Abstract
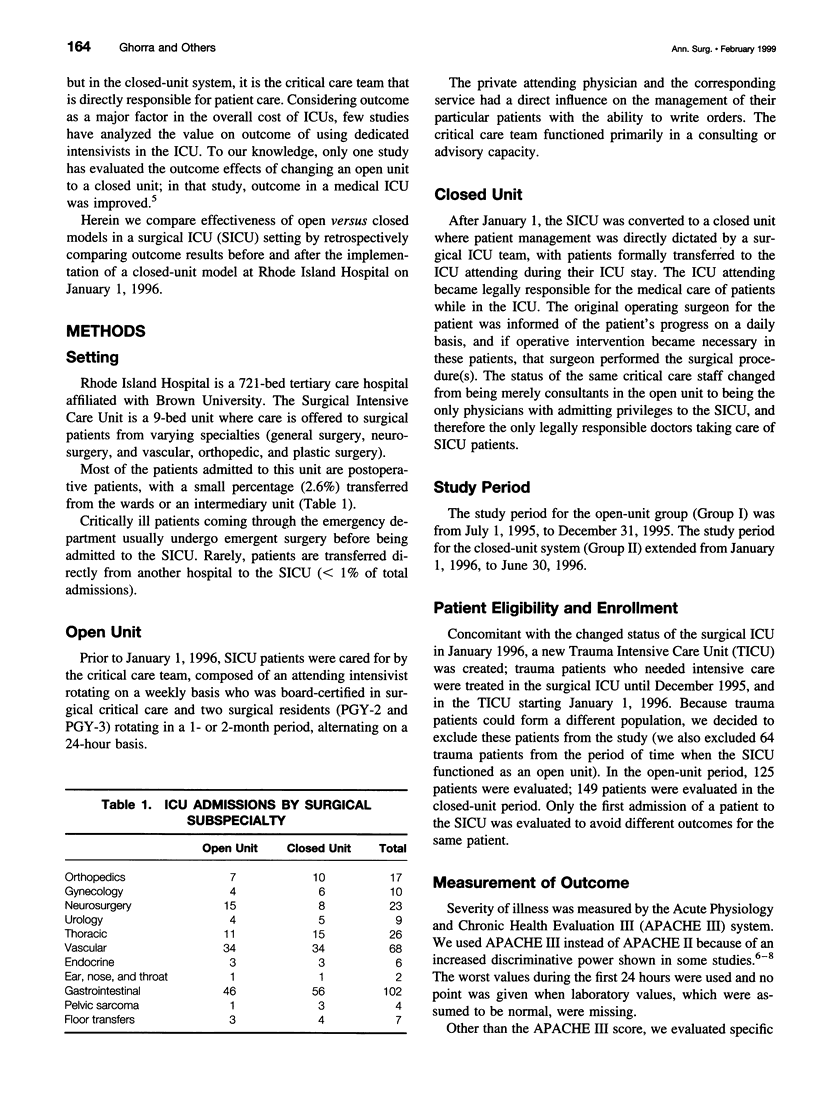
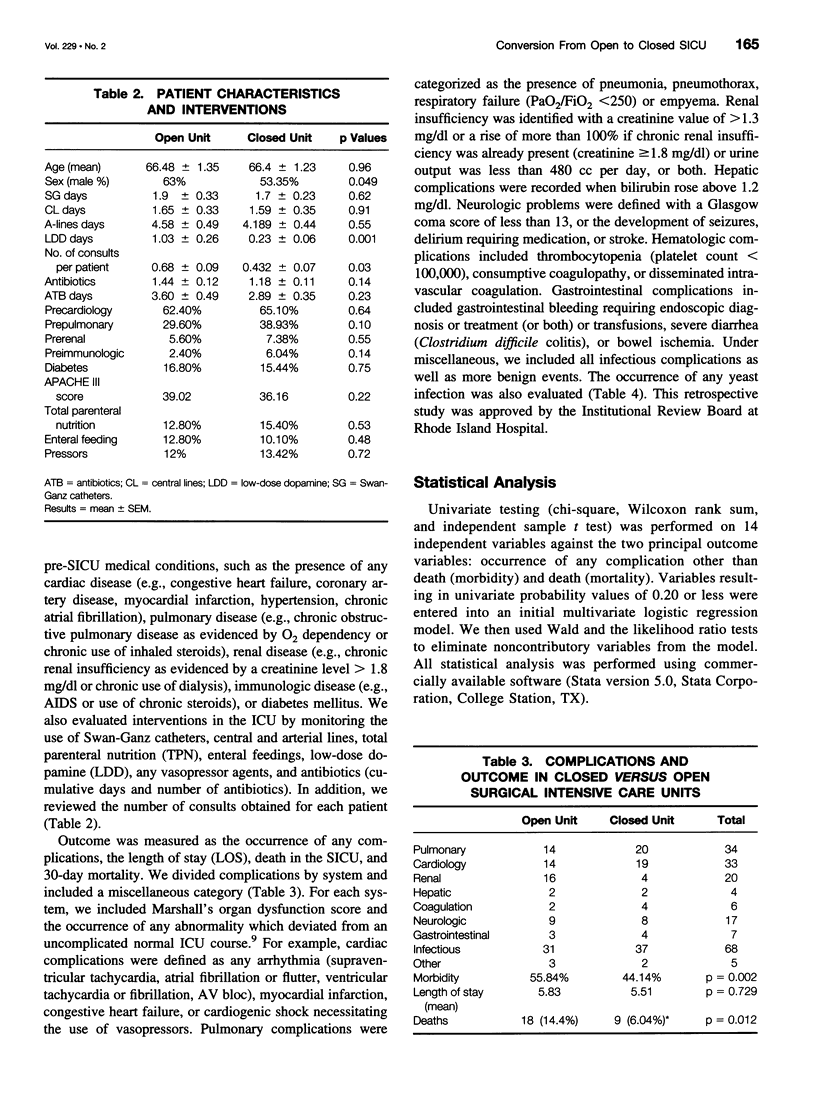
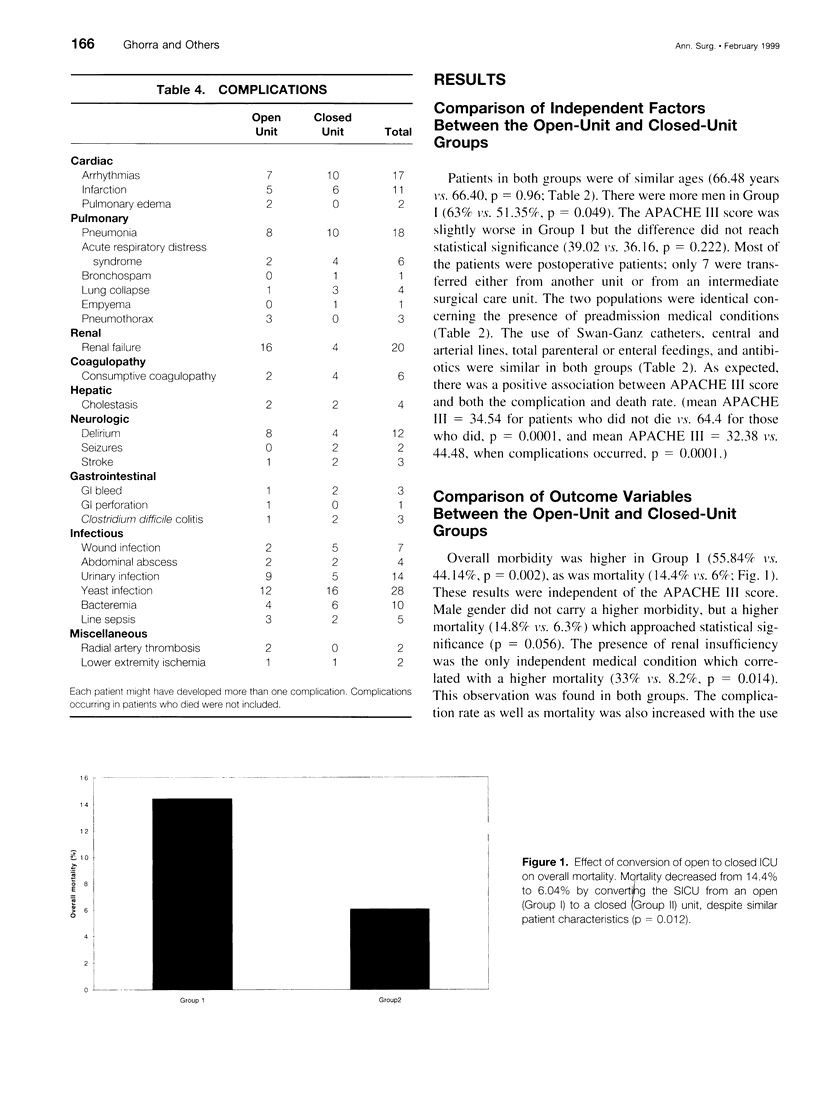
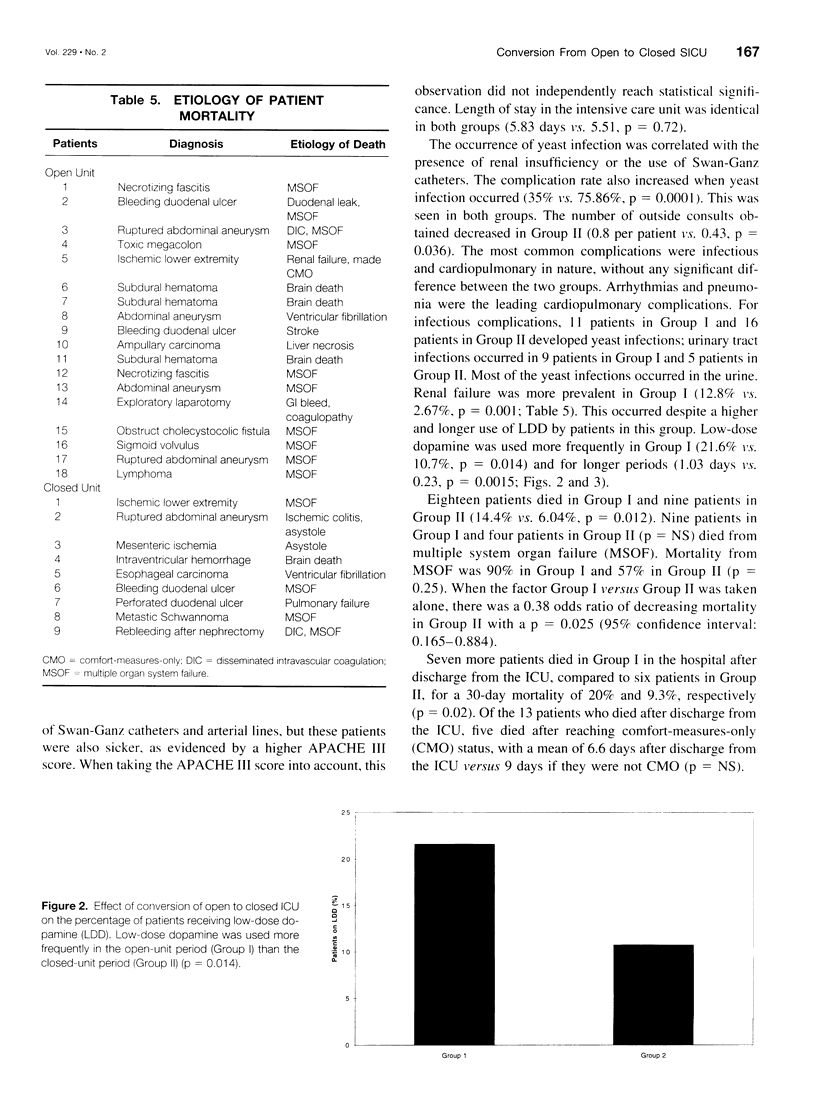
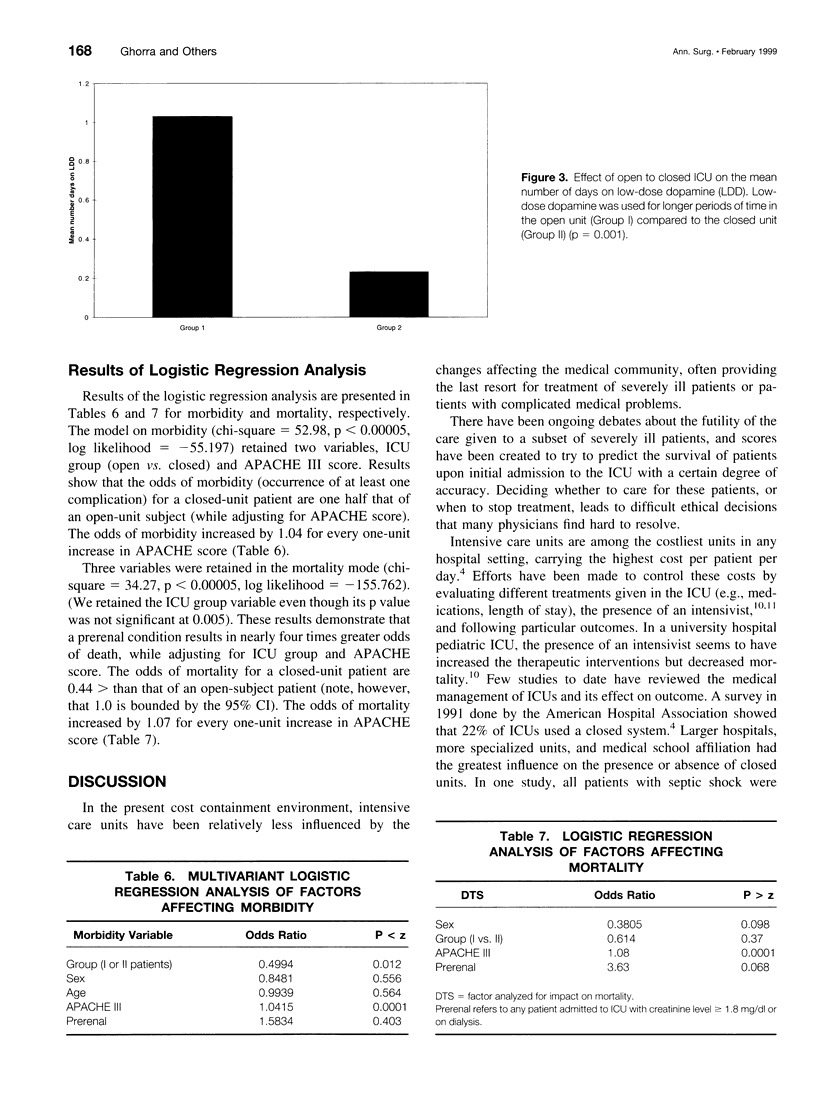
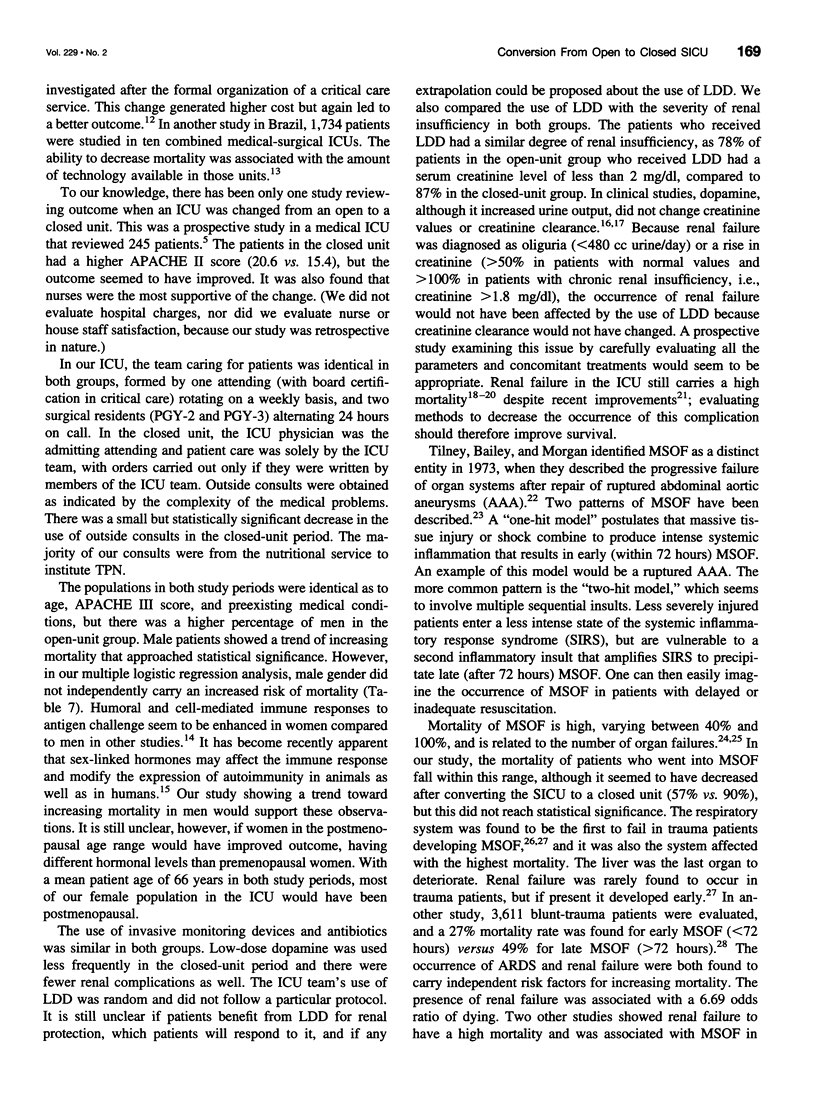
OBJECTIVE: To compare the effect on clinical outcome of changing a surgical intensive care unit from an open to a closed unit. DESIGN: The study was carried out at a surgical intensive care unit in a large tertiary care hospital, which was changed on January 1, 1996, from an open unit, where private attending physicians contributed and controlled the care of their patients, to a closed unit, where patients' medical care was provided only by the surgical critical care team (ABS or ABA board-certified intensivists). A retrospective review was undertaken over 6 consecutive months in each system, encompassing 274 patients (125 in the open-unit period, 149 in the closed-unit period). Morbidity and mortality were compared between the two periods, along with length-of-stay (LOS) and number of consults obtained. A set of independent variables was also evaluated, including age, gender, APACHE III scores, the presence of preexisting medical conditions, the use of