Abstract
Introduction
The aim of this study was to assess the self-reported quality of care for people with knee osteoarthritis in Singapore and to investigate the associations between participant characteristics and functional outcomes at 1 year in relation to the reported quality of care.
Methods
Patients with knee osteoarthritis completed the osteoarthritis quality indicator (OA-QI) questionnaire, a validated patient-reported measure that assesses the clinician’s adherence to evidence-based guidelines for non-surgical knee osteoarthritis education and patient education. The OA-QI includes 17 indicators, with "achievement" defined as a 'Yes' response for each. We calculated individual per-item, overall per-item mean, and per-person achievement rates (%) and examined associations between participant characteristics, achievement rates, and function at 1 year.
Results
A total of 314 participants completed the OA-QI. Referral for physical activity (87.5%) and referral for daily activity aid assessment (15.7%) had the highest and lowest per-item achievement rates, respectively. The overall mean per-item and per-person achievement rates were both 62.2%. Participants educated about steroid injections (adjusted coefficient [95% CI]: 7.23 [1.42–13.04]; p = 0.015) or surgery (adjusted coefficient [95% CI]: 12.65 [5.89–19.40]; p < 0.001) had worse functional outcomes at one year than those who were eligible but not informed. Those not assessed for walking aids and indicating walking issues had poorer outcomes one year later (adjusted coefficient [95% CI]: -9.89 (-19.63, -0.15); p = 0.0470). However, no significant associations were found between per-person achievement rates and 1-year functional outcomes.
Conclusions
The quality of care in Singapore for people with knee osteoarthritis is suboptimal, especially for those needing walking aids and weight loss assistance. However, the quality of care alone does not fully account for long-term outcomes, suggesting that other factors need to be considered.
Keywords: Knee Osteoarthritis, Quality of Care, Non-surgical Management
Introduction
Osteoarthritis is a leading cause of disability worldwide [1]. In Singapore, symptomatic knee osteoarthritis (knee OA) affects 1 in 10 people over the age of 50 [2]. The number of people living with osteoarthritis is expected to continue to rise, in part owing to aging populations, plus increased levels of modifiable risk factors such as obesity and sedentary behavior [3]. Osteoarthritis most often affects the knee joints [4] and commonly results in pain, functional disability, and decreased quality of life [5].
Most international clinical practice guidelines for knee OA recommend a stepwise approach to management where surgical intervention is considered only after non-surgical and pharmacological interventions have been exhausted [6–9]. Non-surgical care is prioritized, as it produces similar outcomes and reduces the risk of severe adverse events compared with surgical interventions [10–12]. Furthermore, non-surgical care is a more cost-effective option, with mean direct costs that are 4 times lower than those of surgical management in Singapore [13]. Additionally, evidence indicates that as many as 25% of knee replacements can be avoided by engaging in appropriate guideline-recommended first-line care [14]. Despite clear guidance, many people with knee OA around the world are not provided with guideline-adherent first-line care before surgery [15, 16]. Implementing guideline recommendations in clinical practice can be challenging due to several factors, such as clinician and patient preferences and the support/culture of the healthcare system [17]. Therefore, overuse of surgical interventions is likely due to the failure of healthcare systems providing optimal and effective guideline-recommended care rather than to the failure of nonsurgical and pharmacological treatments for people with knee OA.
The Osteoarthritis Quality Indicator (OA-QI) questionnaire was developed in 2010 as a patient-reported measure assessing whether non-surgical knee OA management aligns with evidence-based guidelines, covering education, physical activity, weight management, pain management, and referrals [18]. It has been applied internationally to evaluate care quality, highlight inconsistencies, and identify underutilized interventions such as weight management and walking aid referrals. Prior studies have also used OA-QI to uncover barriers to optimal care delivery, including time constraints, patient awareness, and healthcare system limitations [19–22]. To the best of the authors' knowledge, no studies have used the OA-QI to assess self-reported quality of care for individuals with osteoarthritis in Asia or examine its impact on future functional outcomes. A comprehensive evaluation is needed to determine which treatments are regularly discussed with knee OA patients and to identify opportunities for improving the provision of first-line, non-surgical care.
The primary aim of this study was to investigate the self-reported quality of care for people with knee OA in Singapore. The secondary aims included investigating whether associations exist between; i) participant characteristics and the overall quality of care reported or, ii) the overall quality of care reported or individual indicators being addressed with functional outcomes at 1 year.
Methods
Study design and ethical approval
This study was primarily a cross-sectional study assessing the self-reported quality of care among patients with knee OA in Singapore. However, a subset of participants underwent a one-year follow-up for functional outcomes, allowing for a secondary longitudinal analysis. Ethical approval for a large multi-centre prospective cohort study, the Singapore KneE osteoarthriTis CoHort (SKETCH) study, was granted by the National Healthcare Group Domain Specific Review Board (NHG DSRB) Singapore (Reference number: 2021/01113). The SKETCH protocol has been published previously elsewhere [23]. This manuscript reports findings related to the OA-QI questionnaire and is written in alignment with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines [24].
Participants, sampling and recruitment
Participants were eligible if they were independent community mobilizers, met the National Institute for Health and Care Excellence (NICE) clinical diagnostic criteria for knee OA [6] and were conversant in English or Mandarin. Participants were excluded if they; i) had an alternate diagnosis of knee OA (e.g., referred pain from the hip or spine), ii) had other forms of knee arthritis (e.g., inflammatory, posttraumatic), iii) had moderate to severe cognitive impairment (e.g., dementia), iv) had received a previous knee arthroplasty, v) were wheelchair bound, vi) were pregnant or vii) had medical conditions that would medically interfere with rehabilitation involvement (e.g., decompensated heart failure, stroke with significant deficit, or end-stage renal failure).
Participants were recruited from two public hospitals within the National Healthcare Group, Singapore, between June 2021 and February 2022. The study employed a convenience sampling approach, where eligible individuals were identified and invited to participate during their orthopedic or physiotherapy appointments. They had the option to engage immediately during their appointment visit or via a web-based form (FormSG) after their appointment at their own convenience.
