Abstract
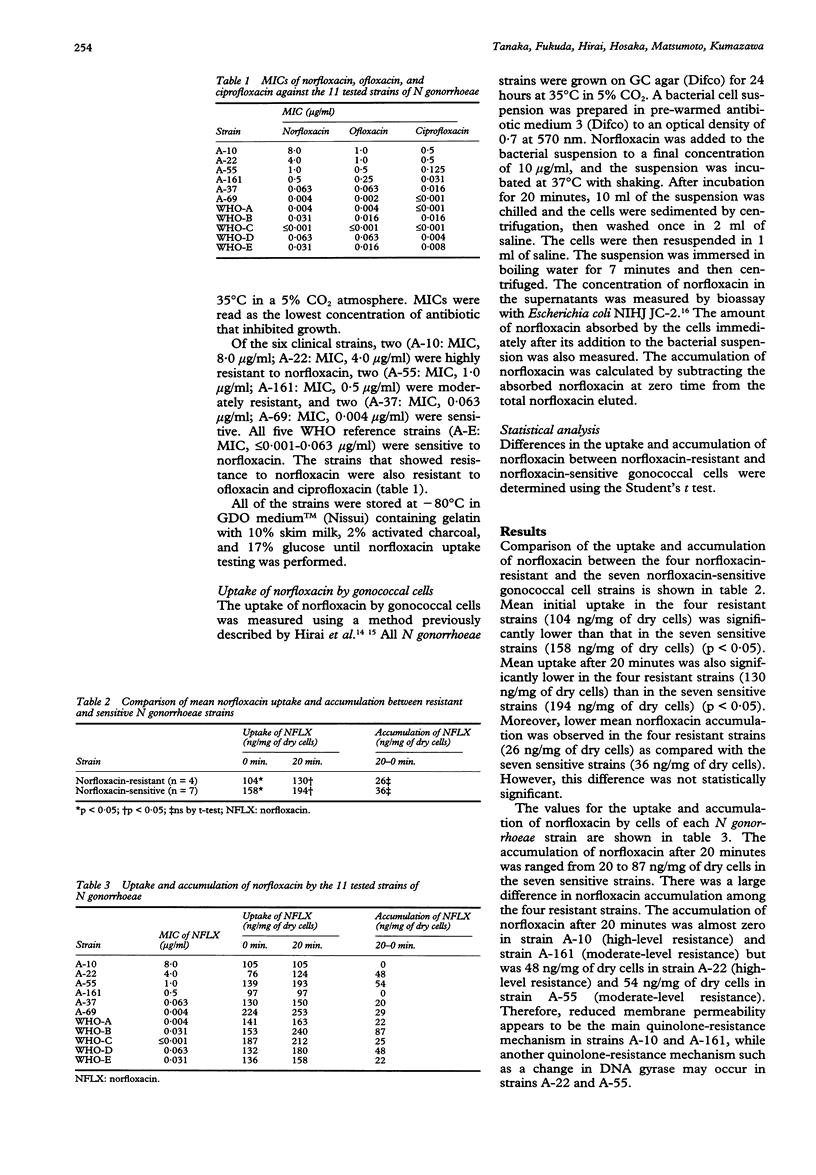
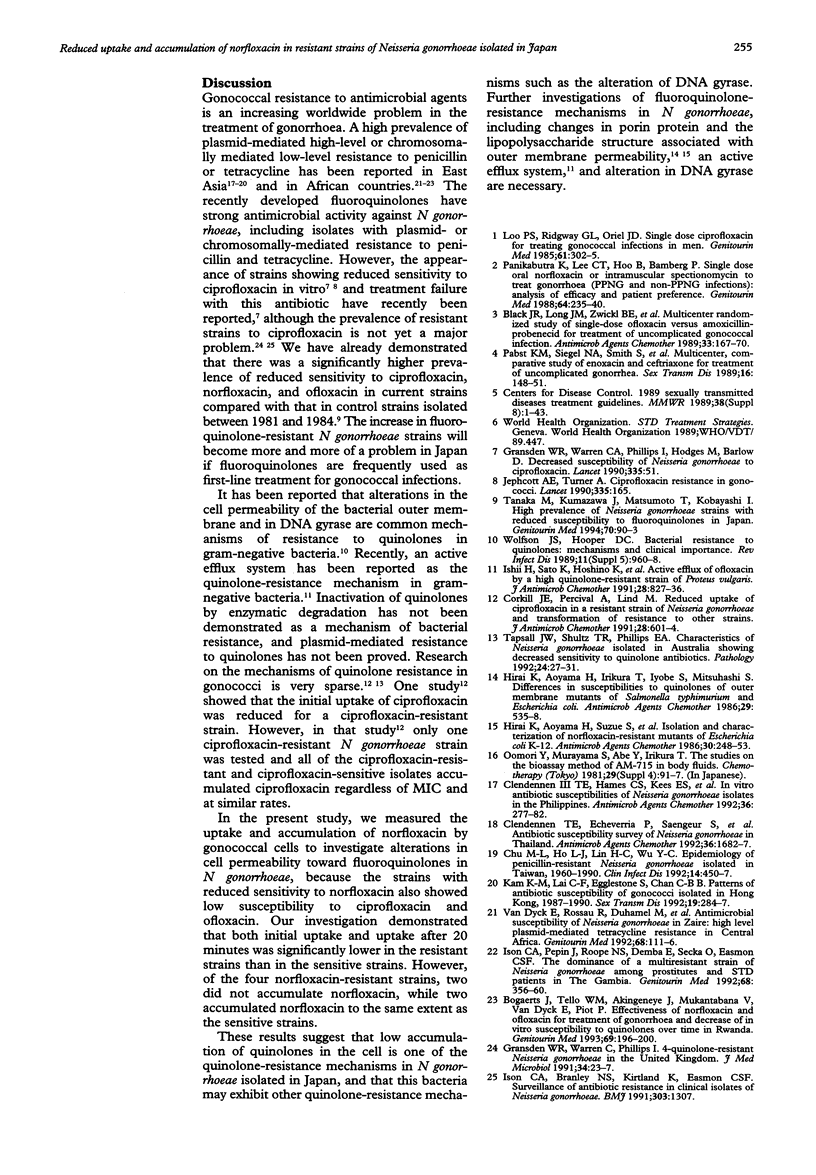
OBJECTIVE--To investigate the alteration of cell permeability toward fluoroquinolones in Neisseria gonorrhoeae, which is a major quinolone-resistance mechanism along with the alteration of DNA gyrase in gram-negative bacteria. The prevalence of fluoroquinolone-resistant N gonorrhoeae strains is rapidly increasing in Japan. MATERIALS AND METHODS--The uptake and accumulation of norfloxacin by gonococcal cells, including six clinical and five World Health Organization (WHO) reference strains, were measured. Of the six clinical strains, two were highly resistant to norfloxacin (MIC 8.0 and 4.0 micrograms/ml), two were moderately resistant (MIC 1.0 and 0.5 microgram/ml), and two were sensitive (MIC 0.063 and 0.004 microgram/ml). All five WHO reference strains were sensitive to norfloxacin (MIC < or = 0.001 to 0.063 microgram/ml). RESULTS--Mean initial norfloxacin uptake in the four resistant strains (104 ng/mg of dry cells) was significantly lower than that in the seven sensitive strains (158 ng/mg of dry cells) (p < 0.05). The mean uptake after 20 minutes was also significantly lower in the four resistant strains (130 ng/mg of dry cells) than in the seven sensitive strains (194 ng/mg of dry cells) (p < 0.05). However, there was no significant difference in mean norfloxacin accumulation after 20 minutes between the four resistant strains (26 ng/mg of dry cells) and the seven sensitive strains (36 ng/mg of dry cells). The accumulation of norfloxacin after 20 minutes was almost zero in two of the four resistant strains, while the remaining two strains accumulated norfloxacin as well as the sensitive strains. CONCLUSIONS--These findings suggest that alteration of bacterial cell permeability is a quinolone-resistance mechanism in N gonorrhoeae isolated in Japan, and that this bacteria may exhibit other mechanisms such as alteration of DNA gyrase.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Black J. R., Long J. M., Zwickl B. E., Ray B. S., Verdon M. S., Wetherby S., Hook E. W., 3rd, Handsfield H. H. Multicenter randomized study of single-dose ofloxacin versus amoxicillin-probenecid for treatment of uncomplicated gonococcal infection. Antimicrob Agents Chemother. 1989 Feb;33(2):167–170. doi: 10.1128/aac.33.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts J., Tello W. M., Akingeneye J., Mukantabana V., Van Dyck E., Piot P. Effectiveness of norfloxacin and ofloxacin for treatment of gonorrhoea and decrease of in vitro susceptibility to quinolones over time in Rwanda. Genitourin Med. 1993 Jun;69(3):196–200. doi: 10.1136/sti.69.