Abstract
Human metapneumovirus (hMPV) is a newly described paramyxovirus that is an important cause of acute respiratory tract disease. We undertook to develop a small animal model of hMPV infection, pathogenesis, and protection. Hamsters, guinea pigs, cotton rats, and nine inbred strains of mice were inoculated intranasally with hMPV. The animals were sacrificed, and nasal and lung tissue virus yields were determined by plaque titration. None of the animals exhibited respiratory symptoms. The quantity of virus present in the nasal tissue ranged from 4.6 × 102 PFU/gram tissue (C3H mice) to greater than 105 PFU/gram (hamster). The amount of virus in the lungs was considerably less than in nasal tissue in each species tested, ranging from undetectable (<5 PFU/g; guinea pigs) to 1.8 × 105 PFU/gram (cotton rat). The peak virus titer in cotton rat lungs occurred on day 4 postinfection. hMPV-infected cotton rat lungs examined on day 4 postinfection exhibited histopathological changes consisting of peribronchial inflammatory infiltrates. Immunohistochemical staining detected virus only at the luminal surfaces of respiratory epithelial cells throughout the respiratory tract. hMPV-infected cotton rats mounted virus-neutralizing antibody responses and were partially protected against virus shedding and lung pathology on subsequent rechallenge with hMPV. Viral antigen was undetectable in the lungs on challenge of previously infected animals. This study demonstrates that the cotton rat is a permissive small animal model of hMPV infection that exhibits lung histopathology associated with infection and that primary infection protected animals against subsequent infection. This model will allow further in vivo studies of hMPV pathogenesis and evaluation of vaccine candidates.
Human metapneumovirus (hMPV) is a recently described virus classified as a member of the family Paramyxoviridae, tentatively assigned to the genus Metapneumovirus within the subfamily Pneumovirus. hMPV is a major cause of acute respiratory tract disease in adults and children worldwide (4, 7, 12, 13, 15, 16, 18, 19, 25, 33, 36, 46, 50, 52, 54). hMPV has also been isolated as a possible copathogen in a subset of severe acute respiratory syndrome (SARS) cases caused by the SARS coronavirus (9, 10, 29, 39). Serological studies in The Netherlands showed that hMPV had been circulating since at least the 1950s and that all subjects were seropositive by 5 years of age (50). A prospective longitudinal cohort study conducted from 1976 to 2001 found that hMPV was one of the most common causes of lower respiratory tract infection in otherwise-healthy outpatient children, second only to respiratory syncytial virus (RSV) (54). That study, and others investigating hospitalized children with hMPV infection (7, 12, 13, 15, 18, 19, 33, 36, 52), have shown that hMPV is associated most frequently with bronchiolitis, laryngotracheobronchitis, and pneumonia and that hMPV-associated disease is clinically indistinguishable from that caused by the related virus RSV.
Genetic analysis of circulating hMPV field strains suggests two major genetic subgroups, each with two minor subgroups (5, 6, 8, 31, 38, 50, 53). Recurrent infection with hMPV has been documented with genetically heterologous (14, 37) and homologous (J. V. Williams, C. K. Wang, R. R. Spaete, and J. E. Crowe, Jr., submitted for publication) strains. The full extent of antigenic relatedness and cross-protective immunity between genetically heterologous subgroups has not been determined (32, 45, 53, 56). Furthermore, the nature of protective immunity and the contributions of humoral and cellular components are not completely elucidated, although both humoral and cellular immunities appear to be important in animal studies (45, 53, 56). While some of these studies can be conducted in humans, an animal model of hMPV infection would greatly facilitate studies of immunity and reinfection and preclinical evaluation of vaccine candidates. Animal models of RSV have been instrumental in elucidating the nature of immunity, exploring mechanisms of pathogenesis, and evaluating candidate vaccines and immunoprophylactic antibodies against that virus (21).
In the current study, we sought to develop a small animal model of hMPV infection. We inoculated numerous species of small animals with hMPV and measured virus replication to determine the most permissive host for hMPV. We then further investigated the most permissive animal to determine the kinetics of virus shedding and the pathological, immunohistochemical, and serologic features of hMPV infection in the animals.
MATERIALS AND METHODS
Virus preparation.
The virus strain used (hMPV strain TN/96-12) was obtained originally from a nasopharyngeal-wash specimen from a young child with upper respiratory tract illness in 1996 in Nashville, TN. Sequence analysis revealed that this strain is a genotype group A1 virus, according the proposed nomenclature (53), and that the strain is closely related genetically to the virus strain NL/00-1, a prototype strain isolated by a Dutch group (51). Virus was grown in LLC-MK2 cells (ATCC CCL-7) with OptiMEM medium (Invitrogen) supplemented with l-glutamine, gentamicin, and amphotericin and incubated at 37°C in a CO2 incubator. The medium for cell propagation was supplemented with 2% fetal calf serum. The medium for virus growth was supplemented with 5 μg/ml trypsin without serum. Several flasks were inoculated with hMPV strain TN/96-12 to generate working stocks of virus. Cell monolayers demonstrating 3 to 4+ cytopathic effect were harvested, sonicated, and clarified, and the supernatant was purified over a 20%-60% discontinuous sucrose gradient by ultracentrifugation at 125,000 × g in a Sorvall AH629 rotor at 4°C for 90 min. The gradient interface was collected into cryovials, flash-frozen in a dry-ice-ethanol slurry, and stored at −80°C. A single batch of this preparation was used as the virus stock for all animal studies. This virus stock was determined to have a titer of 106 PFU/ml by plaque titration in LLC-MK2 cell monolayer cultures. The virus stock that was used in the animal studies had been passaged a total of five times in LLC-MK2 cells.
Generation of guinea pig polyclonal antibodies to hMPV.
Five-week-old guinea pigs (Cavia porcellus; Harlan) were inoculated intranasally with 105 PFU of sucrose gradient-purified live hMPV strain TN/96-12 on two occasions, 3 weeks apart, after which the animals were exsanguinated. We tested the specificity of the guinea pig anti-hMPV antiserum by both immunofluorescent and immunoperoxidase-labeled staining of mock-infected LLC-MK2 cell monolayers or monolayers infected with hMPV, RSV, parainfluenza virus (PIV), or influenza virus. The anti-hMPV antiserum did not cross-react with RSV-, PIV-, influenza virus-, or mock-infected LLC-MK2 cells in our assay (data not shown). We also tested the anti-hMPV antiserum against mock-infected or RSV-, PIV-, influenza virus-, or hMPV-infected cell lysates in immunoblots and found the antiserum to be specific for hMPV detection (data not shown). We tested various dilutions to determine the working concentration, and a 1:1,000 dilution of the guinea pig anti-hMPV antiserum was used for all plaque titrations.
