Abstract
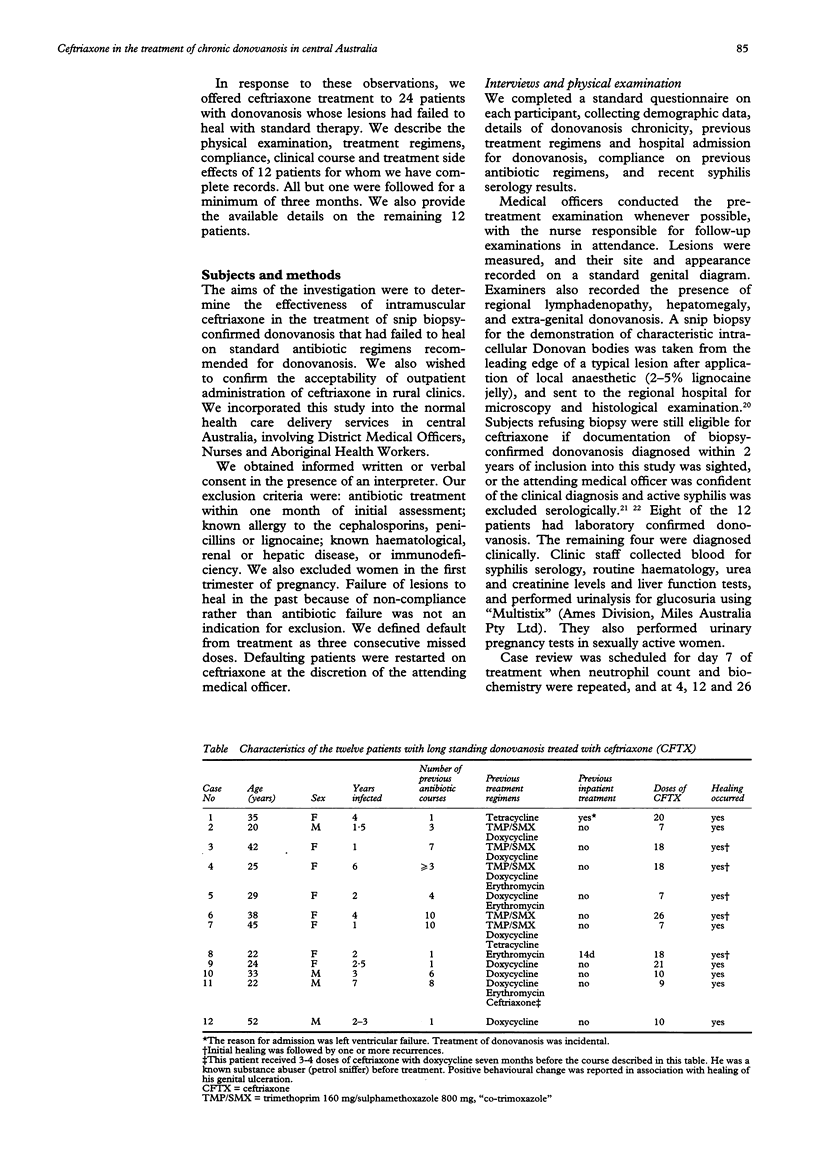
OBJECTIVES--To determine the effectiveness of intramuscular (IM) ceftriaxone sodium in the treatment of chronic donovanosis, and the acceptability to patients and staff of supervised outpatient treatment in rural clinics. METHODS--We collected demographic and sexual health data from participants using a standard questionnaire, and recorded their donovanosis lesions at baseline using genital diagrams. Treatment consisted of a single daily IM injection of 1 g ceftriaxone diluted in 2 ml of 1% lignocaine. Clinic staff followed patients for between three and 12 months, enabling the detection of late recurrences. SETTING--Rural Aboriginal communities in central Australia. PARTICIPANTS--The study describes eight women and four men with chronic donovanosis in detail, and summarises the outcome in 12 additional cases. All cases presented with advanced lesions which had failed to heal on the standard oral antibiotic regimens used in the region. RESULTS--The mean duration of infection was 3.0 years (SD 1.9 years), and between four and ten courses of antibiotics had been prescribed for six of the 12 patients. Patients received between 7-26g of ceftriaxone sodium. Clinical improvement was dramatic in most lesions, and four patients healed completely without recurrence after a total 7-10g of ceftriaxone. Mild recurrences responded to further ceftriaxone or short courses of oral antibiotics. Treatment was well tolerated, and both patient and staff compliance high. CONCLUSION--Donovanosis is an important cause of chronic genital ulceration in central Australia, and is potentially an important risk factor for HIV transmission in Aboriginal communities. The pharmacokinetics and safety profile of ceftriaxone make it a useful and cost-effective agent in the ambulatory management of donovanosis, especially in remote communities. Supervised multidrug regimens of two or more long-acting agents may provide the best answer in donovanosis, administered through the existing health care infrastructure.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashdown L. R., Kilvert G. T. Granuloma inguinale in Northern Queensland. Med J Aust. 1979 Mar 10;1(5):146–148. doi: 10.5694/j.1326-5377.1979.tb128949.x. [DOI] [PubMed] [Google Scholar]
- Bradley J. S., Compogiannis L. S., Murray W. E., Acosta M. A., Tsu G. L. Pharmacokinetics and safety of intramuscular injection of concentrated certriaxone in children. Clin Pharm. 1992 Nov;11(11):961–964. [PubMed] [Google Scholar]
- Brogden R. N., Ward A. Ceftriaxone. A reappraisal of its antibacterial activity and pharmacokinetic properties, and an update on its therapeutic use with particular reference to once-daily administration. Drugs. 1988 Jun;35(6):604–645. doi: 10.2165/00003495-198835060-00002. [DOI] [PubMed] [Google Scholar]
- Cameron D. W., Simonsen J. N., D'Costa L. J., Ronald A. R., Maitha G. M., Gakinya M. N., Cheang M., Ndinya-Achola J. O., Piot P., Brunham R. C. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet. 1989 Aug 19;2(8660):403–407. doi: 10.1016/s0140-6736(89)90589-8. [DOI] [PubMed] [Google Scholar]
