Abstract
Objective: Patients with depression present with psychological and somatic symptoms, including general aches and pains. In primary care, somatic symptoms often dominate. A review of the literature was conducted to ascertain the importance of somatic symptoms in depression in primary care.
Data sources and extraction: MEDLINE, EMBASE, and PsychLIT/PsychINFO databases (1985–January 2004) were searched for the terms depression, depressive, depressed AND physical, somatic, unexplained symptoms, complaints, problems; somatised, somatized symptoms; somatisation, somatization, somatoform, psychosomatic; pain; recognition, underrecognition; diagnosis, underdiagnosis; acknowledgment, underacknowledgment; treatment, undertreatment AND primary care, ambulatory care; primary physician; office; general practice; attribution, reattribution; and normalising, normalizing. Only English-language publications and abstracts were considered.
Study selection: More than 80 papers related to somatic symptoms in depression were identified using the content of their titles and abstracts.
Data synthesis: Approximately two thirds of patients with depression in primary care present with somatic symptoms. These patients are difficult to diagnose, feel an increased burden of disease, rely heavily on health care services, and are harder to treat. Patient and physician factors that prevent discussion of psychological symptoms during consultations must be overcome.
Conclusions: Educational initiatives that raise awareness of somatic symptoms in depression and help patients to reattribute these symptoms should help to improve the recognition of depression in primary care.
Depression is highly prevalent.1 Approximately 20% of patients in primary care present with clinically significant depressive symptoms.2 In certain urban areas of the United Kingdom, up to 17% of the general population are affected.3 Despite improved awareness of the condition in primary care, depression remains difficult to diagnose initially, and the majority of cases are only recognized at subsequent consultations, sometimes several years after the patient's initial visit.4
In primary care, physicians require sophisticated consulting skills to enable them to differentiate a wide range of symptoms from a complex narrative in a short period of time. Symptoms of depression include classic psychological symptoms, such as low mood, loss of interest, poor concentration, and associated anxiety, and somatic symptoms, such as changes in appetite, lack of energy, sleep disturbance, and general aches and pains.5,6 The suspicion of depression is usually raised by the presence of psychological symptoms. However, in approximately two thirds of patients with depression, the clinical picture is dominated by somatic symptoms, such as lack of energy and general aches and pains,7,8 which patients frequently attribute to normalizing causes. As a result, many physicians become preoccupied with lengthy investigations into possible underlying organic disease rather than considering depression as a diagnosis.9 Indeed, depression is mostly difficult to recognize in patients who present with chiefly somatic complaints.8,10
We conducted a review of the recent literature to ascertain the importance of somatic symptoms in depression in primary care, focusing particularly on their effects on the recognition of depressive symptomatology.
DATA SOURCES AND EXTRACTION
An electronic search was performed on the MEDLINE, EMBASE, and PsychLIT/PsychINFO databases to find articles published between 1985 and January 2004 that contained the following terms in the title (PsychLIT/ PsychINFO) and/or abstract (MEDLINE and EMBASE): depression, depressive, depressed AND physical, somatic, unexplained symptoms, complaints, problems; somatised, somatized symptoms; somatisation, somatization, somatoform, psychosomatic; pain; recognition, underrecognition; diagnosis, underdiagnosis; acknowledgment, underacknowledgment; treatment, undertreatment AND primary care, ambulatory care; primary physician; office; general practice; attribution, reattribution; and normalising, normalizing. Non–English-language publications and abstracts were not considered.
The results of the literature search were reviewed to select those of the correct type (i.e., those that focused on the somatic symptoms that are part of depressive disorder), based on the content of their title and abstracts (if available). Articles clearly about the coexistence of depression with a defined organic pathology were not included. Handsearching of citation lists was then performed on selected articles, and other information was included from the authors' own knowledge of the literature, international guidelines, diagnostic tools, and relevant theses.
STUDY SELECTION
MEDLINE, EMBASE, and PsychLIT/PsychINFO database searches identified 2213, 1901, and 2462 citations, respectively. On the basis of the content of titles and abstracts, primary care and general population studies, case series, editorials, and review articles relating to somatic symptoms in depression were selected and reviewed in full. Handsearching of the citation lists in these publications identified several supplementary relevant articles beyond the limits of the literature search. Articles concerning somatic symptoms in depressed patients with organic diseases, such as cancer or arthritis, and patients with the clinical diagnosis of somatoform disorder or somatization disorder were excluded. More than 80 pertinent papers relating to somatic symptoms in depression were identified by this approach and form the basis of this review.
DATA SYNTHESIS
The Lexicon Surrounding Somatic Symptoms in Depression
The language used in the medical literature to describe somatic symptoms in depression is both confusing and contradictory; hence, the broad scope of our literature search. In the interests of consistency, unless directly quoted from a reference, we chose to use the term somatic symptoms throughout this review to describe a range of symptoms that includes changes in appetite and libido, lack of energy, sleep disturbance, nonpainful somatic symptoms (e.g., dizziness, palpitations, dyspnea), and general aches and pains (e.g., headache, backache, musculoskeletal aches, and gastrointestinal disturbances). However, a large number of terms, including physical symptoms (problems or complaints), chronic painful physical conditions, medically unexplained symptoms, somatized symptoms, painful symptoms, somatization, somatoform symptoms, psychosomatic symptoms, and masked depression, have been used interchangeably over the years to describe the phenomenon of somatic symptoms and general aches and pains in depression.