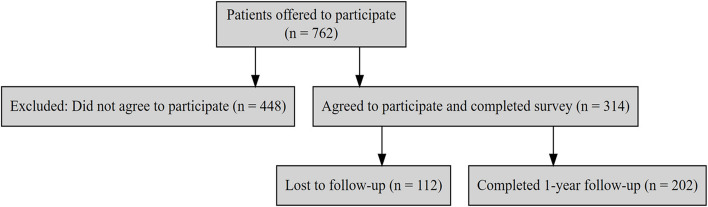
A total of 762 individuals were invited to participate, of whom 314 consented and completed the baseline survey in full, resulting in a 100% survey completion rate among those who consented. A recruitment flowchart summarizing participant selection, exclusions, and follow-up rates is provided in Fig. 1. This flowchart visually represents the number of individuals approached, excluded, enrolled, and lost to follow-up throughout the study.
Fig. 1.
Participant recruitment and follow-up flowchart
Survey questions
After confirming eligibility and providing informed consent, the survey consisted of 3 sections: i) participant characteristics, ii) knee OA symptoms and function, and iii) the OA-QI questionnaire. First, the participants reported their age, height and weight, gender, ethnicity, occupational status (employed, unemployed, homemaker, retired), education level (no formal education, elementary school, high school, diploma holder, degree holder, others) and housing type (public housing, condominium, terrace house, others). These variables were selected based on previous studies examining the influence of demographic and socioeconomic factors on healthcare access, treatment adherence, and functional outcomes in knee OA patients [25, 26]. The knee OA symptoms section assessed the site of symptomatic knee OA (left, right, or both) and the duration since diagnosis. These questions were informed by clinical guidelines and existing research investigating disease duration and joint involvement as potential factors influencing treatment decisions and patient-reported outcome [27].
Joint-specific pain and function were then investigated via the Knee Osteoarthritis Outcome Scale-12 (KOOS-12) [28]. The KOOS-12 is frequently used in knee OA research and consists of three sections of four items related to pain, function (activities of daily living and sport/recreation), and quality of life (QOL). Studies have demonstrated that the KOOS-12 is a reliable and valid alternative to the full-length KOOS, effectively capturing essential aspects of knee health with reduced respondent burden [29]. The participants responded to each item via a five-point Likert scale (0 represents no knee problems, and 4 represents extreme knee problems). Section scores and total KOOS-12 scores were then calculated for each participant before being normalized on a 0–100 scale. KOOS-12 data were collected at baseline and at 1 year to assess changes in functional outcomes over time. In addition, the participants completed the 17-item OA-QI questionnaire [18] at baseline only. The OA-QI questionnaire requires participants to respond to varying questions about their experience of care for their knee OA, such as “yes”, “no” or “do not remember/not relevant”. The 17 items in the OA-QI cover key aspects of non-surgical knee OA management, including referrals, clinical assessment, and treatments, and are aligned with international clinical practice guidelines. These items were developed through a systematic approach involving a comprehensive literature review, expert consultations, and iterative testing to ensure the questionnaire's reliability and feasibility [30], ensuring that the questionnaire reflects core recommendations from organizations such as the National Institute for Health and Care Excellence (NICE) [6], the Osteoarthritis Research Society International (OARSI) [7], and the American College of Rheumatology (ACR) [9]. Although guidelines differ slightly in emphasis, the OA-QI captures universally endorsed first-line treatments, such as patient education, exercise, and weight management, making it a comprehensive and valid tool for assessing adherence to best practices in knee OA care [30, 31].
Sample size estimation
The sample size was estimated with the objective of investigating the factors associated with the provision of more or less comprehensive care via G*Power 3.1.9.4. Given a type I error of 0.05 with 80% power of study, we needed data for at least 264 participants to detect a small effect size of Cohen’s f2 = 0.03 in the multiple linear regression model.
Statistical analyses
Participant responses were deidentified, given a unique identifier number and stored on a secure web-based data management application (Research Electronic Data Capture [REDCAP]). The data were cleaned and analysed by one member of the research team (LCJ) via SPSS version 26.0. The participants’ weight and height were used to calculate their body mass index (BMI kg/m2). The distribution of the continuous variables was checked, and data were deemed to be normally distributed with skewness between −2 and + 2 and kurtosis of between −7 to + 7 as suggested by Hair et al. (2013, and Bryne (2016) [32, 33], as well as a histogram with bell-shaped curve. Continuous varNIiables were presented as mean and standard deviation as they were observed to be normally distributed, while categorical variables were presented as frequency and percentage.
For the OA-QI questionnaire, only ‘yes’/’no’ responses were considered to calculate the achievement rates (i.e., any responses of ‘Don’t remember’, ‘Not overweight’, ‘No such problems’, ‘No pain/discomfort’ or ‘Not severely troubled’ were excluded from analysis). Three types of achievement rates were then calculated; i.e., i. per item (i.e., the number of ‘yes’ responses/number of participants who responded ‘yes’ or ‘no’ for that particular OA-QI item) presented as % and 95% CI, ii. Overall mean per-item OA-QI achievement rate (calculating the mean achievement rate [% and 95% CI] for all 17 OA-QI items), and iii. The mean per-person achievement rate (number of items that an individual reported ‘yes’/number of ‘yes’ or ‘no’ responses they provided) is presented as the mean and 95% CI. The mean achievement rate per person provides a measure of the ‘comprehensiveness’ of treatment.
Linear regression modelling was used to examine the factors associated with the per-person OA-QI achievement rates. The outcome was the per-person OA-QI achievement rate, while the independent variables were the baseline demographic and clinical factors. Simple linear regression was used to screen the variables, and variables with p < 0.200 were included in the variable selection process via the stepwise variable selection method. The rationale of choosing p < 0.200 was because a marginally insignificant variables suggests a statistically suggestive relationship between the independent factors and outcome variables warranting further investigation, and this cut-off has been used in other clinical researches [34].