Animals.
Animals were purchased at 5 to 6 weeks of age from a commercial breeder (Harlan, Indianapolis, IN), fed standard diet and water ad libitum, and kept in species- or strain-specific groups of five in microisolator cages. Mouse strains (Mus musculus) used in this study were 129, AKR, BALB/c, C3H, C57BL/10, CBA, DBA/1, DBA/2, and SJL. Other species were guinea pigs, Syrian golden hamsters (Mesocricetus auratus), and cotton rats (Sigmodon hispidus). The animals were anesthetized by methoxyflurane (Metofane) inhalation, and 100 μl (105 PFU) of a suspension of hMPV strain TN/96-12 was instilled intranasally. Studies have shown that under these conditions a substantial amount of the inoculum is aspirated directly into the lungs, and the nasal turbinates are also inoculated (20, 49). For the initial set of experiments, the animals were infected in groups of five and sacrificed on day 4 postinfection. To determine the kinetics of hMPV replication in cotton rats, animals were sacrificed in groups of three on day 2, 4, 6, 8, 10, or 14 postinfection. The animals were sacrificed by CO2 asphyxiation, and nasal and lung tissues were harvested separately and immediately homogenized in 3 ml of ice-cold Hanks' balanced salt solution. The lungs were pulverized in ice-cold glass homogenizers, and nasal turbinates were ground with sterile sand in a cold porcelain mortar and pestle. Tissue homogenates were centrifuged at 4°C for 10 min at 300 × g, and the supernatants were collected, aliquoted into cryovials, and snap-frozen in liquid nitrogen. Virus yields were measured by plaque titration as described below. The Vanderbilt Institutional Animal Care and Use Committee approved the study.
Virus plaque titration.
Clarified tissue homogenates were thawed quickly at 37°C and diluted in serial 10-fold dilutions in OptiMEM medium supplemented with trypsin. The dilutions were inoculated in triplicate onto LLC-MK2 monolayer cell cultures in 24-well plates and incubated at 37°C for 1 hour with rotation on a tilting rotator (Orbitron II; Boekel Scientific). The wells then were overlaid with 0.75% methylcellulose in OptiMEM medium supplemented with trypsin and incubated at 37°C in a CO2 incubator for 4 days. The monolayers were rinsed, formalin fixed, and stained with guinea pig anti-hMPV serum that we produced as described above, followed by peroxidase-labeled goat anti-guinea pig immunoglobulin (Ig) (Kierkegaard and Perry Laboratories) and TruBlue substrate (Kierkegaard and Perry Laboratories). Plaques were counted, and the titer of virus was expressed as PFU/gram of tissue calculated from the average of three wells. A working stock of hMPV was included in each titration assay as a positive control.
Pathological examination.
The cotton rats were sacrificed by CO2 asphyxiation on day 4 postinfection and dissected. Specimens for histological examination were fixed in 4% buffered paraformaldehyde, embedded in paraffin, sectioned at 5 μm, and stained with hematoxylin and eosin for light microscopy. Lungs were inflated with 4% buffered paraformaldehyde. The following tissues were examined by light microscopy: brain, heart, thymus, nasal turbinates, lung, spleen, and liver. Equivalent tissue sections from an uninfected cotton rat were processed and examined as a control. The sections were reviewed by the pathologist without knowledge of the hMPV infection status of the specimens. All lobes of the lungs were examined, including two sections per lung. For the challenge study, cotton rats were inoculated intranasally with sucrose (mock) or live hMPV and inoculated with live hMPV 21 days later as described below. Four days after rechallenge with hMPV, the animals were sacrificed and the lungs were removed and processed as described above for virus titer and histology.
Immunohistochemistry.
Paraffin-embedded cotton rat lung sections 5 μm in thickness were placed on charged slides and baked overnight at 50°C. The paraffin was removed from the slides, and the sections were placed in heated Target Retrieval Solution (DakoCytomation, Carpinteria, CA) for 20 min. After an additional 20 min of cooling, the slides were rinsed in Tris-buffered saline-Tween for 5 min immediately prior to being immunostained. Endogenous peroxidase was neutralized with 0.03% hydrogen peroxide, and samples were treated with diluted rabbit serum to block nonspecific protein binding. The slides were incubated for 120 min with guinea pig anti-hMPV antiserum that we produced, diluted 1:500. Sections without primary antibody served as negative controls. The Vectastain ABC Elite (Vector Laboratories, Burlingame, CA) system and DAB+ (DakoCytomation) was used to produce localized, visible staining. The slides were counterstained lightly with Mayer's hematoxylin, dehydrated, and coverslipped.
Measurement of neutralizing antibody titers.
Sera were collected from the animals by retro-orbital bleeds at 21 days after infection with hMPV, prior to rechallenge. The sera were mixed in serial twofold dilutions (starting at 1:4) with a working stock of hMPV TN/96-12 in a final concentration previously determined to yield 50 PFU/well. The mixture was incubated at room temperature for 1 hour with rotation. The serum-virus mixtures then were plated in triplicate on LLC-MK2 monolayers in 96-well culture plates and allowed to adsorb at room temperature for 1 hour. The wells then were overlaid with 0.75% methylcellulose in OptiMEM supplemented with trypsin and incubated at 37°C in a CO2 incubator for 4 days. The monolayers were rinsed, formalin fixed, and stained with guinea pig anti-hMPV serum and peroxidase-labeled goat anti-guinea pig Ig as described above. Plaques were counted, and 60% plaque reduction titers were calculated as previously described for RSV in vitro neutralization assays (11, 28). hMPV-positive human serum was used as a positive control in all assays.
Challenge and rechallenge with hMPV.
Two groups of cotton rats were inoculated intranasally as previously described either with 100 μl (105 PFU) of hMPV strain TN/96-12 (six animals; hMPV group) or with 100 μl of 20% sucrose for the mock-infected animals (four animals; mock group). Twenty-one days later, both groups were challenged intranasally with 105 PFU of hMPV strain TN/96-12. Four days later, the animals were sacrificed and terminally exsanguinated. Nasal and lung titers of hMPV were determined as described above. Animals from each group also had lung tissue fixed for immunohistochemical studies as described above. Comparisons between groups were made using Student's t test with a two-tailed distribution assuming unequal variance.
RESULTS
Response to infection.
None of the animals exhibited diminished appetite or activity, ruffled fur, or behavioral changes. No rhinitis, cough, tachypnea, or other evidence of respiratory illness was observed in the animals.
