Abstract
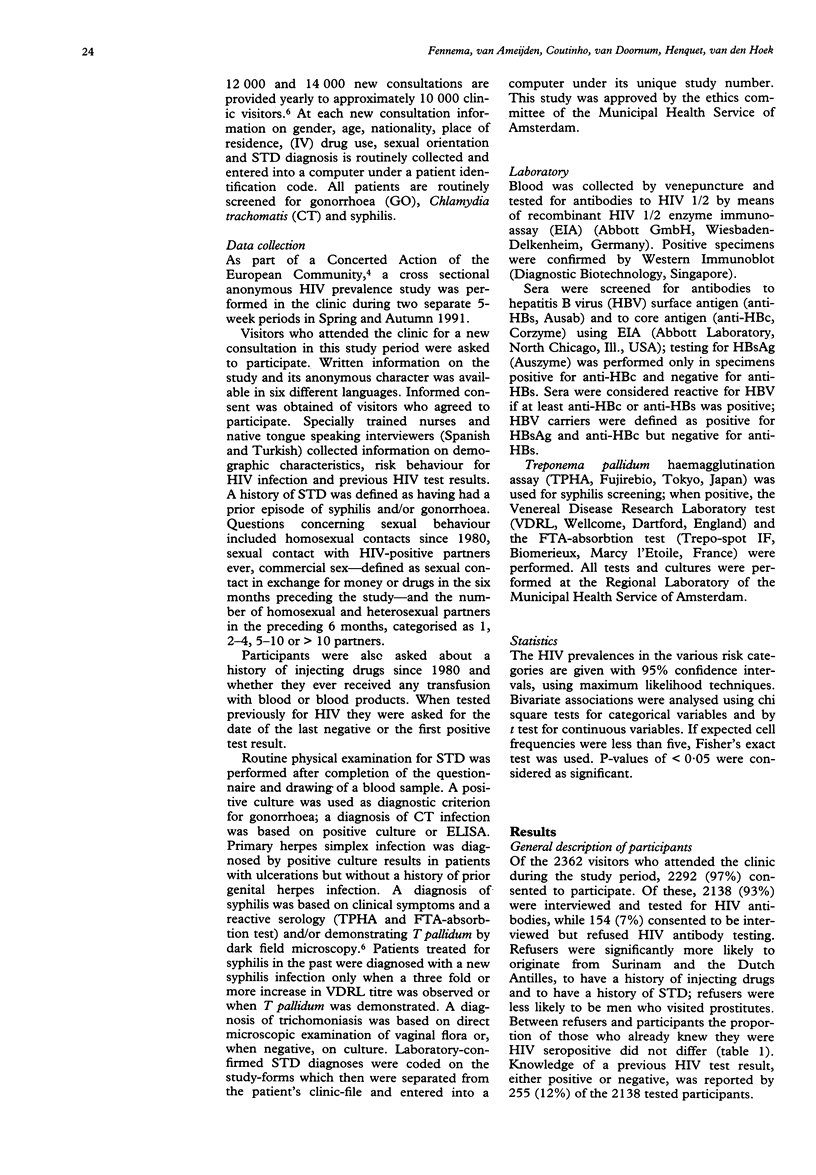
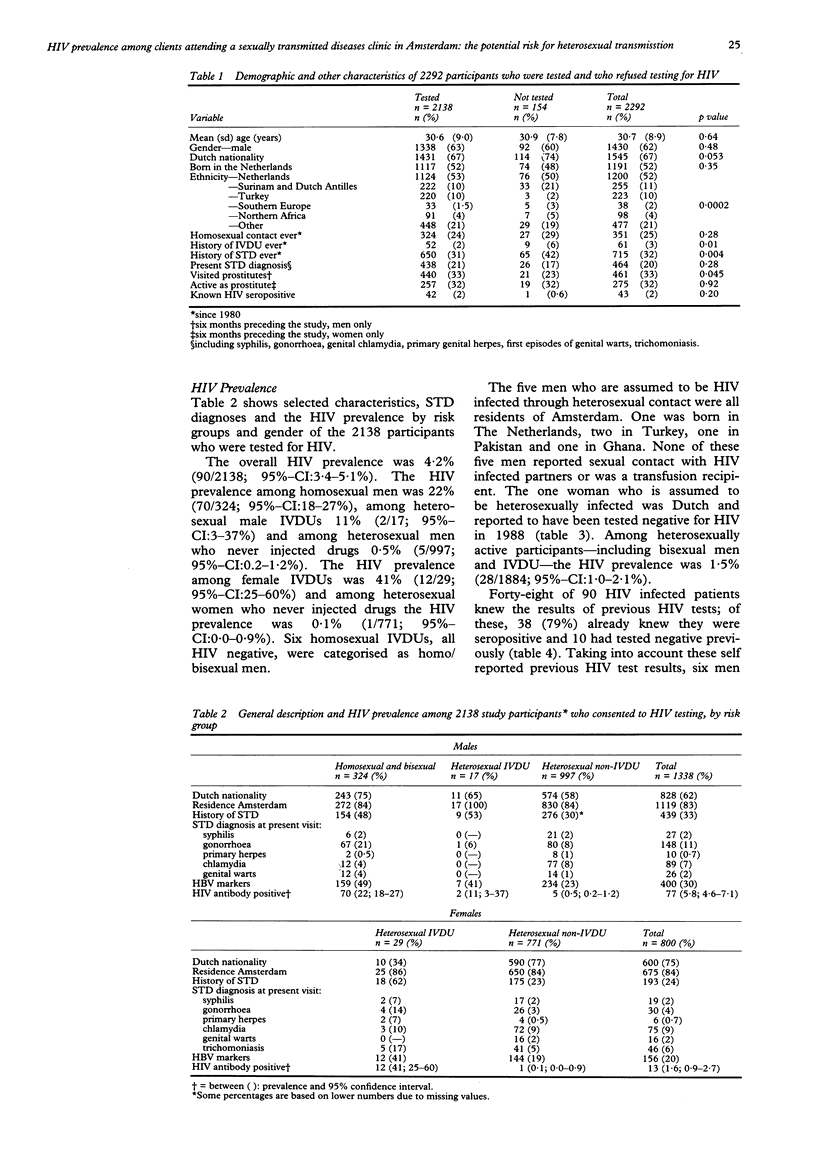
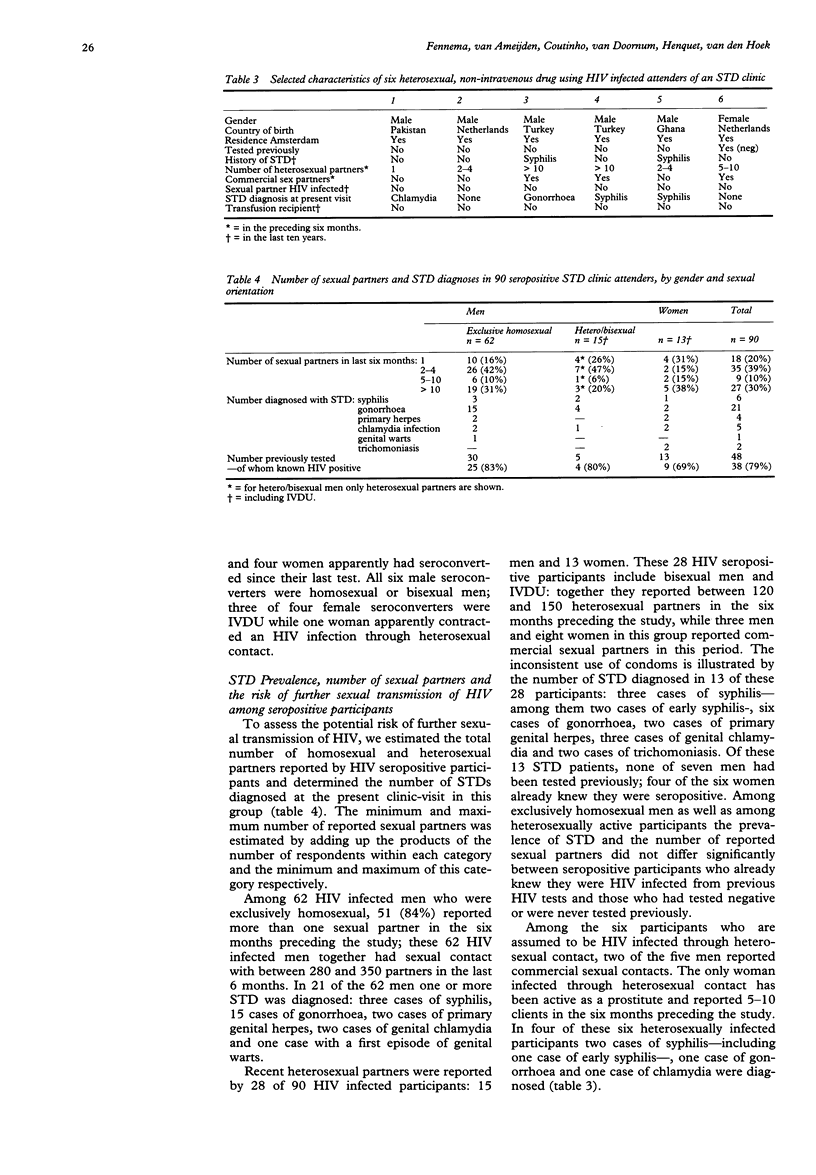
INTRODUCTION--Patients attending a clinic for sexually transmitted diseases (STD) in general have engaged in at risk sexual behaviour. Therefore they are at increased risk of acquiring HIV through sexual contact. OBJECTIVE--To determine the HIV prevalence among patients attending a STD clinic in Amsterdam. METHODS--An anonymous cross sectional study was conducted in two 5-week periods in Spring and Autumn 1991. RESULTS--Of the 2362 patients attending the clinic during the study period, 2292 (97%) consented to participate; of these, 2138 (93%) were interviewed and anonymously tested, while 154 (7%) consented to be interviewed but refused HIV antibody testing. The HIV prevalence was 4.2% (90/2138); 93% of seropositive participants reported homosexual contacts and/or intravenous use of drugs (IVDU). HIV prevalence among heterosexual non-IVDU men was 0.5% and among non-IVDU women 0.1%. Among all heterosexually active participants, including IVDU and bisexual men, the HIV prevalence was 1.5%. The 28 of 90 HIV infected participants that were heterosexually active reported together approximately 135 heterosexual partners in the six months preceding the study; 13 of these 28 heterosexually active participants had a STD diagnosed at their present clinic visit, while four (30%) of them already knew they were HIV infected. CONCLUSIONS--From these data we conclude that there is a substantial risk of further transmission of HIV through heterosexual contact. In order to try to reduce this potential for further sexual transmission of HIV, services offered by the STD clinic should not only include voluntary confidential counselling and HIV testing, but also notification of partners of HIV infected clinic-attendants. Finally, we conclude that anonymous HIV prevalence studies that link HIV test results to risk behaviour for HIV infection can be performed with a high rate of participation. Repeating such prevalence studies in time can help in monitoring the HIV incidence in the heterosexually active population.