On the other hand, multiple linear regression was used to examine the ability of the per-person OA-QI achievement rate and per-item OA-QI achievement rate to predict the 1-year change in functional outcomes, adjusting for baseline age, sex, BMI and KOOS total scores. The outcome was the change in KOOS at 1 year, while regression was performed on each OA-QI indicators separately with age, sex, BMI and baseline KOOS total score in the model. Complete case analysis was performed as the missingness at baseline was low (less than 5%) and relatively high at 1 year follow up data (35.7%) where performing multiple imputation may lead to a biased result. The multicollinearity was tested using Variance Inflation Factor (VIF) and interaction of the final model were checked, while heteroskedasticity was checked via the Bruesch-Pegan/Cook-Weisberg test for all the regression analyses. All the tests were two sided, and statistical significance was denoted by p < 0.05.
Results
We retrieved data for 314 participants. The majority of participants (83.1%) were recruited at orthopedic consultations. Participant characteristics are presented in Table 1. In summary, mean age of participants was 63.38 (SD 8.13), mean BMI was 26.05 (SD 5.98) and KOOS-12 was 64.63 (SD 15.85). Most participants were female (66.6%, n = 209/314), of Chinese ethnicity (78.7%), employed (58.2%), had attained at least high school education (47.8%), lived in public housing (83.4%) and reported bilateral knee OA symptoms (42.4%).
Table 1.
Participant characteristics
| Characteristic or outcome | N | Mean (SD) |
|---|---|---|
| Age (years) | 314 | 63.38 (8.13) |
| BMI (kg/m2) | 306 | 26.05 (5.98) |
| Total KOOS-12 score | 314 | 64.63 (15.85) |
| Subsections: | ||
| Pain | 314 | 63.82 (17.84) |
| Function in daily living (ADL) | 314 | 74.14 (19.37) |
| Knee-related quality of life (QOL) | 314 | 55.85 (18.77) |
| n (%) | ||
| Gender | ||
| Female | 314 | 209 (66.6) |
| Male | 105 (33.4) | |
| Ethnicity | ||
| Chinese | 314 | 247 (78.7) |
| Indian | 31 (9.9) | |
| Malay | 30 (9.6) | |
| Others | 6 (1.9) | |
| Occupational Status | ||
| Employed | 313 | 182 (58.2) |
| Unemployed | 14 (4.5) | |
| Homemaker | 34 (10.9) | |
| Retired | 83 (26.5) | |
| Education | ||
| No formal education | 314 | 13 (4.1) |
| Elementary school | 46 (14.6) | |
| High school | 150 (47.8) | |
| Diploma holder | 53 (16.9) | |
| Degree holder | 40 (12.7) | |
| Others | 12 (3.8) | |
| Housing | ||
| Public housing | 313 | 261 (83.4) |
| Condominium | 23 (7.3) | |
| Terrace house | 23 (7.3) | |
| Others | 6 (1.9) | |
| Localization of knee osteoarthritis | ||
| Unilateral | 314 | 181 (57.6) |
| Bilateral | 133 (42.4) | |
| Time since OA diagnosis | ||
| < 1 year | 313 | 45 (14.4) |
| 1 to 3 years | 103 (32.9) | |
| 4 to 6 years | 70 (22.4) | |
| 7–10 years | 69 (22.0) | |
| more than 10 years | 26 (8.3) | |
BMI Body mass index
Per-item and overall mean per-item and per-person OA-QI achievement rates
The per-item and overall mean per-item OA-QI achievement rates are presented in Table 2. In summary, large variation was observed between each indicator (ranging from 15.68%—87.50%). The highest per-item achievement rates were for referrals for physical activity (mean [95% CI] 87.50%, [83.31, 90.96]), physical activity education (mean [95% CI] 82.74% [78.03, 86.79]) and pain assessment (mean [95% CI] 80.97% [75.96, 85.33]). The lowest per-item achievement rates were for referrals to daily activity aid assessment (mean [95% CI] 15.68% [7.02, 28.59]), referrals to walking aid assessment (mean [95% CI] 25.61% [16.60, 35.1]) and weight reduction referrals (mean [95% CI] 27.41% [21.31, 34.20]). Overall, the mean per-item OA-QI achievement rate was 62.21% (95% CI: 59.71, 64.71).
Table 2.
Per-item and overall mean per-item OA-QI achievement rates
|
Answered Yes or No n = /314 |
Answered Yes n = |
Achievement rate | ||
|---|---|---|---|---|
| OA-QI indicator |
Per- item % |
95% CI Lower, Upper |
||
| Disease development | 279 | 182 | 65.23 | 59.33, 70.81 |
| Treatment | 305 | 203 | 66.56 | 60.96, 71.83 |
| Self-management | 299 | 145 | 48.49 | 42.70, 54.32 |
| Lifestyle | 299 | 164 | 54.85 | 49.02, 60.58 |
| Physical activity | 307 | 254 | 82.74 | 78.03, 86.79 |
| Referral physical activity | 312 | 273 | 87.50 | 83.31, 90.96 |
| Weight reduction | 196 | 149 | 76.02 | 69.42, 81.82 |
| Referral weight reduction | 197 | 54 | 27.41 | 21.31, 34.20 |
| Functional assessment | 97 | 51 | 52.58 | 42.18, 62.81 |
| Walking aid assessment | 82 | 21 | 25.61 | 16.60, 35.1 |
| Other aids assessment | 51 | 8 | 15.68 | 7.02, 28.59 |
| Pain assessment | 289 | 234 | 80.97 | 75.96, 85.33 |
| Paracetamol | 280 | 208 | 74.28 | 68.75, 79.30 |
| Stronger pain killers | 193 | 100 | 51.81 | 44.52, 59.05 |
| NSAIDS information | 184 | 84 | 45.65 | 38.31, 53.14 |
| Joint injection | 177 | 87 | 49.15 | 41.57, 56.76 |
| Surgery | 120 | 62 | 51.67 | 42.37, 60.88 |
| Mean overall OA-QI achievement rate | 314 | 62.21 | 59.71, 64.71 | |
Associations of per-person OA-QI achievement rates with participant characteristics
Differences in mean per-person achievement rates between categorical outcomes are presented, and the relationships between demographics and the OA-QI achievement rate are reported in Table 3. Three significant relationships were observed: i) those who were identified as Indian ethnicity had higher mean per-person OA-QI achievement rates than those who were identified as Chinese (adj. coef [95% CI], 10.94 [2.70, 19.17], p = 0.009); ii) those who lived in public housing had higher mean per-person OA-QI achievement rates than those who resided in condominiums did (adj. coef [95% CI], −12.02 [−21.64, −2.41], p = 0.014); and iii) those who had had osteoarthritis for less than 1 year had lower mean per-person OA-QI achievement rates than those who had been living with osteoarthritis for 1–3 years (adjusted coefficient [95% CI], 9.37 [1.60, 17.15], p = 0.018), 4–6 years (adjusted coefficient [95% CI], 11.27 [2.99, 19.55], p = 0.008), 7–10 years (adjusted coefficient [95% CI], 10.26 [1.92, 18.60], p = 0.016) and 10 + years (adjusted coefficient [95% CI], 13.70 [3.01, 24.38], p = 0.012), respectively.
