Summary
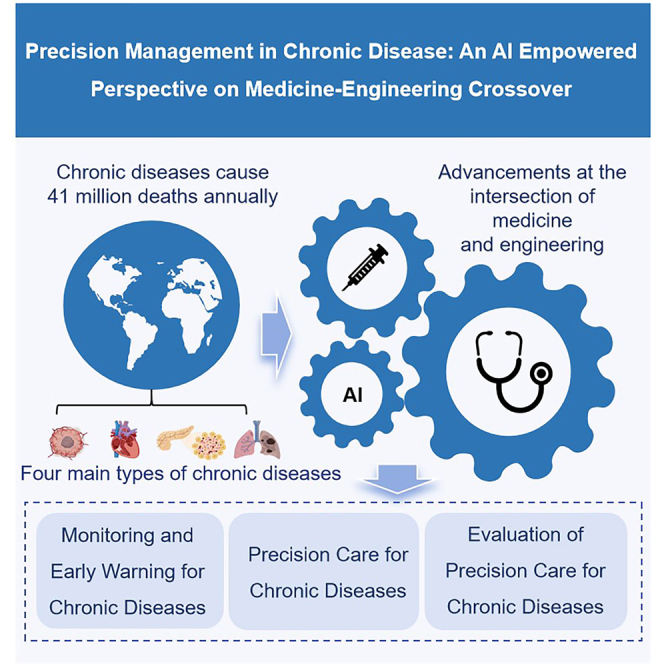
Precision management of chronic diseases is crucial for improving patient quality of life and alleviating global health burdens. Advancements at the intersection of medicine and engineering, particularly through artificial intelligence (AI), have driven significant progress in precision care. From the perspective of the full life span management of chronic diseases, we focus on medicine-engineering crossover for monitoring chronic diseases, developing and implementing precision care plans, and evaluating care outcomes. Through an in-depth discussion, we address key issues such as AI’s potential to enable precision care and the challenges associated with its implementation, including data accuracy, privacy concerns, and clinical adoption. Emphasizing the importance of nurses embracing new technologies and interdisciplinary collaboration, this paper highlights how technological innovation can improve chronic disease management, particularly by enhancing care efficiency and personalizing health interventions. We aim to support the development of integrated healthcare solutions that improve patient outcomes in chronic disease management.
Subject areas: Artificial intelligence, Health sciences, Nursing, Robotics
Graphical abstract
Artificial intelligence; Health sciences; Nursing; Robotics
Introduction
As the global burden of chronic diseases increases, nursing plays a critical role in healthcare systems.1,2 The World Health Organization (WHO) states that chronic diseases cause 41 million deaths each year, accounting for 74% of total fatalities and significantly straining healthcare resources.3 In 2021, the four main types of chronic diseases—cardiovascular diseases (such as heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) and diabetes—account for 80% of all premature deaths attributed to chronic diseases.3 Consequently, prioritizing prevention and management policies for the four main types of chronic diseases is imperative, necessitating global collaboration and a coordinated multidisciplinary approach.4 To address this escalating burden, the WHO has recommended a life course strategy for preventing and controlling chronic diseases,5,6 which encompasses comprehensive management through screening, prevention, treatment, rehabilitation, and long-term follow-up care.7,8
In light of these challenges, there is a significant opportunity for integrating emerging technologies to improve the quality of care.9,10 Developments in artificial intelligence (AI) and the intersection of medicine and engineering are reshaping healthcare practices,11 particularly in chronic disease management.12,13,14,15 The intersection of medicine and engineering approach aims to leverage engineering technologies to develop innovative medical tools that address complex health challenges.16 The application of AI in healthcare is expanding. Research indicated that by analyzing patient health data and incorporating advanced biomedical engineering techniques,17,18 AI could support personalized disease management plans and enhance overall health outcomes.19,20 However, rapid technological advancements have introduced new challenges, including data accuracy, portability, application diversity, and clinical adoption.21 Additionally, ensuring patient data privacy and security22,23 while balancing humanistic care with technological support are crucial.24,25 Moreover, nursing professionals must continuously adapt to new technologies to apply them effectively in clinical settings.26
In this perspective, we discuss how AI empowers precision care for the four main types of chronic diseases across the life span through the intersection of medicine and engineering. At the same time, we consider future trends and challenges in this field and offer specific recommendations for nursing practice. We believe that promoting interdisciplinary collaboration and technological innovation is essential for achieving precision nursing in chronic disease management throughout the life course. By integrating diverse data sources and employing intelligent analysis, we can effectively merge technology with humanistic care, leading to more efficient and personalized chronic disease management services.
Monitoring and early warning for chronic diseases
AI is shifting from a model-centric approach to integrating data value and mechanisms.27 This section will focus on the development and specific applications of interdisciplinary medicine and engineering technologies, along with AI, in the monitoring, and early warning of chronic diseases.
Wearable device technology
Wearable devices have significantly enhanced the efficiency and accuracy of chronic disease monitoring by integrating sensors, the Internet of Things, and AI technologies,15 which have been widely utilized for monitoring cancer, cardiovascular, cerebrovascular, respiratory, and metabolic diseases.28,29,30,31,32,33,34,35,36,37,38 These devices employ a variety of sensors, including electrocardiogram (ECG) sensors,39,40 glucose sensors,41 and integrated sensor systems,28 to monitor heart rate, blood oxygen saturation, respiratory rate, sleep, physical activity, and glucose levels in real-time. However, sensors may be affected by factors such as exercise state, temperature changes, electromagnetic interference, sensor placement, and changes in body position, leading to measurement errors in the data. Many wearable devices and sensors are bulky and uncomfortable, which may limit their long-term use, particularly among patients with chronic conditions.21 Future research could focus on developing smaller, lighter, and more user-friendly devices to improve both usability and patient compliance. Additionally, the accuracy of wearable device monitoring varies, which can lead to unnecessary misdiagnoses, increase the workload of healthcare providers, and heighten patient anxiety.42 Wearable devices for chronic respiratory diseases43,44,45 and diabetes41 enable remote monitoring and cloud-based data sharing, improving patient care and decision-making without hospital visits. Although wearable devices indeed provide valuable information for clinical use, it remains unclear whether patients effectively utilize this information to guide self-management, or even whether they perceive it as useful. There is limited understanding of how chronic disease patients accept wearable devices, or whether specific barriers to implementation exist within certain patient groups.34
Combining AI and machine learning technologies allows wearable devices to deeply analyze data, predict disease deterioration trends, and offer personalized health management recommendations.15,31,35 However, these technologies also raise concerns about data security, algorithm transparency, and potential biases in predictive models. In the future, measures such as data encryption, enhancing algorithm transparency, optimizing training data, and introducing fairness algorithms can effectively reduce the impact of these issues on patients and healthcare services. Additionally, establishing clear ethical frameworks and regulatory mechanisms is essential to protect patients’ privacy and rights. Furthermore, many commercial devices have not undergone rigorous medical validation, which limits their application in clinical settings. In Australia, 73% of wearable technologies currently in use are not yet legislated.34 While some devices offer precise monitoring, the lack of legal regulation makes them challenging to use for clinical decision-making.46 Clinical workflows are inherently dynamic, and while wearable devices must ensure safety in monitoring, healthcare professionals face the added burden of learning new technologies and systems amidst their already demanding workloads. These challenges have limited the integration of wearable devices into clinical practice.47 Future efforts should focus on exploring the advantages and risks of wearable devices in chronic disease management from the perspective of healthcare professionals, enabling their seamless integration into clinical workflows.
