Abstract
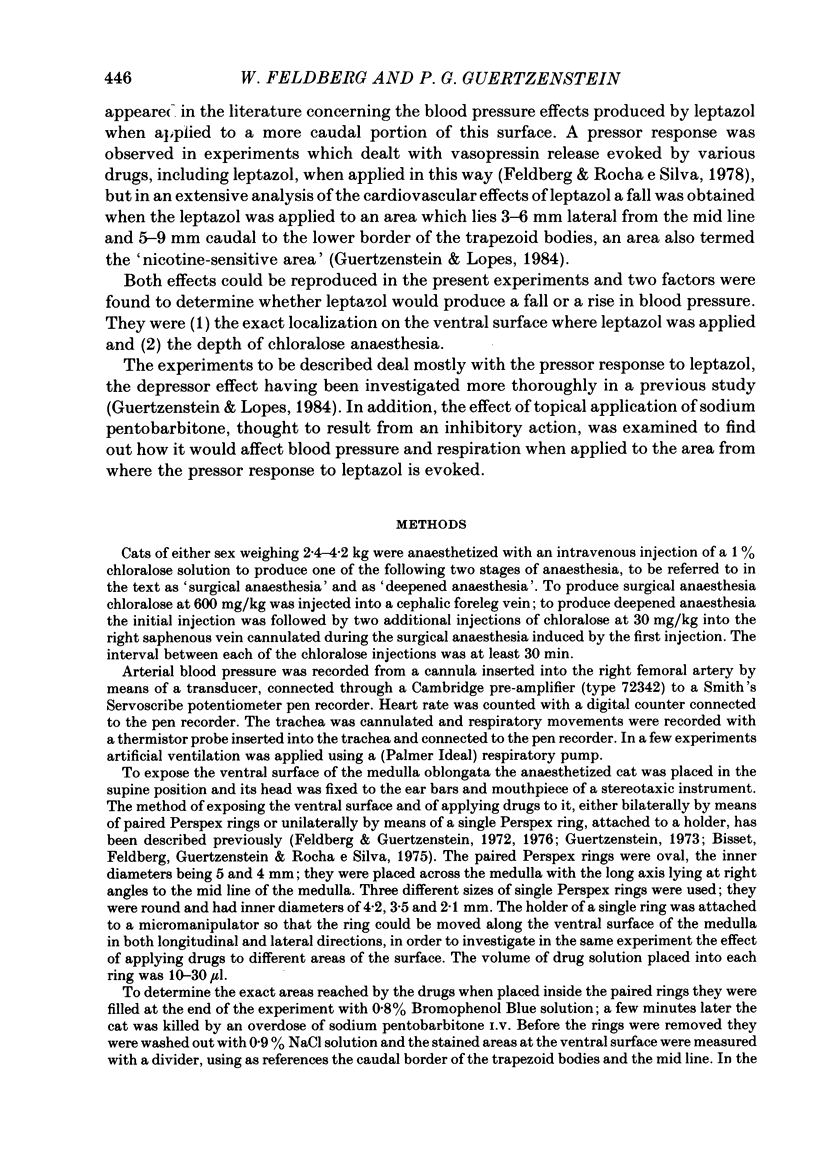
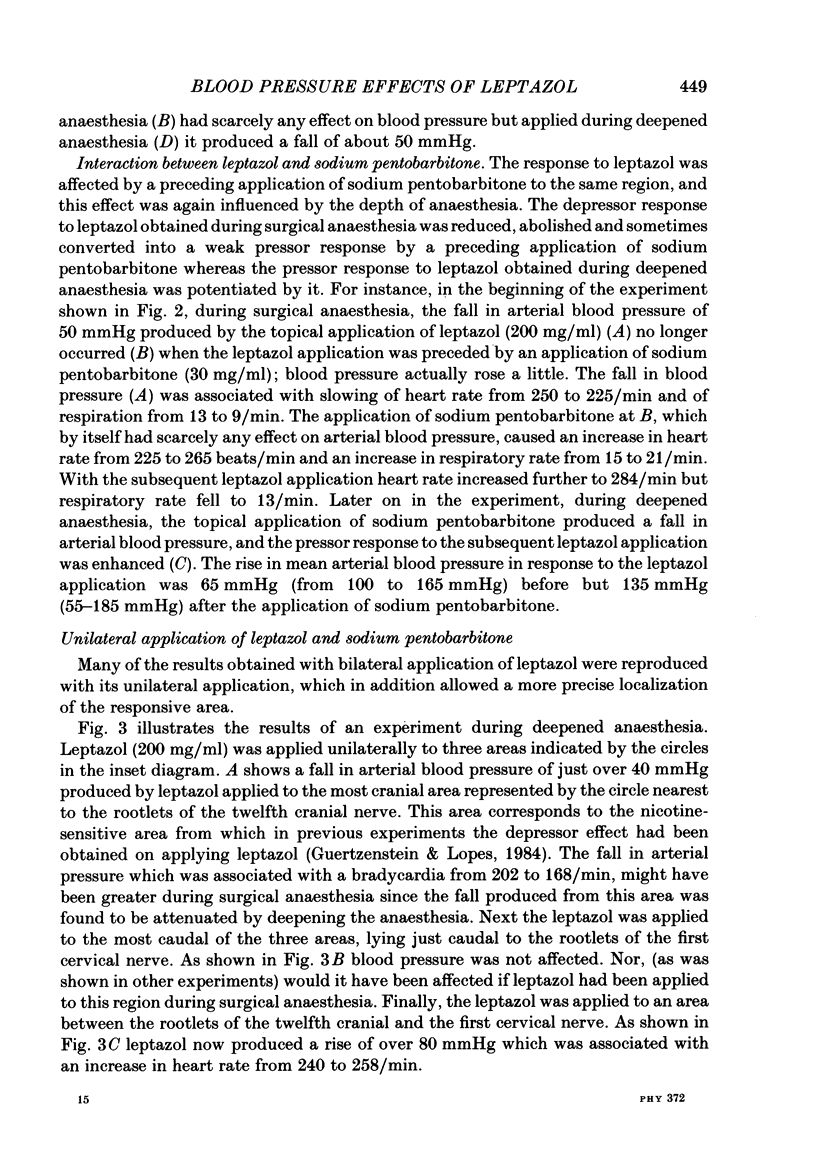
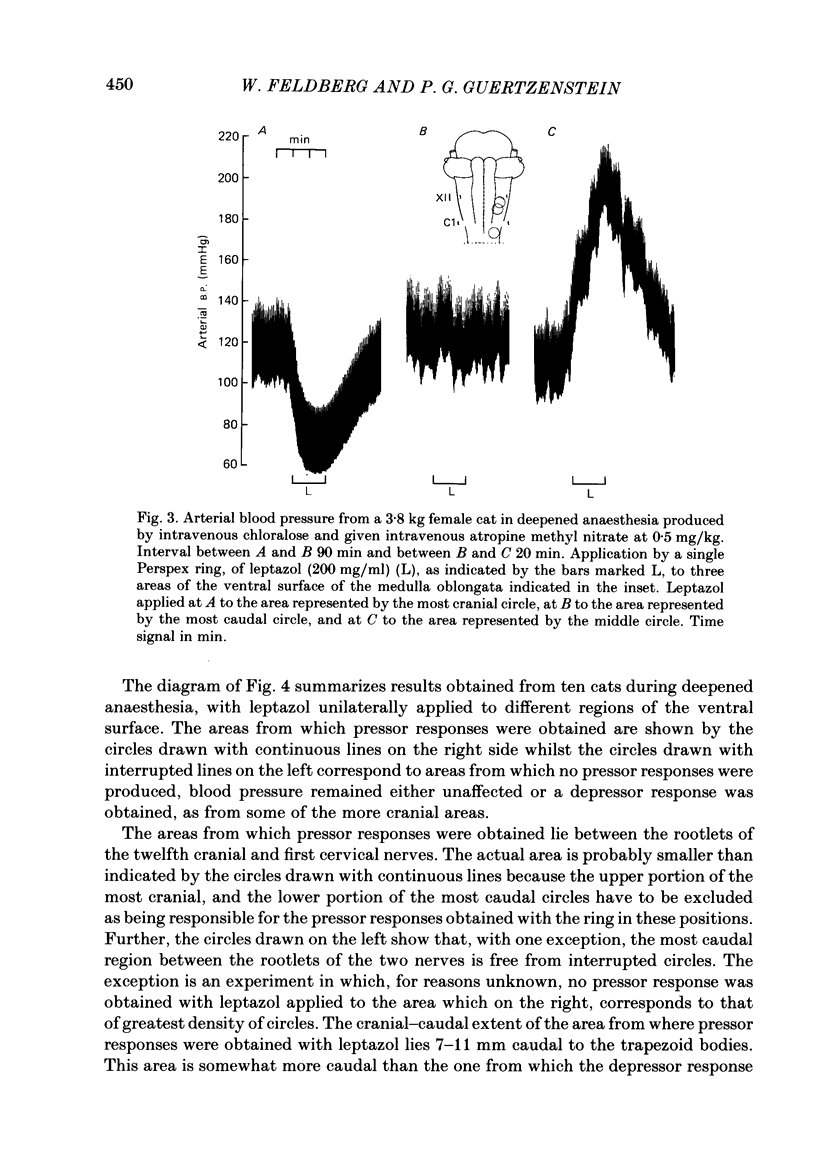
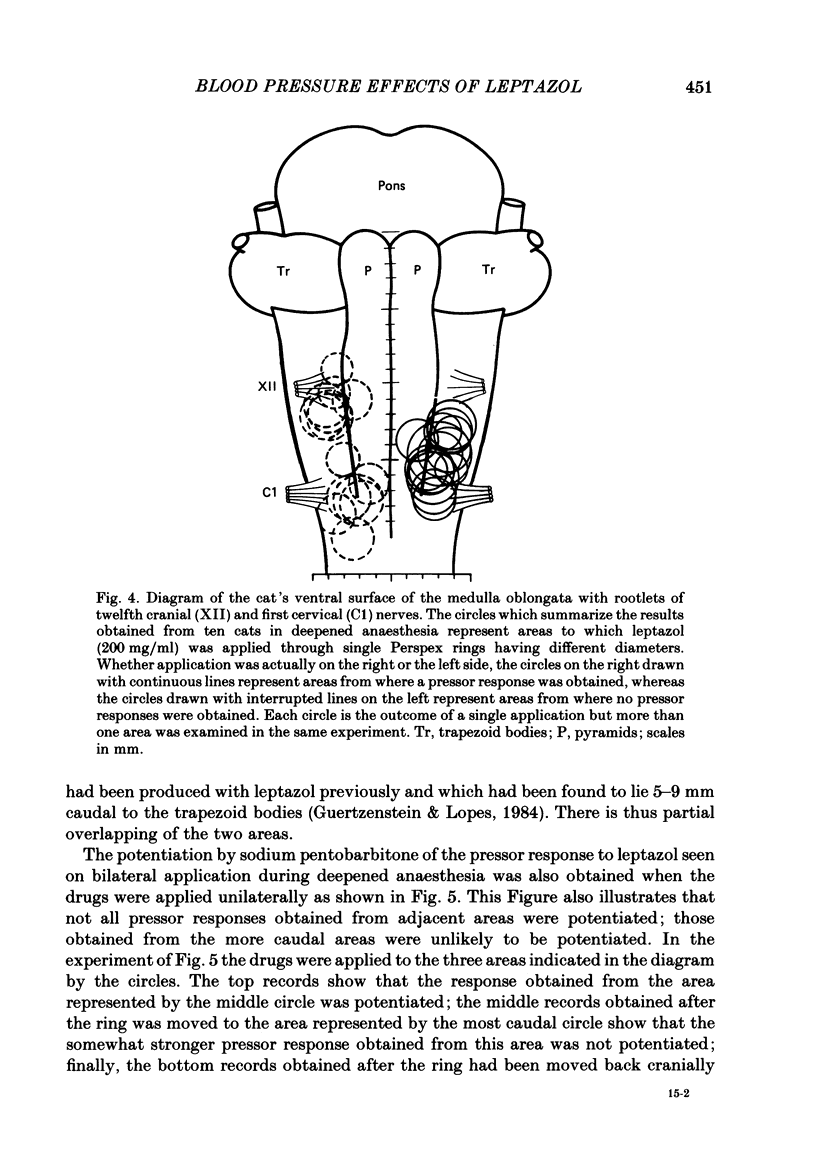
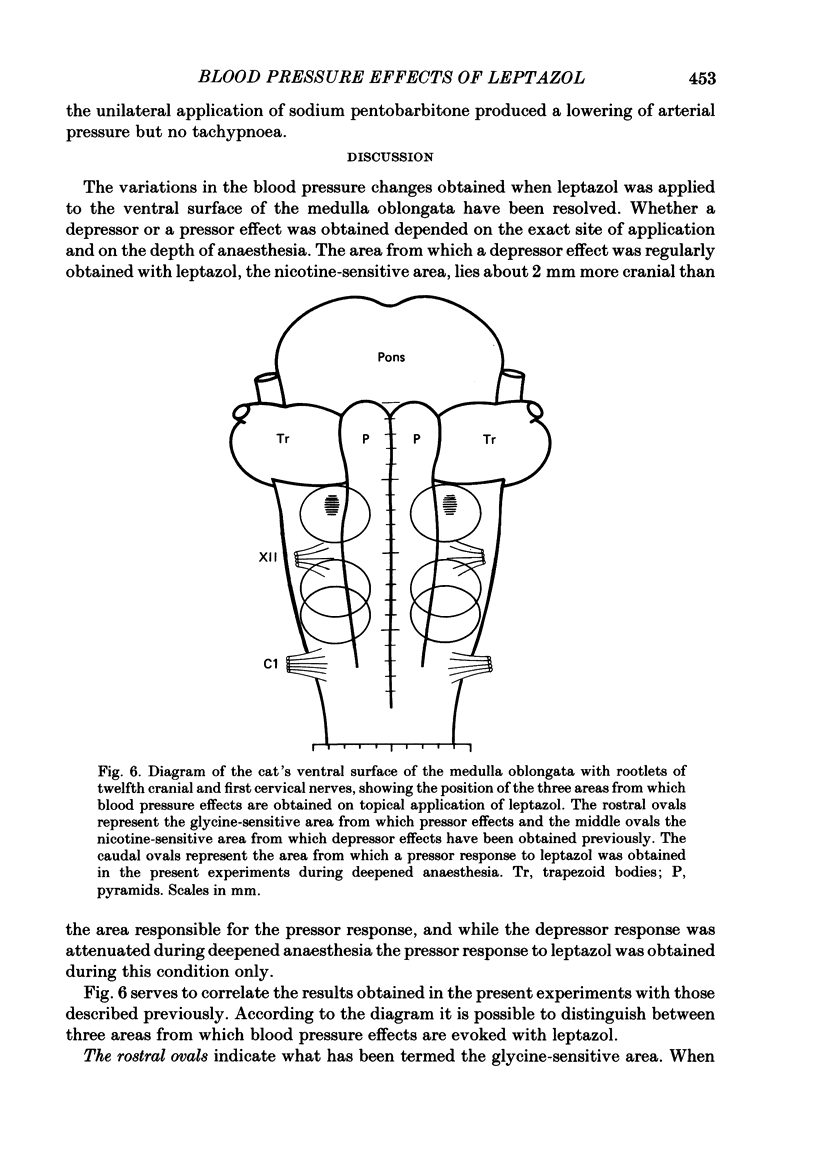
In anaesthetized cats leptazol (200 mg/ml) and sodium pentobarbitone (30 mg/ml) were applied topically to an area of the exposed ventral surface of the medulla oblongata, which lies between the rootlets of the twelfth cranial and first cervical nerve. The drugs were applied either bilaterally by means of paired Perspex rings or unilaterally by