invasive monitoring (Swan-Ganz catheters, central and arterial lines), and the use of antibiotics, low-dose dopamine (LDD) for renal protection, vasopressors, TPN, and enteral feeding. RESULTS: Mortality (14.4% vs. 6.04%, p = 0.012) and the overall complication rate (55.84% vs. 44.14%, p = 0.002) were higher in the open-unit group versus the closed-unit group, respectively. The number of consults obtained was decreased (0.6 vs. 0.4 per patient, p = 0.036), and the rate of occurrence of renal failure was higher in the open-unit group (12.8% vs. 2.67%, p = 0.001). The mean age of the patients was similar in both groups (66.48 years vs. 66.40, p = 0.96). APACHE III scores were slightly higher in the open-unit group but did not reach statistical significance (39.02 vs. 36.16, p = 0.222). There were more men in the first group (63.2% vs. 51.3%). The use of Swan-Ganz catheters or central and arterial lines were identical, as was the use of antibiotics, TPN, and enteral feedings. The use of LDD was higher in the first group, but the LOS was identical. CONCLUSIONS: Conversion of a tertiary care surgical intensive care unit from an open to closed environment reduced dopamine usage and overall complication and mortality rates. These results support the concept that, when possible, patients in surgical intensive care units should be managed by board-certified intensivists in a closed environment.
Full text
PDF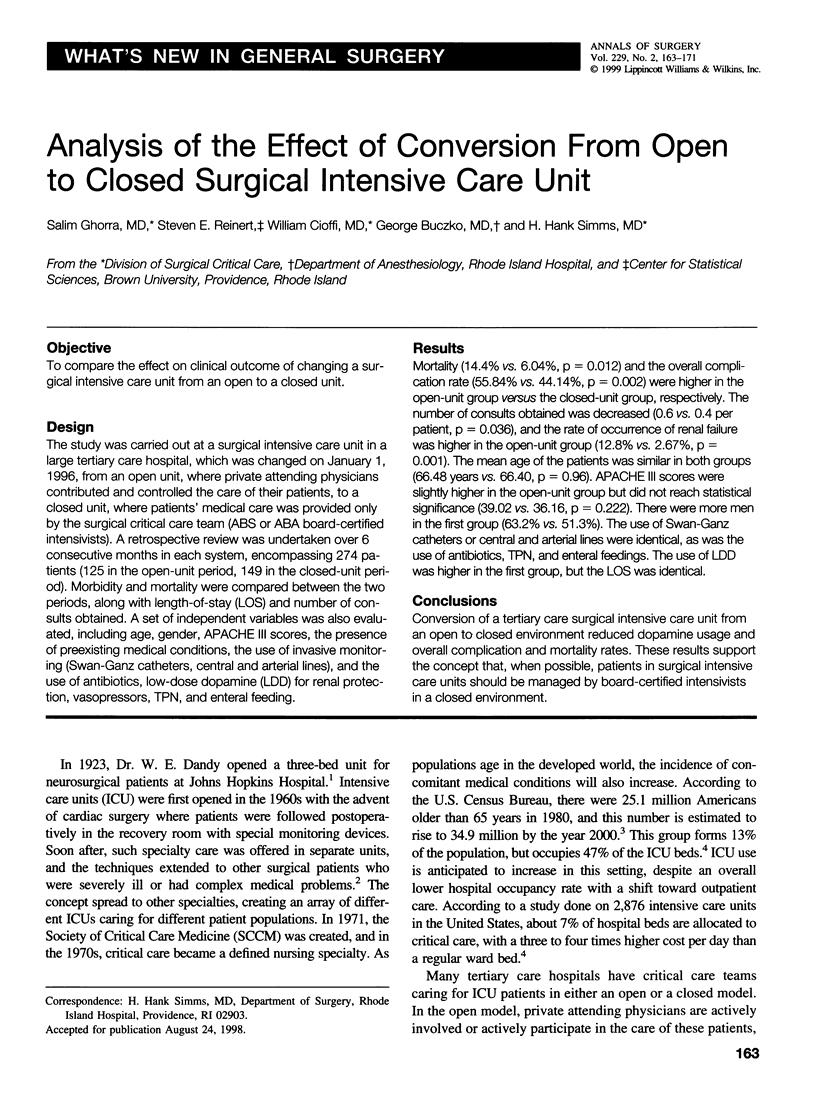


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ansar Ahmed S., Penhale W. J., Talal N. Sex hormones, immune responses, and autoimmune diseases. Mechanisms of sex hormone action. Am J Pathol. 1985 Dec;121(3):531–551. [PMC free article] [PubMed] [Google Scholar]
- Barie P. S., Hydo L. J., Fischer E. Comparison of APACHE II and III scoring systems for mortality prediction in critical surgical illness. Arch Surg. 1995 Jan;130(1):77–82. doi: 10.1001/archsurg.1995.01430010079016. [DOI] [PubMed] [Google Scholar]
- Bastos P. G., Knaus W. A., Zimmerman J. E., Magalhães A., Jr, Sun X., Wagner D. P. The importance of technology for achieving superior outcomes from intensive care. Brazil APACHE III Study Group. Intensive Care Med. 1996 Jul;22(7):664–669. doi: 10.1007/BF01709743. [DOI] [PubMed] [Google Scholar]
- Brivet F. G., Kleinknecht D. J., Loirat P., Landais P. J. Acute renal failure in intensive care units--causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med. 1996 Feb;24(2):192–198. doi: 10.1097/00003246-199602000-00003. [DOI] [PubMed] [Google Scholar]