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu M. L., Ho L. J., Lin H. C., Wu Y. C. Epidemiology of penicillin-resistant Neisseria gonorrhoeae isolated in Taiwan, 1960-1990. Clin Infect Dis. 1992 Feb;14(2):450–457. doi: 10.1093/clinids/14.2.450. [DOI] [PubMed] [Google Scholar]
- Clendennen T. E., 3rd, Hames C. S., Kees E. S., Price F. C., Rueppel W. J., Andrada A. B., Espinosa G. E., Kabrerra G., Wignall F. S. In vitro antibiotic susceptibilities of Neisseria gonorrhoeae isolates in the Philippines. Antimicrob Agents Chemother. 1992 Feb;36(2):277–282. doi: 10.1128/aac.36.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clendennen T. E., Echeverria P., Saengeur S., Kees E. S., Boslego J. W., Wignall F. S. Antibiotic susceptibility survey of Neisseria gonorrhoeae in Thailand. Antimicrob Agents Chemother. 1992 Aug;36(8):1682–1687. doi: 10.1128/aac.36.8.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corkill J. E., Percival A., Lind M. Reduced uptake of ciprofloxacin in a resistant strain of Neisseria gonorrhoeae and transformation of resistance to other strains. J Antimicrob Chemother. 1991 Oct;28(4):601–604. doi: 10.1093/jac/28.4.601. [DOI] [PubMed] [Google Scholar]
- Gransden W. R., Warren C. A., Phillips I., Hodges M., Barlow D. Decreased susceptibility of Neisseria gonorrhoeae to ciprofloxacin. Lancet. 1990 Jan 6;335(8680):51–51. doi: 10.1016/0140-6736(90)90177-7. [DOI] [PubMed] [Google Scholar]
- Hirai K., Aoyama H., Irikura T., Iyobe S., Mitsuhashi S. Differences in susceptibility to quinolones of outer membrane mutants of Salmonella typhimurium and Escherichia coli. Antimicrob Agents Chemother. 1986 Mar;29(3):535–538. doi: 10.1128/aac.29.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirai K., Aoyama H., Suzue S., Irikura T., Iyobe S., Mitsuhashi S. Isolation and characterization of norfloxacin-resistant mutants of Escherichia coli K-12. Antimicrob Agents Chemother. 1986 Aug;30(2):248–253. doi: 10.1128/aac.30.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishii H., Sato K., Hoshino K., Sato M., Yamaguchi A., Sawai T., Osada Y. Active efflux of ofloxacin by a highly quinolone-resistant strain of Proteus vulgaris. J Antimicrob Chemother. 1991 Dec;28(6):827–836. doi: 10.1093/jac/28.6.827. [DOI] [PubMed] [Google Scholar]