Table 3.
Comparison of the mean per-person OA-QI achievement rate with demographic outcomes
| Characteristic | OA-QI achievement rate, mean (95% CI) | Coef (95% CI) |
p value | Adj. coef (95% CI) |
P value |
|---|---|---|---|---|---|
| Age | NA | −0.26 (−0.57, 0.04) | 0.09 | - | - |
| Gender | |||||
| Male | 62.00 (57.37, 66.63) | Ref | - | - | - |
| Female | 62.31 (59.33, 65.29) | 0.31 (−5.00, 5.62) | 0.91 | - | - |
| Ethnicity | |||||
| Chinese | 61.14 (58.30, 63.98) | Ref | - | Ref | - |
| Malay | 59.30 (51.76, 66.84) | −1.84 (−10.34, 6.67) | 0.67 | - | - |
| Indian | 71.60 (63.20, 80.01) | 10.47 (2.08, 18.85) | 0.02 | 10.94 (2.70, 19.17) | 0.01 |
| Others | 72.24 (56.39, 88.10) | 11.11 (−7.07, 29.28) | 0.23 | - | - |
| BMI | NA | −0.21 (−0.63, 0.22) | 0.34 | - | - |
| Occupational Status | |||||
| Employed | 63.55 (60.23, 66.87) | Ref | - | - | - |
| Unemployed | 64.20 (49.30, 79.10) | 0.65 (−11.65, 12.96) | 0.92 | - | - |
| Homemaker | 63.42 (56.07, 70.77) | −0.12 (−8.41, 8.17) | 0.98 | - | - |
| Retired | 58.38 (53.52, 63.25) | −5.16 (−11.04, 0.71) | 0.09 | - | - |
| Education | |||||
| No formal education | 54.93 (45.43, 64.44) | Ref | - | - | - |
| Elementary school | 63.03 (57.20,68.87) | 8.10 (−5.90, 22.10) | 0.26 | - | - |
| High school | 62.79 (58.99, 66.59) | 7.86 (−5.03, 20.74) | 0.23 | - | - |
| Diploma holder | 61.14 (54.57, 67.72) | 6.21 (−7.58, 20.00) | 0.38 | - | - |
| GCE A level, IB | 62.52 (55.47, 69.57) | 7.58 (−6.64, 21.81) | 0.30 | - | - |
| University | 63.29 (47.90, 78.67) | 8.35 (−9.49, 26.19) | 0.36 | - | - |
| Housing | |||||
| Public housing | 62.58 (59.82, 65.34) | Ref | - | Ref | - |
| Condominium | 51.81 (42.96, 60.67) | −10.77 (−20.36, −1.17) | 0.03 | −12.02 (−21.64, −2.41) | 0.01 |
| Terrace house | 65.61 (56.04, 75.19) | 3.03 (−6.56, 2.63) | 0.54 | - | - |
| Others | 69.79 (49.70, 89.88) | 7.21 (−11.01, 25.43) | 0.44 | - | - |
| Localization of knee osteoarthritis | |||||
| Unilateral | 62.01 (58.64, 65.38) | Ref | - | - | - |
| Bilateral | 62.48 (58.71, 66.24) | 0.47 (−4.60, 5.54) | 0.86 | - | - |
| Time since OA diagnosis | |||||
| < 1 year | 54.03 (46.42, 61.63) | Ref | - | Ref | - |
| 1 to 3 years | 61.92 (57.78, 66.05) | 7.89 (0.02, 15.76) | 0.05 | 9.37 (1.60, 17.15) | 0.02 |
| 4 to 6 years | 64.69 (59.57, 69.82) | 10.67 (2.25, 19.09) | 0.01 | 11.27 (2.99, 19.55) | 0.01 |
| 7–10 years | 63.44 (57.81, 69.08) | 9.42 (0.97, 17.86) | 0.03 | 10.26 (1.92, 18.60) | 0.02 |
| more than 10 years | 66.93 (58.42, 75.45) | 12.91 (205, 23.76) | 0.02 | 13.70 (3.01, 24.38) | 0.01 |
| KOOS | NA | −0.12 (−0. 27, 0.04) | 0.15 | - | - |
| Pain | NA | −0.02 (−0.16, 0.12) | 0.77 | - | - |
| ADL | NA | −0.12 (−0.24, 0.01) | 0.08 | - | - |
| QoL | NA | −0.11 (−0.24, 0.02) | 0.10 | - | - |
BMI Body Mass Index, ADL Activities of Daily Living, QoL Quality of Life
Relationships of per-item and per-person OA-QI achievement rates with functional outcomes at 1 year
One-year follow-up data were available for 202 participants. The relationships between the per-item OA-QI achievement rate and functional outcomes at 1 year are presented in Table 4. In summary, those who indicated that they had walking issues and indicated that they did not receive a walking aid assessment had poorer outcomes after 1 year (adjusted coefficient [95% CI]: −9.89 (−19.63, −0.15); p = 0.047). In addition, those who were not informed about injection or surgical options had greater improvements in the KOOS-12 score at 1 year than did those who received information about injections (adjusted coefficient [95% CI]: 7.23 [1.42–13.04]; p = 0.015) or surgery (adjusted coefficient [95% CI]: 12.65 [5.89–19.40]; p < 0.001), respectively. The relationships between the per-person achievement rate and functional outcomes at 1 year are presented in Table 5. In summary, no significant associations were observed.