Full text
PDF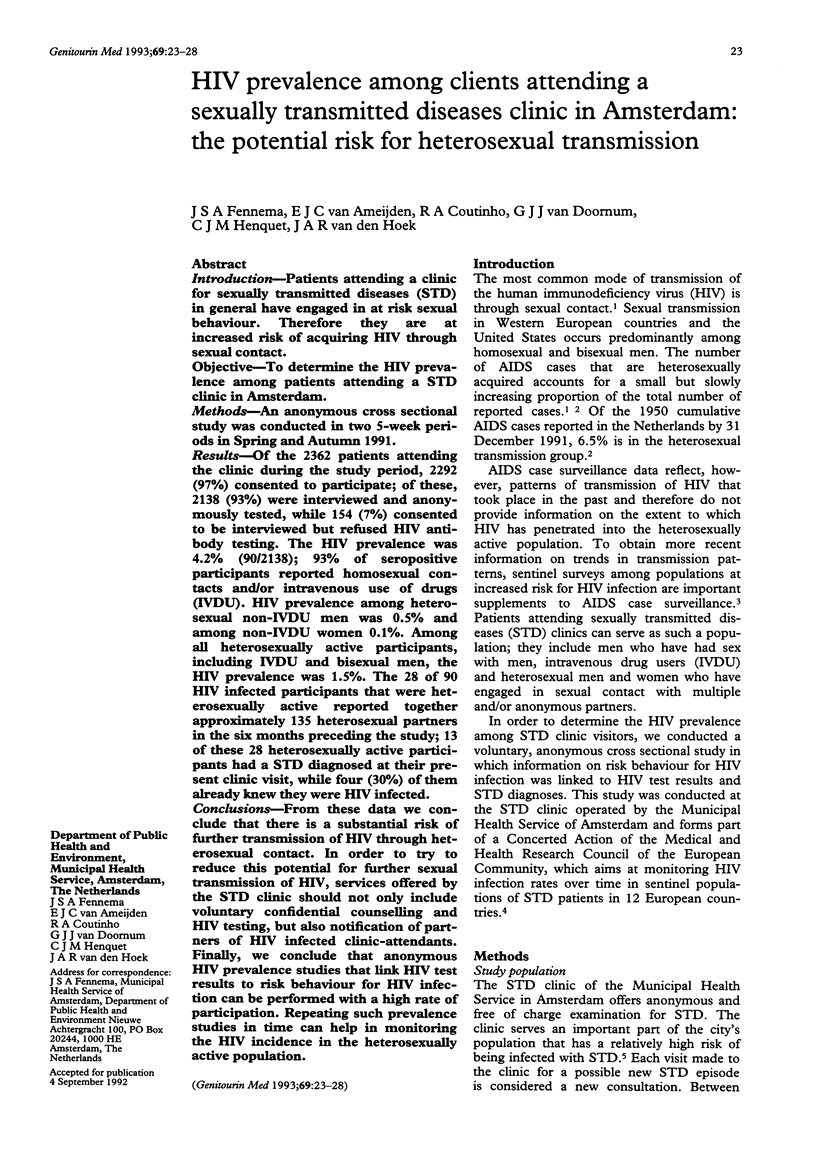
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Giesecke J., Ramstedt K., Granath F., Ripa T., Rådö G., Westrell M. Efficacy of partner notification for HIV infection. Lancet. 1991 Nov 2;338(8775):1096–1100. doi: 10.1016/0140-6736(91)91962-t. [DOI] [PubMed] [Google Scholar]
- Higgins D. L., Galavotti C., O'Reilly K. R., Schnell D. J., Moore M., Rugg D. L., Johnson R. Evidence for the effects of HIV antibody counseling and testing on risk behaviors. JAMA. 1991 Nov 6;266(17):2419–2429. [PubMed] [Google Scholar]
- Holmberg S. D., Stewart J. A., Gerber A. R., Byers R. H., Lee F. K., O'Malley P. M., Nahmias A. J. Prior herpes simplex virus type 2 infection as a risk factor for HIV infection. JAMA. 1988 Feb 19;259(7):1048–1050. [PubMed] [Google Scholar]
- Holmes K. K., Karon J. M., Kreiss J. The increasing frequency of heterosexually acquired AIDS in the United States, 1983-88. Am J Public Health. 1990 Jul;80(7):858–863. doi: 10.2105/ajph.80.7.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooykaas C., van der Velde F. W., van der Linden M. M., van Doornum G. J., Coutinho R. A. The importance of ethnicity as a risk factor for STDs and sexual behaviour among heterosexuals. Genitourin Med. 1991 Oct;67(5):378–383. doi: 10.1136/sti.67.5.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull H. F., Bettinger C. J., Gallaher M. M., Keller N. M., Wilson J., Mertz G. J. Comparison of HIV-antibody prevalence in patients consenting to and declining HIV-antibody testing in an STD clinic. JAMA. 1988 Aug 19;260(7):935–938. [PubMed] [Google Scholar]
- Landis S. E., Schoenbach V. J., Weber D. J., Mittal M., Krishan B., Lewis K., Koch G. G. Results of a randomized trial of partner notification in cases of HIV infection in North Carolina. N Engl J Med. 1992 Jan 9;326(2):101–106. doi: 10.1056/NEJM199201093260205. [DOI] [PubMed] [Google Scholar]
- Piot P., Laga M. Genital ulcers, other sexually transmitted diseases, and the sexual transmission of HIV. BMJ. 1989 Mar 11;298(6674):623–624. doi: 10.1136/bmj.298.6674.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F. A., Simonsen J. N., Cameron D. W., Ndinya-Achola J. O., Kreiss J. K., Gakinya M. N., Waiyaki P., Cheang M., Piot P., Ronald A. R. Cofactors in male-female sexual transmission of human immunodeficiency virus type 1. J Infect Dis. 1991 Feb;163(2):233–239. doi: 10.1093/infdis/163.2.233. [DOI] [PubMed] [Google Scholar]