Patterns of hMPV replication.
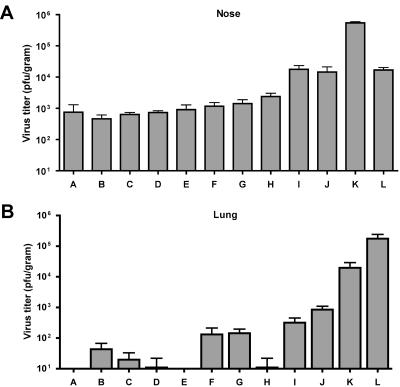
Initial experiments were conducted to measure the amount of hMPV present in the nasal or lung tissues of animals 4 days postinoculation. hMPV was detected in the nasal tissues of all animals, ranging in titer from a mean of 4.6 × 101 PFU/g (C3H mice) to a mean of 5.4 × 105 PFU/g (hamster) (Fig. 1A). There was little variability in the amount of hMPV shed by individual animals within a group of a given mouse strain or animal species. Thus, all animals were at least semipermissive for hMPV replication in the nasal turbinate tissues.
FIG. 1.
(A) Nasal titers of hMPV shed 4 days postinfection from animal strains and species tested. (B) Lung titers of hMPV shed 4 days postinfection from animal strains and species tested. Bars: A, guinea pigs; B, C3H mice; C, CBA mice; D, C57BL/10 mice; E, SJL mice; F, BALB/c mice; G, 129 mice; H, AKR mice; I, DBA/1 mice; J, DBA/2 mice; K, Syrian golden hamsters; L, cotton rats. The error bars indicate standard errors of the means (SEM).
Determination of lung titers of hMPV yielded quite different results, as shown in Fig. 1B. The amount of hMPV replicating in lung tissue ranged from less than detectable (<5 PFU/g; all guinea pigs and SJL mice) to a mean of 1.8 × 105 PFU/g (cotton rat). In several strains of mice (C3H, CBA, C57BL/10, and AKR), hMPV replicated to titers in lung tissue of less than a mean of 102 PFU/g, and even this low level of virus was not present in all animals within these groups. The DBA/2 mice shed a mean of 8.5 × 102 PFU/g, suggesting they are semipermissive for hMPV replication and therefore the most permissive mouse strain tested. We further tested 12-week-old and retired breeder DBA/2 mice, and similar titers of hMPV in nasal turbinates and lung tissue were observed (data not shown). The hamsters again were permissive, shedding a mean of 2 × 104 PFU/g in lung tissue. Strikingly, the cotton rats exhibited a titer in PFU/g of hMPV in lung tissue similar to the concentration with which they were inoculated, showing that they were more permissive for hMPV replication in the lungs than the hamsters in this study, and nearly as much so in the nasal turbinates. The cotton rat thus was selected for further characterization of hMPV replication in vivo.
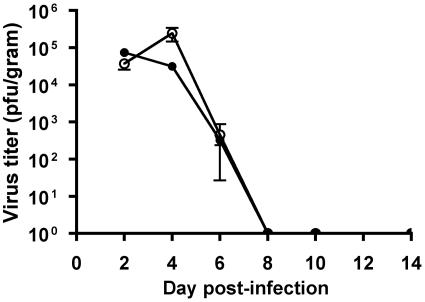
The kinetics of hMPV replication in cotton rats were determined by infecting animals intranasally with 105 PFU of hMPV in a 100-μl volume and sacrificing them at 2, 4, 6, 8, 10, or 14 days postinfection. As shown in Fig. 2, hMPV replication peaked in the nasal turbinates on day 2 at a mean titer of 5.6 × 104 PFU/g and declined swiftly after day 4. Virus was not detected in nasal turbinates after day 6. The replication of hMPV in the lung tissues peaked on day 4 postinfection at a mean titer of 1.8 × 105 PFU/g and declined rapidly. Virus was not detected in the lung after day 6.
FIG. 2.
Kinetics of hMPV replication in cotton rats. Animals were infected by the nasal route and sacrificed at 2, 4, 6, 8, 10, or 14 days postinfection. Closed circles, nose; open circles, lung. The error bars indicate SEM.
Histopathology.
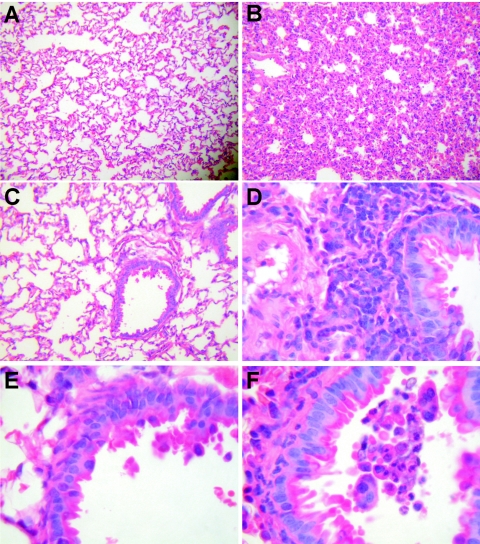
The nasal epithelium of the hMPV-infected animals showed mild subepithelial lymphoid infiltrates between the basement membrane and the cartilage and a loss of ciliated epithelial cells, changes that were not present in the uninfected animals (data not shown). The most striking findings were in the lungs of infected animals examined on day 4 after primary infection (Fig. 3). The lungs of hMPV-infected cotton rats showed peribronchial lymphoplasmocytic infiltrates and edematous thickening of the bronchial submucosa. The large bronchi did not show morphological changes, while the medium and small bronchioles demonstrated hypersecretory epithelial morphology. In addition, there was diffuse mild expansion of the alveolar interstitium due to mononuclear cell infiltrates and edema. Sloughed epithelial cells, neutrophils, macrophages, and amorphous debris were visible in the bronchial lumens. The distribution of the lung lesions was multifocal, and they were locally extensive. Hyperplasia of bronchus-associated lymphoid tissue was observed, as defined by the presence of nodular hyperplasia located at branch points in the respiratory tree. Histopathological changes were not seen in sections of the brain, heart, thymus, lung, spleen, or liver in any infected or uninfected animals (data not shown).
FIG. 3.