Table 4.
Relationships between the per-item OA-QI achievement rate and changes in functional outcomes (total KOOS-12) at 1 year
| OA-QI Indicator | KOOS12 change Mean ± SD |
Adj Coeff (95% CI) |
P value |
|---|---|---|---|
| 1. Disease development | |||
| No | 3.98 ± 16.96 | Ref | |
| Yes | 4.61 ± 15.60 | −0.83 (−6.03, 4.37) | 0.75 |
| 2. Treatment | |||
| No | 3.52 ± 17.07 | Ref | |
| Yes | 5.44 ± 15.30 | 1.78 (−3.21, 6.78) | 0.48 |
| 3. Self-management | |||
| No | 2.32 ± 16.58 | Ref | |
| Yes | 5.71 ± 16.06 | 3.16 (−1.39, 7.71) | 0.17 |
| 4. Lifestyle | |||
| No | 3.97 ± 16.24 | Ref | |
| Yes | 4.25 ± 16.76 | −0.33 (−5.11, 4.45) | 0.89 |
| 5. Physical activity | |||
| No | 3.91 ± 17.00 | Ref | |
| Yes | 4.70 ± 13.70 | 0.73 (−5.16, 6.63) | 0.81 |
| 6. Referral physical activity | |||
| No | 4.54 ± 16.52 | Ref | |
| Yes | −0.45 ± 14.87 | −2.54 (−9.44, 4.35) | 0.47 |
| 7. Weight reduction | |||
| No | 4.27 ± 17.35 | Ref | |
| Yes | 5.73 ± 12.34 | 0.37 (−6.47, 7.21) | 0.92 |
| 8. Referral weight reduction | |||
| No | 8.23 ± 17.13 | Ref | |
| Yes | 2.20 ± 16.90 | −4.69 (−10.71, 1.32) | 0.13 |
| 9. Functional assessment | |||
| No | 3.27 ± 17.87 | Ref | |
| Yes | 0.77 ± 16.95 | −2.53 (−10.10, 5.04) | 0.51 |
| 10. Walking aid assessment | |||
| No | 14.26 ± 14.46 | Ref | |
| Yes | 3.99 ± 18.19 | −9.89 (−19.63, −0.15) | 0.047 |
| 11. Other aids assessment | |||
| No | 6.60 ± 18.70 | Ref | |
| Yes | −3.49 ± 17.76 | −6.52 (21.13, 8.09) | 0.38 |
| 12. Pain assessment | |||
| No | 3.84 ± 16.09 | Ref | |
| Yes | 6.03 ± 17.40 | 2.36 (−3.39, 8.10) | 0.42 |
| 13. Paracetamol | |||
| No | 3.29 ± 16.94 | Ref | |
| Yes | 6.25 ± 15.24 | 4.37 (−0.97, 9.70) | 0.11 |
| 14. Stronger pain killers | |||
| No | 3.28 ± 17.71 | Ref | |
| Yes | 5.65 ± 14.05 | 4.18 (−1.39, 9.75) | 0.14 |
| 15. NSAIDS information | |||
| No | 2.73 ± 18.66 | Ref | |
| Yes | 6.89 ± 14.27 | 4.93 (−0.80, 10.66) | 0.09 |
| 16. Joint injection | |||
| No | 0.65 ± 17.24 | Ref | |
| Yes | 6.19 ± 17.10 | 7.23 (1.42, 13.04) | 0.02 |
| 17. Surgery | |||
| No | −4.98 ± 18.24 | Ref | |
| Yes | 8.39 ± 16.78 | 12.65 (5.89, 19.40) | < 0.001 |
Adjusted for age, sex, BMI and total KOOS score at baseline
Table 5.
Relationships between the per-person OA-QI achievement rate and changes in functional outcomes at 1 year
| Outcome | Adj. Coeff | 95% CI | p value |
|---|---|---|---|
| KOOS Total | −0.05 | −0.16 0.05 | 0.31 |
| KOOS Pain | −0.07 | −0.19, 0.04 | 0.22 |
| KOOS ADL | −0.02 | −0.14, 0.10 | 0.76 |
| KOOS QoL | −0.07 | −0.21, 0.07 | 0.31 |
Adjusted for age, sex, BMI and total KOOS score at baseline
Discussion
In general, the quality indicator achievement rates were underwhelming but were similar to those reported in previous research from outside Asia [19, 21, 22]. Similar to previous research, high achievement rates were observed for patient education on physical activity (87.5%), reflecting global recognition of exercise as a cornerstone of knee OA management. However, referrals for weight management (50%) and walking aid assessments (15.7%) were notably lower, consistent with findings from UK and Canadian studies, where non-pharmacological interventions beyond exercise were also underutilized. These similarities suggest that even in well-resourced healthcare settings, gaps persist in delivering comprehensive non-surgical care. In the Singaporean context, factors such as clinician awareness, healthcare system accessibility, and patient perceptions of these interventions may contribute to the observed trends.
Encouragingly, participants frequently reported being provided with information about first-line interventions, namely, physical activity, exercise, and weight loss. However, information about self-management and coping strategies is infrequently provided, and referrals to specialist weight loss or supportive services (e.g., walking aids and splints) are rarely provided when indicated. The overall quality of care provided was associated with participant ethnicity, housing type, and time since diagnosis, suggesting that care is provided inconsistently. Furthermore, the provision of information about certain topics (i.e., walking aids, injections or surgery) was associated with functional outcomes at 1 year.
It is important to note that the patients recruited for this study were patient referred from primary care to these hospitals. This means that their symptoms were either severe enough or had persisted long enough to warrant referral from primary care to a specialist center. As a result, the need for more extensive treatment discussions—including stronger pain medications or surgical options—was likely appropriate for many participants.
