Abstract
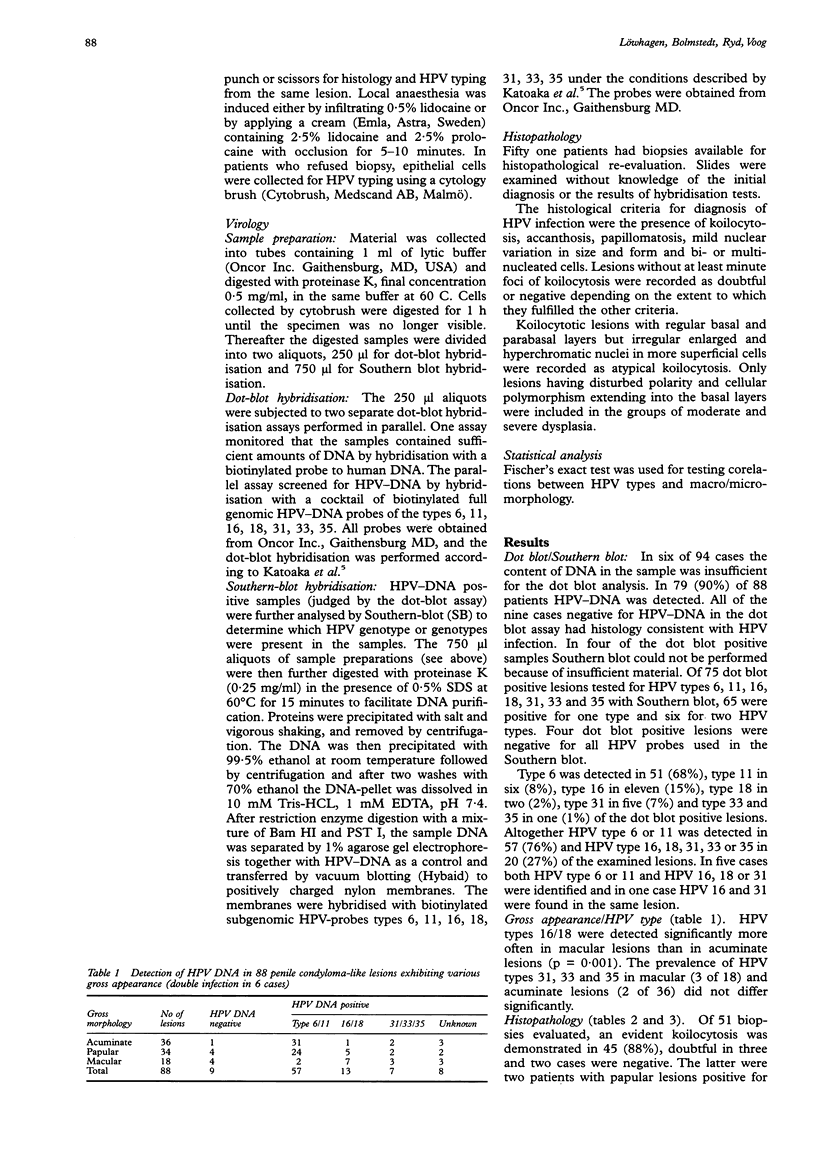
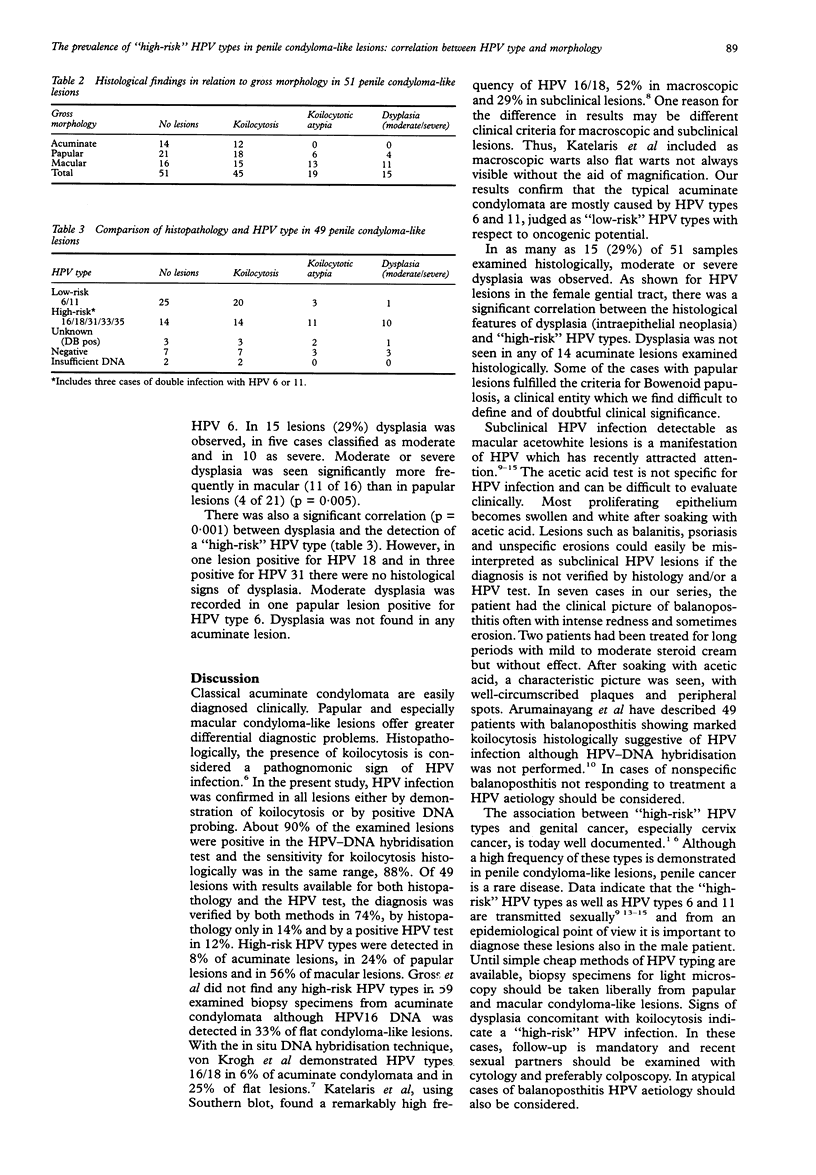
OBJECTIVE--To evaluate the prevalence of "high-risk" human papilloma virus (HPV) types in penile condyloma-like lesions and to correlate HPV types with clinical and histological features. DESIGN--The study included 94 male patients with signs of penile HPV infection. From acuminate, papular and macular lesions, specimens were collected for HPV DNA hybridisation, using the dot blot and Southern blot techniques. Biopsy specimens from 51 cases were examined by light microscopy for signs of koilocytosis and dysplasia. SETTING--The STD outpatient clinic of the Department of Dermatovenereology of Sahlgrenska Hospital, Göteborg, Sweden. RESULTS--In 79 (90%) of 88 patients HPV DNA was detected by dot blot. Of 51 cases examined by histology 88% disclosed an evident koilocytosis. "High-risk" HPV types (16, 18, 31, 33, 35) were demonstrated in 8% of acuminate, 24% of papular and 56% of macular lesions. In 29% of 51 lesions examined histologically moderate to severe dysplasia was observed. There was a significant correlation between "high-risk" HPV types and dysplasia. CONCLUSION--"High-risk" HPV types are prevalent in papular and especially macular penile condyloma-like lesions. The histological finding of koilocytosis concomitant with dysplasia strongly indicates infection with a "high-risk" HPV type. Although the risk of penile cancer is low, it is from an epidemiological point of view important to diagnose these lesions. Until simple tests for HPV typing are available, biopsy for light microscopy (histology) should be obtained liberally from papular and macular condyloma-like lesions. In atypical cases of balanoposthitis HPV aetiology should also be considered.
Full text
