Abstract
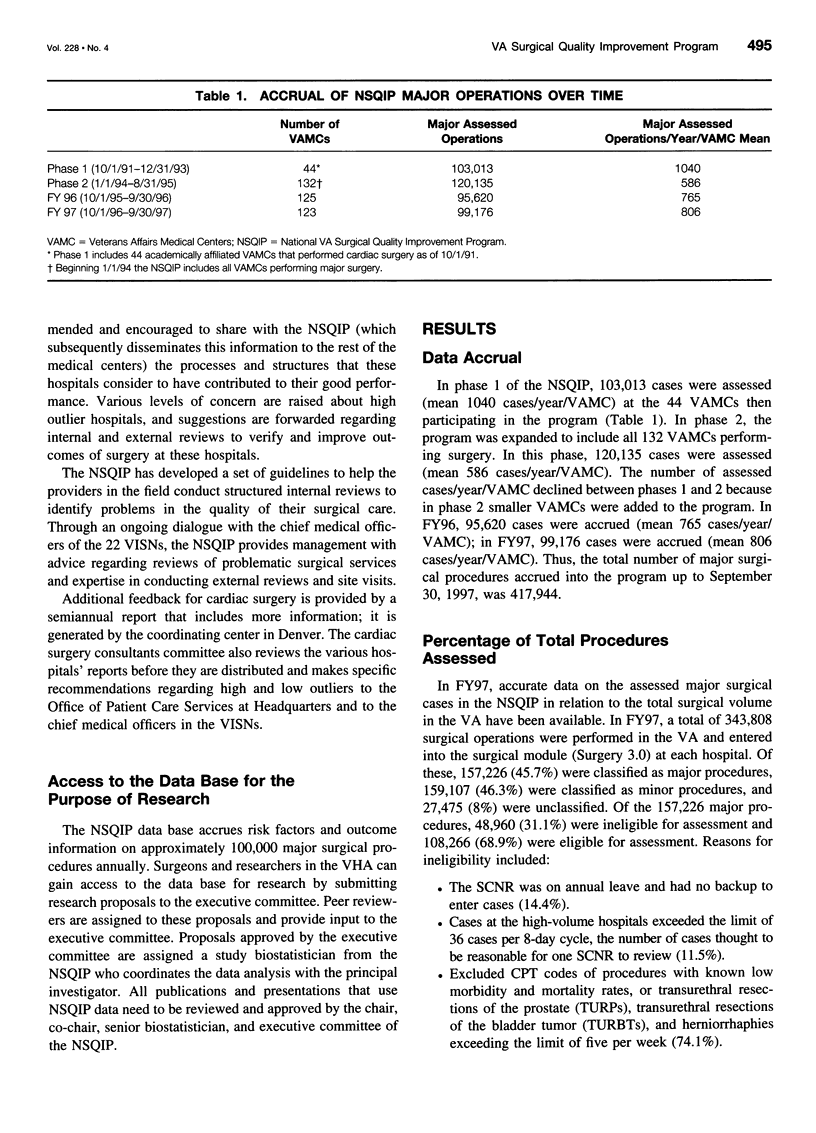
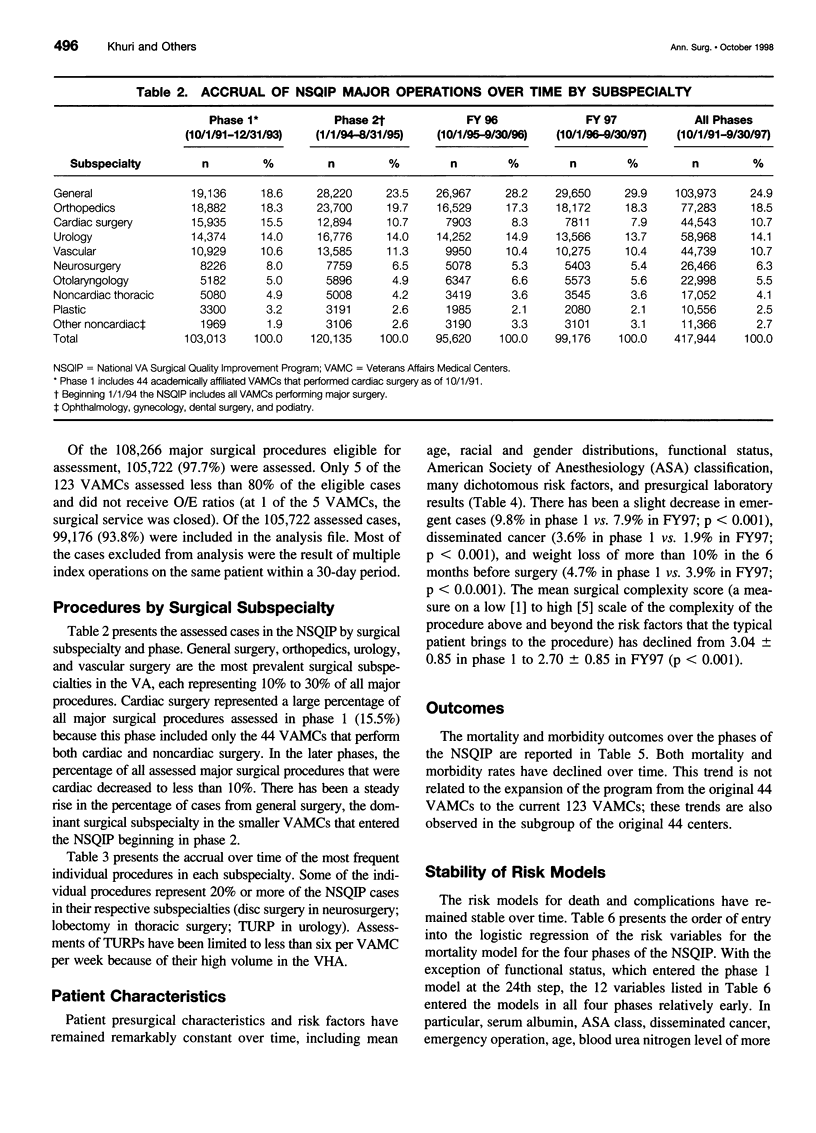
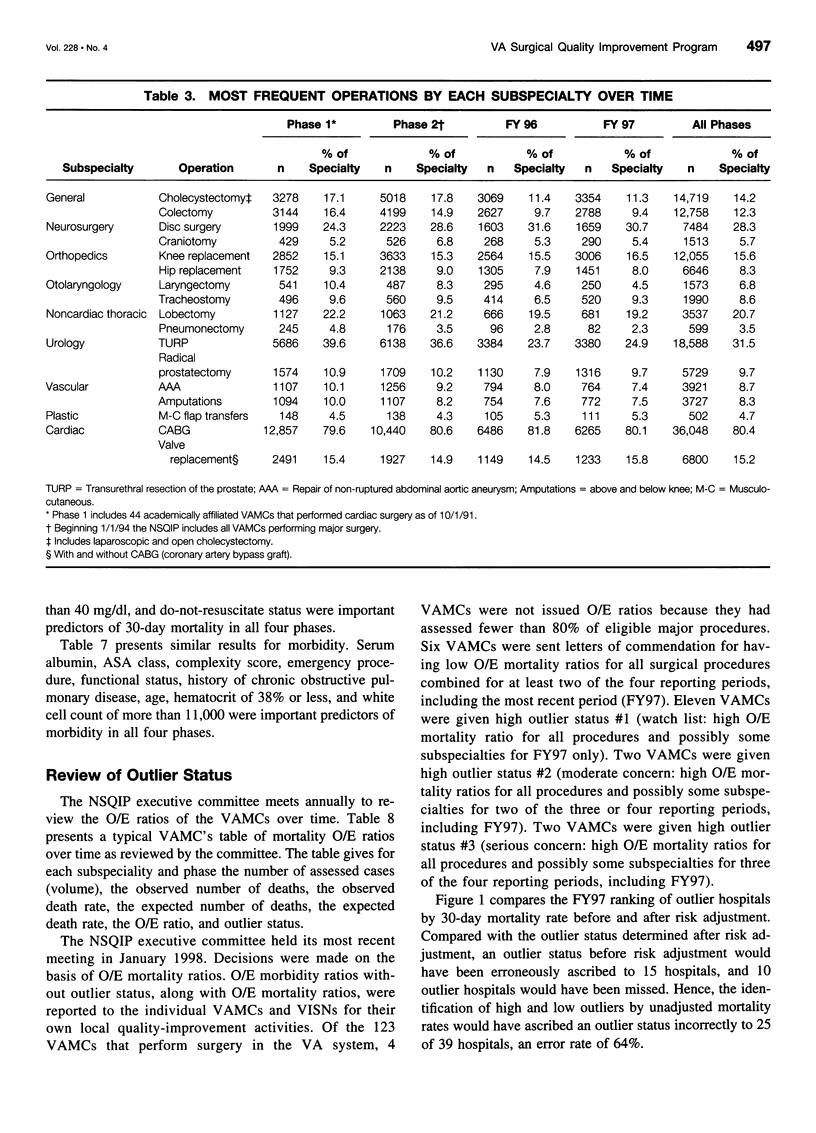
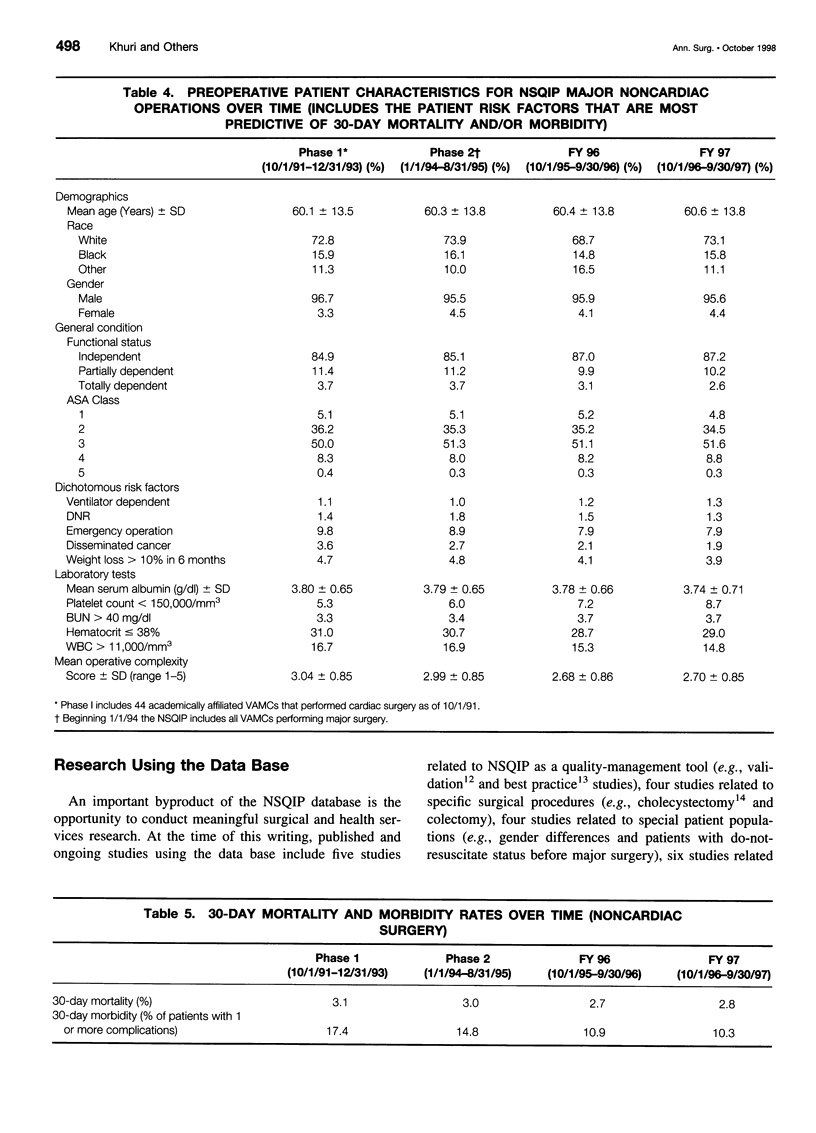
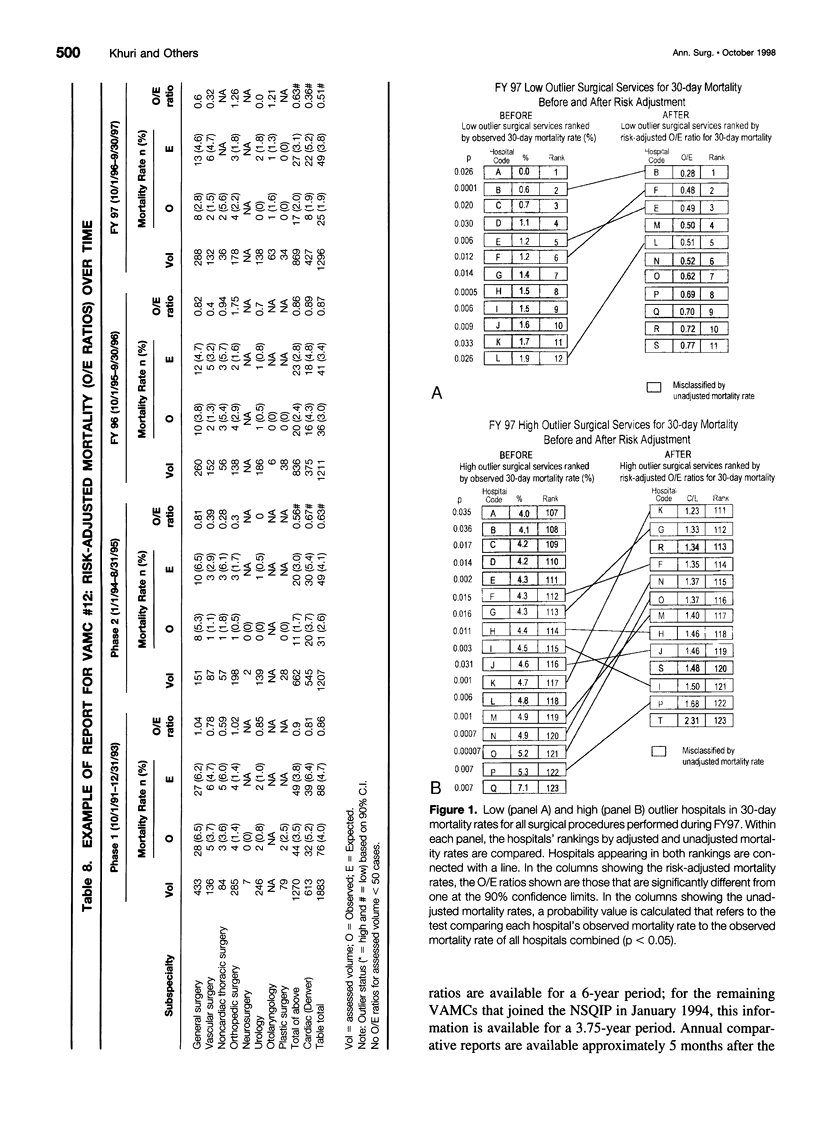
OBJECTIVE: To provide reliable risk-adjusted morbidity and mortality rates after major surgery to the 123 Veterans Affairs Medical Centers (VAMCs) performing major surgery, and to use risk-adjusted outcomes in the monitoring and improvement of the quality of surgical care to all veterans. SUMMARY BACKGROUND DATA: Outcome-based comparative measures of the quality of surgical care among surgical services and surgical subspecialties have been elusive. METHODS: This study included prospective assessment of presurgical risk factors, process of care during surgery, and outcomes 30 days after surgery on veterans undergoing major surgery in 123 medical centers; development of multivariable risk-adjustment models; identification of high and low outlier facilities by observed-to-expected outcome ratios; and generation of annual reports of comparative outcomes to all surgical services in the Veterans Health Administration (VHA). RESULTS: The National VA Surgical Quality Improvement Program (NSQIP) data