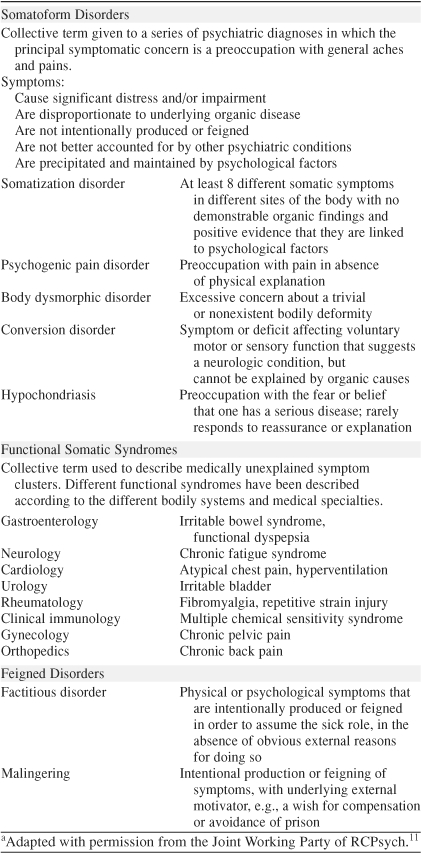
The redundancy of terms used in the medical literature to describe the somatic symptoms of depression is a reflection of the complicated processes of clinical decision making and differential diagnosis in psychiatry and primary care and the differences between the 2 settings. It is important that somatic symptoms associated with depression should not be confused with somatoform disorders, which comprise conversion, somatization, hypochondriasis, and, in particular, somatization disorder, a chronic disorder characterized by a combination of pain and gastrointestinal, sexual, and pseudoneurologic symptoms (Table 1).5,11,12 Differential diagnosis is confounded by the knowledge that there is a high prevalence of depression in patients with somatization disorder. Similarly, there are substantial levels of hypochondriacal, conversion, and somatizing symptoms in patients with depression.13–16 Indeed, results from several surveys suggest that depression, rather than somatoform disorders, may account for most of the somatization symptoms seen in primary care.17–19 Moreover, depressive disorders are common in patients with chronic pain, and pain is a frequent complaint in patients with depression (reviewed in Bair et al.1 and Smith20).
Table 1.
Terminology Used in Relation to Medically Unexplained Conditionsa
While the linguistic constructs of somatization disorder and somatoform disorder are familiar and serviceable tools for the psychiatrist, these diagnostic classifications are less widely used in primary care, in which somatic symptoms, such as general aches and pains, are frequently described as “medically unexplained physical complaints.” Lack of training or expertise is not an adequate explanation for the discrepancy in language between these 2 levels of care. Making a diagnosis in primary care differs from secondary care in that the primary care physician is aware of a patient's background and history. The categorical labels used by psychiatrists may, therefore, be inadequate for the needs of primary care physicians.21 Indeed, in primary care, patients present with individual, complex, and often poignant narratives, which encompass the domains of both mind and body, and are influenced by multiple social, economic, and other forces.21,22 In this setting, categorization can be seen to either trivialize or amplify a patient's problems by removing the context.
Somatic Symptoms Are Prevalent in Depression in Primary Care
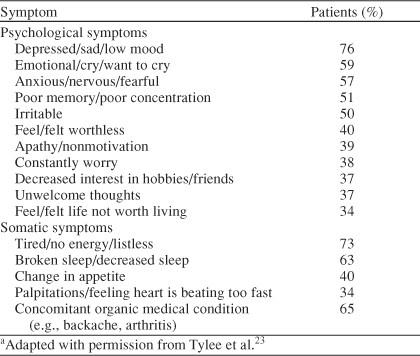
Patients with depression present with a combination of psychological and somatic symptoms. In primary care, somatic symptoms often dominate the clinical picture. During the second phase of the Depression Research in European Society II study (DEPRES II)—a pan-European survey of 1884 individuals previously receiving treatment for depression—2 of the 3 most common symptoms reported in current depressive episodes were somatic (Table 2).23 In another community study conducted by the World Health Organization (WHO),7 69% of participants (N = 1146) meeting criteria for major depression had approached their primary care physician on the basis of somatic symptoms alone, and more than half had multiple medically unexplained somatic symptoms. Similarly, during a retrospective examination of 685 primary care patients in Canada, 76% of patients who were diagnosed with depression or anxiety disorders (N = 75) had identified a somatic symptom as the primary reason for their initial visit to their primary care physician.8 More recently, a U.S. study conducted in 573 patients with depression reported that more than two thirds (69%) of the patients complained of general aches and pains of mild severity or above.24
Table 2.
Prevalence of Psychological and Somatic Symptoms in Patients With Depression During the Depression Research in European Society II Study (N = 1884)a
Somatic symptoms are more commonly reported by certain groups of patients with depression, including women,25,26 particularly pregnant women27; the elderly; those earning a lower income; children; culturally diverse populations; patients with coexisting organic conditions; and the imprisoned (reviewed in Stewart28). Certain cultural groups, including African Americans,29 have a tendency to mention somatic symptoms more frequently, or to focus more heavily on these symptoms when consulting their primary care physician.30–32 Culturally framed symptom interpretations, concepts of mental health, and social stigmas are chiefly responsible. In some countries, depression is seen as a moral or social problem, rather than a mental illness.31 Interestingly, the specific types of somatic symptoms reported by patients differ between cultures, reflecting cultural patterns of symptom significance—for example, abdominal distress, headaches, and neckaches are reported more frequently by patients with depression from Japan than those from the United States.33
The high prevalence of somatic symptoms in depression poses the question, “Can somatic symptoms be considered to be clinical predictors of underlying depression in primary care?” It is known that patients with somatic symptoms have a greater risk of developing depression.34–37 Similarly, patients with depression are more likely than their nondepressed counterparts to develop somatic symptoms in the long term.37,38 Furthermore, the greater the number of somatic symptoms, the greater the likelihood that an individual has depression.37,39,40 A recent study in 1143 Japanese white-collar workers found that the number of somatic symptoms identified on a 12-item somatic symptom checklist positively correlated with the prevalence of depression.39 Indeed, of 902 individuals who did not report any somatic symptoms, only 1 subject met criteria for major depression. Kroenke and colleagues40 also found that multiple somatic symptoms (i.e., 6 or more symptoms) were an independent predictor of depression and anxiety in a study of 500 adults attending a primary care clinic chiefly for somatic complaints. In an earlier study of 1042 consecutive outpatients screened for depressive disorders,41 discriminatory factors indicative of depression included sleep disturbance, fatigue, musculoskeletal complaints, and back pain.
