Abstract
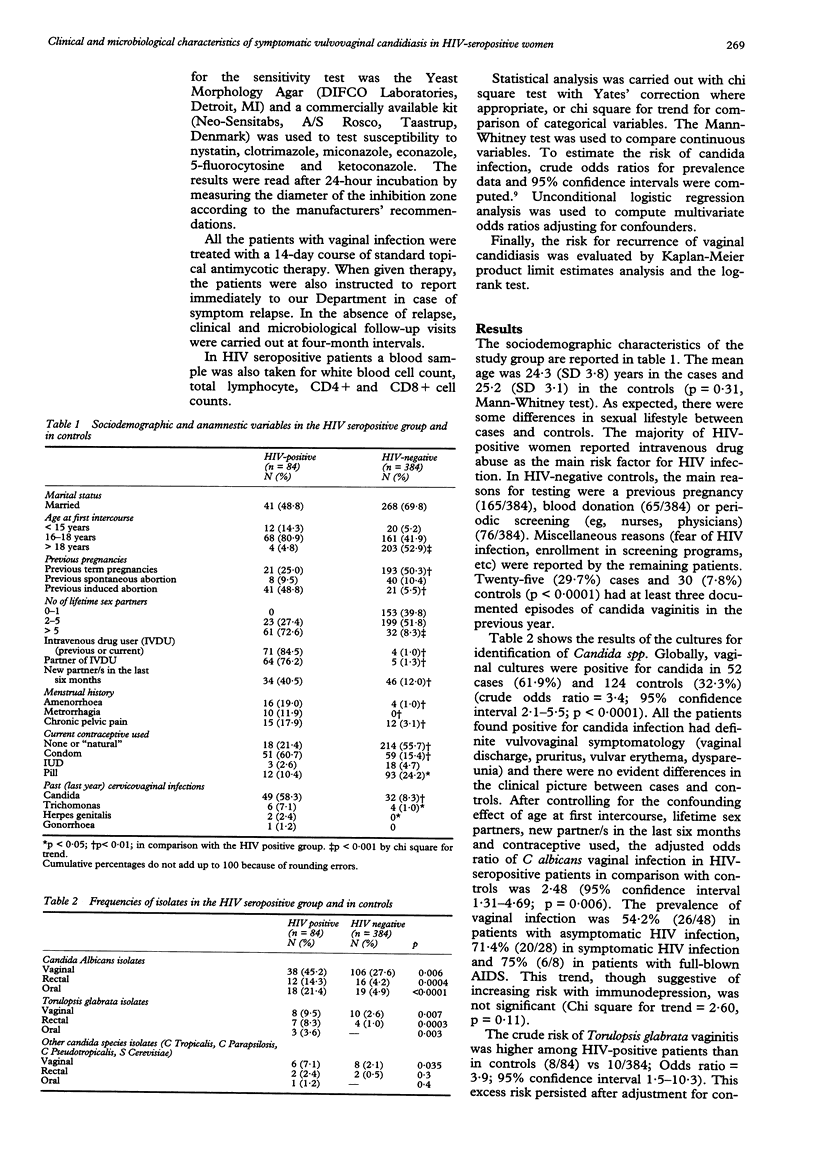
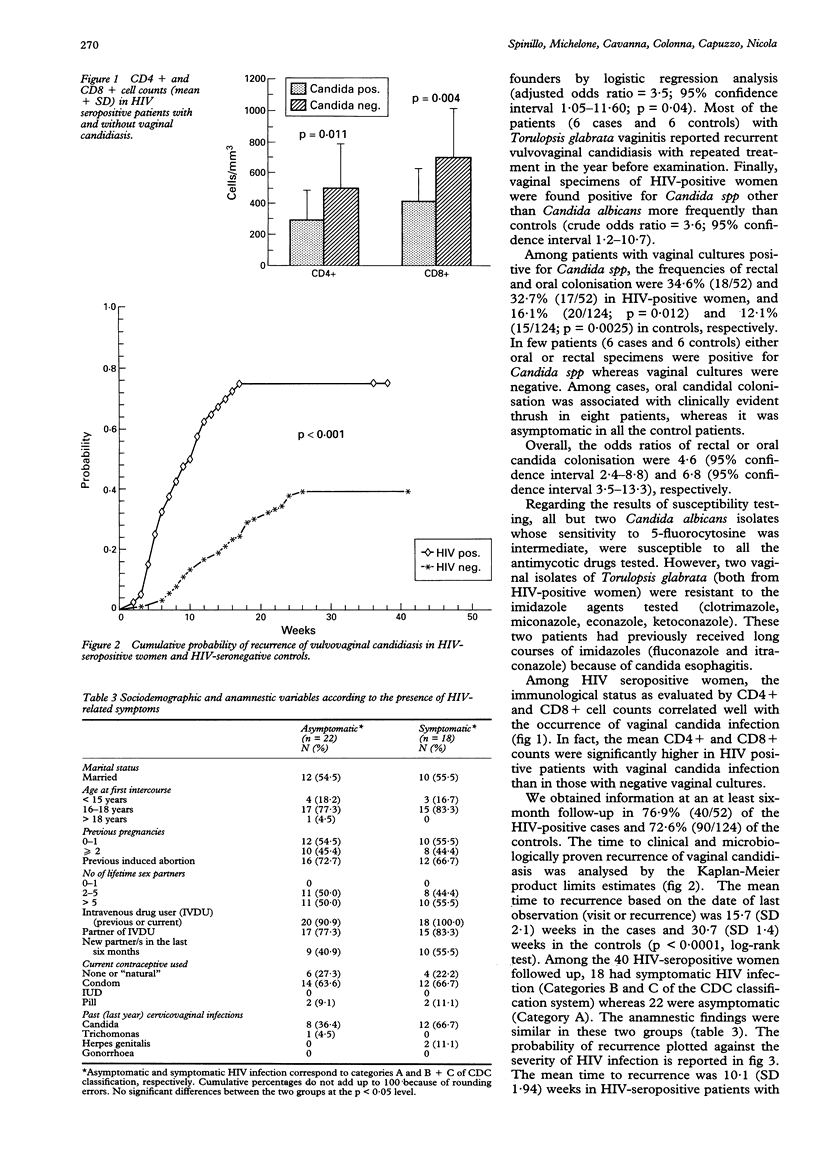
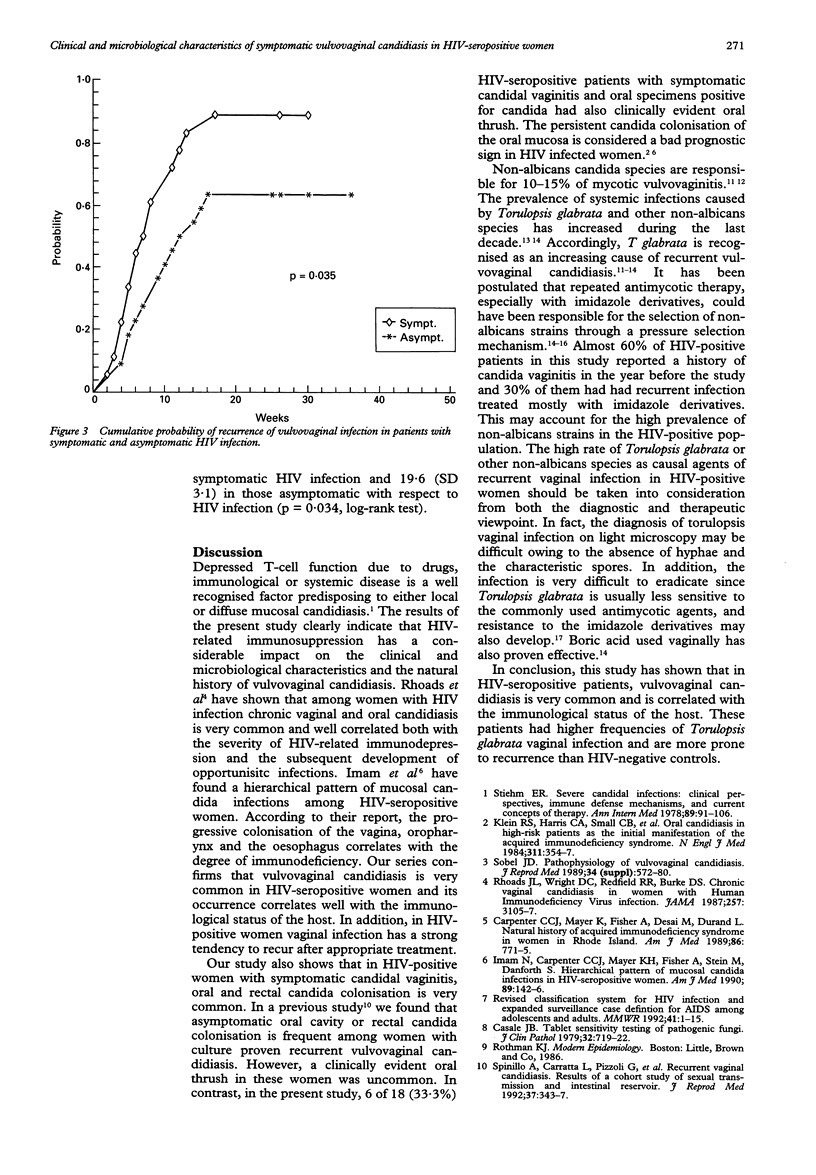
OBJECTIVES--To evaluate the clinical and microbiological characteristics of symptomatic vaginal candidiasis in Human Immunodeficiency Virus (HIV)-seropositive women attending a gynaecologic outpatient clinic for sexually transmitted diseases (STDs). DESIGN--Vaginal, rectal and oral specimens from cases and controls were cultured for Candida spp. SUBJECTS--Eighty-four consecutive HIV-seropositive and 384 HIV-seronegative women with clinical signs of vulvovaginitis. SETTING--A gynaecological out-patient clinic in Pavia, Italy. RESULTS--The overall prevalence of vaginal candidiasis was 61.9% (52/84) in the cases and 32.3% (124/384; p < .001) in the controls. After adjustment by logistic regression analysis for confounding factors (age at first intercourse, lifetime sex partners, new partner/s in the last 6 months, type of contraceptive used), HIV-seropositive patients were at higher risk for both Candida albicans (odds ratio = 2.5; 95% confidence interval 1.31-4.69; p = 0.006) and Torulopsis glabrata vaginitis (OR = 3.5; 95% CI = 1.05-11.60; p = 0.04) than controls. HIV-seropositive subjects had also increased rates of oral and rectal colonisation with Candida