Contactless monitoring technology
While wearable devices face poor compliance and data accuracy challenges, contactless monitoring technologies offer continuous tracking with improved comfort.29,33 Radar sensors have demonstrated potential in monitoring respiratory rates among high-risk opioid users and patients with pulmonary conditions or sleep apnea. Nonetheless, motion artifacts and observer interference may adversely affect the precision of respiratory rate measurements. For instance, when observers position themselves near patients to obtain optimal respiratory readings, the radar may inadvertently detect the observer’s respiratory rate instead.48 For hypertension, contactless technology employs facial camera images to detect pulse waves49 and Doppler radar50 for blood pressure prediction. Combined with smartphone applications, transdermal optical imaging technology enables contactless blood pressure monitoring through video-based remote operation. Unlike cuff-based methods, this approach allows blood pressure measurements to be taken at various times and locations.51 However, the technology has only been validated in individuals with normal blood pressure, and its robustness in monitoring hypertensive or hypotensive subjects remains untested. Moreover, these technologies are primarily designed for measuring blood pressure in a resting state, and it is unclear whether they can reliably monitor blood pressure in different environments (e.g., outdoors, in moving vehicles, or under low light conditions) or during physical activity.49,51 Fritz et al.52 reported that home-based sensors enable remote monitoring of clinically relevant health events, particularly in patients with chronic diseases, and noted that nurses utilizing smart health technologies improved the interpretation and application of sensor data. As frontline healthcare providers, nurses are well-positioned to act as intermediaries for sensor data, offering insights that support remote care and opening new pathways for evidence-based practices.
Pathway to key technologies
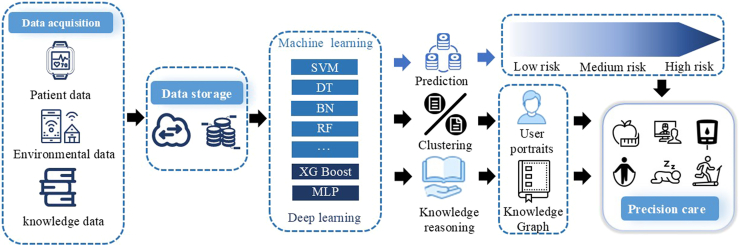
By integrating medical engineering and AI, precision monitoring, prediction, and management of chronic diseases are attainable (Figure 1). Non-invasive sensors and wearable devices continuously capture patients’ physiological and environmental data in real time, transmitting this information to cloud storage via wireless networks for analysis using AI technology. This approach supports early detection and prediction of chronic disease progression. Using AI algorithms such as machine learning and deep learning to integrate diverse data sources helps identify health risks and uncover underlying mechanisms.AI algorithms, like machine learning and deep learning, integrate data to identify health risks, uncover mechanisms, and enable personalized care plans.30 Additionally, these systems dynamically optimize care plans in response to changes in patient health, thereby enhancing care quality.
Figure 1.
Pathway to key technologies for precision care in chronic diseases through AI-empowered perspective on medicine-engineering crossover
SVM, support vector machines; DT, Decision Tree; BN, Bayesian network; RF, Random Forest; XG Boost, eXtreme Gradient Boosting; MLP, Multilayer perceptron.
Challenges and prospects
Wearable devices and non-invasive sensors integrated with AI have been used for chronic disease risk monitoring, but challenges such as poor user interaction, high costs, and low patient acceptance limit their clinical application. Nurses often play a minimal role in technology development, primarily during validation,53 and standardized AI reporting frameworks in nursing research are lacking.26 Additionally, clinical workflows are inherently dynamic, and while wearable devices must ensure safety in monitoring, healthcare professionals face the added burden of learning new technologies and systems amidst their already demanding workloads. These challenges have limited the integration of wearable devices into clinical practice.47
Contactless sensors primarily rely on behavioral characteristics and movement patterns to detect health events, making them less effective for events without significant behavioral changes. While conditions such as blood glucose fluctuations or strokes may eventually affect behavior, environmental sensors alone are insufficient for timely intervention in acute events. Integrating smart home sensors with wearable devices could enhance their utility. Despite their potential, environmental sensors have not been widely adopted in healthcare systems or most countries where research is conducted.54 Older adults often prefer smart home technologies tailored to their specific health needs rather than generalized health monitoring.55
To address the monitoring needs of chronic disease patients, we recommend developing “near-body” monitoring technologies for unobtrusive, continuous health tracking and proactive feedback across various scenarios. Reliable evaluations of monitoring devices are essential to ensure accuracy and stability. Attention should focus on precise, non-invasive solutions for patients with multiple chronic conditions, along with establishing standards for “near-body” monitoring systems to ensure consistency and wide applicability. Nurses should collaborate closely with interdisciplinary team members, including physicians, engineers, and data scientists, throughout the technology development process. This collaboration ensures that the resulting technological products effectively integrate nursing practices with innovative solutions. We believe that the active involvement of nurses will enhance the usability, operational efficiency, and clinical effectiveness of monitoring and early warning technologies in real-world healthcare settings.
Given that data collected from wearable devices and non-invasive sensors exhibit wide differences in terms of collection, wear protocols, device properties, and processing protocols. To address the challenges associated with data collection, processing, and sharing, collaborative efforts, such as those led by the WHO, are essential. These efforts should include outlining a minimum set of specifications for wearable devices, engaging industry stakeholders and manufacturers in, establishing a set of required and desirable outcomes from wearable devices, identifying and developing (open source) algorithms for the outcomes, and developing and testing a questionnaire suitable to complement the use of a wearable device within the WHO-STEPS surveillance protocol.56
Precision care for chronic diseases
The integration of medicine and engineering has led to the widespread application of AI in chronic disease care. This section explores the application of AI in personalized chronic disease care, focusing on the application of human-computer interaction technology in enhancing patient experience and acceptance in chronic disease care. It also examines the challenges these technologies encounter in chronic disease management and proposes potential solutions.
AI-driven user-centered care
As “Internet plus” progresses in nursing, AI is increasingly used for personalized care models,26 including dietary57 and exercise recommendations.58,59 For instance, the Alme Health Coach system assists chronic disease patients with meal planning, sleep monitoring, medication reminders, and AI analysis to identify medication non-adherence.60 User-centered design (UCD) is increasingly used in AI-assisted precision care. Chatterjee et al.61 utilized UCD to analyze usage context and gather qualitative data, resulting in the eCoach app, which promotes healthy lifestyles through personalized activity recommendations. This app meets users’ demands for visualized recommendations while considering their cultural context, quality of life, and values. The program is limited to step prediction and visualization, lacking monitoring of physical activity and sleep. The credibility, reliability, and effectiveness of its recommendations are unclear, and its impact on behavior change remains unevaluated, restricting real-world applicability. Bernier et al. developed personalized cardiac rehabilitation plans for patients in remote areas.62 The absence of decision-makers and managers at the organizational level creates challenges for promoting and implementing the program. Involvement from decision-makers is essential in public policy formulation, ensuring strategic support and resource allocation to drive practice changes and enable smooth implementation.63 Korpershoek et al.64 designed a mobile health intervention based on behavior change theory for COPD patients, enabling effective self-management. Limited funding and resources for designing and developing intervention content required the research team to make choices and prioritize. As a result, only the most critical or impactful interventions were selected, and not all potential designs or features could be implemented.