PDF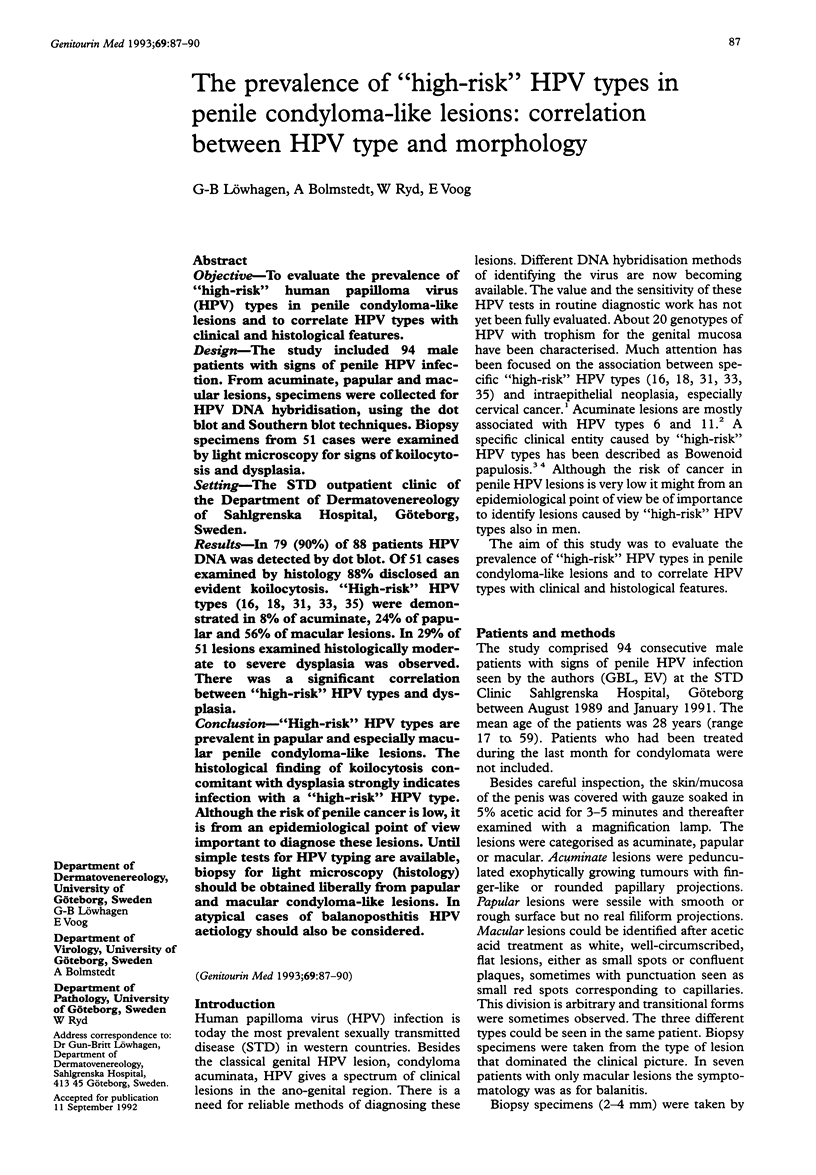
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arumainayagam J. T., Sumathipala A. H., Smallman L. A., Shahmanesh M. Flat condylomata of the penis presenting as patchy balanoposthitis. Genitourin Med. 1990 Aug;66(4):251–253. doi: 10.1136/sti.66.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion M. J., McCance D. J., Mitchell H. S., Jenkins D., Singer A., Oriel J. D. Subclinical penile human papillomavirus infection and dysplasia in consorts of women with cervical neoplasia. Genitourin Med. 1988 Apr;64(2):90–99. doi: 10.1136/sti.64.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow V. T., Tay S. K., Tham K. M., Lim-Tan S. K., Bernard H. U. Subclinical human papillomavirus infection of the male lower genital tract: colposcopy, histology and DNA analysis. Int J STD AIDS. 1991 Jan-Feb;2(1):41–45. doi: 10.1177/095646249100200108. [DOI] [PubMed] [Google Scholar]
- Gross G., Ikenberg H., Gissmann L., Hagedorn M. Papillomavirus infection of the anogenital region: correlation between histology, clinical picture, and virus type. Proposal of a new nomenclature. J Invest Dermatol. 1985 Aug;85(2):147–152. doi: 10.1111/1523-1747.ep12276576. [DOI] [PubMed] [Google Scholar]
- Kataoka A., Claesson U., Hansson B. G., Eriksson M., Lindh E. Human papillomavirus infection of the male diagnosed by Southern-blot hybridization and polymerase chain reaction: comparison between urethra samples and penile biopsy samples. J Med Virol. 1991 Mar;33(3):159–164. doi: 10.1002/jmv.1890330304. [DOI] [PubMed] [Google Scholar]
- Katelaris P. M., Cossart Y. E., Rose B. R., Thompson C. H., Sorich E., Nightingale B., Dallas P. B., Morris B. J. Human papillomavirus: the untreated male reservoir. J Urol. 1988 Aug;140(2):300–305. doi: 10.1016/s0022-5347(17)41588-6. [DOI] [PubMed] [Google Scholar]