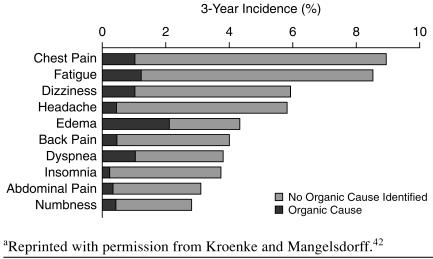
Nevertheless, it is still important to remember that not all somatic symptoms reported in primary care indicate a possible depression diagnosis. It is essential that physicians continue to investigate organic pathologies as the source of these complaints. In the event of medically unexplained complaints, however, a psychological cause should be considered. Indeed, studies show that most somatic symptoms reported by patients in primary care cannot be linked to an identifiable organic disease. Kroenke and Mangelsdorff42 demonstrated this succinctly during a retrospective review of 1000 patient records in which they examined the incidence, etiology, and outcome of 14 common somatic symptoms. Notably, these symptoms included 8 of the most common complaints reported in primary care. An organic cause for the symptoms was found in only 16% of cases (Figure 1); 10% of cases were thought to be of psychological origin; the rest were of unknown origin. Khan and colleagues43 made similar observations in a sample of 289 primary care patients with somatic symptoms; 48% of the symptoms were deemed to be of psychological or unknown origin.
Figure 1.
3-Year Incidence of 10 Common Somatic Symptoms and Proportion of Symptoms With a Suspected Organic Origin (N = 1000)a
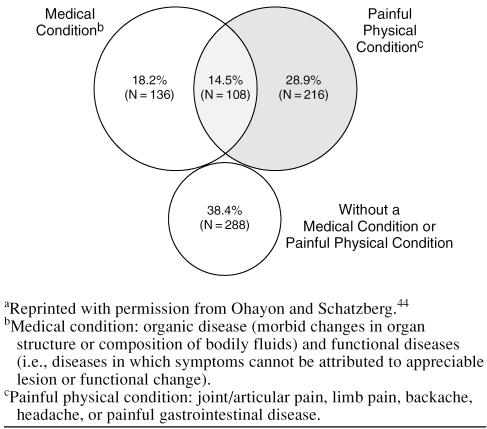
The relationship between general aches and pains, organic disease, and depression was explored during a cross-sectional telephone survey conducted by Ohayon and Schatzberg44 in 18,980 individuals across 5 European countries. In total, 748 participants (4%) in the study met criteria for major depressive disorder; of these, 43.4% had experienced headaches, gastrointestinal disturbances, and joint/articular, limb, or back aches, and 32.7% of patients had a coexisting organic condition. The organic condition, however, could explain the presence of pain in only one third of cases (Figure 2). These results suggest that if an organic condition presents that explains somatic symptoms, it is unlikely that the symptoms are somatized, even if depression exists; however, when an organic condition is present but not sufficient to explain the amount/quality of the somatic symptoms, depression may be playing a role.
Figure 2.
Prevalence of Somatic Symptoms and Organic Conditions in 748 Individuals With Major Depressive Disorder in Primary Carea
Somatic Symptoms Increase the Burden of Depression
Somatic symptoms increase the already marked burden and disability associated with depression. Data from the U.S. National Household Survey45—a cross-sectional community-based study of 1486 adults with major depression or dysthymia—found that patients with general aches and pains that included arthritic/rheumatic-like pain, back problems, and severe headaches (N = 938) had poorer physical and mental health status and reported more psychiatric distress than patients without general aches and pains.45 Ohayon and Schatzberg's large pan-European cross-sectional study44 demonstrated that depressive moods were prolonged in patients with general aches and pains by, on average, approximately 6 months.
While few studies have examined the effect of somatic symptoms in depression on quality of life, what is known is that patients with depression who achieve full remission following treatment demonstrate greater improvements in physical functioning than nonresponders.46 Addressing both the psychological and somatic symptoms of depression would appear, therefore, to be necessary to achieve and maintain remission.
The increased burden of somatic symptoms in patients with depression leads to increased utilization of health care services and greater economic burden.45,47–49 In the U.S. National Household Survey,45 depressed patients suffering from general aches and pains made approximately 20% more visits to their health care providers each year than those without aches and pains. Interestingly, these patients were 20% less likely to see a mental health specialist than patients who did not report general aches and pains. Clearly, the burden of treating these patients falls heavily on the primary care health system. Luber and colleagues49 also found that the presence of somatic symptoms, including general aches and pains, was predictive of increased total ambulatory costs in 3481 elderly patients at 1 primary care practice. The number of somatic symptoms correlated with service utilization costs. The economic burden of somatic symptoms in depression also extends to employers. A claims-based study in the United States showed that medical costs were elevated 2.8- and 4-fold in depressed patients with backache and migraine, respectively.50
Somatic Symptoms Decrease the Recognition of Depression
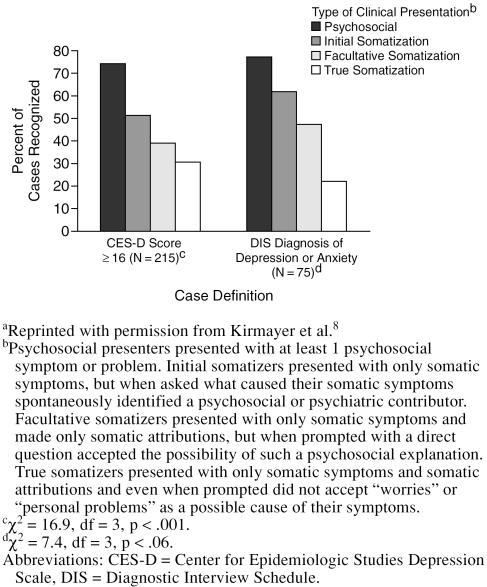
Although most primary care physicians are skilled at recognizing and treating depression, and most cases are eventually recognized, there is still some evidence of underrecognition and undertreatment, particularly at the initial clinic visit.4 While time constraints during consultations are doubtlessly a contributing factor, somatic presentation and failure to observe and respond to these cues during the patient interview are among the major reasons for underdiagnosis. Indeed, depression is less likely to be recognized in patients who present with somatic symptoms than in patients who present with predominantly psychological symptoms (Figure 3).6,8,51
Figure 3.
