Abstract
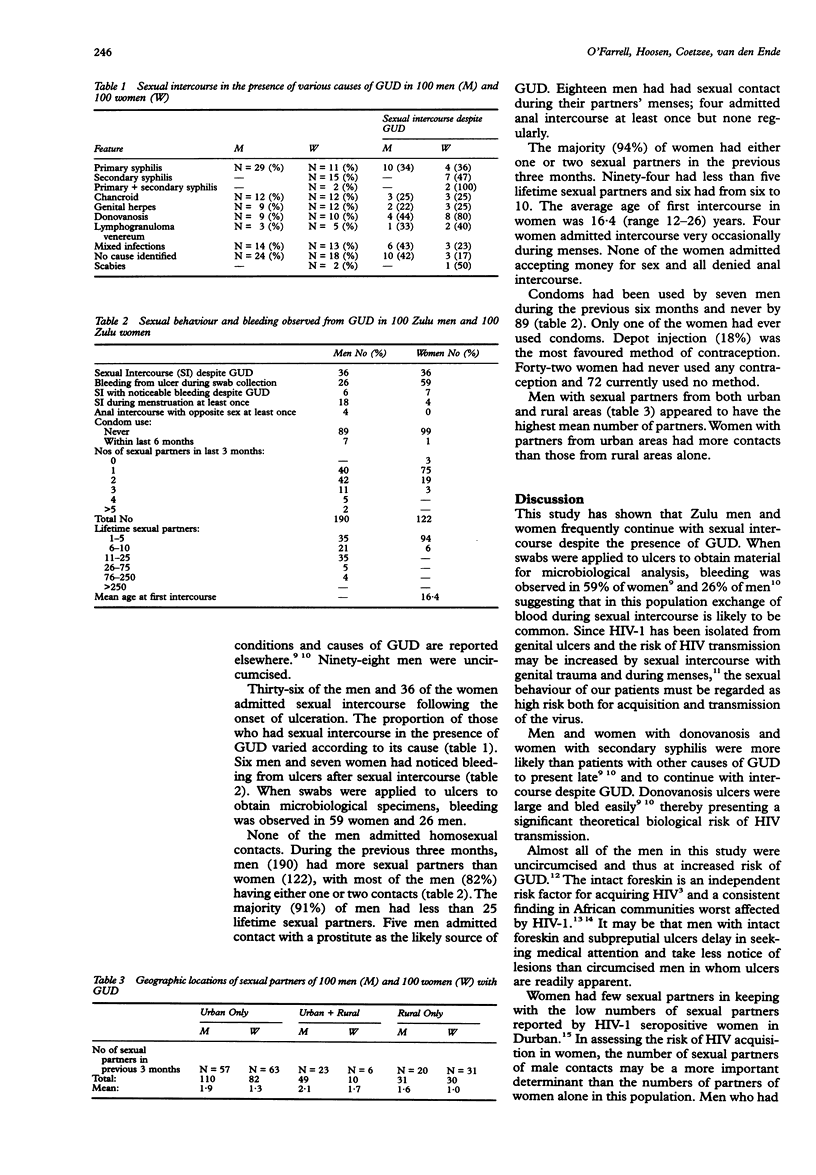
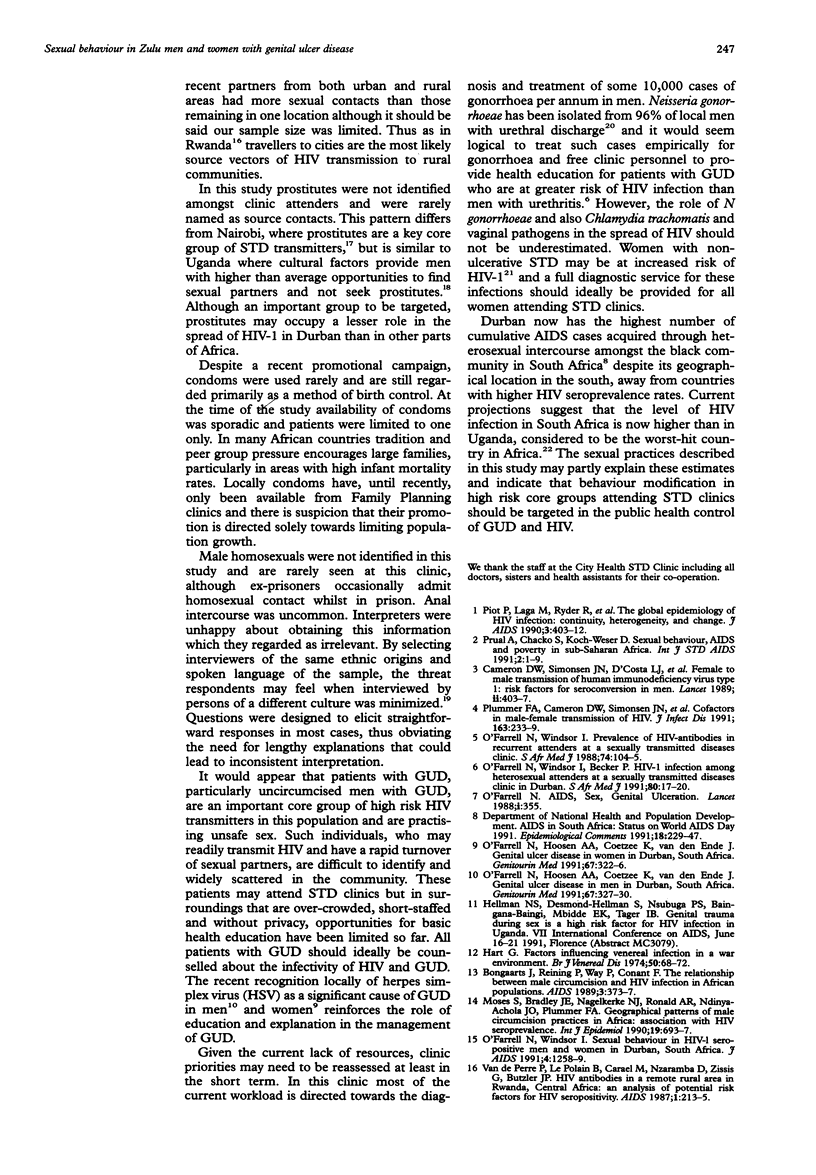
OBJECTIVE--To investigate patterns of sexual behaviour in men and women with genital ulcer disease (GUD) and their relevance to HIV-1 transmission. METHODS--A sexual behaviour questionnaire was administered by the same interviewer to all participants who were also entered into a study of the microbial aetiology of GUD. SETTING--City Health Sexually Transmitted Diseases Clinic, King Edward VIII Hospital, Durban, South Africa. PARTICIPANTS--100 Zulu men and 100 Zulu women. RESULTS--36 (%) of men and 36 (%) of women had continued with sexual intercourse despite GUD. Patients with donovanosis and secondary syphilis were more likely than those with other causes of GUD to have intercourse despite ulcers. During swab collection bleeding was observed from ulcers in 59 women and 26 men. Prostitutes were not identified and were rarely named as source contacts. Men had more sexual partners (190) than women (122) during the previous three months. Condom use was minimal. Men who migrated between urban and rural areas appeared to have the most sexual partners. Urban women had more partners than women from rural areas. CONCLUSIONS--Men and women with GUD are practising riskful sexual behaviour and could benefit from behaviour modification programmes. In this community men who travel between urban and rural areas and who present late with GUD that bleeds easily are probably the most important high-frequency HIV transmitter core group. A significant potential risk of blood to blood contact during sexual intercourse exists in patients with GUD.
Full text
PDF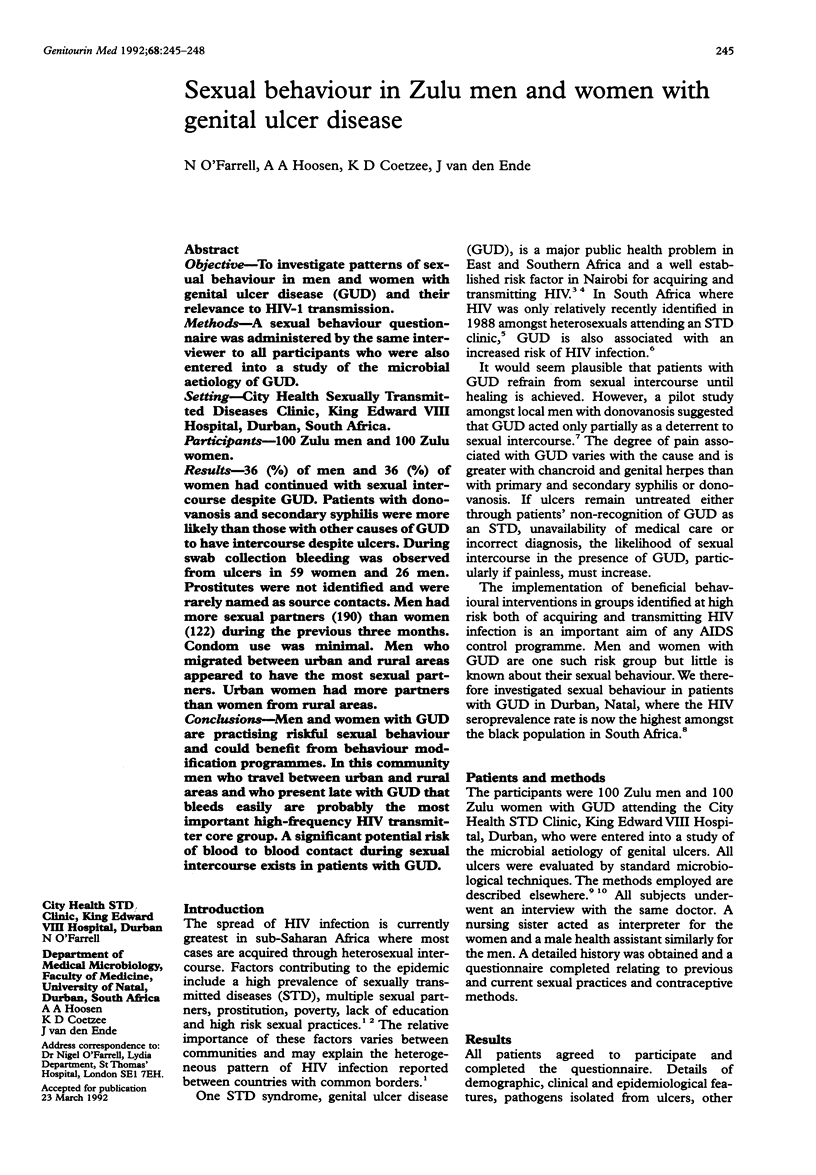

