Abstract
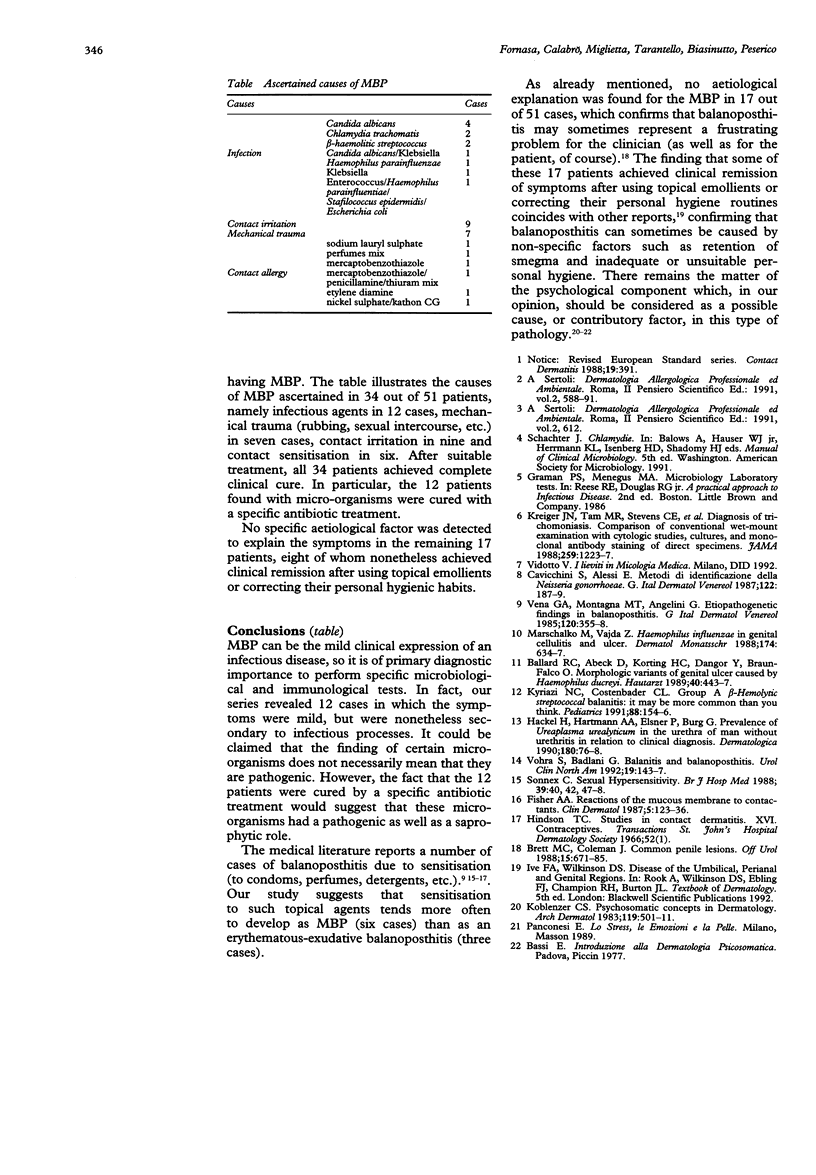
AIM--To identify and study cases of mild balanoposthitis (MBP) with penile pathology among patients observed at a dermatology clinic over an 18-month period. MATERIALS--The study included 321 patients with penile pathology. The term MBP was used to describe balanoposthitis of a localised, inflammatory nature with few, non-specific symptoms and a tendency to become chronic or recur. Two hundred and seventy had diseases clearly identifiable by clinical examination or laboratory tests; 51 cases were diagnosed as MBP and these patients had blood tests (to evaluate immune status) and microbiological examination; when these proved negative, a series of patch tests was also used. RESULTS--Of the 51 patients diagnosed as having MBP, the cause was ascertained in 34 cases (infection, mechanical trauma, contact irritation, contact allergy, etc.), whereas no specific aetiological factor was detected to explain the symptoms in the remaining 17 cases.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ballard R. C., Abeck D., Korting H. C., Dangor Y., Braun-Falco O. Morphologische Varianten des durch Haemophilus ducreyi bedingten Genitalulkus. Hautarzt. 1989 Jul;40(7):443–447. [PubMed] [Google Scholar]
- Cavicchini S., Alessi E. Metodi di identificazione della Neisseria gonorrhoeae. G Ital Dermatol Venereol. 1987 Apr;122(4):187–189. [PubMed] [Google Scholar]
- Fisher A. A. Reactions of the mucous membrane to contactants. Clin Dermatol. 1987 Apr-Jun;5(2):123–136. doi: 10.1016/0738-081x(87)90014-9. [DOI] [PubMed] [Google Scholar]
- Hackel H., Hartmann A. A., Elsner P., Burg G. Prevalence of Ureaplasma urealyticum in the urethra of men without urethritis in relation to clinical diagnosis. Dermatologica. 1990;180(2):76–78. doi: 10.1159/000247995. [DOI] [PubMed] [Google Scholar]
- Koblenzer C. S. Psychosomatic concepts in dermatology. A dermatologist-psychoanalyst's viewpoint. Arch Dermatol. 1983 Jun;119(6):501–512. [PubMed] [Google Scholar]
- Krieger J. N., Tam M. R., Stevens C. E., Nielsen I. O., Hale J., Kiviat N. B., Holmes K. K. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA. 1988 Feb 26;259(8):1223–1227. doi: 10.1001/jama.259.8.1223. [DOI] [PubMed] [Google Scholar]
- Kyriazi N. C., Costenbader C. L. Group A beta-hemolytic streptococcal balanitis: it may be more common than you think. Pediatrics. 1991 Jul;88(1):154–156. [PubMed] [Google Scholar]
- Marschalko M., Vajda Z. Haemophilus influencae bei Genital-Zellulitis und Geschwür. Dermatol Monatsschr. 1988;174(10):634–637. [PubMed] [Google Scholar]
- Sonnex C. Sexual hypersensitivity. Br J Hosp Med. 1988 Jan;39(1):40, 42, 47-8. [PubMed] [Google Scholar]
- Vena G. A., Montagna M. T., Angelini G. Rilievi eziopatogenetici nelle balanopostiti. G Ital Dermatol Venereol. 1985 Sep-Oct;120(5):355–358. [PubMed] [Google Scholar]
- Vohra S., Badlani G. Balanitis and balanoposthitis. Urol Clin North Am. 1992 Feb;19(1):143–147. [PubMed] [Google Scholar]