- Cavenee M. R., Farris J. R., Spalding T. R., Barnes D. L., Castaneda Y. S., Wendel G. D., Jr Treatment of gonorrhea in pregnancy. Obstet Gynecol. 1993 Jan;81(1):33–38. [PubMed] [Google Scholar]
- Coovadia Y. M., Steinberg J. L., Kharsany A. Granuloma inguinale (donovanosis) of the oral cavity. A case report. S Afr Med J. 1985 Nov 23;68(11):815–817. [PubMed] [Google Scholar]
- Francke E. L., Neu H. C. Chloramphenicol and tetracyclines. Med Clin North Am. 1987 Nov;71(6):1155–1168. doi: 10.1016/s0025-7125(16)30803-3. [DOI] [PubMed] [Google Scholar]
- GHOSH S., GHOSH R. Donovanosis treated with erythromycin parenterally. Report of first case. Br J Vener Dis. 1959 Dec;35:260–261. doi: 10.1136/sti.35.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg B. R., Lal S., Sivamani S. Efficacy of co-trimoxazole in Donovanosis. A preliminary report. Br J Vener Dis. 1978 Oct;54(5):348–349. doi: 10.1136/sti.54.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hook E. W., 3rd, Roddy R. E., Handsfield H. H. Ceftriaxone therapy for incubating and early syphilis. J Infect Dis. 1988 Oct;158(4):881–884. doi: 10.1093/infdis/158.4.881. [DOI] [PubMed] [Google Scholar]
- Kafetzis D. A., Brater D. C., Fanourgakis J. E., Voyatzis J., Georgakopoulos P. Ceftriaxone distribution between maternal blood and fetal blood and tissues at parturition and between blood and milk postpartum. Antimicrob Agents Chemother. 1983 Jun;23(6):870–873. doi: 10.1128/aac.23.6.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreiss J. K., Coombs R., Plummer F., Holmes K. K., Nikora B., Cameron W., Ngugi E., Ndinya Achola J. O., Corey L. Isolation of human immunodeficiency virus from genital ulcers in Nairobi prostitutes. J Infect Dis. 1989 Sep;160(3):380–384. doi: 10.1093/infdis/160.3.380. [DOI] [PubMed] [Google Scholar]
- Kuberski T. Granuloma inguinale (donovanosis). Sex Transm Dis. 1980 Jan-Mar;7(1):29–36. doi: 10.1097/00007435-198001000-00009. [DOI] [PubMed] [Google Scholar]
- Latif A. S., Mason P. R., Paraiwa E. The treatment of donovanosis (granuloma inguinale). Sex Transm Dis. 1988 Jan-Mar;15(1):27–29. doi: 10.1097/00007435-198801000-00006. [DOI] [PubMed] [Google Scholar]
- Le Saux N., Ronald A. R. Role of ceftriaxone in sexually transmitted diseases. Rev Infect Dis. 1989 Mar-Apr;11(2):299–309. doi: 10.1093/clinids/11.2.299. [DOI] [PubMed] [Google Scholar]
- Mertens T. E., Hayes R. J., Smith P. G. Epidemiological methods to study the interaction between HIV infection and other sexually transmitted diseases. AIDS. 1990 Jan;4(1):57–65. doi: 10.1097/00002030-199001000-00008. [DOI] [PubMed] [Google Scholar]
- O'Farrell N. Failure of single dose ceftriaxone in donovanosis (granuloma inguinale) Genitourin Med. 1991 Jun;67(3):269–270. doi: 10.1136/sti.67.3.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Farrell N. Failure of single dose spectinomycin in granuloma inguinale (donovanosis). Trans R Soc Trop Med Hyg. 1990 Nov-Dec;84(6):862–862. doi: 10.1016/0035-9203(90)90109-r. [DOI] [PubMed] [Google Scholar]