Human-computer interaction optimization
In addition to addressing user needs, integrating medicine, engineering, and AI aims to enhance user acceptance and interaction experience by optimizing human-computer interaction. For example, a cohort study that integrated wearable devices, environmental intelligence technology, open environmental data, and AI-assisted telecare platforms has successfully provided personalized health services to chronic disease patients.65 The system is currently used in Taiwan and Japan.65 Beyond collecting lifestyle data such as sleep, heart rate, and steps, further exploration of data collection technologies for other lifestyle factors is needed. Implementing digital twin models could also provide automated, personalized health promotion recommendations for chronic disease patients. Furthermore, AI-driven chatbots leverage natural language processing and multimodal interactions to enhance self-management acceptance among chronic disease patients.66 There is a lack of comprehensive and detailed technical descriptions of AI-driven chatbots, with most studies largely neglecting their security considerations. Voice-based conversational agents (VCA) could prevent and manage chronic and mental health issues.67 VCA lacks a clear implementation framework, with unresolved questions about its effectiveness and scalability as a supplement or alternative for healthcare practitioners. Current studies focus primarily on short-term feasibility. Long-term studies are needed to demonstrate the technology’s effectiveness and cost-effectiveness compared to conventional methods.
Although AI technology demonstrates immense potential in personalized care, its implementation comes with risks and ethical challenges. The primary issue lies in the “algorithmic black box” problem, where the processes of input, operation, and output are opaque, unknowable, and often unexplainable. To address algorithmic bias, solutions such as designing interpretable algorithms, ensuring algorithm transparency and documentation, and building user-friendly interactive interfaces can be employed.68 On the one hand, interactive visualization tools can allow users to modify input features and observe output changes, thereby helping them understand the model’s behavior. On the other hand, a user feedback mechanism should be established to report inaccurate predictions or offer suggestions for improvement, which will enhance the model’s interpretability and transparency. Moreover, concerns about security, data protection, and regulatory barriers hinder the seamless integration of AI in chronic disease care.53 AI technology must comply with relevant data protection regulations, implement encryption, and de-identification, and establish strict access control mechanisms. Additionally, patient-informed consent should be ensured, and regular security audits and monitoring should be conducted to prevent data leakage and misuse. Finally, as AI technology becomes increasingly integrated into the healthcare field, medical staff may face the risk of technological replacement, particularly in auxiliary diagnosis and decision-making. To ensure the sustainability of AI applications, the role of healthcare professionals should shift from traditional task execution to more supervisory and decision-support responsibilities. Human-centered generative AI design, which enhances human-computer collaboration and complementarity, should be prioritized, along with regular training to improve both clinical skills and technological adaptability, helping medical staff adjust to new workflows.
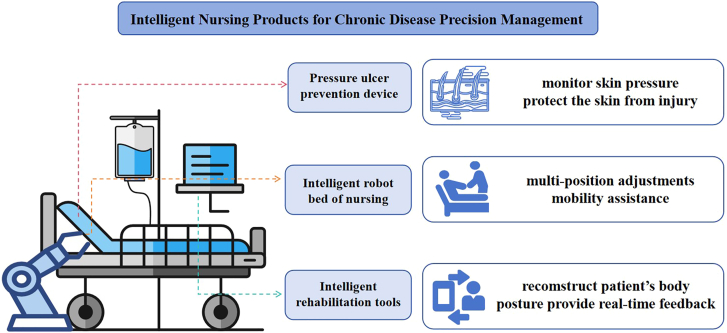
Intelligent nursing products for chronic disease precision management
Previous literature has pointed out that precision nursing represents the main trend in professional and individualized nursing. However, current nursing practices may not fully meet the requirements for individualized and needs-based care.69 The convergence of healthcare and engineering has led to the emergence of intelligent nursing products, which are transforming the healthcare landscape and enabling precise management of chronic disease care. Currently, the main intelligent nursing products include pressure ulcer prevention device, intelligent nursing robot bed, and intelligent rehabilitation tools (Figure 2).
Figure 2.
Intelligent nursing products for chronic disease precision management
Pressure ulcer prevention device
Prevention of pressure ulcers is an important component of the health management of stroke patients, particularly those who are bedridden for extended periods. To address this challenge, a key focus in pressure ulcer care has been the development of products designed to monitor skin pressure and protect the skin from injury. For patients at high risk of developing pressure ulcers, a novel solution has been created in the form of an anti-pressure ulcer airbag pillow. This specially designed, shaped airbag is intended for use in both supine and prone positions,70 offering targeted protection to vulnerable areas of the body. The goal of this innovation is to enhance the comfort and safety of long-term bedridden patients, thereby reducing the risk of pressure ulcers. Furthermore, a wireless wearable system has been developed to monitor human stress and prevent pressure-related injuries. This system employs pressure sensors to collect real-time data on skin pressure, which is then transmitted via Bluetooth to compatible devices. Nurses can access detailed pressure information from various areas of the patient’s body, allowing for timely and informed interventions.71 By integrating precise pressure monitoring with products designed to protect the skin, nurses can more effectively detect and prevent pressure ulcers at an early stage. This proactive approach not only helps identify potential risks before they develop into serious complications but also ensures that patients receive personalized, timely care tailored to their individual needs.
Intelligent nursing robot bed
The emergence of intelligent robot nursing beds represents a significant advancement in the integration of technology within the healthcare sector, particularly in elderly care and for individuals with limited mobility. These intelligent nursing beds are designed to offer a variety of functions, including multi-position adjustments and mobility assistance. These features not only enhance patient comfort but also help reduce the burden on nursing staff and improve overall care quality. Previous studies have led to the development of intelligent nursing beds controlled by sophisticated multi-axis robotic systems. These systems work together to perform essential tasks such as adjusting the bed’s position (lying flat, lifting the back, bending the legs, sitting up), turning the patient, and even providing toileting assistance-functions critical to effective patient care. In addition, some models of intelligent robot nursing beds are equipped to assist with patient movement by integrating with clinical robots. In clinical settings, these robots are equipped with a range of advanced technologies, including speech recognition sensors, infrared cameras, CCD cameras, and laser rangefinders, to enable autonomous navigation.72 They also act as guides for the smart nursing beds, ensuring precise alignment and coordinated movement. Moreover, intelligent robot nursing beds can achieve seamless, automatic docking with intelligent wheelchairs through specialized visual docking methods, the fusion of visual and ultrasonic techniques, visual servo control, and networked systems.73 This combination of robotic technology and intelligent nursing beds is poised to revolutionize patient care by providing a level of precision and customization that was previously unimaginable. By integrating advanced robotics with sophisticated nursing bed systems, it offers more efficient, personalized, and effective healthcare solutions tailored to the specific needs of those with mobility challenges. This fusion not only enhances the quality of care but also ensures that patients receive the precise attention and interventions they require, leading to improved outcomes and overall well-being.
Intelligent rehabilitation tools
People with chronic diseases often experience impairments in multiple systems of the body, including motor dysfunction, cognitive decline, and eating disorders, all of which can severely impact their quality of life and independence. As medical research continues to evolve, virtual reality (VR) has emerged as a promising tool for enhancing cognitive abilities and improving overall rehabilitation outcomes. VR, known for its immersive and interactive capabilities, offers unique opportunities for personalized care and rehabilitation, particularly for individuals dealing with chronic conditions. One notable advancement in this area is the use of VR devices to address motor dysfunction and cognitive impairment in patients with chronic diseases. By utilizing sparse motion signals captured by VR devices, clinicians can reconstruct the patient’s full body posture in real time. These reconstructed postures are then analyzed and compared with established standard postures using sophisticated algorithms and machine-learning techniques.74 The system can detect deviations from optimal posture and, based on these insights, offer real-time, corrective guidance to patients. By using this advanced system, healthcare providers can offer more precise and individualized nursing management.