However, not all patients may require extensive treatment information at an early stage of knee OA. While comprehensive patient education is essential, delivering information about advanced interventions too early (e.g., corticosteroid injections, surgery) could cause unnecessary concern or discourage engagement with non-surgical strategies. Future initiatives should tailor the timing and depth of education based on the patient’s disease severity and individual needs. Overall, our findings can be used to inform initiatives to improve the quality of care that is being provided to people with knee OA in Singapore.
Improving the quality of osteoarthritis care in Singapore
Encouragingly, most participants reported being provided information about, and referred to, an appropriate service for, physical activity and exercise, considering that three-quarters of people with knee OA in Singapore reported low levels of physical activity [35]. Physical activity and exercise should be encouraged in this population, as they are inexpensive and effective guidelines that recommend first-line interventions that are suitable for all people regardless of age, sex, ethnicity or severity of the disease [6]. However, other important information that may facilitate becoming more physically active, such as lifestyle changes or coping strategies, is often not provided. Encouragingly, weight management was reported as being discussed with the majority of individuals for whom it was appropriate. However, disappointingly, only one in two people were referred to appropriate weight loss services. Considering that weight management is an integral part of guideline-adherent care [6–8], the reasons for the lack of referrals should be investigated further. Improving knowledge about, and access to, weight management services, among other services for which referral rates are low (i.e., walking and daily mobility aids) available in Singapore, has great potential to improve patient outcomes for patients with knee OA and its associated comorbidities.
An investigation of the relationship of the per-item OA-QI achievement rate with 1-year KOOS-12 outcomes revealed that participants who experienced acute deterioration of symptoms and who were engaged in a discussion about corticosteroid injections had worse 1-year KOOS-12 outcomes than those who also experienced an acute exacerbation but did not engage in a discussion about corticosteroid injections. However, we are unable to tell if an injection was actually offered or received. Injections are widely perceived as a treatment option to provide immediate symptom relief during an acute exacerbation [36]. One possible explanation for our findings is that patients who discussed injections may have had more severe symptoms or more persistent functional limitations, which could have influenced their treatment trajectory. Given that our study population was hospital-referred, it is likely that these patients had already exhausted some non-surgical options before considering injections, potentially contributing to worse functional outcomes at 1 year. Additionally, discussion of injections might have influenced treatment decisions, leading some patients to prioritize short-term symptom relief over long-term strategies such as physical therapy or lifestyle modifications, which are essential for sustained functional improvement and behavioural change [37]. Further research is needed to determine whether the provision of information on injections reflects underlying disease severity rather than acting as a direct predictor of poorer outcomes and to examine how discussions about different treatment options influence patient adherence to long-term management strategies.
We also observed that participants who experienced walking difficulties but were not assessed for walking aids had poorer outcomes in their 1-year KOOS than did those whose need for walking aids was evaluated. This observation suggests a potential benefit of walking aid assessment in knee OA patients experiencing mobility challenges. The assessment and subsequent use of walking aids might contribute to better outcomes by improving mobility, reducing pain, and enhancing overall quality of life [6]. This aligns with the literature emphasizing the importance of addressing mobility issues in osteoarthritis management [6–8].
Going beyond quality of care to achieve good outcomes
We did not identify any significant relationships between age, sex, BMI, education, or severity of knee symptoms and the per-person OA-QI achievement rate. However, we did observe that individuals of Indian ethnicity and those residing in public housing had higher per-person OA-QI achievement rates (indicating more comprehensive care) than those who were of Chinese ethnicity or who were residing in condominiums, respectively. These findings were unexpected, and the reasons behind these associations are not immediately clear. It is possible that socioeconomic factors, cultural attitudes towards healthcare, or accessibility to healthcare resources could play a role. However, without further research specifically targeting these demographics, it is challenging to draw definitive conclusions. Importantly, these findings should also be interpreted with caution because of the lower sample sizes in the comparator groups. Further research is encouraged to understand the complex interplay of ethnicity, living conditions, and healthcare quality in the context of knee OA treatment.
We did not identify any relationship between the comprehensiveness of care (i.e., per-person OA-QI achievement rate) at baseline and 1-year KOOS-12 outcomes. One potential explanation for this finding is the multifactorial nature of health outcomes in patients with knee OA. The quality of clinical care contributes to only 20% of the social determinants of health. Other factors, such as socioeconomic status (40%), the physical environment (10%), and health behaviors (30%), play greater roles in determining and improving health [38, 39]. These findings suggest that factors other than the quality of care might have a more significant impact on KOOS outcomes than the comprehensiveness of osteoarthritis care alone [40–42]. This underscores the complexity of healthcare outcomes and the necessity of adopting a holistic approach for managing knee OA, which takes into account the wide array of factors influencing patient health and well-being. Our findings suggest that while comprehensiveness or quality of care is undoubtedly important, it is just one of many components that contributes to overall health outcomes in patients with knee OA. Much of osteoarthritis care needs to be targeted at behavioral changes, and one session of information might not be sufficient to provide the necessary push to lead to such changes [37].
Strengths and Limitations
One key strength of this study is that it was adequately powered to assess associations between OA-QI achievement rates and functional outcomes, providing robust statistical analysis and reliable conclusions. Additionally, this study provides valuable insights into the quality of knee OA care in Singapore, a region where such evaluations have been limited. By applying a validated, internationally recognized quality indicator (OA-QI) questionnaire, we were able to systematically assess adherence to evidence-based non-surgical management guidelines. The depth and breadth of our analysis also help identify specific gaps in clinical practice, which could inform future quality improvement initiatives.
However, our findings may not be fully generalizable to all individuals with knee osteoarthritis in Singapore. Singapore is a unique country in Asia with a diverse ethnic composition and relatively high average income levels, meaning that our results may not be representative of the wider Asian region. Additionally, the majority of participants in our study were recruited through orthopedic surgeons, which presents a potential limitation due to selection bias. Patients seen in orthopedic settings are likely to have more severe or long-standing symptoms and may have already exhausted non-surgical treatment options before being referred. As a result, their responses may not reflect the experiences of individuals with milder OA who are primarily managed in primary care settings. These differences could influence perceived treatment accessibility, referral rates, and overall quality indicator achievement rates, as primary care physicians may emphasize earlier-stage interventions such as lifestyle modifications and physical therapy before referring to specialists.