means of a single Perspex ring. Their effects on arterial blood pressure, heart rate and respiration were examined during two stages of anaesthesia, during 'surgical anaesthesia' produced by an intravenous injection of chloralose at 60 mg/kg, and during deeper anaesthesia attained by two additional intravenous injections of chloralose at 30 mg/kg. Both the bilateral and unilateral application of leptazol produced a fall in arterial blood pressure during surgical anaesthesia, but a rise during deepened anaesthesia. After a preceding topical application of sodium pentobarbitone the fall became attenuated or abolished, whereas the rise became potentiated. Sodium pentobarbitone itself affected blood pressure as well as respiration when applied bilaterally. It then produced pronounced tachypnoea independent of the depth of anaesthesia and a fall in arterial blood pressure during deepened anaesthesia. Its unilateral application did not affect respiration, nor did it affect usually arterial blood pressure, although during deepened anaesthesia it occasionally produced a fall in blood pressure. The area from which the pressor response to leptazol was obtained lay 7-11 mm caudal to the lower border of the trapezoid bodies, i.e. about 2 mm more caudally than the 'nicotine-sensitive area' from which a depressor response to leptazol is evoked. Thus the two areas, though not identical, overlap. The result obtained with sodium pentobarbitone suggest that the area for the pressor response to leptazol plays a role in maintaining vasomotor tone during deepened anaesthesia and exerts a strong inhibitory effect on the respiratory rate during both surgical and deepened anaesthesia.
