Abstract
Objective: To ascertain the frequencies of 4 prospectively determined pain complaints among adolescents meeting the criteria for major depressive episode (MDE) relative to nonaffectively ill controls.
Method: In a community mental health clinic for the indigent situated on the border of the United States and Mexico (Rio Grande City, Tex.), adolescents (age range, 12–17 years) who consecutively presented to the clinic from August 2001 to November 2003 received structured psychiatric diagnostic screens for depression and mania using the modules from the DSM-IV. Subsequently, all subjects were asked whether they had had significant (distressing or bothersome) backache, abdominal pain, headaches, or myalgia in the last 7 days. We compared patients meeting the criteria for MDE with individuals without affective symptomatology. Significance of the differences between groups was assessed using the Fisher exact test and multivariate logistic regression analysis. The odds ratios were adjusted for age and sex.
Results: One hundred thirty-two subjects met the criteria for MDE. Forty-eight had non-affective disorders. Seventy-six percent of the subjects meeting the criteria for MDE had at least 1 pain complaint compared to 33% of the control subjects (p < .0001). Fifty percent of the subjects in the midst of a MDE had at least 2 pain complaints compared to 6% of the control subjects (p < .0001). Twenty-nine percent of the subjects in the midst of a MDE had at least 3 pain complaints compared to 2% of the control subjects (p < .0001). Fourteen percent of the subjects in the midst of a MDE had all 4 pain complaints compared to none of the control subjects (p = .002). The odds ratio of subjects with a MDE having a pain complaint relative to control subjects was 5.8 (p < .0001).
Conclusion: That in excess of three fourths of clinically depressed adolescents had 1 or more pain complaints has important implications for adolescent psychiatry and primary care, as well as somatic medicine.
Unexplained somatic complaints, including pain, are a common phenomenon among depressed adults.1–5 However, to the best of our knowledge, an article about the prevalence of pain complaints among depressed adolescents has yet to be published. In the present article, we report the frequency of 4 prospectively determined pain complaints among adolescents, none of whom presented with a chief complaint of pain, meeting the criteria for major depressive episode (MDE) relative to psychiatric controls.
Investigators conducting a study for the World Health Organization discovered that 69% of all depressed patients diagnosed with MDE in a primary care setting presented only because of the presence of unexplained and significant somatic symptoms.2 In a recent review of the literature, Greden4 estimated that in excess of two thirds of all adults presenting with a chief complaint of depression have pain symptoms. Comparable data are not available for children or adolescents.
A MEDLINE search conducted by us combining the terms adolescents, depression, and pain disclosed 1146 entries for the period of 1966 through December 31, 2004. None presented the results of a systematic study devoted to the presence of pain among adolescents with primary disorders of mood.
Massi et al.,6 in a relevant article not focusing upon depressed youths but rather those presenting with any type of emotional or behavioral disturbance, found that there is a relationship between depression and a variety of general somatic complaints. Fifty-eight percent of these emotionally/behaviorally disturbed youths who were incidentally diagnosed with MDE had headaches. Stewart7 suggested that so-called physical symptoms (generalized somatic distress—not merely pain) are a prominent feature of juvenile-onset affective disorders.
These contributions—the impetus provided by the extant adult literature, our clinical experience, and the absence of an identifiable comparable report in the MEDLINE database—led us to specifically address the issue of pain complaints in depressed children and adolescents. The content of this report is restricted to data pertaining to depressed adolescents.
We first present data on the rates of 4 prospectively ascertained pain syndromes in depressed adolescents. We then progress to a consideration of the treatment implications of these pain syndromes followed by a discussion of the relevance of the findings for psychiatrists and primary care physicians.
METHOD
The patients are all adolescents between the ages of 12 and 17 years who presented from August 2001 to November 2003 in a public sector psychiatric outpatient clinic for the destitute in Rio Grande City, Tex. The threshold for referral is moderate to severe impairment in multiple domains. The age range of 12 to 17 years includes, by convention, adolescence in the psychiatric pediatric literature.
The racial composition of the community was 99% Hispanic and 1% other. Rio Grande City is a small town of about 15,000 people. It is located in far-reaching Starr County. There is little movement into the community. This semi-closed community provides an ambience in which there is a relatively limited genetic variance. We suspect that this accounts for a high prevalence of bipolarity among its inhabitants.
The patients are 132 consecutively, prospectively evaluated adolescent subjects meeting the DSM-IV8 criteria for MDE and 48 psychiatric control subjects. The patients were physically healthy and did not have medical comorbidity that might explain the pain and were not receiving psychiatric treatment at study entry. Indeed, the clinic in which services were delivered was the only option for psychiatric care in the community apart from that delivered by primary care physicians. None, in contrast to adults seen in the clinic, were receiving treatment from primary care physicians.