Additionally, this study did not collect deformity severity, which could have provided further insights into structural disease progression and treatment response. Deformity severity was not prioritized as it does not always correlate with symptoms or functional limitations. However, we recognize that it may play a role in treatment decision-making and long-term outcomes, and future studies could study its impact more comprehensively.
While we collected time since OA diagnosis, we did not include treatment duration as a covariate due to conceptual challenges in defining it accurately. Treatment exposure varies widely among patients—some may have long-standing symptoms but minimal engagement with healthcare services, while others may have short symptom duration but extensive treatment histories. Without detailed data on treatment history and intensity, adjusting for treatment duration could introduce misclassification bias, potentially leading to misleading conclusions. Future research should consider a more nuanced approach to measuring treatment exposure, incorporating both duration and intensity of care received.
Furthermore, incorporating each KOOS-12 subscale separately as covariates risked overfitting, given our sample size, potentially leading to spurious associations. While the subscales capture distinct patient-reported outcomes, we opted for the total KOOS-12 score as a composite measure to maintain model robustness. Future studies with larger cohorts and detailed symptom tracking should explore the independent influence of subscales.
Another limitation is our reliance on self-reported data, which introduces the potential for recall bias and inaccuracies in patient responses. This underscores the need for more robust assessment methods, such as qualitative interviews or documentation reviews, to cross-validate findings.
Despite these limitations, our study provides important insights into the quality of knee OA care in a hospital-referred population and highlights opportunities for improving non-surgical management strategies. Future studies should aim to build on these findings by expanding to primary care settings and incorporating additional data sources.
Conclusion
This study provides valuable insights into the quality of osteoarthritis care in Singapore, highlighting both strengths and areas for improvement. Encouragingly, high achievement rates were observed in key areas such as physical activity referrals, patient education, and pain assessment, which align with international care standards. However, significant gaps remain, particularly in referrals for daily activity aids, walking aid assessments, and comprehensive weight management support, indicating opportunities for improvement in non-surgical knee OA care. Notably, the OA-QI did not serve as a strong predictor of 1-year functional outcomes, suggesting that patient outcomes are influenced by multifaceted factors beyond traditional quality indicators. This underscores the complexity of knee OA management, where socioeconomic status, treatment adherence, and behavioral factors may play a crucial role in long-term prognosis. Overall, while some aspects of knee OA management meet global best practices, this study highlights the need for a more holistic and individualized approach to care delivery, ensuring equitable access to essential interventions for all patients. Future research should further study these multifactorial influences, helping to develop more effective, patient-centered treatment strategies for individuals with knee OA.
Acknowledgements
We would like to thank Pearl Koh Yuan Zhen and Koong Mun Ee for their initial work on this project.
This study was supported by the National Medical Research Council (NMRC) Population Health Research Grant, which provided funding for this project.
Clinical trial number
Not applicable.
Authors’ contributions
LT and AG were the main manuscript writers. CJ ran the statistical analysis of the paper as well as the writing of the results section. BT gave guidance and feedback on the study. All authors reviewed the manuscript.
Funding
None to declare.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from National Healthcare group, Domain Specific Review Board, Ref no. 2021/01113 and patient informed consent was taken prior to taking part in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vos T, Lim SS, Abbafati C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung YY, Ma S, Noviani M. Validation of screening questionnaires for evaluation of knee osteoarthritis prevalence in the general population of Singapore. Int J Rheum Dis. 2018;21(3):629–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turkiewicz A, Petersson IF, Björk J. Current and future impact of osteoarthritis on health care: a population-based study with projections to year 2032. Osteoarthritis Cartilage. 2014;22(11):1826–32. [DOI] [PubMed] [Google Scholar]
- 4.Cross M, Smith E, Hoy D. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30. [DOI] [PubMed] [Google Scholar]
- 5.Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59. [DOI] [PubMed] [Google Scholar]
- 6.National Institute for Health and Care Excellence (NICE). Osteoarthritis: care and management in adults. London: NICE; 2014. Available from: https://www.nice.org.uk/guidance/cg177.