Effect of Clinical Presentation on Primary Care Physicians' Recognition of True Psychiatric Casesa
In 1985, Bridges and Goldberg10 reported that primary care physicians misdiagnosed more than 50% of psychiatric patients who presented with somatic symptoms. In 1993, during a retrospective examination of consecutive patients at 2 primary care clinics in Canada, Kirmayer and colleagues8 found that 78% of patients with major depression who had presented with a primary complaint of somatic symptoms had been misdiagnosed. The underlying reasons are complex, encompassing patient and physician characteristics, what patients say to their primary care physician, how and when they say it, and how the physician interviews the patient (reviewed in Docherty52 and Tylee53). Primary care physicians are often anxious not to miss a life-threatening organic condition, and those who are less confident in depression diagnoses will investigate somatic symptoms first—sometimes at length—before considering depression as the underlying cause.9
In primary care, the depressed patient's tendency to attribute unexplained somatic symptoms to a normalizing nonpathologic cause, rather than a psychological cause, is a principal driver in misdiagnosis.54–57 Physicians at 1 primary care practice in the United Kingdom failed to recognize depression (or anxiety) in 85% of patients with a normalizing attributional style, compared with 38% of patients with a psychologizing style.54 Furthermore, a questionnaire-based study conducted at 6 primary care practices in Australia found that depressed patients with an extreme normalizing style were 20 times less likely to receive a current depression diagnosis and 4 times less likely to receive a lifetime depression diagnosis compared to those with a low normalizing style.55 Interestingly, another U.K. study demonstrated that patients with more severe depression, which is recognized more frequently than mild to moderate forms in primary care, had higher psychologizing styles and lower normalizing styles.56
Stigmatization surrounding mental illness can make discussion of psychological issues uncomfortable, leading patients to normalize their symptoms. This is particularly apparent during initial visits to primary care physicians, before an intimate relationship and a feeling of trust have been established. Notably, in the WHO primary care study,7 a somatic presentation occurred more frequently in patients who did not have an ongoing relationship with their primary care physician.
Patients with depression are also acutely aware of time constraints during primary care consultations, a factor that can lead them to self-restrict the time spent explaining their symptoms.58 Short consultation times, combined with “competing demand” between somatic and psychological symptoms and the fear of stigma attached to a depression diagnosis, interact to decrease the chance that the condition is even discussed.59,60 If mentioned at all, patients frequently wait until toward the end of primary care consultations to share psychological concerns.61 This is a critical determinant in misdiagnosis. In 1 study,61 physicians from 36 primary care practices in the United Kingdom were 5 times less likely to recognize depression when psychological symptoms were mentioned late in the consultation, compared with when psychological symptoms were mentioned within the first 4 symptoms.
These data imply that the recognition of depression is patient-led. However, the way in which a primary care physician conducts the consultation and responds to the type and sequence of symptoms revealed by the patient also influences the likelihood that psychological symptoms are mentioned62 and ultimately, therefore, whether a diagnosis is made.63 Bucholz and Robins64 found that certain symptoms, such as loss of appetite or weight loss, and particular patient characteristics, such as being female or separated or widowed, appeared to encourage physicians to discuss depressive illness. A U.S. focus group study65 in which 21 primary care physicians considered approaches to depression diagnoses revealed that physicians tend to approach a depression diagnosis in 1 of 3 ways: by investigating somatic complaints first, by initially focusing on psychological symptoms, or by examining both psychological and somatic aspects in tandem. Patient characteristics and verbal, vocal (e.g., sighing), and postural cues determine which path is utilized.62 Some physicians are less likely to allow patients to express these cues. Closed, hypothesis-driven questioning, in particular, can suppress verbal cues given by the patients, discouraging them from revealing their psychological symptoms.62 A holistic and narrative approach that includes appropriately timed, open, and directive questions about psychological issues should be encouraged. Furthermore, physicians must apply equal diagnostic weighting to symptoms regardless of when they are mentioned.
Somatic Symptoms Complicate the Treatment of Depression
Patients with depression and somatic symptoms are harder to treat. Papakostas and colleagues66 showed that somatic symptoms were present in 95% of patients with treatment-resistant depression (N = 40) who had enrolled in a 6-week treatment study. Logistic regression analysis demonstrated that the number of somatic symptoms was a risk factor for further treatment resistance and tended to predict a poorer response to treatment. Indeed, the severity of somatic symptoms appears to be correlated to poor treatment response. Bair and colleagues24 used data from the ARTIST (A Randomized Trial Investigating SSRI Treatment) study—a randomized study with naturalistic follow-up conducted in the United States in 37 primary care clinics—to show that the severity of baseline general aches and pains could predict response to antidepressant treatment. More than two thirds of the depressed patients in this study reported general aches and pains of varying severity at baseline. Analysis of depression outcomes after 3 months of therapy with selective serotonin reup-take inhibitors revealed that patients with moderately severe aches and pains at baseline were 2 times less likely to respond to treatment. Patients with severe aches and pains at baseline were 4.1 times less likely to respond to treatment.
Interestingly, in the ARTIST study, residual general aches and pains of mild severity or above were present in 58% of patients with depression after 3 months of antide-pressant treatment.24 Residual depressive symptoms are known for their association with poor outcome in depression. In a study of 60 patients treated to remission and then followed up for 15 months, Paykel and colleagues67 found that 19 patients had residual depressive symptoms; the most common residual symptoms were somatic, occurring in 18 (95%) of the 19 patients. Relapse occurred in 76% of patients with residual symptoms who were available for follow-up, compared with only 25% of patients without residual symptoms (10/40 patients). Indeed, patients with residual symptoms relapsed almost 3 times faster than those without.
