Abstract
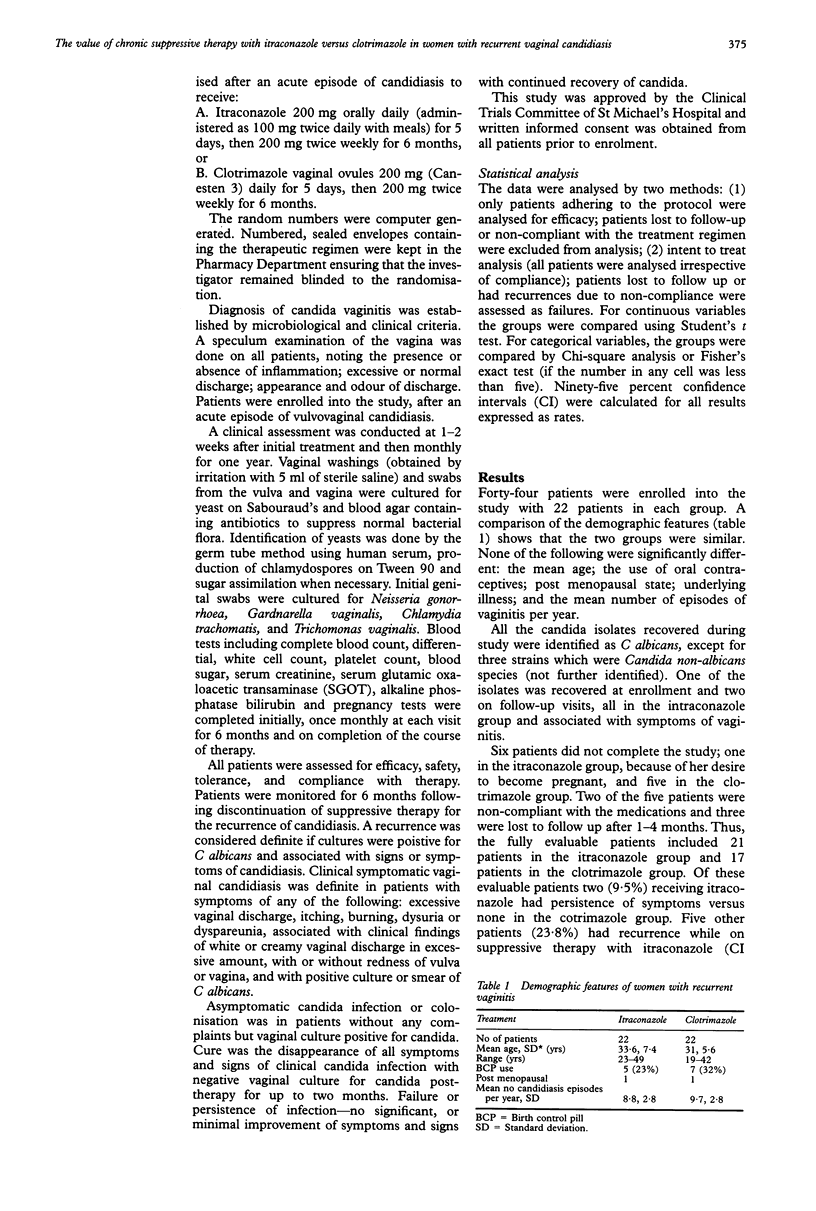
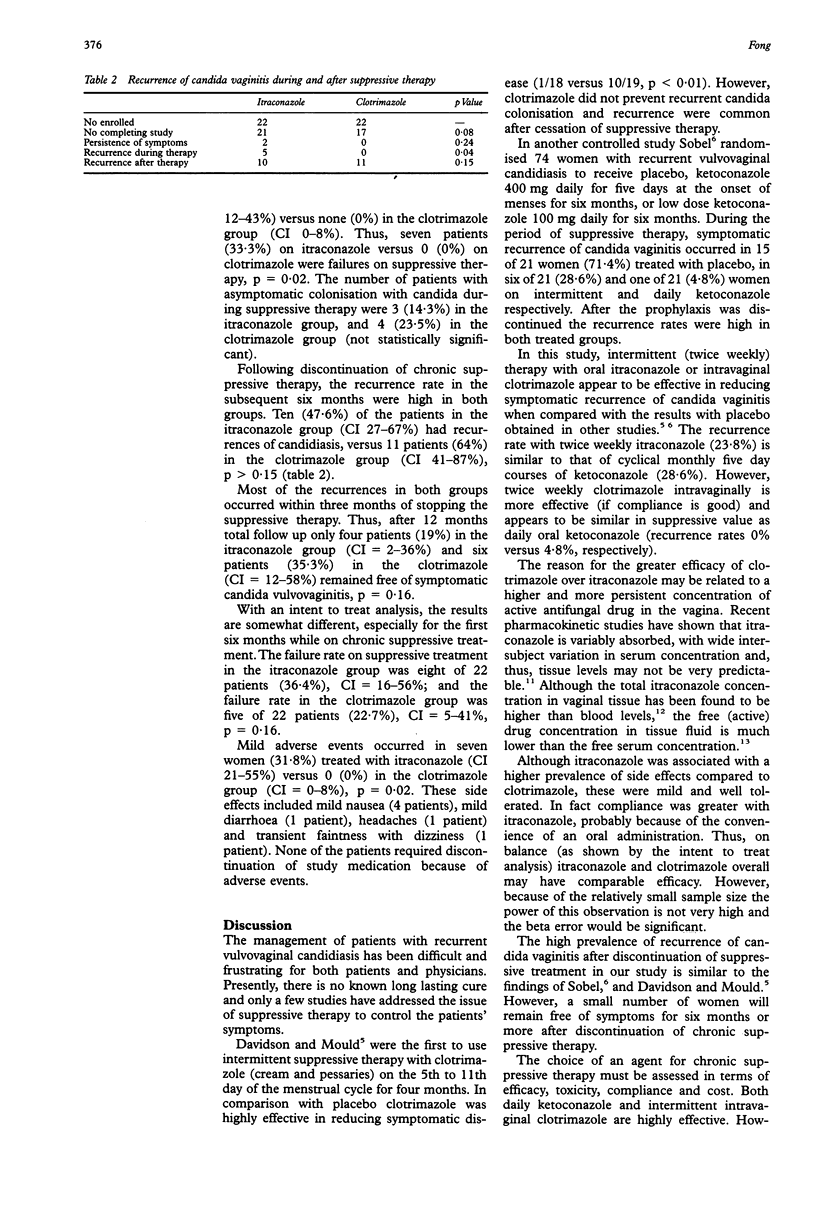
OBJECTIVE--To determine the comparative efficacy of oral itraconazole versus intravaginal clotrimazole in suppressing recurrent episodes of vulvovaginal candidiasis. DESIGN--Prospective randomised open study of women with recurrent vulvovaginal candidiasis. Clinical and microbiological assessments were made monthly for 12 months. SETTING--Women's Clinic of a University teaching hospital. SUBJECTS--Forty-four otherwise healthy, non-pregnant women, with at least four proven episodes of candida vaginitis in the last year were enrolled into the study. INTERVENTION--After an acute episode of candida vaginitis, 22 women received oral itraconazole 200 mg daily for five days, then 200 mg twice weekly for six months; and 22 women received intra-vaginal clotrimazole 200 mg ovules daily for five days, then 200 mg twice weekly for six months. MAIN OUTCOME MEASURES--Symptomatic recurrent clinical vulvovaginal candidiasis during the first six months of suppressive therapy was the major endpoint. A secondary endpoint was recurrent candida vaginitis within six months after completion of therapy. RESULTS--Six patients did not complete the study, one in the itraconazole group and five in the clotrimazole group. Of the evaluable patients, seven of 21 patients (33.3%) in the itraconazole group versus none (0%) of 17 patients on clotrimazole were failures on suppressive therapy, p = 0.02. Following discontinuation of suppressive therapy, recurrences of candida