In recent years, our team has been at the forefront of developing innovative, precision care devices for chronic disease management, aiming to enhance the quality of life and the level of care for patients. Our innovations focus on addressing the unique needs of bedridden individuals, the elderly, and those with chronic conditions, offering greater comfort, attention, and clinical support. One key initiative is the design of devices that assist with physical rehabilitation and support bedside care, particularly benefiting patients with dementia or cognitive impairments. These devices facilitate functional exercises that help maintain limb mobility and strength, even for those who are unable to undergo traditional therapy. Equipped with sensors, the devices track rehabilitation progress and provide real-time feedback for personalized care. By integrating data from smart beds and assistive devices, healthcare professionals gain a comprehensive understanding of the patient’s condition, enabling them to make informed decisions and improve patient outcomes. Through these advancements, we aim to provide more effective, tailored care for those who need it most, ultimately improving both their health and quality of life.
Challenges and prospects
Despite the potential of intelligent care products in chronic disease management, their widespread adoption faces multiple obstacles, including technical barriers and human factors.75 Many wearable devices and sensors are bulky and uncomfortable, which may limit their long-term use, particularly among patients with chronic conditions.21 Future research could focus on developing smaller, lighter, more user-friendly and affordable devices that improve usability, patient compliance and expand the range of their applicability. Furthermore, many existing human-machine integration technologies are designed for specific patient groups or conditions, which can restrict their broader applicability to a wider range of chronic diseases and diverse populations. To address this limitation, future advancements in personalized health management technology may aim to create more adaptable systems that can meet the varying needs of different patient groups. While current robotic systems are effective at performing specific tasks, they struggle to address the dynamic and emotional needs of patients. The inability to provide comprehensive, compassionate care-an essential aspect of effective medical practice-remains a significant barrier. Patient interaction and emotional support are vital in managing chronic diseases, and the lack of flexibility in robotic systems limits their overall effectiveness.
In addition to these technical barriers, there are other human factors that may impede the widespread adoption of intelligent care products. User acceptance of intelligent care products among the users faces significant challenges.76 Their struggle with intricate health data, digital records, and alerts can lead to confusion and disengagement. Cost constraints, the loss of a personal touch, and concerns about privacy further hinder the increase in user acceptance. Thus, the integration of intelligent care products must not only focus on technological advancements but also prioritize maintaining the human element in healthcare to ensure patient satisfaction and effective treatment outcomes. Training nurses on intelligent care products presents another challenge, as it necessitates proficiency in digital interfaces, data analysis, and AI-driven systems.77 Although smart products have been utilized in recent years for case guidance and coursework training for clinical staff, there has been a lack of involvement in how to integrate intelligent care products into clinical practice.78 The transition toward technology-driven nursing requires nurses to become information integrators and health managers, which necessitates technical skills and an understanding of the role of technology in enhancing human care. Consequently, future curricula for nurses must include modules on emerging technologies, data interpretation, and AI ethics. Furthermore, intelligent care products into workflows are challenging. These challenges stem from the need to ensure seamless interoperability with current systems, maintain user-friendliness for healthcare professionals, and adapt to the unique needs of individual patients. Healthcare institutions must ensure compatibility with EHR systems, establish data interoperability protocols, and train staff. They must also anticipate workflow disruptions and develop mitigation strategies. While intelligent care products holds the promise of streamlining documentation processes and elevating patient care, there are notable concerns pertaining to privacy, liability, and the risk of bias.79 Furthermore, some nursing staff are reluctant to introduce intelligent care products into clinical settings due to concerns about being replaced, which makes it even more difficult for these products to integrate into clinical practice.80
In our view, overcoming challenges related to device portability, application diversity, and clinical adoption is crucial for providing more effective, accessible, and customized solutions for chronic disease management. Moreover, AI-driven self-management tools for chronic diseases should incorporate emotional support features to foster a more compassionate, holistic approach to care. Addressing technical issues while adhering to rigorous technology ethics and moral outlooks is the first step to enhance user satisfaction. Ensuring these products respect patient autonomy and adhere to stringent ethical guidelines is paramount. Providing training courses that emphasize ethical considerations in the use of AI and intelligent care technologies, along with supporting digital facilities, is key to achieving comprehensive application. Continuous improvement of relevant training for medical staff and promoting compatibility with clinical facilities should be prioritized, while fostering a culture of ethical practice and responsible innovation within the healthcare sector.
Evaluation of precision care for chronic diseases
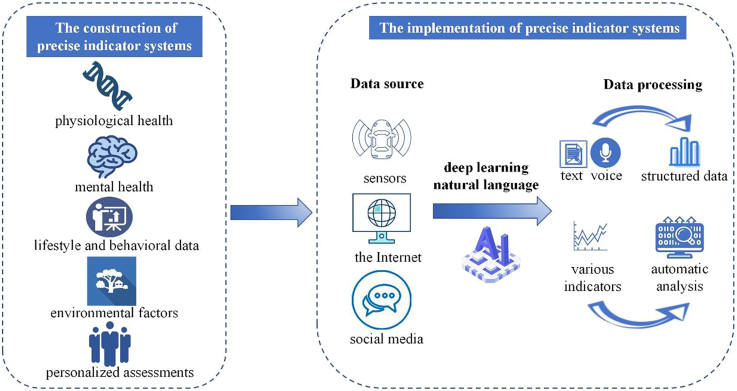
The construction of evaluation indicator systems
The construction of traditional evaluation indicator systems primarily relies on the synthesis of established medical knowledge and clinical practice,81,82 which give rise to challenges including inadequate dynamism, lack of precision, and a singular level of hierarchy driven by empirical experience. The construction of an evaluation indicator system based on language modeling and AI is efficient and intelligent, enabling the processing and analysis of extensive unstructured data to automatically extract valuable information, thereby constructing more intelligent and personalized indicator systems.83,84 The currently constructed evaluation indicator systems mainly focus on physiological health (including genomics), mental health, lifestyle and behavioral data, environmental factors, personalized health assessments and so on. When assessing the impact of long-term exercise training on physical function and cardiopulmonary function in adults with chronic disease, key indicators such as cardiopulmonary fitness and submaximal gait were included.85 Twenty-seven genome-wide loci associated with white matter hyperintensity volume, an important imaging marker of cerebral small vessel disease were identified, in a cohort of 50,970 elderly individuals.86 Furthermore, by integrating wearable devices, open environmental data, indoor air quality sensors, location-based smartphone applications, and more, sustainable and real-time monitoring of indicators such as lifestyle and environmental factors can be achieved.87 In summary, through the application of AI technology, a comprehensive and precise construction of the required indicators can be achieved, thereby forming a comprehensive evaluation indicator system that is conducive to the full-cycle assessment of various chronic diseases.
AI-driven evaluation indicator systems
Evaluation of interventions using traditional evaluation indicator systems yields relatively limited or monotonous results that are highly subjective and unable to meet the demands of increasingly complex health management.85 At present, a new type of evaluation indicator system has been gradually applied, data from different channels can be processed and analyzed with the help of the fusion of big data and deep learning, natural language processing technology and other means. For instance, in the field of mental health, the use of AI and natural language technology has enabled the mining of behavioral or mental health insights from information on the Internet or from personal social media interactions.88 AI and natural language processing technology can transform user-input text or voice data into structural data, and automatically monitor and analyze changes in relevant indicators, thus enhancing the comprehensiveness and flexibility of the evaluation indicator system.89 Cardiac magnetic resonance imaging (CMR) is the gold standard for cardiac function assessment and plays a crucial role in diagnosing cardiovascular disease (CVD). Previous research has demonstrated the capability of AI-empowered CMR to detect previously unrecognized features, substantially enhancing the efficiency and scalability of cardiac function assessment, thereby facilitating improvements in the screening and diagnosis of CVD.90 However, all of the above evaluation indicator systems were only constructed at the time of construction, and large-scale, multi-center validation was not implemented. In the real world, evaluation indicator systems remain challenging in terms of the difficulty of quantifying multi-dimensional indicators, personalized differences, and the timeliness of implementation and feedback.