- Simonsen J. N., Cameron D. W., Gakinya M. N., Ndinya-Achola J. O., D'Costa L. J., Karasira P., Cheang M., Ronald A. R., Piot P., Plummer F. A. Human immunodeficiency virus infection among men with sexually transmitted diseases. Experience from a center in Africa. N Engl J Med. 1988 Aug 4;319(5):274–278. doi: 10.1056/NEJM198808043190504. [DOI] [PubMed] [Google Scholar]
- Stamm W. E., Handsfield H. H., Rompalo A. M., Ashley R. L., Roberts P. L., Corey L. The association between genital ulcer disease and acquisition of HIV infection in homosexual men. JAMA. 1988 Sep 9;260(10):1429–1433. [PubMed] [Google Scholar]
- Wykoff R. F., Jones J. L., Longshore S. T., Hollis S. L., Quiller C. B., Dowda H., Gamble W. B. Notification of the sex and needle-sharing partners of individuals with human immunodeficiency virus in rural South Carolina: 30-month experience. Sex Transm Dis. 1991 Oct-Dec;18(4):217–222. doi: 10.1097/00007435-199110000-00004. [DOI] [PubMed] [Google Scholar]
- van Griensven G. J., de Vroome E. M., Tielman R. A., Goudsmit J., van der Noordaa J., de Wolf F., Coutinho R. A. Impact of HIV antibody testing on changes in sexual behavior among homosexual men in The Netherlands. Am J Public Health. 1988 Dec;78(12):1575–1577. doi: 10.2105/ajph.78.12.1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haastrecht H. J., van den Hoek J. A., Coutinho R. A. Evidence for a change in behaviour among heterosexuals in Amsterdam under the influence of AIDS. Genitourin Med. 1991 Jun;67(3):199–206. doi: 10.1136/sti.67.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Hoek A., van Haastrecht H. J., Coutinho R. A. Heterosexual behaviour of intravenous drug users in Amsterdam: implications for the AIDS epidemic. AIDS. 1990 May;4(5):449–453. doi: 10.1097/00002030-199005000-00011. [DOI] [PubMed] [Google Scholar]
- van den Hoek J. A., van Haastrecht H. J., Coutinho R. A. Little change in sexual behavior in injecting drug users in Amsterdam. J Acquir Immune Defic Syndr. 1992;5(5):518–522. [PubMed] [Google Scholar]