Histopathology of hMPV infection in cotton rat lungs. (A) At low power, the control lung is free of interstitial infiltrates, with normal airways (hematoxylin and eosin [HE]; original magnification, ×25). (B) In contrast, the interstitium of the hMPV-infected lung is expanded by mononuclear cells (HE; original magnification, ×25). (C) Higher magnification of the uninfected lung does not show interstitial infiltrates or peribronchial inflammation (HE; original magnification, ×62.5). (D) Higher magnification of hMPV-infected lung shows hypersecretory changes of the epithelium and peribronchiolar mononuclear cell infiltrate (HE; original magnification, ×125). (E) No significant bronchiolar inflammation is present in control lung (HE; original magnification, ×250). (F) Thickening of bronchial submucosa with neutrophils and macrophages present in lumen of hMPV-infected lung (HE; original magnification, ×250).
Immunohistochemistry.
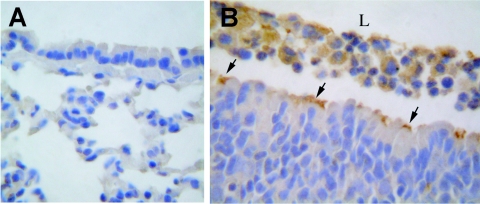
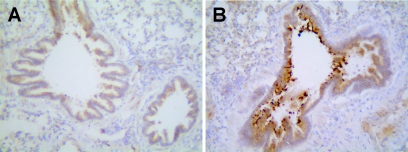
Tissue sections, including lung, from the uninfected animal did not exhibit reactivity with the anti-hMPV serum (Fig. 4A). Immunostained sections of brain, heart, thymus, spleen, or liver from uninfected or hMPV-infected cotton rats were negative (data not shown). hMPV antigen was detected only in respiratory epithelial tissue in sections from hMPV-infected cotton rats, at the luminal surfaces of respiratory epithelial cells (Fig. 4B). hMPV antigen staining was seen in respiratory epithelial cells from nasal tissue to the bronchioles. The pattern of viral antigen was discontinuous and tended to occur in clusters of adjacent cells. HMPV antigen was detected in both morphologically normal and degenerated epithelial cells. Luminal cellular debris that included both sloughed epithelial cells and macrophages stained positive for hMPV antigen. This staining appeared to be specific, demonstrating the presence of hMPV antigen, but it could not be determined whether the macrophages were actually infected with hMPV or had phagocytosed cellular debris from infected epithelial cells.
FIG. 4.
Immunohistochemistry of hMPV infection in cotton rat lungs. (A) Control lung is negative for hMPV antigen, with minimal background (hematoxylin counterstain; original magnification, ×250). (B) HMPV-infected lung. hMPV antigen is detected at the luminal surfaces of ciliated cells in a discontinuous pattern (arrows). Note mixed inflammatory cells in airway lumen (L) (hematoxylin counterstain; original magnification, ×250).
Protective immunity and antibody response.
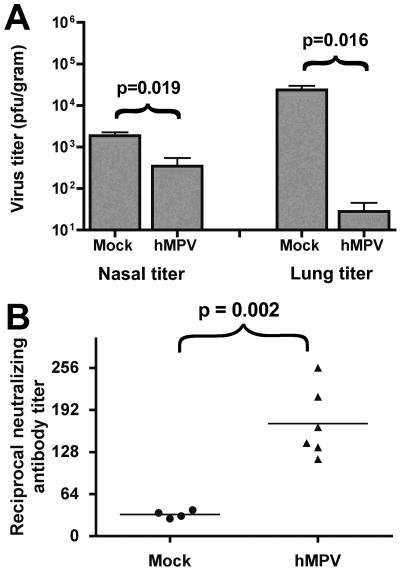
Cotton rats that were mock infected were not protected against subsequent hMPV challenge and shed significant amounts of virus from both the nose and lungs (Fig. 5A). As in the initial experiments, the concentration of virus in tissues was higher in the lungs than in nasal tissues. Although the numbers of individual animals with any amount of detectable virus shedding did not differ significantly between the mock-infected and previously hMPV-infected groups, the degree of protection was significant in both nasal and lung tissues. The animals that had been infected previously showed a modest level of protection against nasal infection with hMPV, with a diminished level of virus shedding that was significant in magnitude compared to the mock-infected animals (P = 0.019). Two of the previously infected animals did not replicate detectable virus in the nasal tissues. Strikingly, the previously infected cotton rats exhibited a high degree of protection against repeated hMPV infection in the lung, exhibiting more than a 3,000-fold restriction of virus replication compared with mock-infected animals (P = 0.016). Four of the previously infected animals did not replicate detectable levels of virus in the lungs following the second hMPV inoculation.
FIG. 5.
(A) Nasal and lung titers of hMPV shed in challenge of previously infected cotton rats. The animals were previously inoculated with 20% sucrose (mock) or 105 PFU live virus (hMPV). All animals were infected with live hMPV 21 days later and sacrificed 4 days postinfection. The error bars indicate SEM. (B) Virus neutralizing antibody titers of cotton rats in the two groups from panel A. Horizontal lines indicate mean titers. All comparisons by Student's t test, two-tailed, assuming unequal variance.
We determined the serum virus neutralizing antibody responses in these two groups of animals (Fig. 5B). The mean reciprocal serum neutralizing antibody titer at day 21 post-primary infection (just prior to rechallenge) differed significantly between the mock-infected and previously hMPV-infected animals (1:32 versus 1:180; P = 0.002). The hMPV serum neutralizing antibody titers in the previously hMPV-infected animals ranged from 1:132 to 1:256.
Effect of immunity on immunohistochemistry.
We attempted to identify hMPV in the lungs of previously infected animals that had no detectable virus shedding on challenge to confirm the absence of hMPV in the animals' lungs. Immunohistochemical staining of lung sections from previously infected animals showed that hMPV antigen could not be detected on day 4 following the challenge inoculation (Fig. 6A). By comparison, hMPV antigen was detected in lung sections from mock-infected cotton rats that were subsequently challenged with hMPV at levels and in a pattern similar to those seen in animals with primary infection (Fig. 6B).
FIG. 6.
Immunohistochemistry of hMPV infection in lungs of previously hMPV-infected or mock-infected cotton rats challenged with live hMPV. The animals were previously inoculated with 20% sucrose (mock) or 105 PFU live virus (hMPV). All animals were infected with live hMPV 21 days later and sacrificed 4 days postinfection. (A) Lung from previously hMPV-infected animal is negative for hMPV antigen, with minimal background (hematoxylin counterstain; original magnification, ×250). (B) Lung from animal previously mock infected with sucrose. Abundant hMPV antigen is detected at the luminal surfaces of ciliated cells and in intraluminal debris in a pattern similar to that previously shown for primary infection (hematoxylin counterstain; original magnification, ×250).