Challenges and prospects
As shown in Figure 3, scholars are currently working on the use of AI and natural language technology to construct evaluation indicator systems to achieve scientific evaluation. Despite the remarkable advantages of AI technologies in data processing and pattern recognition, practical challenges such as data quality issues, data missingness, or biases in processed datasets persist, casting doubts on their reliability and accuracy in nursing decision-making.91 Hence, there is a pressing need to ensure their stability and precision in practical applications. During the data collection process, rigorous quality control measures should be implemented, encompassing the selection of data sources, the accuracy of data entry, and regular data audit procedures. In the data preprocessing phase, outlier detection and handling, identification and merging of duplicate data, and imputation of missing values are crucial steps to guarantee data accuracy and reliability. It is essential to identify potential bias types within datasets, such as selection bias, measurement bias, and classification bias, and to mitigate these biases through methods such as weighting adjustments, stratified sampling, or Bayesian approaches, thereby enhancing data representativeness. The handling of patients’ sensitive information by AI poses ethical and privacy risks, including data breaches and algorithmic biases, which may trigger trust crises.92 Consequently, stringent data protection policies must be formulated, encompassing data privacy safeguards, data usage permissions, and data access controls. The establishment of standardized data sharing agreements is vital, and techniques such as encryption and anonymization can also be employed to safeguard data security. Additionally, the inadequate integration of the evaluation indicator system with clinical practice is also a challenge that must be addressed.93 In the future, it is necessary to work on the systematic integration of a variety of evaluation indicator systems and to practice them in the clinic in order to construct a scientific indicator system that can be applied to the clinic (Figure 3).
Figure 3.
Empowerment of AI in the construction and implementation of precise indicator systems
Conclusion
The integration of AI with the medical-industrial sector has revolutionized the healthcare landscape, particularly in the precision management of chronic diseases. AI technology and cross-industry collaboration are increasingly being applied in symptom monitoring, early disease detection, development of tailored management programs, intelligent care products, and evaluation of health management outcomes. This shift has moved chronic disease management from a generic to a more personalized and refined approach. However, this integration presents unique challenges, including resistance to technological shifts, constrained clinical applicability, inadequate fulfillment of dynamic and emotional patient needs, concerns over data accuracy and user privacy, and difficulties in seamlessly integrating with clinical practice. To surmount these hurdles and harness the full potential of AI, interdisciplinary collaboration holds the key. To this end, we propose the establishment of interdisciplinary communication platforms that bring together nursing scholars, engineers, clinicians, and other stakeholders to engage in discourse and jointly explore the synergies between AI and nursing practice. Furthermore, we encourage and support the formation of interdisciplinary teams through collaborative research project proposals, fostering deep collaboration within the nexus of nursing and medical engineering. Lastly, to uphold the ethical and effective deployment of AI in healthcare, we will actively advocate for policy reforms. This includes urging relevant bodies to develop more robust regulations and establish ethical review mechanisms to ensure that the development and application of AI technologies align with ethical principles. Through the implementation of these strategies, we are confident that we can amplify the influence of the nursing and medical engineering integration, propel the widespread adoption of AI technologies in healthcare, and ultimately deliver more precise and high-quality nursing services to patients with chronic conditions.
Acknowledgments
This study was funded by the National Natural Science Foundation of China (Grant No. 72174012) and the National Natural Science Foundation of China (Grant No. 72204122).
Author contributions
Conceptualization, H.Y.S. and Y.M.S.; writing–original draft, C.Q.D., Y.J., Z.M.F., Y.Q., T.Y., and Y.Y.; writing–review and editing, H.Y.S. and Y.M.S.; funding acquisition, H.Y.S. and Y.J.; supervision, H.Y.S. and Y.M.S. All authors contributed to manuscript revision and approved the submitted version.
Declaration of interests
The authors declare that they have no conflict of interest.
Contributor Information
Yumei Sun, Email: sym8022@163.com.
Hongyu Sun, Email: sunhongyu@bjmu.edu.cn.
References
- 1.Forbes A., While A. The nursing contribution to chronic disease management: a discussion paper. Int. J. Nurs. Stud. 2009;46:119–130. doi: 10.1016/j.ijnurstu.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Grady P.A., Gough L.L. Nursing Science: Claiming the Future. J. Nurs. Scholarsh. 2015;47:512–521. doi: 10.1111/jnu.12170. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Noncommunicable diseases. 2024. (Accessed at https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
- 4.Ferrari A.J., Santomauro D.F., Aali A., Abate Y.H., Abbafati C., Abbastabar H., Abd ElHafeez S., Abdelmasseh M., Abd-Elsalam S., Abdollahi A., Abdullahi A. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet (London, England) 2024;403:2133–2161. doi: 10.1016/S0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Global Action Plan for the Prevention and Control of NCDs 2013–2020. 2019. (Accessed at https://www.who.int/nmh/events/ncd_action_plan/en/.
- 6.Wagner C., Carmeli C., Jackisch J., Kivimäki M., van der Linden B.W.A., Cullati S., Chiolero A. Life course epidemiology and public health. Lancet Public Health. 2024;9:e261–e269. doi: 10.1016/S2468-2667(24)00018-5. [DOI] [PubMed] [Google Scholar]
- 7.Organization WH. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. 2020.