base includes 417,944 major surgical procedures performed between October 1, 1991, and September 30, 1997. In FY97, 11 VAMCs were low outliers for risk-adjusted observed-to-expected mortality ratios; 13 VAMCs were high outliers for risk-adjusted observed-to-expected mortality ratios. Identification of high and low outliers by unadjusted mortality rates would have ascribed an outlier status incorrectly to 25 of 39 hospitals, an error rate of 64%. Since 1994, the 30-day mortality and morbidity rates for major surgery have fallen 9% and 30%, respectively. CONCLUSIONS: Reliable, valid information on patient presurgical risk factors, process of care during surgery, and 30-day morbidity and mortality rates is available for all major surgical procedures in the 123 VAMCs performing surgery in the VHA. With this information, the VHA has established the first prospective outcome-based program for comparative assessment and enhancement of the quality of surgical care among multiple institutions for several surgical subspecialties. Key features to the success of the NSQIP are the support of the surgeons who practice in the VHA, consistent clinical definitions and data collection by dedicated nurses, a uniform nationwide informatics system, and the support of VHA administration and managerial staff.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berwick D. M. Continuous improvement as an ideal in health care. N Engl J Med. 1989 Jan 5;320(1):53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- Brook R. H., McGlynn E. A., Cleary P. D. Quality of health care. Part 2: measuring quality of care. N Engl J Med. 1996 Sep 26;335(13):966–970. doi: 10.1056/NEJM199609263351311. [DOI] [PubMed] [Google Scholar]
- Chen A. Y., Daley J., Pappas T. N., Henderson W. G., Khuri S. F. Growing use of laparoscopic cholecystectomy in the national Veterans Affairs Surgical Risk Study: effects on volume, patient selection, and selected outcomes. Ann Surg. 1998 Jan;227(1):12–24. doi: 10.1097/00000658-199801000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley J. Criteria by which to evaluate risk-adjusted outcomes programs in cardiac surgery. Ann Thorac Surg. 1994 Dec;58(6):1827–1835. doi: 10.1016/0003-4975(94)91722-1. [DOI] [PubMed] [Google Scholar]
- Daley J., Forbes M. G., Young G. J., Charns M. P., Gibbs J. O., Hur K., Henderson W., Khuri S. F. Validating risk-adjusted surgical outcomes: site visit assessment of process and structure. National VA Surgical Risk Study. J Am Coll Surg. 1997 Oct;185(4):341–351. [PubMed] [Google Scholar]