DISCUSSION
We showed that the cotton rat (Sigmodon hispidus) is permissive for hMPV replication in both nasal turbinate and lung tissues and exhibited higher replication of virus in the lungs than in nasal turbinates. Peak levels of virus replication in tissues occurred on day 4 postinfection. Although clinical symptoms were not observed, hMPV infection was associated with significant inflammation in the lower respiratory tract. Pathological changes were not seen in any of multiple other tissues examined or in uninfected animals. Immunostaining for hMPV showed viral antigen present only at the apical surfaces of respiratory epithelial cells throughout the respiratory tract, suggesting a tropism for polarized respiratory epithelial cells. hMPV infection induced a partially protective immune response against hMPV replication on subsequent challenge in cotton rats, as evidenced by the decreased virus shedding in the lungs of previously infected animals. Incomplete protection was induced in the upper respiratory tract, as a reduced level of virus replication was detected following challenge. The animals also mounted a virus-specific serum neutralizing antibody response following mucosal infection. It is possible that the route of inoculation may have influenced the discrepancy in protection we observed, but we think it is unlikely for several reasons. First, studies have shown that in rodents, intranasal inoculations of sufficient volume given under anesthesia are aspirated into the lung (20, 49). Second, although all inoculations of hMPV were performed in similar fashion (100-μl volume intranasally while the animal was under anesthesia), the cotton rats shed a higher concentration of virus from lung tissue. These findings suggest that the mechanisms of immunity against hMPV in the upper and lower respiratory tracts may differ or that the efficiency of the immune mechanisms in the upper respiratory tract is reduced. This finding is consistent with studies of the related pneumovirus RSV in animals or in humans. Studies have demonstrated that passively acquired or actively induced serum neutralizing antibodies against RSV protect the lower but not the upper airways from disease (42, 43). Epidemiologic studies have shown that humans can be reinfected with hMPV and that lower respiratory tract infection early in life may be followed by upper respiratory tract infection alone with subsequent hMPV infection, suggesting a similar discordance between the efficacy of immune-mediated protection of the upper and lower respiratory tracts (54; Williams et al., submitted).
The original report describing hMPV found that chickens and turkeys were not permissive for hMPV replication, while macaques could be infected (50). Recently, the same group reported the pathological features of hMPV infection in cynomolgus macaques (30). In that study, histopathological changes similar to those we report here were observed, including disruption of the epithelial architecture, sloughing of epithelial cells, loss of ciliation, and presence of inflammatory infiltrates in the lungs. Similar to what we observed in cotton rats, histopathologic changes were not seen in any other tissues. Immunohistochemical staining in the macaques also revealed viral antigen to be localized almost exclusively at the apical surfaces of ciliated respiratory epithelial cells. This finding is concordant with the clinical data describing hMPV infection in humans, which has found evidence only of respiratory tract disease (7, 12, 13, 15, 18, 19, 36, 52, 54). These observations are also similar to those made with RSV infection in humans and in animal models (1, 20, 24, 34, 40, 41). Like many other members of the paramyxovirus family, hMPV appears to exhibit a primary tropism limited to respiratory epithelia in immunocompetent hosts. The biological reasons for this predilection are not clear but could involve the distribution of cellular receptors or differential expression of host proteins, such as proteases, that are necessary for the viral life cycle. Appropriate animal models are critical to investigate the roles of these factors in pathogenesis.
Inbred strains of mice, particularly the BALB/c strain, have been used extensively as small animal models of RSV infection. However, for studies of immunogenicity and vaccine-induced protection against a respiratory virus that measure reduction in virus titer as a correlate of protection, a high level of virus replication is desirable. Similar to our results for hMPV, studies of RSV in small animals have shown that mice are also less permissive for RSV replication in the lungs than are cotton rats. Prince et al. inoculated 20 inbred mouse strains with 103.3 to 103.7 PFU of RSV, and the BALB/c strain replicated RSV to a mean titer of 6 × 104 PFU/g in nasal tissues but only 2 × 103 in the lungs (41). Interestingly, in that study, DBA/2 mice were the strain most permissive for RSV replication in both nasal and lung tissues, similar to what we observed for hMPV. In contrast to reports of RSV infection in mice showing increased permissiveness in older animals (20), we did not detect a difference in permissiveness of DBA/2 mice for hMPV infection at different ages. Taylor et al. inoculated BALB/c mice intranasally with 104 PFU of RSV. Similarly, the level of virus replication was 102.5 to 103.9 PFU/g in the nose and 103.4 to 104.5 in the lungs (48). Graham et al. showed similar results by inoculating BALB/c mice with RSV and correlated lung histopathological changes with the titer of virus inoculum. Histopathological changes were observed consistently only with a high inoculum of 107 PFU, while pathological changes were minimal with an inoculum of 106 PFU and absent with 105 PFU (20). Thus, in all these studies, virus replication and lung histopathology required inoculation with a high titer of RSV, and virus titers in infected tissues were substantially lower than the inoculating concentration of virus.
In contrast, Prince et al. inoculated cotton rats with 104 PFU of RSV and detected 105 PFU/g in the lungs and 105 to 106 in nasal tissues (40). Histopathologic examination of the cotton rat lungs during infection revealed prominent involvement of ciliated respiratory epithelial cells with sloughing into the lumen. Terminal bronchioles were affected far more than alveoli, and immunofluorescent staining for RSV antigen was detected only in epithelial cells or intraluminal debris. These changes, and the kinetics of RSV shedding in cotton rats, are consistent with studies of RSV infection and pathology in humans (1, 17, 23, 34). Based on these and similar immunological studies (22, 42, 43, 47), the cotton rat has been used as an in vivo RSV infection model in the development of two antibody formulations used to prevent severe RSV disease in high-risk premature infants. RSVIg, a polyclonal pooled human immunoglobulin product that possesses high neutralizing activity against RSV, and palivizumab, a humanized anti-RSV F protein monoclonal antibody, both advanced to clinical trials based on studies of efficacy in cotton rats (26, 27, 44, 55).
Our data differ from some recent reports of hMPV infection of small animals. Alvarez et al. described a biphasic pattern of hMPV replication in BALB/c mice, with peak titers of 108 PFU/g lung tissue on day 7 postinfection, declining to 105.8 PFU/g on day 10 and reaching a second peak of 107 PFU/g on day 14 (2, 3). In that study, hMPV could be detected in the lung at 104 PFU/g at 28 days and persisted until 60 days postinfection. These results are discordant with our findings in BALB/c mice. We repeated the inoculation of BALB/c mice with hMPV in a second experiment and found the same low levels of hMPV replication in lung tissue (data not shown). MacPhail et al. (32) found levels of hMPV replication in BALB/c mice very similar to our results, 103.4 PFU/g in the nose and 102.4 PFU/g in the lung. These discrepant results may reflect differences in virus strains, animals, or methods. While the BALB/c model of hMPV infection will undoubtedly be useful, limited data in humans suggest that prolonged shedding of hMPV is unusual in immunocompetent hosts (13; Williams et al., submitted). Prolonged shedding of RSV in healthy humans has not been described (17, 23, 24). Thus, we think that an animal model with kinetics that may be more reflective of human infection is desirable.