- 8.Berry-Millett R., Bodenheimer T.S. Care management of patients with complex health care needs. Synth. Proj. Res. Synth. Rep. 2009:52372. [PubMed] [Google Scholar]
- 9.Li T., Feng H., Bandugula V., Ding Y. Designing a Consumer-centric Care Management Program by Prioritizing Interventions Using Deep Learning Causal Inference. AMIA Jt. Summits Transl. Sci. Proc. 2024;2024:584–592. [PMC free article] [PubMed] [Google Scholar]
- 10.Prabhakaran D., Jeemon P., Roy A. Cardiovascular Diseases in India: Current Epidemiology and Future Directions. Circulation. 2016;133:1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 11.Singh A.P., Saxena R., Saxena S., Maurya N.K. Artificial Intelligence Revolution in Healthcare: Transforming Diagnosis, Treatment, and Patient Care. Asian J. Adv. Res. 2024;7:241–263. [Google Scholar]
- 12.Barr N., Vania D., Randall G., Mulvale G. Impact of information and communication technology on interprofessional collaboration for chronic disease management: a systematic review. J. Health Serv. Res. Policy. 2017;22:250–257. doi: 10.1177/1355819617714292. [DOI] [PubMed] [Google Scholar]
- 13.Swartwout E., Deyo P., El-Zein A. Effectiveness of technology use for engaging community dwelling adults with chronic disease in self-care behavior management in health care: a systematic review protocol. JBI Database System Rev. Implement. Rep. 2016;14:87–95. doi: 10.11124/JBISRIR-2016-002535. [DOI] [PubMed] [Google Scholar]
- 14.Subramanian M., Wojtusciszyn A., Favre L., Boughorbel S., Shan J., Letaief K.B., Pitteloud N., Chouchane L. Precision medicine in the era of artificial intelligence: implications in chronic disease management. J. Transl. Med. 2020;18:472. doi: 10.1186/s12967-020-02658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xie Y., Lu L., Gao F., He S.J., Zhao H.J., Fang Y., Yang J.M., An Y., Ye Z.W., Dong Z. Integration of artificial intelligence, blockchain, and wearable technology for chronic disease management: a new paradigm in smart healthcare. Curr. Med. Sci. 2021;41:1123–1133. doi: 10.1007/s11596-021-2485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Javaid M., Haleem A., Singh R.P., Suman R. Sustaining the healthcare systems through the conceptual of biomedical engineering: A study with recent and future potentials. Biomed. Technol. 2023;1:39–47. [Google Scholar]
- 17.Jeong I.C., Bychkov D., Searson P.C. Wearable devices for precision medicine and health state monitoring. IEEE Trans. Biomed. Eng. 2019;66:1242–1258. doi: 10.1109/TBME.2018.2871638. [DOI] [PubMed] [Google Scholar]
- 18.Zaki H. Synergies in Healthcare: Integrating Biomedical Engineering, Medical Devices, and Artificial Intelligence. EasyChair. 2024 doi: 10.13140/RG.2.2.15608.21760. Preprint at. [DOI] [Google Scholar]
- 19.Islam R., Sultana A., Islam M.R. A comprehensive review for chronic disease prediction using machine learning algorithms. J. Electr. Syst. Inf. Technol. 2024;11:27. [Google Scholar]
- 20.Alanazi R. Identification and prediction of chronic diseases using machine learning approach. J. Healthc. Eng. 2022;2022 doi: 10.1155/2022/2826127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yin R., Wang D., Zhao S., Lou Z., Shen G. Wearable sensors-enabled human-machine interaction systems: from design to application. Adv. Funct. Mater. 2021;31 [Google Scholar]
- 22.Esmaeilzadeh P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: A perspective for healthcare organizations. Artif. Intell. Med. 2024;151 doi: 10.1016/j.artmed.2024.102861. [DOI] [PubMed] [Google Scholar]
- 23.Price W.N., 2nd, Cohen I.G. Privacy in the age of medical big data. Nat. Med. 2019;25:37–43. doi: 10.1038/s41591-018-0272-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwang A.S., Tannou T., Nanthakumar J., Cao W., Chu C.H., Zeytinoglu Atici C., Scane K., Yu A., Tsang W., Chan J., Lea P. Co-creating Humanistic AI AgeTech to Support Dynamic Care Ecosystems: A Preliminary Guiding Model. Gerontologist. 2024;65 doi: 10.1093/geront/gnae093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coghlan S. Robots and the Possibility of Humanistic Care. Int. J. Soc. Robot. 2022;14:2095–2108. doi: 10.1007/s12369-021-00804-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Gerich H., Moen H., Block L.J., Chu C.H., DeForest H., Hobensack M., Michalowski M., Mitchell J., Nibber R., Olalia M.A., et al. Artificial Intelligence -based technologies in nursing: A scoping literature review of the evidence. Int. J. Nurs. Stud. 2022;127 doi: 10.1016/j.ijnurstu.2021.104153. [DOI] [PubMed] [Google Scholar]
- 27.Ferruz N., Zitnik M., Oudeyer P.-Y., Hine E., Sengupta N., Shi Y., Mincu D., Mann S.P., Das P., Stella F. Anniversary AI reflections. Nat. Mach. Intell. 2024;6:6–12. [Google Scholar]
- 28.Zheng N.S., Annis J., Master H., Han L., Gleichauf K., Ching J.H., Nasser M., Coleman P., Desine S., Ruderfer D.M., et al. Sleep patterns and risk of chronic disease as measured by long-term monitoring with commercial wearable devices in the All of Us Research Program. Nat. Med. 2024;30:2648–2656. doi: 10.1038/s41591-024-03155-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang G., Pang G., Pang Z., Gu Y., Mantysalo M., Yang H. Non-Invasive Flexible and Stretchable Wearable Sensors With Nano-Based Enhancement for Chronic Disease Care. IEEE Rev. Biomed. Eng. 2019;12:34–71. doi: 10.1109/RBME.2018.2887301. [DOI] [PubMed] [Google Scholar]
- 30.Xie Y., Lu L., Gao F., He S.J., Zhao H.J., Fang Y., Yang J.M., An Y., Ye Z.W., Dong Z. Integration of Artificial Intelligence, Blockchain, and Wearable Technology for Chronic Disease Management: A New Paradigm in Smart Healthcare. Curr. Med. Sci. 2021;41:1123–1133. doi: 10.1007/s11596-021-2485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu C.T., Li G.H., Huang C.T., Cheng Y.C., Chen C.H., Chien J.Y., Kuo P.H., Kuo L.C., Lai F. Acute Exacerbation of a Chronic Obstructive Pulmonary Disease Prediction System Using Wearable Device Data, Machine Learning, and Deep Learning: Development and Cohort Study. JMIR Mhealth Uhealth. 2021;9 doi: 10.2196/22591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma A., Badea M., Tiwari S., Marty J.L. Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring. Molecules. 2021;26 doi: 10.3390/molecules26030748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah A.J., Althobiani M.A., Saigal A., Ogbonnaya C.E., Hurst J.R., Mandal S. Wearable technology interventions in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. NPJ Digit. Med. 2023;6:222. doi: 10.1038/s41746-023-00962-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mattison G., Canfell O., Forrester D., Dobbins C., Smith D., Töyräs J., Sullivan C. The Influence of Wearables on Health Care Outcomes in Chronic Disease: Systematic Review. J. Med. Internet Res. 2022;24 doi: 10.2196/36690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jafleh E.A., Alnaqbi F.A., Almaeeni H.A., Faqeeh S., Alzaabi M.A., Al Zaman K. The Role of Wearable Devices in Chronic Disease Monitoring and Patient Care: A Comprehensive Review. Cureus. 2024;16 doi: 10.7759/cureus.68921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alvarez P., Sianis A., Brown J., Ali A., Briasoulis A. Chronic disease management in heart failure: focus on telemedicine and remote monitoring. Rev. Cardiovasc. Med. 2021;22:403–413. doi: 10.31083/j.rcm2202046. [DOI] [PubMed] [Google Scholar]