Subjects with MDE include 88 with major depressive disorder (MDD) and 44 with bipolar disorder. The latter include individuals with bipolar I disorder, depressed; bipolar II disorder, depressed; and individuals in mixed states.
The psychiatric control subjects include individuals with conduct disorder, substance abuse, and variants of adjustment disorder not accompanied by depressed or anxious mood, and those with no Axis I disorder.
The subjects received a structured diagnostic interview to determine the presence of MDE and mania using the modules from the Structured Clinical Interview for DSM-IV (Clinical Version).9 Following the completion of the interview using these modules, the patients were asked whether they had experienced significant abdominal pain, headache, back pain, or myalgia “in the last week.” The entirety of this evaluative procedure is applied to all children, adolescents, and adults entering the clinic regardless of presenting complaint. Hence, the data were collected in and through the process of delivering routine clinical services, and informed consent was not needed.
Patients with MDD and bipolar disorder will be grouped together and referred to as “affectively ill subjects.” The control subjects will simply be referred to as the “nonaffectively ill subjects” for the sake of convenience.
The data were assessed for significance using the Fisher exact text and multivariate logistic regression analysis. The odds ratios were adjusted for age and sex. Sex but not age was a significant variable in the model. Hence, the odds ratios had to be adjusted only for sex. All measures of variance in the text refer to the standard deviation (SD) of the mean.
RESULTS
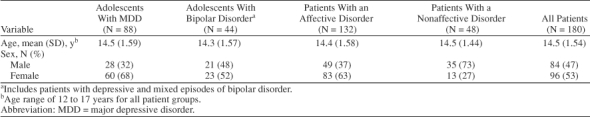
The demographic characteristics of the patients are summarized in Table 1. The primary difference between groups was the sex distribution. The male-to-female ratio for subjects with MDD was 1:2.1. The male-to-female ratio for subjects with bipolar disorder was 1:1.1. The sex distributions are consistent with those reported for adults with unipolar depression10 and bipolar disorder.11 The male-to-female ratio for control subjects was 2.7:1.
Table 1.
Demographic Characteristics of Adolescents With Affective or Nonaffective Disorders
Twenty-four percent versus 67% of the patients with and without affective disorders, respectively, did not have a pain complaint (Table 2). This difference is highly significant (p < .0001). Seventy-six percent of the affectively ill patients (100 of 132) had 1 or more pain syndromes compared to just 33% of control patients (16 of 48). This difference is also highly significant (p < .0001). Patients with MDD and those with bipolar disorder were equally likely to have 1 or more pain complaints.
Table 2.
Number of Pain Syndromes Per Patient Groupa
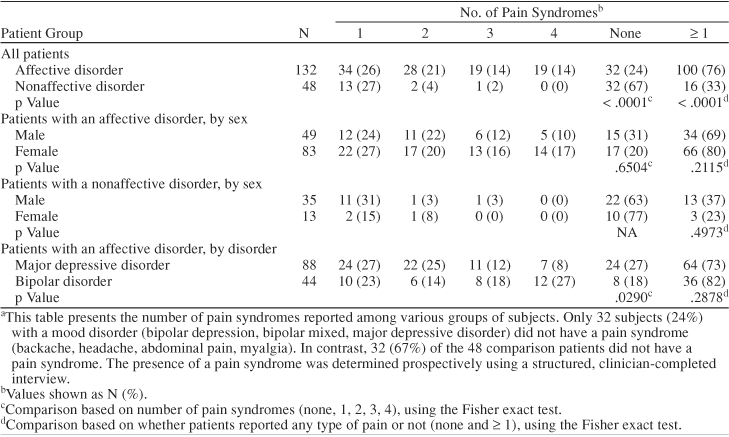
Affectively and nonaffectively ill patients did not differ in the rates with which they simply had 1, 2, 3, or 4 pain complaints (see Table 2). However, the affectively ill patients were significantly more likely to have ≥ 1, ≥ 2, ≥ 3, or all of the pain complaints than the nonaffectively ill patients. All of these differences are significant at p < .0001, except for “all 4 pain syndromes,” for which the difference was significant at p = .002. These data are summarized in Table 3.
Table 3.