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bongaarts J., Reining P., Way P., Conant F. The relationship between male circumcision and HIV infection in African populations. AIDS. 1989 Jun;3(6):373–377. doi: 10.1097/00002030-198906000-00006. [DOI] [PubMed] [Google Scholar]
- Cameron D. W., Simonsen J. N., D'Costa L. J., Ronald A. R., Maitha G. M., Gakinya M. N., Cheang M., Ndinya-Achola J. O., Piot P., Brunham R. C. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet. 1989 Aug 19;2(8660):403–407. doi: 10.1016/s0140-6736(89)90589-8. [DOI] [PubMed] [Google Scholar]
- Hart G. Factors influencing venereal infection in a war environment. Br J Vener Dis. 1974 Feb;50(1):68–72. doi: 10.1136/sti.50.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson A. Social context of human immunodeficiency virus transmission in Africa: historical and cultural bases of east and central African sexual relations. Rev Infect Dis. 1989 Sep-Oct;11(5):716–731. doi: 10.1093/clinids/11.5.716. [DOI] [PubMed] [Google Scholar]
- Moses S., Bradley J. E., Nagelkerke N. J., Ronald A. R., Ndinya-Achola J. O., Plummer F. A. Geographical patterns of male circumcision practices in Africa: association with HIV seroprevalence. Int J Epidemiol. 1990 Sep;19(3):693–697. doi: 10.1093/ije/19.3.693. [DOI] [PubMed] [Google Scholar]
- Moses S., Plummer F. A., Ngugi E. N., Nagelkerke N. J., Anzala A. O., Ndinya-Achola J. O. Controlling HIV in Africa: effectiveness and cost of an intervention in a high-frequency STD transmitter core group. AIDS. 1991 Apr;5(4):407–411. [PubMed] [Google Scholar]
- O'Farrell N. AIDS, sex, and genital ulceration. Lancet. 1988 Feb 13;1(8581):355–355. doi: 10.1016/s0140-6736(88)91143-9. [DOI] [PubMed] [Google Scholar]