vaginitis were similar, 10 (47.6%) of patients on itraconazole (95% confidence interval (CI) 27-67%), versus 11 (64%) patients on clotrimazole (CI 41-87%), p = 0.15. CONCLUSION--Intermittent suppressive therapy with clotrimazole was more effective than itraconazole in preventing recurrent candida vaginitis, provided patients adhered to the regimen. Recurrence of vaginitis was common with both regimens after stopping suppressive therapy.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Davidson F., Mould R. F. Recurrent genital candidosis in women and the effect of intermittent prophylactic treatment. Br J Vener Dis. 1978 Jun;54(3):176–183. doi: 10.1136/sti.54.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardin T. C., Graybill J. R., Fetchick R., Woestenborghs R., Rinaldi M. G., Kuhn J. G. Pharmacokinetics of itraconazole following oral administration to normal volunteers. Antimicrob Agents Chemother. 1988 Sep;32(9):1310–1313. doi: 10.1128/aac.32.9.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz B. J., Edelstein S. W., Lippman L. Sexual transmission of Candida. Obstet Gynecol. 1987 Jun;69(6):883–886. [PubMed] [Google Scholar]
- Lewis J. H., Zimmerman H. J., Benson G. D., Ishak K. G. Hepatic injury associated with ketoconazole therapy. Analysis of 33 cases. Gastroenterology. 1984 Mar;86(3):503–513. [PubMed] [Google Scholar]
- Miles M. R., Olsen L., Rogers A. Recurrent vaginal candidiasis. Importance of an intestinal reservoir. JAMA. 1977 Oct 24;238(17):1836–1837. doi: 10.1001/jama.238.17.1836. [DOI] [PubMed] [Google Scholar]