MacPhail et al. also tested cotton rats for hMPV replication and found less than 102 PFU/g of virus in the nose and lungs (32). However, a group experienced in cotton rat RSV studies found cotton rats to be permissive for hMPV replication in nose and lungs, with a peak titer of 103.6 PFU/g in the nose and 104.4 PFU/g in the lung on day 4 postinfection (56). Most of the animals cleared infection by day 10, and all mounted serum neutralizing antibody responses. The animals in that study were not rechallenged to measure protection. The lack of permissivity observed by MacPhail et al. may reflect differences in viral strains or cell culture methods, differences between animals, or varying levels of experience with cotton rats as an animal model. Nonetheless, our results and the results of Wyde et al. (56) clearly show that cotton rats are permissive for hMPV replication in both nose and lungs to high titers.
Our findings suggest that the cotton rat is a permissive animal model to study pathogenesis and an appropriately sensitive model to measure the effects of vaccines or prophylactic antibodies on virus replication and histopathology. The cotton rat has been used as a model for a number of infectious diseases, including RSV, adenovirus, and measles (35). In addition, many immunologic and molecular reagents are now commercially available that are cotton rat specific, providing an array of tools necessary to further explore the pathogenesis and immune response to hMPV in this permissive model. Of the mouse strains tested, the DBA/2 strain exhibited the highest level of virus replication in tissues. Although less permissive for replication than cotton rats, the DBA/2 mouse is an experimental host for hMPV infection that may be appropriate when particular immune mechanisms can be studied only in a murine system because of transgenic or knockout technologies or reagent availability.
Acknowledgments
We thank Greg Hanley and Maggie McTighe for assistance with animal care and Kelly Parman for assistance with immunohistochemistry.
Financial support was provided by National Institutes of Health grant K08 AI56170 (J.V.W.) from the National Institute of Allergy and Infectious Diseases.
REFERENCES
- 1.Aherne, W., T. Bird, S. D. Court, P. S. Gardner, and J. McQuillin. 1970. Pathological changes in virus infections of the lower respiratory tract in children. J. Clin. Pathol. 23:7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alvarez, R., K. S. Harrod, W. J. Shieh, S. Zaki, and R. A. Tripp. 2004. Human metapneumovirus persists in BALB/c mice despite the presence of neutralizing antibodies. J. Virol. 78:14003-14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvarez, R., and R. A. Tripp. 2005. The immune response to human metapneumovirus is associated with aberrant immunity and impaired virus clearance in BALB/c mice. J. Virol. 79:5971-5978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bastien, N., D. Ward, P. Van Caeseele, K. Brandt, S. H. Lee, G. McNabb, B. Klisko, E. Chan, and Y. Li. 2003. Human metapneumovirus infection in the Canadian population. J. Clin. Microbiol. 41:4642-4646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bastien, N., S. Normand, T. Taylor, D. Ward, T. C. Peret, G. Boivin, L. J. Anderson, and Y. Li. 2003. Sequence analysis of the N, P, M and F genes of Canadian human metapneumovirus strains. Virus Res. 93:51-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biacchesi, S., M. H. Skiadopoulos, G. Boivin, C. T. Hanson, B. R. Murphy, P. L. Collins, and U. J. Buchholz. 2003. Genetic diversity between human metapneumovirus subgroups. Virology 315:1-9. [DOI] [PubMed] [Google Scholar]
- 7.Boivin, G., Y. Abed, G. Pelletier, L. Ruel, D. Moisan, S. Cote, T. C. T. Peret, D. D. Erdman, and L. J. Anderson. 2002. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J. Infect. Dis. 186:1330-1334. [DOI] [PubMed] [Google Scholar]
- 8.Boivin, G., I. Mackay, T. P. Sloots, S. Madhi, F. Freymuth, D. Wolf, Y. Shemer-Avni, H. Ludewick, G. C. Gray, and E. LeBlanc. 2004. Global genetic diversity of human metapneumovirus fusion gene. Emerg. Infect. Dis. 10:1154-1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan, P. K., J. S. Tam, C. W. Lam, E. Chan, A. Wu, C. K. Li, T. A. Buckley, K. C. Ng, G. M. Joynt, F. W. Cheng, K. F. To, N. Lee, D. S. Hui, J. L. Cheung, I. Chu, E. Liu, S. S. Chung, and J. J. Sung. 2003. Human metapneumovirus detection in patients with severe acute respiratory syndrome. Emerg. Infect. Dis. 9:1058-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan, P. K., K. F. To, A. Wu, G. M. Tse, K. F. Chan, S. F. Lui, J. J. Sung, J. S. Tam, and B. Tomlinson. 2004. Human metapneumovirus-associated atypical pneumonia and SARS. Emerg. Infect. Dis. 10:497-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coates, H. V., D. W. Alling, and R. M. Chanock. 1966. An antigenic analysis of respiratory syncytial virus isolates by a plaque reduction neutralization test. Am. J. Epidemiol. 83:299-313. [DOI] [PubMed] [Google Scholar]
- 12.Dollner, H., K. Risnes, A. Radtke, and S. A. Nordbo. 2004. An outbreak of human metapneumovirus infection in Norwegian children. Pediatr. Infect. Dis. J. 23:436-440. [DOI] [PubMed] [Google Scholar]
- 13.Ebihara, T., R. Endo, H. Kikuta, N. Ishiguro, H. Ishiko, M. Hara, Y. Takahashi, and K. Kobayashi. 2004. Human metapneumovirus infection in Japanese children. J. Clin. Microbiol. 42:126-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ebihara, T., R. Endo, N. Ishiguro, T. Nakayama, H. Sawada, and H. Kikuta. 2004. Early reinfection with human metapneumovirus in an infant. J. Clin. Microbiol. 42:5944-5946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esper, F., R. A. Martinello, D. Boucher, C. Weibel, D. Ferguson, M. L. Landry, and J. S. Kahn. 2004. A 1-year experience with human metapneumovirus in children aged <5 years. J. Infect. Dis. 189:1388-1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falsey, A. R., D. Erdman, L. J. Anderson, and E. E. Walsh. 2003. Human metapneumovirus infections in young and elderly adults. J Infect. Dis. 187:785-790. [DOI] [PubMed] [Google Scholar]