A naturalistic long-term follow-up of these patients showed that subjects remitting with residual symptoms continued to have more depressive symptoms and impairment to their global, social, leisure, and work functioning over the long term.68 There was a trend toward earlier recurrence in patients with residual symptoms compared to those without; 42% and 56% of patients with residual symptoms recurred within 1 and 2 years, respectively, compared with 20% and 42% of patients without.
Implications of Somatic Symptoms in Depression: Can Training Help?
It is important that primary care physicians acquire specific skills for the recognition of depression. To date, there has been a tendency to focus on the psychological symptoms of depression rather than the somatic symptoms. Indeed, during a recent Australian primary care survey,69 only one quarter of physicians reported basing a diagnosis of depression on somatic symptoms (e.g., vegetative symptoms, malaise, and multiple consultations). Even if depression is recognized in patients with somatic symptoms, the focus on and severity of somatic symptoms can detract from a patient's willingness to comply with treatment.59 Improved awareness of the importance of somatic symptoms in depression among primary care physicians, refined interviewing techniques, and training schemes that focus on teaching patients to reattribute somatic causality may help.
Perhaps one of the most important steps in ensuring the success of educational intervention is directing it to where it is most needed. Low prevalence rates for depression, high levels of medically unexplained somatic symptoms, and low antidepressant prescription rates are useful predictors of sectors of the primary health care system in which training may be warranted.70 With increasing numbers of patients with depression now having initial contact with a practice nurse rather than a physician and the implementation by the U.K. National Health Service (NHS) of NHS Direct (a nurse-led service), training in recognition of depression is vital among this staff group; detection rates for depression have been shown to be low among practice nurses.71 Indeed, nurses' confidence in dealing with depressed patients has been shown to improve following training.72
Encouraging results have been seen in the past when educational initiatives were used to improve the recognition of depression in primary care. The most prominent data came from a program instigated by the Swedish Committee for the Prevention and Treatment of Depression during the 1980s on the island of Gotland.73 Improving primary care physicians' knowledge of the diagnosis and treatment of depression by means of 2-day seminars led to improved recognition rates for depression, coupled with significant decreases in inpatient care, morbidity, mortality, and costs.73 Over a 3-year evaluation period, an overall economic benefit of $26 million was noted.74 The Defeat Depression Campaign, successfully implemented in the United Kingdom during the 1990s, was one of several international educational initiatives that used the Gotland study as a model.75 A primary care survey conducted in 1996 at the end of the campaign showed a positive impact of the national initiative, but also highlighted a need for supplementary local and practice-based training.76
In contrast to the Gotland study, the Hampshire Depression Project, which used seminar-based education to improve knowledge of current best practice guidelines for depression,77 failed to increase the sensitivity or specificity of the recognition of depressive symptoms.78 Notably, the Hospital Anxiety and Depression Scale (HADS)79 was used to confirm the presence of substantial depressive symptoms in this study. Despite its widespread use, the HADS excludes somatic symptoms.79,80
None of these studies focused specifically on education about somatic symptoms in depression as a means to improve recognition. Nevertheless, their results convey useful lessons for the design of future educational programs. Indeed, while pronounced effects on the recognition of depression were clearly evident following the short-term educational program in Gotland, improvements had reverted to baseline values within 3 years, illustrating the need to repeat educational initiatives every couple of years to maintain long-term effects.81
Several studies have examined the effect of training primary care physicians in reattribution skills as a method of improving the recognition of depression. As discussed previously, in primary care, patients with depression tend to attribute somatic symptoms to normalizing causes.54–56 Teaching patients to reattribute somatic symptoms to psychological problems entails making patients feel understood (in particular, their beliefs about the cause of their symptoms), providing feedback on the results of their physical examinations and medical history while offering a tentative suggestion that somatic symptoms may be linked to psychological and lifestyle factors (i.e., changing the agenda), and then, if the patient seems willing to accept this suggestion, fully explaining the link between the somatic symptoms and the psychological cause. In essence, primary care physicians must try to find explanations compatible with the patient's experience of illness that may change his or her belief about the cause.
Training primary care physicians in reattribution skills has been shown to improve interviewing and specific reattribution ability, leading to improvements in patient-doctor communication.82–85 In 1 study,85 separate cohorts of 103 and 112 patients visited 8 primary care physicians before and after the physicians had undergone an 8-hour reattribution skills training program. Patients reported greater satisfaction with the service they received (i.e., they felt that they had received the help they had wanted) and attributed psychological symptoms less to somatic causes when visiting primary care physicians who had undergone reattribution training.85 Overall, the technique was cost-effective.83 Although primary care costs did not change, the cost of referrals to secondary care, external health providers, and private health care decreased by 23%. A study of the effectiveness of a training course to educate primary care registrars in reattribution skills in somatizing patients is ongoing. The results of this study are awaited with interest.
DISCUSSION
In general, both patients and physicians appear to have a set agenda of issues to discuss during a primary care visit. Some problems are addressed, while others are left to subsequent visits, if addressed at all. When depression is present, somatic complaints often dominate the clinical picture, impeding the discussion of psychological complaints and thus masking the depression diagnosis. The failure to recognize depression in these cases is largely a consequence of patient-related barriers, in particular, normalizing attributional style; however, specific physician-related barriers, such as the inability to elicit psychological symptoms or respond to verbal/nonverbal cues during the consultation, also contribute.
Failure to recognize somatic symptoms, such as low energy, sleep disturbance, reduced appetite and libido, and general aches and pains, as components of depressive illness is associated with significant health care expenditure. Depressed patients with somatic symptoms usually feel a greater burden of disease and consequently tend to rely heavily on primary care services. In addition, in many cases, patients are subjected to costly and time-consuming investigations to determine whether organic conditions underlie their symptoms.
Traditionally used criteria for depression may be partly to blame for the lack of awareness that surrounds the importance of somatic symptoms in depression. Until their recent revision, DSM-IV criteria for major depressive disorder did not include any mention of somatic symptoms. Widely used rating scales, such as the HADS, were even refined during their development to exclude somatic symptoms in order that diagnosis should not be overcomplicated.