- Brown J. J., Sullivan G. Effect on ICU mortality of a full-time critical care specialist. Chest. 1989 Jul;96(1):127–129. doi: 10.1378/chest.96.1.127. [DOI] [PubMed] [Google Scholar]
- Carson S. S., Stocking C., Podsadecki T., Christenson J., Pohlman A., MacRae S., Jordan J., Humphrey H., Siegler M., Hall J. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comparison of 'open' and 'closed' formats. JAMA. 1996 Jul 24;276(4):322–328. [PubMed] [Google Scholar]
- Castella X., Artigas A., Bion J., Kari A. A comparison of severity of illness scoring systems for intensive care unit patients: results of a multicenter, multinational study. The European/North American Severity Study Group. Crit Care Med. 1995 Aug;23(8):1327–1335. doi: 10.1097/00003246-199508000-00005. [DOI] [PubMed] [Google Scholar]
- Civetta J. M., Hudson-Civetta J. A., Nelson L. D. Evaluation of APACHE II for cost containment and quality assurance. Ann Surg. 1990 Sep;212(3):266–276. doi: 10.1097/00000658-199009000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deitch E. A. Multiple organ failure. Pathophysiology and potential future therapy. Ann Surg. 1992 Aug;216(2):117–134. doi: 10.1097/00000658-199208000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunham C. M., Damiano A. M., Wiles C. E., Cushing B. M. Post-traumatic multiple organ dysfunction syndrome--infection is an uncommon antecedent risk factor. Injury. 1995 Jul;26(6):373–378. doi: 10.1016/0020-1383(95)00061-d. [DOI] [PubMed] [Google Scholar]
- Groeger J. S., Guntupalli K. K., Strosberg M., Halpern N., Raphaely R. C., Cerra F., Kaye W. Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization. Crit Care Med. 1993 Feb;21(2):279–291. doi: 10.1097/00003246-199302000-00022. [DOI] [PubMed] [Google Scholar]
- Harvey A. M. Neurosurgical genius - Walter Edward Dandy. Johns Hopkins Med J. 1974 Nov;135(5):358–368. [PubMed] [Google Scholar]
- Henderson I. S., Beattie T. J., Kennedy A. C. Dopamine hydrochloride in oliguric states. Lancet. 1980 Oct 18;2(8199):827–828. doi: 10.1016/s0140-6736(80)90174-9. [DOI] [PubMed] [Google Scholar]
- Knaus W. A., Wagner D. P. Multiple systems organ failure: epidemiology and prognosis. Crit Care Clin. 1989 Apr;5(2):221–232. [PubMed] [Google Scholar]
- Levy E. M., Viscoli C. M., Horwitz R. I. The effect of acute renal failure on mortality. A cohort analysis. JAMA. 1996 May 15;275(19):1489–1494. [PubMed] [Google Scholar]