- 17.Falsey, A. R., M. A. Formica, J. J. Treanor, and E. E. Walsh. 2003. Comparison of quantitative reverse transcription-PCR to viral culture for assessment of respiratory syncytial virus shedding. J. Clin. Microbiol. 41:4160-4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freymouth, F., A. Vabret, L. Legrand, N. Eterradossi, F. Lafay-Delaire, J. Brouard, and B. Guillois. 2003. Presence of the new human metapneumovirus in French children with bronchiolitis. Pediatr. Infect. Dis. J. 22:92-94. [DOI] [PubMed] [Google Scholar]
- 19.Galiano, M., C. Videla, S. S. Puch, A. Martinez, M. Echavarria, and G. Carballal. 2004. Evidence of human metapneumovirus in children in Argentina. J. Med. Virol. 72:299-303. [DOI] [PubMed] [Google Scholar]
- 20.Graham, B. S., M. D. Perkins, P. F. Wright, and D. T. Karzon. 1988. Primary respiratory syncytial virus infection in mice. J. Med. Virol. 26:153-162. [DOI] [PubMed] [Google Scholar]
- 21.Graham, B. S., T. R. Johnson, and R. S. Peebles. 2000. Immune-mediated disease pathogenesis in respiratory syncytial virus infection. Immunopharmacology 48:237-247. [DOI] [PubMed] [Google Scholar]
- 22.Gruber, W. C., S. Z. Wilson, B. J. Throop, and P. R. Wyde. 1987. Immunoglobulin administration and ribavirin therapy: efficacy in respiratory syncytial virus infection of the cotton rat. Pediatr. Res. 21:270-274. [DOI] [PubMed] [Google Scholar]
- 23.Hall, C. B., R. G. Douglas, Jr., and J. M. Geiman. 1976. Respiratory syncytial virus infections in infants: quantitation and duration of shedding. J. Pediatr. 89:11-15. [DOI] [PubMed] [Google Scholar]
- 24.Hall, C. B. 2001. Respiratory syncytial virus and parainfluenza virus. N. Engl. J. Med. 344:1917-1928. [DOI] [PubMed] [Google Scholar]
- 25.Ijpma, F. F., D. Beekhuis, M. F. Cotton, C. H. Pieper, J. L. Kimpen, B. G. van den Hoogen, G. J. van Doornum, and D. M. Osterhaus. 2004. Human metapneumovirus infection in hospital referred South African children. J. Med. Virol. 73:486-493. [DOI] [PubMed] [Google Scholar]
- 26.Johnson, S., C. Oliver, G. A. Prince, V. G. Hemming, D. S. Pfarr, S. C. Wang, M. Dormitzer, J. O'Grady, S. Koenig, J. K. Tamura, R. Woods, G. Bansal, D. Couchenour, E. Tsao, W. C. Hall, and J. F. Young. 1997. Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus. J. Infect. Dis. 176:1215-1224. [DOI] [PubMed] [Google Scholar]
- 27.Johnson, S., S. D. Griego, D. S. Pfarr, M. L. Doyle, R. Woods, D. Carlin, G. A. Prince, S. Koenig, J. F. Young, and S. B. Dillon. 1999. A direct comparison of the activities of two humanized respiratory syncytial virus monoclonal antibodies: MEDI-493 and RSHZl9. J. Infect. Dis. 180:35-40. [DOI] [PubMed] [Google Scholar]
- 28.Karron, R. A., P. F. Wright, R. B. Belshe, B. Thumar, R. Casey, F. Newman, F. P. Polack, V. B. Randolph, A. Deatly, J. Hackell, W. Gruber, B. R. Murphy, and P. L. Collins. 2005. Identification of a recombinant live attenuated respiratory syncytial virus vaccine candidate that is highly attenuated in infants. J. Infect. Dis. 191:1093-1104. [DOI] [PubMed] [Google Scholar]
- 29.Kuiken, T., R. A. Fouchier, M. Schutten, G. F. Rimmelzwaan, G. van Amerongen, D. van Riel, J. D. Laman, T. de Jong, G. van Doornum, W. Lim, A. E. Ling, P. K. Chan, J. S. Tam, M. C. Zambon, R. Gopal, C. Drosten, S. van der Werf, N. Escriou, J. C. Manuguerra, K. Stohr, J. S. Peiris, and A. D. Osterhaus. 2003. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 362:263-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuiken, T., B. G. van den Hoogen, D. A. van Riel, J. D. Laman, G. van Amerongen, L. Sprong, R. A. Fouchier, and A. D. Osterhaus. 2004. Experimental human metapneumovirus infection of cynomolgus macaques (Macaca fascicularis) results in virus replication in ciliated epithelial cells and pneumocytes with associated lesions throughout the respiratory tract. Am. J. Pathol. 164:1893-1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mackay, I. M., S. Bialasiewicz, Z. Waliuzzaman, G. R. Chidlow, D. C. Fegredo, S. Laingam, P. Adamson, G. B. Harnett, W. Rawlinson, M. D. Nissen, and T. P. Sloots. 2004. Use of the P gene to genotype human metapneumovirus identifies 4 viral subtypes. J. Infect. Dis. 190:1913-1918. [DOI] [PubMed] [Google Scholar]
- 32.MacPhail, M., J. H. Schickli, R. S. Tang, J. Kaur, C. Robinson, R. A. Fouchier, A. D. Osterhaus, R. R. Spaete, and A. A. Haller. 2004. Identification of small-animal and primate models for evaluation of vaccine candidates for human metapneumovirus (hMPV) and implications for hMPV vaccine design. J. Gen. Virol. 85:1655-1663. [DOI] [PubMed] [Google Scholar]
- 33.Maggi, F., M. Pifferi, M. Vatteroni, C. Fornai, E. Tempestini, S. Anzilotti, L. Lanini, E. Andreoli, V. Ragazzo, M. Pistello, S. Specter, and M. Bendinelli. 2003. Human metapneumovirus associated with respiratory tract infections in a 3-year study of nasal swabs from infants in Italy. J. Clin. Microbiol. 41:2987-2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neilson, K. A., and E. J. Yunis. 1990. Demonstration of respiratory syncytial virus in an autopsy series. Pediatr. Pathol. 10:491-502. [DOI] [PubMed] [Google Scholar]
- 35.Niewiesk, S., and G. Prince. 2002. Diversifying animal models: the use of hispid cotton rats (Sigmodon hispidus) in infectious diseases. Lab. Anim. 36:357-372. [DOI] [PubMed] [Google Scholar]