Number of Pain Syndromes for Patients With Affective or Nonaffective Disordersa
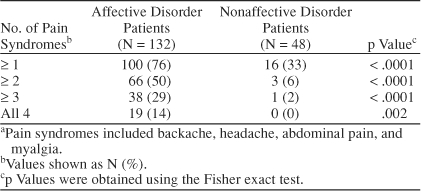
Table 4 presents the frequencies with which affectively and nonaffectively ill patients had each of the pain complaints or any 1 of the 4 pain complaints whatsoever. These results are presented using the multivariate logistic regression model specified in the Method section. The odds ratios and their 95% confidence intervals are also presented. The affectively ill subjects were more likely to have backache (p = .0027), headache (p < .0001), abdominal pain (p = .0061), and myalgia (p = .0026). The odds ratio of an affectively ill subject having any form of pain was 5.8 (p < .0001).
Table 4.
Type of Pain Syndromes by Patient Groupa
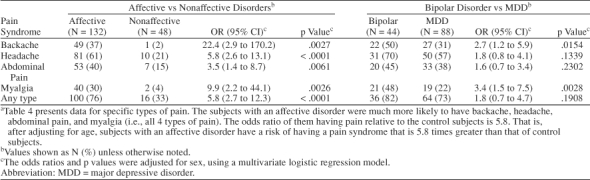
Bipolar patients (50%) were more likely to have backache than patients with MDD (31%). The odds ratio was 2.7 (p = .015). This finding could not be explained by antecedent psychotropic–mediated weight gain, as the patients were all drug-naive subjects. Patients with bipolar disorder were also more likely to have myalgia (48%) than the patients with MDD (22%). The odds ratio was 3.4 (p = .003). A higher but statistically insignificant percentage of the bipolar patients had headache (70% vs. 57%). There was no significant difference in the frequencies with which bipolar patients and those with MDD had, as ascertained by patient description, migraine headaches (30% vs. 25%). Neither bipolar nor MDD patients were significantly more likely to have abdominal pain (45% vs. 38%, respectively).
The odds ratios for each type of pain for subjects with and without affective disorders, and for the bipolar and MDD patients in particular, and their 95% confidence intervals are shown in Table 4.
DISCUSSION
Seventy-six percent of the depressed adolescents and 33% of the control subjects had 1 or more pain complaints. This figure is higher than those typically reported for adults in the literature, which reports that in excess of two thirds of all patients present with unexplained somatic symptoms that include but are not restricted to pain complaints.2 A pain complaint rate of 76% would, based on the literature—not clinical experience—be an extremely high rate among depressed adults. However, the high rate of pain complaints among adolescents reported here may be a consequence of our systematic method of investigation.
The depressed adolescents were more likely to have each of the 4 pain complaints (backache, headache, abdominal pain, and myalgia) recorded than were control patients. The bipolar patients were significantly more likely to have backache and myalgia than the subjects with MDD, suggesting that bipolar patients may be more inclined to experience skeletal muscle pain than patients with MDD. A future study would ideally record arthralgia as an independent type of pain. Many of our patients with bipolar depression reported whole body pain. Some patients ached as if they had the flu. Thus, a question to the effect of, “Does your entire body hurt or ache?” might be reasonably included as a pain category in a future study in an effort at separating subjects with MDD and bipolar disorder. Further, some patients diagnosed with fibromyalgia, a complex somatic pain syndrome associated with high affective comorbidity and frequently resistant to antidepressant therapy, might conceivably be suffering from bipolar spectrum disorders. A separation into unipolar and bipolar fibromyalgia subtypes might yield more successful interventions for identified individuals.
Eighty-two percent of the bipolar patients had at least 1 pain syndrome compared to 73% of the unipolar patients. The high base rate of pain complaints among the subjects in both diagnostic groups renders this study inadequately powered to meaningfully test the hypothesis that there are global differences in the rates of these complaints between them. Demonstrating such a difference would require a very large database indeed.
The design of this study differs from those involving adults. We were able to identify patients with a structured interview–verified primary disorder of mood and then compare them to patients in a control group comprising adolescents with nonaffective disorders. The control group excluded patients with any identifiable affective symptoms such as anxiety or depression. The use of such a control group is a strength that, to the best of our knowledge, is lacking in the extant adult literature.
We were also able to determine the presence of pain complaints prospectively in all subjects. We did not have to rely upon either spontaneous reports or a chart review. One must assume that reliance on either method would result in false negatives and lower base rates of pain complaints.
Our findings have strong clinical implications. First, persistent pain can indicate that a patient has not been optimally treated. We regard persistent headaches and the presence of other residual symptoms of depression to be an indication for more aggressive pharmacotherapy and vigilance. Dilsaver et al.12 reported that aggressive treatment with tranylcypromine, a monoamine oxidase inhibitor, and bupropion completely eliminated “unexplained” pain complaints in adults with wintertime depression presenting in a mood disorders clinic. Many of these patients had sought medical consultation prior to presentation in the clinic only to find no relief.