- McCarthy J. T. Prognosis of patients with acute renal failure in the intensive-care unit: a tale of two eras. Mayo Clin Proc. 1996 Feb;71(2):117–126. doi: 10.4065/71.2.117. [DOI] [PubMed] [Google Scholar]
- Moore F. A., Moore E. E., Read R. A. Postinjury multiple organ failure: role of extrathoracic injury and sepsis in adult respiratory distress syndrome. New Horiz. 1993 Nov;1(4):538–549. [PubMed] [Google Scholar]
- Morris J. A., Jr, Mucha P., Jr, Ross S. E., Moore B. F., Hoyt D. B., Gentilello L., Landercasper J., Feliciano D. V., Shackford S. R. Acute posttraumatic renal failure: a multicenter perspective. J Trauma. 1991 Dec;31(12):1584–1590. doi: 10.1097/00005373-199112000-00003. [DOI] [PubMed] [Google Scholar]
- Pollack M. M., Katz R. W., Ruttimann U. E., Getson P. R. Improving the outcome and efficiency of intensive care: the impact of an intensivist. Crit Care Med. 1988 Jan;16(1):11–17. doi: 10.1097/00003246-198801000-00003. [DOI] [PubMed] [Google Scholar]
- Regel G., Grotz M., Weltner T., Sturm J. A., Tscherne H. Pattern of organ failure following severe trauma. World J Surg. 1996 May;20(4):422–429. doi: 10.1007/s002689900067. [DOI] [PubMed] [Google Scholar]