- 7.Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–89. [DOI] [PubMed] [Google Scholar]
- 8.Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–35. [DOI] [PubMed] [Google Scholar]
- 9.Kolasinski SL, Neogi T, Hochberg MC. American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2019;72(2):220–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skou ST, Roos EM, Laursen MB. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthritis Cartilage. 2018;26(9):1170–80. [DOI] [PubMed] [Google Scholar]
- 11.Skou ST, Roos E, Laursen M. Cost-effectiveness of total knee replacement in addition to non-surgical treatment: a 2-year outcome from a randomised trial in secondary care in Denmark. BMJ Open. 2020;10(1):e033495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skou ST, Roos EM, Laursen MB. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373(17):1597–606. [DOI] [PubMed] [Google Scholar]
- 13.Xie F, Thumboo J, Fong KY. Direct and indirect costs of osteoarthritis in Singapore: a comparative study among multiethnic Asian patients with osteoarthritis. J Rheumatol. 2007;34(1):165–71. [PubMed] [Google Scholar]
- 14.Allen KD, Choong PF, Davis AM. Osteoarthritis: models for appropriate care across the disease continuum. Best Pr Res Clin Rheumatol. 2016;30(3):503–35. [DOI] [PubMed] [Google Scholar]
- 15.Bennell KL, Bayram C, Harrison C. Trends in management of hip and knee osteoarthritis in general practice in Australia over an 11-year window: a nationwide cross-sectional survey. Lancet Reg Health-West Pac. 2021;12:100187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cronström A, Dahlberg LE, Nero H, Hammarlund CS. I was considering surgery because I believed that was how it was treated”: a qualitative study on willingness for joint surgery after completion of a digital management program for osteoarthritis. Osteoarthritis Cartilage. 2019;27(7):1026–32. [DOI] [PubMed] [Google Scholar]
- 17.Hunter DJ, Neogi T, Hochberg MC. Quality of osteoarthritis management and the need for reform in the US. Arthritis Care Res. 2011;63(1):31–8. [DOI] [PubMed] [Google Scholar]
- 18.Østerås N, Garratt A, Grotle M, Natvig B, Kjeken I, Kvien TK. Patient-reported quality of care for osteoarthritis: development and testing of the osteoarthritis quality indicator questionnaire. Arthritis Care Res. 2013;65. 10.1002/acr.21976. [DOI] [PubMed]
- 19.Ingelsrud LH, Roos EM, Gromov K, Jensen SS, Troelsen A. Patients report inferior quality of care for knee osteoarthritis prior to assessment for knee replacement surgery–a cross-sectional study of 517 patients in Denmark. Acta Orthop. 2020;91(1):82–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blackburn S, Higginbottom A, Taylor R, et al. Patient-reported quality indicators for osteoarthritis: a patient and public generated self-report measure for primary care. Res Involv Engagem. 2016;2(1):1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grønhaug G, Østerås N, Hagen KB. Quality of hip and knee osteoarthritis management in primary health care in a Norwegian county: a cross-sectional survey. BMC Health Serv Res. 2014;14(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larmer PJ, Bennett K, Baldwin JN, Bassett S, O’Brien DW. Quality indicators for hip and knee osteoarthritis management in New Zealand: A patient survey. N Z J Physiother. 2019;47(3):183–92. [Google Scholar]
- 23.Tan BY, Goh ZZS, Lim CJ, et al. Singapore KneE osTeoarthritis CoHort (SKETCH): protocol for a multi-centre prospective cohort study. BMC Musculoskelet Disord. 2023;24(1):104. 10.1186/s12891-023-06207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7. [DOI] [PubMed] [Google Scholar]
- 25.Boddu SP, Gill VS, Haglin JM, Brinkman JC, Deckey DG, Bingham JS. Lower Income and Nonheterosexual Orientation Are Associated With Poor Access to Care in Patients With Knee Osteoarthritis. Arthroplasty Today. 2024;27: 101353. 10.1016/j.artd.2024.101353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reyes AM, Katz JN. Racial/Ethnic and Socioeconomic Disparities in Osteoarthritis Management. Rheum Dis Clin North Am. 2021;47(1):21–40. 10.1016/j.rdc.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heidari B. Knee osteoarthritis diagnosis, treatment and associated factors of progression: part II. Casp J Intern Med. 2011;2(3):249–55. [PMC free article] [PubMed] [Google Scholar]
- 28.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 29.Gandek B, Roos EM, Franklin PD, Ware JE. A 12-item short form of the Knee injury and Osteoarthritis Outcome Score (KOOS-12): tests of reliability, validity and responsiveness. Osteoarthritis Cartilage. 2019;27(5):762–70. 10.1016/j.joca.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 30.Østerås N, Hagen K, Garratt A, et al. Quality of osteoarthritis care: test-retest reliability and feasibility of the osteoarthritis quality indicator questionnaire. Osteoarthritis Cartilage. 2012;20:185–6. [Google Scholar]
- 31.Gandek B, Roos EM, Franklin PD, Ware JE. A 12-item short form of the Knee injury and Osteoarthritis Outcome Score (KOOS-12): tests of reliability, validity and responsiveness. Osteoarthritis Cartilage. 2019;27:762. 10.1016/j.joca.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 32.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 7th ed. Essex: Pearson Education Limited; 2013.
- 33.Byrne BM. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming, 3rd. Routledge; 2016. 10.4324/9781315757421.
- 34.Wang YX, Yang H, Luo H, et al. Peripapillary Scleral Bowing Increases with Age and is Inversely Associated with Peripapillary Choroidal Thickness in Healthy Eyes. Am J Ophthalmol. 2020;217:91–103. 10.1016/j.ajo.2020.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goff AJ, Jones LE, Lim CJ, Tan BY. A cross sectional study exploring the relationship of self-reported physical activity with function, kinesiophobia, self-efficacy and quality of life in an Asian population seeking care for knee osteoarthritis. BMC Musculoskelet Disord. 2024;25(1):74. 10.1186/s12891-024-07181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayub S, Kaur J, Hui M, et al. Efficacy and safety of multiple intra-articular corticosteroid injections for osteoarthritis-a systematic review and meta-analysis of randomized controlled trials and observational studies. Rheumatol Oxf Engl. 2021;60(4):1629–39. 10.1093/rheumatology/keaa808. [DOI] [PubMed] [Google Scholar]
- 37.Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS ONE. 2019;14(7): e0219482. 10.1371/journal.pone.0219482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rethorn ZD. Association of Burden and Prevalence of Arthritis With Disparities in Social Risk Factors, Findings From 17 US States. Prev Chronic Dis. 2022;19. 10.5888/pcd19.210277. [DOI] [PMC free article] [PubMed]
- 39.Whitman A, De Lew N, Chappel A, Aysola V, Zuckerman R, Sommers BD. Addressing social determinants of health: examples of successful evidence-based strategies and current federal efforts. Office of the Assistant Secretary for Planning and Evaluation. 2022. Available from: https://aspe.hhs.gov/reports/sdoh-evidence-review.
- 40.Allen KD, Golightly YM. State of the evidence. Curr Opin Rheumatol. 2015;27(3). https://journals.lww.com/co-rheumatology/fulltext/2015/05000/state_of_the_evidence.12.aspx. [DOI] [PMC free article] [PubMed]
- 41.Reyes C, Garcia-Gil M, Elorza JM, et al. Socio-economic status and the risk of developing hand, hip or knee osteoarthritis: a region-wide ecological study. Osteoarthritis Cartilage. 2015;23(8):1323–9. 10.1016/j.joca.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 42.Felson DT, Niu J, Clancy M, Sack B, Aliabadi P, Zhang Y. Effect of recreational physical activities on the development of knee osteoarthritis in older adults of different weights: the Framingham Study. Arthritis Rheum. 2007;57(1):6–12. 10.1002/art.22464. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.