The American Psychiatric Association's recent revision of DSM-IV criteria (DSM-IV-TR)5 to include somatic symptoms as a symptom of depression is indicative of an increasing awareness of the importance of somatic symptoms in depression. The new criteria refer to “excessive worry over physical health and complaints of pain (e.g., headaches or joint, abdominal, or other pains)”5(p352) among the associated features of major depressive disorder. Indeed, guidelines currently in development at the National Institute of Clinical Excellence in the United Kingdom for the management of depression define the condition as low mood and a range of emotional, cognitive, physical (i.e., somatic), and behavioral symptoms.
A holistic approach to recognition is clearly necessary, and primary care physicians need to have a high index of suspicion for depression when faced with medically unexplained somatic symptoms, including general aches and pains and lack of energy. Educational initiatives that raise awareness of the full spectrum of symptoms in depression, as well as aiming to improve attitudes and consulting skills in primary care, should be of benefit.
Footnotes
Funding for this review was provided by Eli Lilly and Company Limited, Basingstoke, Hampshire, and Boehinger Ingelheim Limited, Bracknell, Berkshire, U.K.
Limited information from this review has been presented previously in a short editorial article in Primary Care Mental Health (Tylee A, Ghandi P. Somatic symptoms and general aches and pains in primary care: indicators for depression? Primary Care Mental Health 2004;2:133–136).
Dr. Tylee has acted over many years as an ad hoc consultant for most of the drug companies that make antidepressants. Dr. Gandhi is currently an employee of Eli Lilly and Company Limited.
REFERENCES
- Bair MJ, Robinson RL, and Katon W. et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003 163:2433–2445. [DOI] [PubMed] [Google Scholar]
- Zung WW, Broadhead WE, Roth ME. Prevalence of depressive symptoms in primary care. J Fam Pract. 1993;37:337–344. [PubMed] [Google Scholar]
- Ayuso-Mateos JL, Vazquez-Barquero JL. Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry. 2001;179:308–316. doi: 10.1192/bjp.179.4.308. [DOI] [PubMed] [Google Scholar]
- Kessler D, Bennewith O, and Lewis G. et al. Detection of depression and anxiety in primary care: follow up study. BMJ. 2002 325:1016–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association. 2003 [Google Scholar]
- NICE Draft Guidelines. December 2003. Depression: the Management of Depression in Primary and Secondary Care. London, UK: National Institute for Clinical Excellence. 2003 [Google Scholar]
- Simon GE, VonKorff M, and Piccinelli M. et al. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999 341:1329–1335. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Robbins JM, and Dworkind M. et al. Somatisation and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993 150:734–741. [DOI] [PubMed] [Google Scholar]
- Schulberg HC, McClelland M. A conceptual model for educating primary care providers in the diagnosis and treatment of depression. Gen Hosp Psychiatry. 1987;9:1–10. doi: 10.1016/0163-8343(87)90094-6. [DOI] [PubMed] [Google Scholar]
- Bridges KW, Goldberg DP. Somatic presentation of DSM-III psychiatric disorders in primary care. J Psychopharmacol Res. 1985;29:563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- Joint Working Party of RCPsych. The Psychological Care of Medical Patients. London, UK: Royal College of Psychiatry. 2003 [Google Scholar]
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorders. Geneva, Switzerland: World Health Organization. 1992 [Google Scholar]
- Kirmayer LJ, Robbins JM. Three forms of somatization in primary care: prevalence, co-occurrence, and sociodemographic characteristics. J Nerv Ment Dis. 1991;179:646–655. doi: 10.1097/00005053-199111000-00001. [DOI] [PubMed] [Google Scholar]
- Robbins JM, Kirmayer LJ. Transient and persistent hypochondriacal worry in primary care. Psychol Med. 1996;26:575–589. doi: 10.1017/s0033291700035650. [DOI] [PubMed] [Google Scholar]
- Keeley R, Smith M, Miller J. Somatoform symptoms and treatment non-adherence in depressed family medicine outpatients. Arch Fam Med. 2000;9:46–54. doi: 10.1001/archfami.9.1.46. [DOI] [PubMed] [Google Scholar]
- Fisch RZ. Masked depression: its interrelations with somatization, hypochondriasis and conversion. Int J Psychiatry Med. 1987;17:367–379. doi: 10.2190/cr7j-wu5n-hc5x-2jq5. [DOI] [PubMed] [Google Scholar]
- Katon W, Russo J. Somatic symptoms and depression. J Fam Pract. 1989;29:65–69. [PubMed] [Google Scholar]
- Mathews RJ, Weinman ML, Mirabi M. Physical symptoms of depression. Br J Psychiatry. 1981;139:293–296. [PubMed] [Google Scholar]
- Waxman HM, McCreary G, and Weinrit RM. et al. A comparison of somatic complaints among depressed and nondepressed older persons. Gerontologist. 1985 25:501–507. [DOI] [PubMed] [Google Scholar]
- Smith GR. The epidemiology and treatment of depression when it coexists with somatoform disorders, somatization, or pain. Gen Hosp Psychiatry. 1992;14:265–272. doi: 10.1016/0163-8343(92)90097-t. [DOI] [PubMed] [Google Scholar]
- Launer J. A narrative approach to mental health in general practice. BMJ. 1999;318:117–119. doi: 10.1136/bmj.318.7176.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B, Nolan P, and Crawford P. et al. Interaction, language and the “narrative turn” in psychotherapy and psychiatry. Soc Sci Med. 1996 43:1569–1578. [DOI] [PubMed] [Google Scholar]
- Tylee A, Gastpar M, and Lepine JP. et al. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability, and current management of depression in the community. DEPRES Steering Committee. Int Clin Psychopharmacol. 1999 14:139–151. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, and Eckert GJ. et al. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004 66:17–22. [DOI] [PubMed] [Google Scholar]
