Abstract
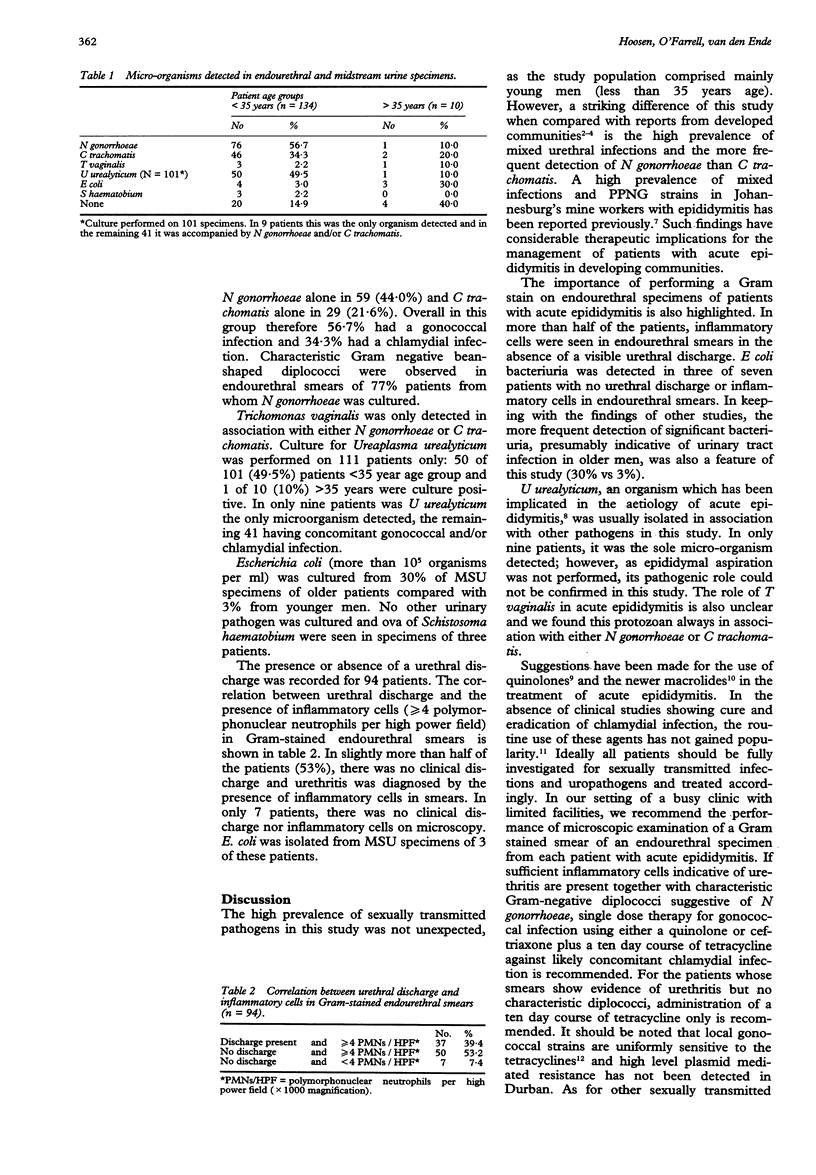
OBJECTIVE--To investigate the aetiology of acute epididymitis in a developing community with a view of determining appropriate antimicrobial therapy. SETTING--City Health Sexually Transmitted Diseases Clinic, King Edward VIII Hospital, Durban, South Africa. PARTICIPANTS--144 adult men with clinically diagnosed acute epididymitis. METHOD--Endourethral swab and midstream urine (MSU) specimens were processed to detect sexually transmitted pathogens and urinary tract infections. RESULTS--The majority of patients (93%) were less than 35 years of age. Neisseria gonorrhoeae and/or Chlamydia trachomatis were detected in 78% of patients: N gonorrhoeae in 57%, C trachomatis in 34% and both in 13%. Escherichia coli was cultured more frequently from MSU specimens of older patients, 30% versus 3%. In 53% of patients urethritis was diagnosed by the presence of inflammatory cells in endourethral smears in the absence of a visible urethral discharge. CONCLUSION--In our setting of a busy clinic with limited facilities, we recommend the performance of a Gram stain on endourethral specimens from patients with acute epididymitis. If inflammatory cells and Gram negative diplococci are detected, treatment with antimicrobial agents to cover both penicillinase-producing N gonorrhoeae strains and C trachomatis is recommended. If Gram negative diplococci are not detected in the presence of microscopic evidence of urethritis, treatment for chlamydial infection alone is recommended.