spp. Finally, the time to recurrence of vaginal infection was significantly shorter in HIV-seropositive patients than controls and was correlated with the severity of HIV-induced immunodepression. CONCLUSIONS--Vulvovaginal candidiasis is very common in HIV-seropositive women and its prevalence is correlated with the immunological status of the host. These patients have higher frequencies of Torulopsis glabrata vaginal infection and are more prone to recurrence than HIV-seronegative controls.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carpenter C. C., Mayer K. H., Fisher A., Desai M. B., Durand L. Natural history of acquired immunodeficiency syndrome in women in Rhode Island. Am J Med. 1989 Jun;86(6 Pt 2):771–775. doi: 10.1016/0002-9343(89)90471-3. [DOI] [PubMed] [Google Scholar]
- Casals J. B. Tablet sensitivity testing on pathogenic fungi. J Clin Pathol. 1979 Jul;32(7):719–722. doi: 10.1136/jcp.32.7.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. E., Jr, Lehrer R. I., Stiehm E. R., Fischer T. J., Young L. S. Severe candidal infections: clinical perspective, immune defense mechanisms, and current concepts of therapy. Ann Intern Med. 1978 Jul;89(1):91–106. doi: 10.7326/0003-4819-89-1-91. [DOI] [PubMed] [Google Scholar]