- Law C., Merianos A., Thompson C., Rose B., Cossart Y., Grace J. Manifestations of anogenital HPV infection in the male partners of women with anogenital warts and/or abnormal cervical smears. Int J STD AIDS. 1991 May-Jun;2(3):188–194. doi: 10.1177/095646249100200308. [DOI] [PubMed] [Google Scholar]
- Sand Petersen C., Albrectsen J., Larsen J., Sindrup J., Tikjøb G., Ottevanger V., Karlsmark T., Fogh H., Mellon Mogensen A., Wolff-Sneedorff A. Subclinical human papilloma virus infection in condylomata acuminata patients attending a VD clinic. Acta Derm Venereol. 1991;71(3):252–255. [PubMed] [Google Scholar]
- Schneider A., Kirchmayr R., De Villiers E. M., Gissmann L. Subclinical human papillomavirus infections in male sexual partners of female carriers. J Urol. 1988 Dec;140(6):1431–1434. doi: 10.1016/s0022-5347(17)42065-9. [DOI] [PubMed] [Google Scholar]
- Schwartz R. A., Janniger C. K. Bowenoid papulosis. J Am Acad Dermatol. 1991 Feb;24(2 Pt 1):261–264. doi: 10.1016/0190-9622(91)70039-5. [DOI] [PubMed] [Google Scholar]
- Syrjänen K., Syrjänen S. Epidemiology of human papilloma virus infections and genital neoplasia. Scand J Infect Dis Suppl. 1990;69:7–17. [PubMed] [Google Scholar]
- Wade T. R., Kopf A. W., Ackerman A. B. Bowenoid papulosis of the penis. Cancer. 1978 Oct;42(4):1890–1903. doi: 10.1002/1097-0142(197810)42:4<1890::aid-cncr2820420430>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- von Krogh G., Syrjänen S. M., Syrjänen K. J. Advantage of human papillomavirus typing in the clinical evaluation of genitoanal warts. Experience with the in situ deoxyribonucleic acid hybridization technique applied on paraffin sections. J Am Acad Dermatol. 1988 Mar;18(3):495–503. doi: 10.1016/s0190-9622(88)70072-9. [DOI] [PubMed] [Google Scholar]