- O'Farrell N., Hoosen A. A., Coetzee K. D., van den Ende J. Genital ulcer disease in men in Durban, South Africa. Genitourin Med. 1991 Aug;67(4):327–330. doi: 10.1136/sti.67.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Farrell N., Hoosen A. A., Coetzee K. D., van den Ende J. Genital ulcer disease in women in Durban, South Africa. Genitourin Med. 1991 Aug;67(4):322–326. doi: 10.1136/sti.67.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Farrell N., Windsor I., Becker P. HIV-1 infection among heterosexual attenders at a sexually transmitted diseases clinic in Durban. S Afr Med J. 1991 Jul 6;80(1):17–20. [PubMed] [Google Scholar]
- O'Farrell N., Windsor I. Prevalence of HIV antibody in recurrent attenders at a sexually transmitted disease clinic. S Afr Med J. 1988 Aug 6;74(3):104–105. [PubMed] [Google Scholar]
- O'Farrell N., Windsor I. Sexual behavior in HIV-1-seropositive Zulu men and women in Durban, South Africa. J Acquir Immune Defic Syndr. 1991;4(12):1258–1259. [PubMed] [Google Scholar]
- Piot P., Laga M., Ryder R., Perriëns J., Temmerman M., Heyward W., Curran J. W. The global epidemiology of HIV infection: continuity, heterogeneity, and change. J Acquir Immune Defic Syndr. 1990;3(4):403–412. [PubMed] [Google Scholar]
- Plummer F. A., Simonsen J. N., Cameron D. W., Ndinya-Achola J. O., Kreiss J. K., Gakinya M. N., Waiyaki P., Cheang M., Piot P., Ronald A. R. Cofactors in male-female sexual transmission of human immunodeficiency virus type 1. J Infect Dis. 1991 Feb;163(2):233–239. doi: 10.1093/infdis/163.2.233. [DOI] [PubMed] [Google Scholar]
- Prual A., Chacko S., Koch-Weser D. Sexual behaviour, AIDS and poverty in Sub-Saharan Africa. Int J STD AIDS. 1991 Jan-Feb;2(1):1–9. doi: 10.1177/095646249100200101. [DOI] [PubMed] [Google Scholar]
- Van de Perre P., Le Polain B., Carael M., Nzaramba D., Zissis G., Butzler J. P. HIV antibodies in a remote rural area in Rwanda, Central Africa: an analysis of potential risk factors for HIV seropositivity. AIDS. 1987 Dec;1(4):213–215. [PubMed] [Google Scholar]