Paykel et al.13 reported that residual symptoms of a depressive syndrome, which would include pain, are very strong predictors of early relapse. Early relapse occurred in 76% of patients (13 of 17) with residual symptoms as opposed to 25% of those (10 of 40) without these symptoms. This observation, coupled with that of Dilsaver and colleagues,12 argues for the aggressive treatment of depression in the face of ongoing residual signs and symptoms of a depressive syndrome.
The findings in the present study also raise the possibility that many adolescents presenting in primary care settings with chronic, recurrent idiopathic pain or more generally “physical symptoms” may be depressed. The number of pain complaints, as inferred from the adult literature, may be related to the probability of undetected depression. In a study involving adults, 23% of all patients with 4 physical, but not necessarily pain, symptoms were depressed and 60% with 9 or more symptoms were depressed.14 A physical symptom could include fatigue and a whole host of other somatic complaints. Thus, it is reasonable for clinicians in primary care settings to presume that there is an increasingly high probability that an adolescent is depressed as the number of somatic complaints, including pain complaints, rises.
We propose that youths presenting with idiopathic pain in any clinical setting be screened for the signs and symptoms of a depressive syndrome and, if indicated, receive the apposite therapy. We also encourage psychiatrists and primary care physicians alike to remember the maxim, “Where there is pain there is depression [see references 15 and 16] and where there is depression there is pain [see references 12, 17, and 18],” to be ingrained into their consciousness. Remembering this maxim can spare clinicians frustration and feelings of helplessness by allowing them to see their otherwise untreatable patients receiving dramatic relief from pain.
Drug name: tranylcypromine (Parnate).
Footnotes
This work was not supported by external funding.
Dr. Akiskal has been a consultant for, has received honoraria from, and has been on the speakers board for Bristol-Myers Squibb, AstraZeneca, Eli Lilly, Sanofi, GlaxoSmithKline, and Abbott. Drs. Dilsaver and Manning and Mr. Wu report no financial or other relationship relevant to the subject of this article.
REFERENCES
- Simon GE, Von Korff M, and Piccinelli M. et al. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999 341:658–659. [DOI] [PubMed] [Google Scholar]
- Sartorius N. Physical symptoms of depression as public health concern. J Clin Psychiatry. 2003 64suppl 7. 3–4. [PubMed] [Google Scholar]
- Sartorious N, Davidian H, and Ernberg G. et al. Depressive Disorders in Different Cultures. Geneva, Switzerland: World Health Organization. 1983 [Google Scholar]
- Greden JF. Physical symptoms in depression: unmet needs. J Clin Psychiatry. 2003 64suppl 7. 5–11. [PubMed] [Google Scholar]
- Moldin SO, Scheftner WA, and Rice JP. et al. Association between major depressive disorder and physical illness. Psychol Med. 1993 23:755–761. [DOI] [PubMed] [Google Scholar]
- Massi G, Favilla L, and Milepiedi S. et al. Somatic symptoms in children and adolescents referred for emotional and behavioral disorders. Psychiatry. 2000 63:140–149. [DOI] [PubMed] [Google Scholar]
- Stewart DE. Physical symptoms of depression: unmet needs in special populations. J Clin Psychiatry. 2003 64suppl 7. 12–16. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- First MB, Spitzer RL, and Gibbon M. et al. The Structured Clinical Interview of DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, DC: American Psychiatric Association. 1997 [Google Scholar]
- Weissman MM, Leaf PJ, and Holzer CE. et al. The epidemiology of depression: an update on sex differences. J Affect Disord. 1984 7:179–188. [DOI] [PubMed] [Google Scholar]
- Belmaker RH. Bipolar disorder. N Engl J Med. 2004;351:476–486. doi: 10.1056/NEJMra035354. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, Del Medico VJ, Qamar AB. State-dependent pain in winter depression. Br J Psychiatry. 1993;163:672–674. doi: 10.1192/bjp.163.5.672. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Ramana R, and Cooper Z. et al. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995 25:1171–1180. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, and Williams JB. et al. Physical symptoms in primary care: predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994 3:774–779. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry. 1996;168:101–108. [PubMed] [Google Scholar]
- Ruoff GE. Depression in patient with chronic pain. J Fam Pract. 1996 43suppl 6. S25–S33. [PubMed] [Google Scholar]
- Lindsay P, Wyckoff M. The depression pain syndrome and its response to antidepressants. Psychosomatics. 1981;22:571–577. doi: 10.1016/S0033-3182(81)73478-9. [DOI] [PubMed] [Google Scholar]
- von Knorring L. The experience of pain in depressed patients. Neuropsychopharmacology. 1975;1:155–165. doi: 10.1159/000117488. [DOI] [PubMed] [Google Scholar]