- Silverstein B. Gender difference in the prevalence of clinical depression: the role played by depression associated with somatic symptoms. Am J Psychiatry. 1999;156:480–482. doi: 10.1176/ajp.156.3.480. [DOI] [PubMed] [Google Scholar]
- Betrus PA, Elmore SK, Hamilton PA. Women and somatization: unrecognized depression. Health Care Women Int. 1995;16:287–297. doi: 10.1080/07399339509516182. [DOI] [PubMed] [Google Scholar]
- Kelly RH, Russo J, Katon W. Somatic complaints among pregnant women cared for in obstetrics: normal pregnancy or depressive and anxiety symptom amplification revisited? Gen Hosp Psychiatry. 2001;23:107–113. doi: 10.1016/s0163-8343(01)00129-3. [DOI] [PubMed] [Google Scholar]
- Stewart DE. Physical symptoms of depression: unmet needs in special populations. J Clin Psychiatry. 2003 64suppl 7. 12–16. [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ. Clinical presentations of major depression by African Americans and whites in primary medical care practice. J Affect Disord. 1996;41:181–191. doi: 10.1016/s0165-0327(96)00085-7. [DOI] [PubMed] [Google Scholar]
- Parker G, Cheah YC, Roy K. Do the Chinese somatize depression? a cross-cultural study. Soc Psychol Psychiatr Epidemiol. 2001;26:287–293. doi: 10.1007/s001270170046. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: implications for diagnosis and treatment. J Clin Psychiatry. 2001 62suppl 13. 22–30. [PubMed] [Google Scholar]
- Britton EL, Lawrenson RA, Fuller AJ. The prevalence of depression in Turkish speaking patients in an East London general practice. Prim Care Psychiatry. 2000;6:33–36. [Google Scholar]
- Waza K, Graham AV, and Zyzanski SJ. et al. Comparison of symptoms in Japanese and American depressed primary care patients. Fam Pract. 1999 16:528–533. [DOI] [PubMed] [Google Scholar]
- Terre L, Poston WS, Foreyt J. Do somatic complaints predict subsequent symptoms of depression? Psychother Psychosom. 2003;72:261–267. doi: 10.1159/000071897. [DOI] [PubMed] [Google Scholar]
- Barkow K, Heun R, and Ustun TB. et al. Identification of items which predict later development of depression in primary health care. Eur Arch Psychiatry Clin Neurosci. 2001 251suppl 2. 21–26. [DOI] [PubMed] [Google Scholar]
- Patten SB. Long-term medical conditions and major depression in a Canadian population study at waves 1 and 2. J Affect Disord. 2001;63:35–41. doi: 10.1016/s0165-0327(00)00186-5. [DOI] [PubMed] [Google Scholar]
- Hotopf M, Mayou R, and Wadsworth M. et al. Temporal relationships between physical symptoms and psychiatric disorders: results from a national birth cohort. Br J Psychiatry. 1998 173:255–261. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: a prospective study of depression as a risk factor. Pain. 1993;55:251–258. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- Nakao M, Yano E. Reporting of somatic symptoms as a screening marker for detecting major depression in a population of Japanese white-collar workers. J Clin Epidemiol. 2003;56:1021–1026. doi: 10.1016/s0895-4356(03)00154-9. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med. 1997;103:339–347. doi: 10.1016/s0002-9343(97)00241-6. [DOI] [PubMed] [Google Scholar]
- Gerber PD, Barrett JE, and Barrett JA. et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med. 1992 7:170–173. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- Khan AA, Khan A, and Harezlak J. et al. Somatic symptoms in primary care: etiology and outcome. Psychosomatics. 2003 44:471–478. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60:39–47. doi: 10.1001/archpsyc.60.1.39. [DOI] [PubMed] [Google Scholar]
- Bao Y, Sturm R, Croghan TW. A national study of the effect of chronic pain on the use of health care by depressed persons. Psychiatr Serv. 2003;54:693–697. doi: 10.1176/appi.ps.54.5.693. [DOI] [PubMed] [Google Scholar]
- Doraiswamy P, Khan ZM, and Donahue RMJ. et al. Quality of life in geriatric depression: a comparison of remitters, partial responders, and non-responders. Am J Geriatr Psychiatry. 2001 9:423–428. [PubMed] [Google Scholar]
- Fifer SK, Buesching DP, and Henke CJ. et al. Functional status and somatization as predictors of medical offset in anxious and depressed patients. Value Health. 2003 6:40–50. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Leong SA, and Birnbaum HG. et al. The economic burden of depression with painful symptoms. J Clin Psychiatry. 2003 64suppl 7. 17–23. [PubMed] [Google Scholar]
- Luber MP, Meyers BS, and Williams-Russo PG. et al. Depression and service utilization in elderly primary care patients. Am J Geriatr Psychiatry. 2001 9:169–176. [PubMed] [Google Scholar]
- Sheehan DV. Establishing the real cost of depression. Manag Care. 2002;11:7–10. [PubMed] [Google Scholar]
- Magruder-Habib K, Zung WW, Feussner JR. Improving physicians' recognition and treatment of depression in general medical care: results of a randomized clinical trial. Med Care. 1990;28:239–250. doi: 10.1097/00005650-199003000-00004. [DOI] [PubMed] [Google Scholar]
- Docherty JP. Barriers to the diagnosis of depression in primary care. J Clin Psychiatry. 1997 58suppl 1. 5–10. [PubMed] [Google Scholar]
- Tylee A. Depression in the community: physician and patient perspective. J Clin Psychiatry. 1999 60suppl 7. 12–16. [PubMed] [Google Scholar]
- Kessler D, Lloyd K, and Lewis G. et al. Cross sectional study of symptom attribution and recognition of depression and anxiety in primary care. BMJ. 1999 318:436–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G, Parker K. Influence of symptom attribution on reporting depression and recourse to treatment. Aust N Z J Psychiatry. 2003;37:469–474. doi: 10.1046/j.1440-1614.2003.01205.x. [DOI] [PubMed] [Google Scholar]
