yee T. H., Jackson L., Beale R., Bihari D. Protecting the gut and the liver in the critically ill: effects of dopexamine. Crit Care Med. 1994 May;22(5):789–795. doi: 10.1097/00003246-199405000-00013. [DOI] [PubMed] [Google Scholar]
- Tokyay R., Zeigler S. T., Heggers J. P., Loick H. M., Traber D. L., Herndon D. N. Effects of anesthesia, surgery, fluid resuscitation, and endotoxin administration on postburn bacterial translocation. J Trauma. 1991 Oct;31(10):1376–1379. doi: 10.1097/00005373-199110000-00010. [DOI] [PubMed] [Google Scholar]
- Tuchschmidt J., Fried J., Astiz M., Rackow E. Elevation of cardiac output and oxygen delivery improves outcome in septic shock. Chest. 1992 Jul;102(1):216–220. doi: 10.1378/chest.102.1.216. [DOI] [PubMed] [Google Scholar]
- williams R. A., Wilson S. E. A model for the study of nonocclusive intestinal ischaemia. Br J Exp Pathol. 1980 Oct;61(5):461–464. [PMC free article] [PubMed] [Google Scholar]