- Horowitz B. J. Mycotic vulvovaginitis: a broad overview. Am J Obstet Gynecol. 1991 Oct;165(4 Pt 2):1188–1192. doi: 10.1016/s0002-9378(12)90725-5. [DOI] [PubMed] [Google Scholar]
- Imam N., Carpenter C. C., Mayer K. H., Fisher A., Stein M., Danforth S. B. Hierarchical pattern of mucosal candida infections in HIV-seropositive women. Am J Med. 1990 Aug;89(2):142–146. doi: 10.1016/0002-9343(90)90291-k. [DOI] [PubMed] [Google Scholar]
- Kerridge D., Nicholas R. O. Drug resistance in the opportunistic pathogens Candida albicans and Candida glabrata. J Antimicrob Chemother. 1986 Oct;18 (Suppl B):39–49. doi: 10.1093/jac/18.supplement_b.39. [DOI] [PubMed] [Google Scholar]
- Klein R. S., Harris C. A., Small C. B., Moll B., Lesser M., Friedland G. H. Oral candidiasis in high-risk patients as the initial manifestation of the acquired immunodeficiency syndrome. N Engl J Med. 1984 Aug 9;311(6):354–358. doi: 10.1056/NEJM198408093110602. [DOI] [PubMed] [Google Scholar]
- Komshian S. V., Uwaydah A. K., Sobel J. D., Crane L. R. Fungemia caused by Candida species and Torulopsis glabrata in the hospitalized patient: frequency, characteristics, and evaluation of factors influencing outcome. Rev Infect Dis. 1989 May-Jun;11(3):379–390. doi: 10.1093/clinids/11.3.379. [DOI] [PubMed] [Google Scholar]