- Reynolds H. N., Haupt M. T., Thill-Baharozian M. C., Carlson R. W. Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive care unit. JAMA. 1988 Dec 16;260(23):3446–3450. [PubMed] [Google Scholar]
- Sauaia A., Moore F. A., Moore E. E., Haenel J. B., Read R. A., Lezotte D. C. Early predictors of postinjury multiple organ failure. Arch Surg. 1994 Jan;129(1):39–45. doi: 10.1001/archsurg.1994.01420250051006. [DOI] [PubMed] [Google Scholar]
- Shen G. K., Montgomery D. W., Ulrich E. D., Mahoney K. R., Zukoski C. F. Up-regulation of prolactin gene expression and feedback modulation of lymphocyte proliferation during acute allograft rejection. Surgery. 1992 Aug;112(2):387–394. [PubMed] [Google Scholar]
- Shusterman N., Strom B. L., Murray T. G., Morrison G., West S. L., Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987 Jul;83(1):65–71. doi: 10.1016/0002-9343(87)90498-0. [DOI] [PubMed] [Google Scholar]
- Tilney N. L., Bailey G. L., Morgan A. P. Sequential system failure after rupture of abdominal aortic aneurysms: an unsolved problem in postoperative care. Ann Surg. 1973 Aug;178(2):117–122. doi: 10.1097/00000658-197308000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]