- Ison C. A., Branley N. S., Kirtland K., Easmon C. S. Surveillance of antibiotic resistance in clinical isolates of Neisseria gonorrhoeae. BMJ. 1991 Nov 23;303(6813):1307–1307. doi: 10.1136/bmj.303.6813.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ison C. A., Pepin J., Roope N. S., Demba E., Secka O., Easmon C. S. The dominance of a multiresistant strain of Neisseria gonorrhoeae among prostitutes and STD patients in The Gambia. Genitourin Med. 1992 Dec;68(6):356–360. doi: 10.1136/sti.68.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jephcott A. E., Turner A. Ciprofloxacin resistance in gonococci. Lancet. 1990 Jan 20;335(8682):165–165. doi: 10.1016/0140-6736(90)90035-4. [DOI] [PubMed] [Google Scholar]
- Kam K. M., Lai C. F., Egglestone S., Chan C. B. Patterns of antibiotic susceptibility of gonococci isolated in Hong Kong, 1987-1990. Sex Transm Dis. 1992 Sep-Oct;19(5):284–287. doi: 10.1097/00007435-199209000-00008. [DOI] [PubMed] [Google Scholar]
- Loo P. S., Ridgway G. L., Oriel J. D. Single dose ciprofloxacin for treating gonococcal infections in men. Genitourin Med. 1985 Oct;61(5):302–305. doi: 10.1136/sti.61.5.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabst K. M., Siegel N. A., Smith S., Black J. R., Handsfield H. H., Hook E. W., 3rd Multicenter, comparative study of enoxacin and ceftriaxone for treatment of uncomplicated gonorrhea. Sex Transm Dis. 1989 Jul-Sep;16(3):148–151. doi: 10.1097/00007435-198907000-00006. [DOI] [PubMed] [Google Scholar]
- Panikabutra K., Lee C. T., Ho B., Bamberg P. Single dose oral norfloxacin or intramuscular spectinomycin to treat gonorrhoea (PPNG and non-PPNG infections): analysis of efficacy and patient preference. Genitourin Med. 1988 Aug;64(4):235–240. doi: 10.1136/sti.64.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M., Kumazawa J., Matsumoto T., Kobayashi I. High prevalence of Neisseria gonorrhoeae strains with reduced susceptibility to fluoroquinolones in Japan. Genitourin Med. 1994 Apr;70(2):90–93. doi: 10.1136/sti.70.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapsall J. W., Shultz T. R., Phillips E. A. Characteristics of Neisseria gonorrhoeae isolated in Australia showing decreased sensitivity to quinolone antibiotics. Pathology. 1992 Jan;24(1):27–31. doi: 10.3109/00313029209063616. [DOI] [PubMed] [Google Scholar]
- Van Dyck E., Rossau R., Duhamel M., Behets F., Laga M., Nzila M., Bygdeman S., Van Heuverswijn H., Piot P. Antimicrobial susceptibility of Neisseria gonorrhoeae in Zaire: high level plasmid-mediated tetracycline resistance in central Africa. Genitourin Med. 1992 Apr;68(2):111–116. doi: 10.1136/sti.68.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]