- Daley J., Khuri S. F., Henderson W., Hur K., Gibbs J. O., Barbour G., Demakis J., Irvin G., 3rd, Stremple J. F., Grover F. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997 Oct;185(4):328–340. [PubMed] [Google Scholar]
- Grover F. L., Johnson R. R., Shroyer A. L., Marshall G., Hammermeister K. E. The Veterans Affairs Continuous Improvement in Cardiac Surgery Study. Ann Thorac Surg. 1994 Dec;58(6):1845–1851. doi: 10.1016/0003-4975(94)91725-6. [DOI] [PubMed] [Google Scholar]
- Hammermeister K. E., Johnson R., Marshall G., Grover F. L. Continuous assessment and improvement in quality of care. A model from the Department of Veterans Affairs Cardiac Surgery. Ann Surg. 1994 Mar;219(3):281–290. doi: 10.1097/00000658-199403000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni L. I. How much are we willing to pay for information about quality of care? Ann Intern Med. 1997 Mar 1;126(5):391–393. doi: 10.7326/0003-4819-126-5-199703010-00009. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I. Using risk-adjusted outcomes to assess clinical practice: an overview of issues pertaining to risk adjustment. Ann Thorac Surg. 1994 Dec;58(6):1822–1826. doi: 10.1016/0003-4975(94)91721-3. [DOI] [PubMed] [Google Scholar]
- Khuri S. F., Daley J., Henderson W., Barbour G., Lowry P., Irvin G., Gibbs J., Grover F., Hammermeister K., Stremple J. F. The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg. 1995 May;180(5):519–531. [PubMed] [Google Scholar]
- Khuri S. F., Daley J., Henderson W., Hur K., Gibbs J. O., Barbour G., Demakis J., Irvin G., 3rd, Stremple J. F., Grover F. Risk adjustment of the postoperative mortality rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997 Oct;185(4):315–327. [PubMed] [Google Scholar]
- Kizer K. W., Pane G. A. The "new VA": delivering health care value through integrated service networks. Ann Emerg Med. 1997 Dec;30(6):804–807. doi: 10.1016/s0196-0644(97)70053-2. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr, Sherbourne C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- Young G. J., Charns M. P., Daley J., Forbes M. G., Henderson W., Khuri S. F. Best practices for managing surgical services: the role of coordination. Health Care Manage Rev. 1997 Fall;22(4):72–81. doi: 10.1097/00004010-199710000-00010. [DOI] [PubMed] [Google Scholar]