Full text
PDF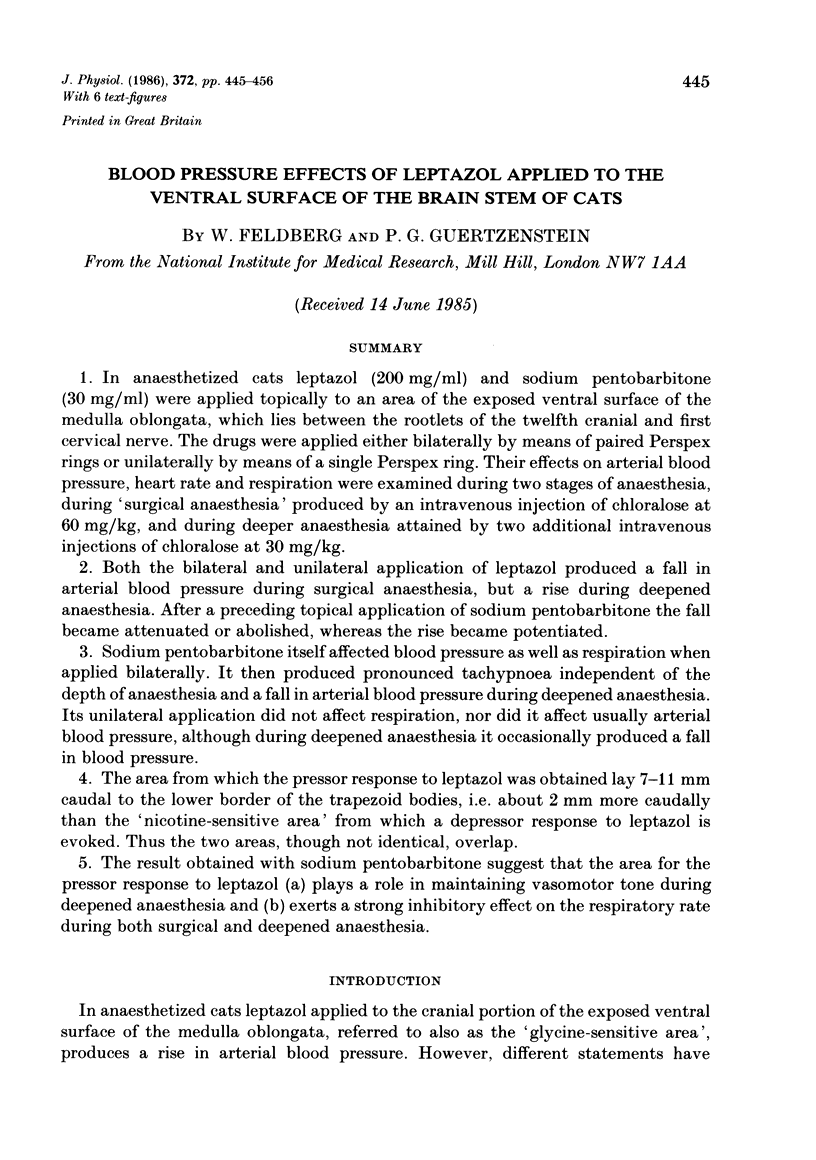

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Feldberg W., Guertzenstein P. G. A vasodepressor effect of pentobarbitone sodium. J Physiol. 1972 Jul;224(1):83–103. doi: 10.1113/jphysiol.1972.sp009882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldberg W., Guertzenstein P. G., Rocha e Silva M., Jr Vasopressin release by nicotine: the site of action. Br J Pharmacol. 1975 Aug;54(4):463–474. doi: 10.1111/j.1476-5381.1975.tb07592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldberg W., Guertzenstein P. G. Vasodepressor effects obtained by drugs acting on the ventral surface of the brain stem. J Physiol. 1976 Jun;258(2):337–355. doi: 10.1113/jphysiol.1976.sp011423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldberg W., Rocha e Silva M., Jr Inhibition of vasopressin release to carotid occlusion by gamma-aminobutyric acid and glycine. Br J Pharmacol. 1981 Jan;72(1):17–24. doi: 10.1111/j.1476-5381.1981.tb09099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldberg W., Rocha e Silva M., Jr Vasopressin release produced in anaesthetized cats by antagonists of gamma-aminobutyric acid and glycine. Br J Pharmacol. 1978 Jan;62(1):99–106. doi: 10.1111/j.1476-5381.1978.tb07011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guertzenstein P. G. Blood pressure effects obtained by drugs applied to the ventral surface of the brain stem. J Physiol. 1973 Mar;229(2):395–408. doi: 10.1113/jphysiol.1973.sp010145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guertzenstein P. G., Lopes O. U. Cardiovascular responses evoked from the nicotine-sensitive area on the ventral surface of the medulla oblongata in the cat. J Physiol. 1984 Feb;347:345–360. doi: 10.1113/jphysiol.1984.sp015069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guertzenstein P. G., Silver A. Fall in blood pressure produced from discrete regions of the ventral surface of the medulla by glycine and lesions. J Physiol. 1974 Oct;242(2):489–503. doi: 10.1113/jphysiol.1974.sp010719. [DOI] [PMC free article] [PubMed] [Google Scholar]