- O'Farrell N. HIV, genital ulceration, and granuloma inguinale. Br Med J (Clin Res Ed) 1988 Mar 26;296(6626):935–935. doi: 10.1136/bmj.296.6626.935-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piot P., Laga M., Ryder R., Perriëns J., Temmerman M., Heyward W., Curran J. W. The global epidemiology of HIV infection: continuity, heterogeneity, and change. J Acquir Immune Defic Syndr. 1990;3(4):403–412. [PubMed] [Google Scholar]
- Plummer F. A., Simonsen J. N., Cameron D. W., Ndinya-Achola J. O., Kreiss J. K., Gakinya M. N., Waiyaki P., Cheang M., Piot P., Ronald A. R. Cofactors in male-female sexual transmission of human immunodeficiency virus type 1. J Infect Dis. 1991 Feb;163(2):233–239. doi: 10.1093/infdis/163.2.233. [DOI] [PubMed] [Google Scholar]
- Plummer F. A., Wainberg M. A., Plourde P., Jessamine P., D'Costa L. J., Wamola I. A., Ronald A. R. Detection of human immunodeficiency virus type 1 (HIV-1) in genital ulcer exudate of HIV-1-infected men by culture and gene amplification. J Infect Dis. 1990 Apr;161(4):810–811. doi: 10.1093/infdis/161.4.810. [DOI] [PubMed] [Google Scholar]
- ROBINSON R. C. V., WELLS T. L. Intramuscular chloramphenicol in the treatment of gonorrhea and granuloma inguinale. Am J Syph Gonorrhea Vener Dis. 1952 May;36(3):264–268. [PubMed] [Google Scholar]
- Ramanan C., Sarma P. S., Ghorpade A., Das M. Treatment of donovanosis with norfloxacin. Int J Dermatol. 1990 May;29(4):298–299. doi: 10.1111/j.1365-4362.1990.tb02568.x. [DOI] [PubMed] [Google Scholar]
- Richens J. The diagnosis and treatment of donovanosis (granuloma inguinale). Genitourin Med. 1991 Dec;67(6):441–452. doi: 10.1136/sti.67.6.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richens J. The diagnosis and treatment of donovanosis (granuloma inguinale). Genitourin Med. 1991 Dec;67(6):441–452. doi: 10.1136/sti.67.6.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sackett D. L., Holland W. W. Controversy in the detection of disease. Lancet. 1975 Aug 23;2(7930):357–359. doi: 10.1016/s0140-6736(75)92790-7. [DOI] [PubMed] [Google Scholar]
- Schöfer H., Vogt H. J., Milbradt R. Ceftriaxone for the treatment of primary and secondary syphilis. Chemotherapy. 1989;35(2):140–145. doi: 10.1159/000238661. [DOI] [PubMed] [Google Scholar]
- Scully B. E., Fu K. P., Neu H. C. Pharmacokinetics of ceftriaxone after intravenous infusion and intramuscular injection. Am J Med. 1984 Oct 19;77(4C):112–116. [PubMed] [Google Scholar]
- Sehgal V. N., Prasad A. L. Donovanosis. Current concepts. Int J Dermatol. 1986 Jan-Feb;25(1):8–16. doi: 10.1111/j.1365-4362.1986.tb03396.x. [DOI] [PubMed] [Google Scholar]
- Sengupta S. K., Das N. Donovanosis affecting cervix, uterus, and adnexae. Am J Trop Med Hyg. 1984 Jul;33(4):632–636. doi: 10.4269/ajtmh.1984.33.632. [DOI] [PubMed] [Google Scholar]