- Bower P, West R, and Tylee A. et al. Symptom attribution and the recognition of psychiatric morbidity. J Psychosom Res. 2000 48:157–160. [DOI] [PubMed] [Google Scholar]
- Robbins JM, Kirmayer LJ. Attributions of common somatic symptoms. Psychol Med. 1991;21:1029–1045. doi: 10.1017/s0033291700030026. [DOI] [PubMed] [Google Scholar]
- Pollock K, Grime J. Patients' perceptions of entitlement to time in general practice consultations for depression: qualitative study. BMJ. 2002;325:687. [PMC free article] [PubMed] [Google Scholar]
- Nutting PA, Rost K, and Smith J. et al. Competing demands from physical problems: effect on initiating and completing depression care over 6 months. Arch Fam Med. 2000 9:1059–1064. [DOI] [PubMed] [Google Scholar]
- Rost K, Nutting P, and Smith J. et al. The role of competing demands in the treatment provided to primary care patients with major depression. Arch Fam Med. 2000 9:150–154. [DOI] [PubMed] [Google Scholar]
- Tylee A, Freeling P, and Kerry S. et al. How does the content of consultations affect the recognition by general practitioners of major depression in women? Br J Gen Pract. 1995 45:575–578. [PMC free article] [PubMed] [Google Scholar]
- Davenport S, Goldberg D, Millar T. How psychiatric disorders are missed during medical consultations. Lancet. 1987;2:439–441. doi: 10.1016/s0140-6736(87)90970-6. [DOI] [PubMed] [Google Scholar]
- Marks JN, Goldberg DP, Hillier VF. Determinants of the ability of general practitioners to detect psychiatric illness. Psychol Med. 1979;9:337–353. doi: 10.1017/s0033291700030853. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Robins LN. Who talks to a doctor about existing depressive illness? J Affect Disord. 1987;12:241–250. doi: 10.1016/0165-0327(87)90033-4. [DOI] [PubMed] [Google Scholar]
- Carney PA, Rhodes LA, and Eliassen MS. et al. Variations in approaching the diagnosis of depression: a guided focus group study. J Fam Pract. 1998 46:73–82. [PubMed] [Google Scholar]
- Papakostas GI, Petersen T, and Denninger J. et al. Somatic symptoms in treatment-resistant depression. Psychiatry Res. 2003 118:39–45. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Ramana R, and Cooper Z. et al. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995 25:1171–1180. [DOI] [PubMed] [Google Scholar]
- Kennedy N, Paykel ES. Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord. 2004;80:135–144. doi: 10.1016/S0165-0327(03)00054-5. [DOI] [PubMed] [Google Scholar]
- Krupinski J, Tiller JWG. The identification and treatment of depression by general practitioners. Aust N Z J Psychiatry. 2002;35:827–832. doi: 10.1046/j.1440-1614.2001.00960.x. [DOI] [PubMed] [Google Scholar]
- Rutz W. Improvement of care for people suffering from depression: the need for comprehensive education. Int Clin Psychopharmacol. 1999 14suppl 3. S27–S33. [DOI] [PubMed] [Google Scholar]
- Plummer SE, Gournay K, and Goldberg D. et al. Detection of psychological distress by practice nurses in general practice. Psychol Med. 2000 30:1233–1237. [DOI] [PubMed] [Google Scholar]
- Payne F, Harvey K, and Jessopp L. et al. Knowledge, confidence and attitudes towards mental health of nurses working in NHS Direct and the effects of training. J Adv Nurs. 2002 40:549–559. [DOI] [PubMed] [Google Scholar]
- Rutz W, Walinder J, and Eberhard G. et al. An educational program on depressive disorders for general practitioners on Gotland: background and evaluation. Acta Psychiatr Scand. 1989 79:19–26. [DOI] [PubMed] [Google Scholar]
- Rutz W, Carlsson P, and von Knorring L. et al. Cost-benefit analysis of an educational program for general practitioners by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992 85:457–464. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Tylee A, and Wright A. et al. The Defeat Depression Campaign: psychiatry in the public arena. Am J Psychiatry. 1997 154suppl 6. 59–65. [DOI] [PubMed] [Google Scholar]
- Rix S, Paykel ES, and Lelliott P. et al. Impact of a national campaign on GP education: an evaluation of the Defeat Depression Campaign. Br J Gen Pract. 1999 49:99–102. [PMC free article] [PubMed] [Google Scholar]
- Stevens L, Kinmonth A-L, and Peveler RC. et al. The Hampshire Depression Project: development and piloting of clinical practice guidelines and education about depression in primary health care. Med Educ. 1997 31:375–379. [DOI] [PubMed] [Google Scholar]
- Thompson C, Kinmonth AL, and Stevens L. et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000 355:185–191. [DOI] [PubMed] [Google Scholar]
- Snaith RP. The Hospital Anxiety and Depression Scale [editorial] Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Rutz W, von Knorring L, Walinder J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992;85:83–88. doi: 10.1111/j.1600-0447.1992.tb01448.x. [DOI] [PubMed] [Google Scholar]
- Kaaya S, Goldberg D, Gask L. Management of somatic presentations of psychiatric illness in general medical settings: evaluation of a new training course for general practitioners. Med Educ. 1992;26:138–144. doi: 10.1111/j.1365-2923.1992.tb00139.x. [DOI] [PubMed] [Google Scholar]
- Morriss RK, Gask L, and Ronalds C. et al. Clinical and patient satisfaction outcomes of a new treatment for somatized mental disorder taught to general practitioners. Br J Gen Pract. 1999 49:263–267. [PMC free article] [PubMed] [Google Scholar]
- Gask L, Goldberg D, and Porter R. et al. The treatment of somatization: evaluation of a training package with general practice trainees. J Psychosom Res. 1989 33:697–703. [DOI] [PubMed] [Google Scholar]
- Morriss RK, Gask L. Treatment of patients with somatized mental disorder: effects of reattribution training on outcomes under the direct control of the family doctor. Psychosomatics. 2002;43:394–399. doi: 10.1176/appi.psy.43.5.394. [DOI] [PubMed] [Google Scholar]