- 37.Faro J.M., Yue K.L., Singh A., Soni A., Ding E.Y., Shi Q., McManus D.D. Wearable device use and technology preferences in cancer survivors with or at risk for atrial fibrillation. Cardiovasc. Digit. Health J. 2022;3:S23–S27. doi: 10.1016/j.cvdhj.2022.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teo N.R., Siew L.E.D., Ang W.H.D., Lau Y. Wearable-Technology-Assisted Interventions for Breast-Cancer Survivors: A Meta-Analysis and Meta-Regression. Semin. Oncol. Nurs. 2023;39 doi: 10.1016/j.soncn.2023.151403. [DOI] [PubMed] [Google Scholar]
- 39.Liu C., Zhang X., Zhao L., Liu F., Chen X., Yao Y., Li J. Signal quality assessment and lightweight QRS detection for wearable ECG SmartVest system. IEEE Internet Things J. 2019;6:1363–1374. [Google Scholar]
- 40.Beach C., Krachunov S., Pope J., Fafoutis X., Piechocki R.J., Craddock I., Casson A.J. An ultra low power personalizable wrist worn ECG monitor integrated with IoT infrastructure. IEEE Access. 2018;6:44010–44021. [Google Scholar]
- 41.Liu Y., Yu Q., Ye L., Yang L., Cui Y. A wearable, minimally-invasive, fully electrochemically-controlled feedback minisystem for diabetes management. Lab Chip. 2023;23:421–436. doi: 10.1039/d2lc00797e. [DOI] [PubMed] [Google Scholar]
- 42.Segura Anaya L.H., Alsadoon A., Costadopoulos N., Prasad P.W.C. Ethical Implications of User Perceptions of Wearable Devices. Sci. Eng. Ethics. 2018;24:1–28. doi: 10.1007/s11948-017-9872-8. [DOI] [PubMed] [Google Scholar]
- 43.Charlton P.H., Birrenkott D.A., Bonnici T., Pimentel M.A.F., Johnson A.E.W., Alastruey J., Tarassenko L., Watkinson P.J., Beale R., Clifton D.A. Breathing rate estimation from the electrocardiogram and photoplethysmogram: A review. IEEE Rev. Biomed. Eng. 2018;11:2–20. doi: 10.1109/RBME.2017.2763681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin X., Zhang T., Cao J., Wen H., Fei T., Liu S., Wang R., Ren H., Zhao H. Flexible piezoresistive sensors based on conducting polymer-coated fabric applied to human physiological signals monitoring. J. Bionic Eng. 2020;17:55–63. [Google Scholar]
- 45.Kotriwar Y., Kachhara S., Harikrishnan K., Ambika G. Higher order spectral analysis of ECG signals. arXiv. 2018 doi: 10.48550/arXiv.1809.0845. Preprint at. [DOI] [Google Scholar]
- 46.Lu L., Zhang J., Xie Y., Gao F., Xu S., Wu X., Ye Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth. 2020;8 doi: 10.2196/18907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sullivan C., Staib A., Ayre S., Daly M., Collins R., Draheim M., Ashby R. Pioneering digital disruption: Australia's first integrated digital tertiary hospital. Med. J. Aust. 2016;205:386–389. doi: 10.5694/mja16.00476. [DOI] [PubMed] [Google Scholar]
- 48.Goldfine C.E., Oshim F.T., Carreiro S.P., Chapman B.P., Ganesan D., Rahman T. Respiratory Rate Monitoring in Clinical Environments with a Contactless Ultra-Wideband Impulse Radar-based Sensor System. Proc. Annu. Hawaii Int. Conf. Syst. Sci. 2020;2020:3366–3375. [PMC free article] [PubMed] [Google Scholar]
- 49.Adachi Y., Edo Y., Ogawa R., Tomizawa R., Iwai Y., Okumura T. Noncontact Blood Pressure Monitoring Technology using Facial Photoplethysmograms. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2019;2019:2411–2415. doi: 10.1109/EMBC.2019.8856439. [DOI] [PubMed] [Google Scholar]
- 50.Ohata T., Ishibashi K., Sun G. Non-Contact Blood Pressure Measurement Scheme Using Doppler Radar. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2019;2019:778–781. doi: 10.1109/EMBC.2019.8857056. [DOI] [PubMed] [Google Scholar]
- 51.Luo H., Yang D., Barszczyk A., Vempala N., Wei J., Wu S.J., Zheng P.P., Fu G., Lee K., Feng Z.P. Smartphone-Based Blood Pressure Measurement Using Transdermal Optical Imaging Technology. Circ. Cardiovasc. Imaging. 2019;12 doi: 10.1161/CIRCIMAGING.119.008857. [DOI] [PubMed] [Google Scholar]
- 52.Fritz R., Wuestney K., Dermody G., Cook D.J. Nurse-in-the-loop smart home detection of health events associated with diagnosed chronic conditions: A case-event series. Int. J. Nurs. Stud. Adv. 2022;4 doi: 10.1016/j.ijnsa.2022.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Minghui Y., Hu Y., Lu Z. How do nurses work in chronic management in the age of artificial intelligence? development and future prospects. Digit. Health. 2023;9 doi: 10.1177/20552076231221057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dermody G., Fritz R., Glass C., Dunham M., Whitehead L. Factors influencing community-dwelling older adults' readiness to adopt smart home technology: A qualitative exploratory study. J. Adv. Nurs. 2021;77:4847–4861. doi: 10.1111/jan.14996. [DOI] [PubMed] [Google Scholar]
- 55.Choi Y.K., Thompson H.J., Demiris G. Internet-of-Things Smart Home Technology to Support Aging-in-Place: Older Adults' Perceptions and Attitudes. J. Gerontol. Nurs. 2021;47:15–21. doi: 10.3928/00989134-20210310-03. [DOI] [PubMed] [Google Scholar]
- 56.Physical activity measurement and surveillance in adults: report of a scoping and planning meeting, 27-28 November 2023. 2023.https://www.who.int/publications/i/item/9789240095557.
- 57.Berube L.T., Popp C.J., Curran M., Hu L., Pompeii M.L., Barua S., Bernstein E., Salcedo V., Li H., St-Jules D.E., et al. Diabetes Telemedicine Mediterranean Diet (DiaTeleMed) Study: study protocol for a fully remote randomized clinical trial evaluating personalized dietary management in individuals with type 2 diabetes. Trials. 2024;25:506. doi: 10.1186/s13063-024-08337-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li Y., Li X. The Artificial Intelligence System for the Generation of Sports Education Guidance Model and Physical Fitness Evaluation Under Deep Learning. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.917053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fabbrizio A., Fucarino A., Cantoia M., De Giorgio A., Garrido N.D., Iuliano E., Reis V.M., Sausa M., Vilaça-Alves J., Zimatore G., et al. Smart Devices for Health and Wellness Applied to Tele-Exercise: An Overview of New Trends and Technologies Such as IoT and AI. Health Care. 2023;11 doi: 10.3390/healthcare11121805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Huang C.-Y., Ting Y.-H. A Chronic Disease Diet Recommendation System Based on Domain Ontology and Decision Tree. J. Adv. Comput. Intell. Intell. Inf. 2017;21:474–482. doi: 10.20965/jaciii.2017.p0474. [DOI] [Google Scholar]
- 61.Chatterjee A., Prinz A., Gerdes M., Martinez S., Pahari N., Meena Y.K. ProHealth eCoach: user-centered design and development of an eCoach app to promote healthy lifestyle with personalized activity recommendations. BMC Health Serv. Res. 2022;22:1120. doi: 10.1186/s12913-022-08441-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bernier J., Breton M., Poitras M.E. Co-designing a cardiac rehabilitation program with knowledge users for patients with cardiovascular disease from a remote area. BMC Health Serv. Res. 2024;24:869. doi: 10.1186/s12913-024-11321-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Steen M., Manschot M., De Koning N. Benefits of co-design in service design projects. Int. J. Des. 2011;5:53–60. [Google Scholar]