Full text
PDF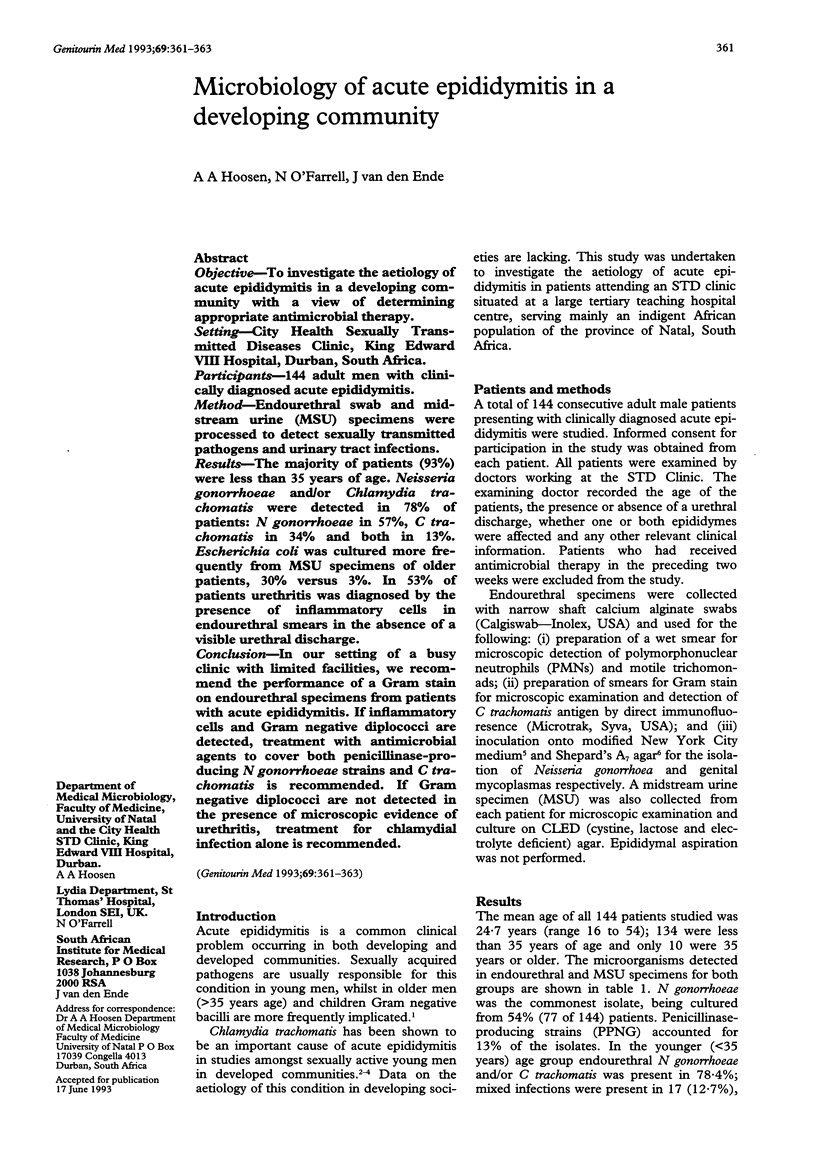

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coovadia Y. M., Van den Ende J., Hoosen A. A., Kharsany A. Susceptibility of penicillinase-producing and non-penicillinase-producing strains of Neisseria gonorrhoeae isolated in Durban, South Africa, to 15 beta-lactam antibiotics. Sex Transm Dis. 1988 Jan-Mar;15(1):30–34. doi: 10.1097/00007435-198801000-00007. [DOI] [PubMed] [Google Scholar]
- Costa P., Desclaux d'Arramon F., Gouby A., Navratil H., Geny F., Galtier M., Bressolle F. Disposition of roxithromycin in the epididymis after repeated oral administration. J Antimicrob Chemother. 1992 Aug;30(2):197–201. doi: 10.1093/jac/30.2.197. [DOI] [PubMed] [Google Scholar]
- Hawkins D. A., Taylor-Robinson D., Thomas B. J., Harris J. R. Microbiological survey of acute epididymitis. Genitourin Med. 1986 Oct;62(5):342–344. doi: 10.1136/sti.62.5.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalil N., Doble A., Gilchrist C., Taylor-Robinson D. Infection of the epididymis by Ureaplasma urealyticum. Genitourin Med. 1988 Dec;64(6):367–368. doi: 10.1136/sti.64.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulcahy F. M., Bignell C. J., Rajakumar R., Waugh M. A., Hetherington J. W., Ewing R., Whelan P. Prevalence of chlamydial infection in acute epididymo-orchitis. Genitourin Med. 1987 Feb;63(1):16–18. doi: 10.1136/sti.63.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard M. C., Lunceford C. D. Differential agar medium (A7) for identification of Ureaplasma urealyticum (human T mycoplasmas) in primary cultures of clinical material. J Clin Microbiol. 1976 Jun;3(6):613–625. doi: 10.1128/jcm.3.6.613-625.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young H. Cultural diagnosis of gonorrhoea with modified New York City (MNYC) medium. Br J Vener Dis. 1978 Feb;54(1):36–40. doi: 10.1136/sti.54.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]