- 36.Peiris, J. S., W. H. Tang, K. H. Chan, P. L. Khong, Y. Guan, Y. L. Lau, and S. S. Chu. 2003. Children with respiratory disease associated with metapneumovirus in Hong Kong. Emerg. Infect. Dis. 9:628-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pelletier, G., P. Dery, Y. Abed, and G. Boivin. 2002. Respiratory tract reinfections by the new human Metapneumovirus in an immunocompromised child. Emerg. Infect. Dis. 8:976-978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peret, T. C., Y. Abed, L. J. Anderson, D. D. Erdman, and G. Boivin. 2004. Sequence polymorphism of the predicted human metapneumovirus G glycoprotein. J. Gen. Virol. 85:679-686. [DOI] [PubMed] [Google Scholar]
- 39.Poutanen, S. M, D. E. Low, B. Henry, S. Finkelstein, D. Rose, K. Green, R. Tellier, R. Draker, D. Adachi, M. Ayers, A. K. Chan, D. M. Skowronski, I. Salit, A. E. Simor, A. S. Slutsky, P. W. Doyle, M. Krajden, M. Petric, R. C. Brunham, and A. J. McGeer. 2003. National Microbiology Laboratory, Canada; Canadian Severe Acute Respiratory Syndrome Study Team. Identification of severe acute respiratory syndrome in Canada. N. Engl. J. Med. 348:1995-2005. [DOI] [PubMed] [Google Scholar]
- 40.Prince, G. A., A. B. Jenson, R. L. Horswood, E. Camargo, and R. M. Chanock. 1978. The pathogenesis of respiratory syncytial virus infection in cotton rats. Am. J. Pathol. 93:771-791. [PMC free article] [PubMed] [Google Scholar]
- 41.Prince, G. A., R. L. Horswood, J. Berndt, S. C. Suffin, and R. M. Chanock. 1979. Respiratory syncytial virus infection in inbred mice. Infect. Immun. 26:764-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prince, G. A., V. G. Hemming, R. L. Horswood, and R. M. Chanock. 1985. Immunoprophylaxis and immunotherapy of respiratory syncytial virus infection in the cotton rat. Virus Res. 3:193-206. [DOI] [PubMed] [Google Scholar]
- 43.Prince, G. A., R. L. Horswood, and R. M. Chanock. 1985. Quantitative aspects of passive immunity to respiratory syncytial virus infection in infant cotton rats. J. Virol. 55:517-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siber, G. R., D. Leombruno, J. Leszczynski, J. McIver, D. Bodkin, R. Gonin, C. M. Thompson, E. E. Walsh, P. A. Piedra, and V. G. Hemming. 1994. Comparison of antibody concentrations and protective activity of respiratory syncytial virus immune globulin and conventional immune globulin. J. Infect. Dis. 169:1368-1373. [DOI] [PubMed] [Google Scholar]
- 45.Skiadopoulos, M. H., S. Biacchesi, U. J. Buchholz, J. M. Riggs, S. R. Surman, E. Amaro-Carambot, J. M. McAuliffe, W. R. Elkins, M. St Claire, P. L. Collins, and B. R. Murphy. 2004. The two major human metapneumovirus genetic lineages are highly related antigenically, and the fusion (F) protein is a major contributor to this antigenic relatedness. J. Virol. 78:6927-6937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stockton, J., I. Stephenson, D. Fleming, and M. Zambon. 2002. Human metapneumovirus as a cause of community-acquired respiratory illness. Emerg. Infect. Dis. 8:897-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sun, C. S., P. R. Wyde, S. Z. Wilson, and V. Knight. 1983. Cell-mediated cytotoxic responses in lungs of cotton rats infected with respiratory syncytial virus. Am. Rev. Respir. Dis. 127:460-464. [DOI] [PubMed] [Google Scholar]
- 48.Taylor, G., E. Stott, M. Hughes, and P. Collins. 1984. Respiratory syncytial virus infection in mice. Infect. Immun. 43:649-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Teramoto, S., T. Matsuse, T. Oka, H. Ito, Y. Fukuchi, and Y. Ouchi. 1998. Investigation of effects of anesthesia and age on aspiration in mice through LacZ gene transfer by recombinant E1-deleted adenovirus vectors. Am. J. Respir. Crit. Care Med. 158:1914-1919. [DOI] [PubMed] [Google Scholar]
- 50.Van Den Hoogen, B. G., J. C. DeJong, J. Groen, T. Kuiken, R. DeGroot, R. A. M. Fouchier, and D. M. E. Osterhaus. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 7:719-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van den Hoogen, B. G., T. M. Bestebroer, A. D. Osterhaus, and R. A. Fouchier. 2002. Analysis of the genomic sequence of a human metapneumovirus. Virology 295:119-132. [DOI] [PubMed] [Google Scholar]
- 52.Van den Hoogen, B. G., G. J. van Doornum, J. C. Fockens, J. J. Cornelissen, W. E. Beyer, R. de Groot, A. D. M. E. Osterhaus, and R. A. M. Fouchier. 2003. Prevalence and clinical symptoms of human metapneumovirus infection in hospitalized patients. J. Infect. Dis. 188:1571-1577. [DOI] [PubMed] [Google Scholar]
- 53.van den Hoogen, B. G., S. Herfst, L. Sprong, P. A. Cane, E. Forleo-Neto, R. L. de Swart, A. D. Osterhaus, and R. A. Fouchier. 2004. Antigenic and genetic variability of human metapneumoviruses. Emerg. Infect. Dis. 10:658-666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams, J. V., P. A. Harris, S. J. Tollefson, L. L. Halburnt-Rush, J. M. Pingsterhaus, K. M. Edwards, P. F. Wright, and J. E. Crowe, Jr. 2004. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N. Engl. J. Med. 350:443-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wyde, P. R., D. K. Moore, T. Hepburn, C. L. Silverman, T. G. Porter, M. Gross, G. Taylor, S. G. Demuth, and S. B. Dillon. 1995. Evaluation of the protective efficacy of reshaped human monoclonal antibody RSHZ19 against respiratory syncytial virus in cotton rats. Pediatr. Res. 38:543-550. [DOI] [PubMed] [Google Scholar]
- 56.Wyde, P. R., S. N. Chetty, A. M. Jewell, S. L. Schoonover, and P. A. Piedra. 2005. Development of a cotton rat-human metapneumovirus (hMPV) model for identifying and evaluating potential hMPV antivirals and vaccines. Antivir. Res. 66:57-66. [DOI] [PubMed] [Google Scholar]