- Schäfer-Korting M., Korting H. C., Lukacs A., Heykants J., Behrendt H. Levels of itraconazole in skin blister fluid after a single oral dose and during repetitive administration. J Am Acad Dermatol. 1990 Feb;22(2 Pt 1):211–215. doi: 10.1016/0190-9622(90)70026-e. [DOI] [PubMed] [Google Scholar]
- Silva Cruz A., Andrade L., Oliveira J. E., Sobral J. L. An open assessment of three different treatment regimens of itraconazole for the management of vaginal candidosis. Pharmatherapeutica. 1988;5(3):189–192. [PubMed] [Google Scholar]
- Sobel J. D. Recurrent vulvovaginal candidiasis. A prospective study of the efficacy of maintenance ketoconazole therapy. N Engl J Med. 1986 Dec 4;315(23):1455–1458. doi: 10.1056/NEJM198612043152305. [DOI] [PubMed] [Google Scholar]
- Sobel J. D. Vulvovaginal candidiasis--what we do and do not know. Ann Intern Med. 1984 Sep;101(3):390–392. doi: 10.7326/0003-4819-101-3-390. [DOI] [PubMed] [Google Scholar]
- Van Cutsem J., Van Gerven F., Janssen P. A. Activity of orally, topically, and parenterally administered itraconazole in the treatment of superficial and deep mycoses: animal models. Rev Infect Dis. 1987 Jan-Feb;9 (Suppl 1):S15–S32. doi: 10.1093/clinids/9.supplement_1.s15. [DOI] [PubMed] [Google Scholar]
- Witkin S. S., Yu I. R., Ledger W. J. Inhibition of Candida albicans--induced lymphocyte proliferation by lymphocytes and sera from women with recurrent vaginitis. Am J Obstet Gynecol. 1983 Dec 1;147(7):809–811. doi: 10.1016/0002-9378(83)90044-3. [DOI] [PubMed] [Google Scholar]