- Meunier F. Prevention and mycoses in immunocompromised patients. Rev Infect Dis. 1987 Mar-Apr;9(2):408–416. doi: 10.1093/clinids/9.2.408. [DOI] [PubMed] [Google Scholar]
- Redondo-Lopez V., Lynch M., Schmitt C., Cook R., Sobel J. D. Torulopsis glabrata vaginitis: clinical aspects and susceptibility to antifungal agents. Obstet Gynecol. 1990 Oct;76(4):651–655. [PubMed] [Google Scholar]
- Rhoads J. L., Wright D. C., Redfield R. R., Burke D. S. Chronic vaginal candidiasis in women with human immunodeficiency virus infection. JAMA. 1987 Jun 12;257(22):3105–3107. [PubMed] [Google Scholar]
- Sobel J. D. Candidal vulvovaginitis. Clin Obstet Gynecol. 1993 Mar;36(1):153–165. doi: 10.1097/00003081-199303000-00021. [DOI] [PubMed] [Google Scholar]
- Sobel J. D. Pathophysiology of vulvovaginal candidiasis. J Reprod Med. 1989 Aug;34(8 Suppl):572–580. [PubMed] [Google Scholar]
- Spinillo A., Carratta L., Pizzoli G., Lombardi G., Cavanna C., Michelone G., Guaschino S. Recurrent vaginal candidiasis. Results of a cohort study of sexual transmission and intestinal reservoir. J Reprod Med. 1992 Apr;37(4):343–347. [PubMed] [Google Scholar]
- Spinillo A., Pizzoli G., Colonna L., Nicola S., De Seta F., Guaschino S. Epidemiologic characteristics of women with idiopathic recurrent vulvovaginal candidiasis. Obstet Gynecol. 1993 May;81(5 ):721–727. [PubMed] [Google Scholar]