- 64.Korpershoek Y.J.G., Hermsen S., Schoonhoven L., Schuurmans M.J., Trappenburg J.C.A. User-Centered Design of a Mobile Health Intervention to Enhance Exacerbation-Related Self-Management in Patients With Chronic Obstructive Pulmonary Disease (Copilot): Mixed Methods Study. J. Med. Internet Res. 2020;22 doi: 10.2196/15449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu C.T., Wang S.M., Su Y.E., Hsieh T.T., Chen P.C., Cheng Y.C., Tseng T.W., Chang W.S., Su C.S., Kuo L.C., et al. A Precision Health Service for Chronic Diseases: Development and Cohort Study Using Wearable Device, Machine Learning, and Deep Learning. IEEE J. Transl. Eng. Health Med. 2022;10 doi: 10.1109/JTEHM.2022.3207825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kurniawan M.H., Handiyani H., Nuraini T., Hariyati R.T.S., Sutrisno S. A systematic review of artificial intelligence-powered (AI-powered) chatbot intervention for managing chronic illness. Ann. Med. 2024;56 doi: 10.1080/07853890.2024.2302980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bérubé C., Schachner T., Keller R., Fleisch E., V Wangenheim F., Barata F., Kowatsch T. Voice-Based Conversational Agents for the Prevention and Management of Chronic and Mental Health Conditions: Systematic Literature Review. J. Med. Internet Res. 2021;23 doi: 10.2196/25933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Coglianese C., Lehr D. Transparency and algorithmic governance. Adm. Law Rev. 2019;71:1–56. [Google Scholar]
- 69.Shun S.C. Precision Nursing: The Mainstream Trend in Professional Individualized Care. J. Nurs. Res. 2023;31:e262. doi: 10.1097/jnr.0000000000000552. [DOI] [PubMed] [Google Scholar]
- 70.Cao Y., Wang C., Huang J., Wang W., Mao X., Wang K. Study on anti-pressure ulcer heterotypic air-cell pillow pad and human external pressure sensing method. J. Mach. Des. 2024;41:158–163. [Google Scholar]
- 71.Park H., Kim K., Kweon S.J., Gul O., Choi J., Oh Y.S., Park I., Je M. A Wireless and Wearable Body-Pressure-Monitoring System for the Prevention of Pressure-Induced Skin Injuries. IEEE Trans. Biomed. Circuits Syst. 2023;17:889–899. doi: 10.1109/TBCAS.2023.3288126. [DOI] [PubMed] [Google Scholar]
- 72.Nguyen H.H., Nguyen T.N., Clout R., Gibson A., Nguyen H.T. Development of an assistive patient mobile system for hospital environments. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2013;2013:2491–2494. doi: 10.1109/EMBC.2013.6610045. [DOI] [PubMed] [Google Scholar]
- 73.Lei X., Tang C., Tang X. High-precision docking of wheelchair/beds through LIDAR and visual information. Front. Bioeng. Biotechnol. 2024;12 doi: 10.3389/fbioe.2024.1446512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dai X., Zhang Z., Zhao S., Liu X., Chen X. Full-body pose reconstruction and correction in virtual reality for rehabilitation training. Front. Neurosci. 2024;18 doi: 10.3389/fnins.2024.1388742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Barchielli C., Marullo C., Bonciani M., Vainieri M. Nurses and the acceptance of innovations in technology-intensive contexts: the need for tailored management strategies. BMC Health Serv. Res. 2021;21:639. doi: 10.1186/s12913-021-06628-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang B., Zhang R., Wang Y. Mechanism Influencing Older People's Willingness to Use Intelligent Aged-Care Products. Healthcare. 2021;9 doi: 10.3390/healthcare9070864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yadav S. Embracing Artificial Intelligence: Revolutionizing Nursing Documentation for a Better Future. Cureus. 2024;16 doi: 10.7759/cureus.57725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ogundiya O., Rahman T.J., Valnarov-Boulter I., Young T.M. Looking Back on Digital Medical Education Over the Last 25 Years and Looking to the Future: Narrative Review. J. Med. Internet Res. 2024;26 doi: 10.2196/60312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rony M.K.K., Parvin M.R., Ferdousi S. Advancing nursing practice with artificial intelligence: Enhancing preparedness for the future. Nurs. Open. 2024;11:1–9. doi: 10.1002/nop2.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ramadan O.M.E., Alruwaili M.M., Alruwaili A.N., Elsehrawy M.G., Alanazi S. Facilitators and barriers to AI adoption in nursing practice: a qualitative study of registered nurses' perspectives. BMC Nurs. 2024;23:891. doi: 10.1186/s12912-024-02571-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lu J., Sun X., Zhang Y. Establishment and analysis of quality index system for pediatric tumor nursing. Technol. Health Care. 2024;32:4343–4351. doi: 10.3233/THC-240252. [DOI] [PubMed] [Google Scholar]
- 82.Zou X., Li S., Fang M., Hu M., Bian Y., Ling J., Yu S., Jing L., Li D., Huang J. Acute Physiology and Chronic Health Evaluation II Score as a Predictor of Hospital Mortality in Patients of Coronavirus Disease 2019. Crit. Care Med. 2020;48:e657–e665. doi: 10.1097/CCM.0000000000004411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rossettini G., Cook C., Palese A., Pillastrini P., Turolla A. Pros and Cons of Using Artificial Intelligence Chatbots for Musculoskeletal Rehabilitation Management. J. Orthop. Sports Phys. Ther. 2023;53:728–734. doi: 10.2519/jospt.2023.12000. [DOI] [PubMed] [Google Scholar]
- 84.Valero-Ramon Z., Fernandez-Llatas C., Valdivieso B., Traver V. Dynamic Models Supporting Personalised Chronic Disease Management through Healthcare Sensors with Interactive Process Mining. Sensors. 2020;20 doi: 10.3390/s20185330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Weiner D.E., Liu C.K., Miao S., Fielding R., Katzel L.I., Giffuni J., Well A., Seliger S.L. Effect of Long-term Exercise Training on Physical Performance and Cardiorespiratory Function in Adults With CKD: A Randomized Controlled Trial. Am. J. Kidney Dis. 2023;81:59–66. doi: 10.1053/j.ajkd.2022.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sargurupremraj M., Suzuki H., Jian X., Sarnowski C., Evans T.E., Bis J.C., Eiriksdottir G., Sakaue S., Terzikhan N., Habes M., et al. Cerebral small vessel disease genomics and its implications across the lifespan. Nat. Commun. 2020;11:6285. doi: 10.1038/s41467-020-19111-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Husnain A., Hussain H.K., Shahroz H.M., Ali M., Hayat Y. A Precision Health Initiative for Chronic Conditions: Design and Cohort Study Utilizing Wearable Technology, Machine Learning, and Deep Learning. Int. J. Adv. Eng. Technol. Innov. 2024;1:118–139. [Google Scholar]
- 88.D'Alfonso S. AI in mental health. Curr. Opin. Psychol. 2020;36:112–117. doi: 10.1016/j.copsyc.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 89.Omiye J.A., Gui H., Rezaei S.J., Zou J., Daneshjou R. Large Language Models in Medicine: The Potentials and Pitfalls : A Narrative Review. Ann. Intern. Med. 2024;177:210–220. doi: 10.7326/M23-2772. [DOI] [PubMed] [Google Scholar]
- 90.Wang Y.R.J., Yang K., Wen Y., Wang P., Hu Y., Lai Y., Wang Y., Zhao K., Tang S., Zhang A., et al. Screening and diagnosis of cardiovascular disease using artificial intelligence-enabled cardiac magnetic resonance imaging. Nat. Med. 2024;30:1471–1480. doi: 10.1038/s41591-024-02971-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Goessinger E.V., Gottfrois P., Mueller A.M., Cerminara S.E., Navarini A.A. Image-Based Artificial Intelligence in Psoriasis Assessment: The Beginning of a New Diagnostic Era? Am. J. Clin. Dermatol. 2024;25:861–872. doi: 10.1007/s40257-024-00883-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gonzalez-Garcia A., Pérez-González S., Benavides C., Pinto-Carral A., Quiroga-Sánchez E., Marqués-Sánchez P. Impact of Artificial Intelligence–Based Technology on Nurse Management: A Systematic Review. J. Nurs. Manag. 2024;2024 [Google Scholar]
- 93.Plana D., Shung D.L., Grimshaw A.A., Saraf A., Sung J.J.Y., Kann B.H. Randomized Clinical Trials of Machine Learning Interventions in Health Care: A Systematic Review. JAMA Netw. Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.33946. [DOI] [PMC free article] [PubMed] [Google Scholar]