Abstract
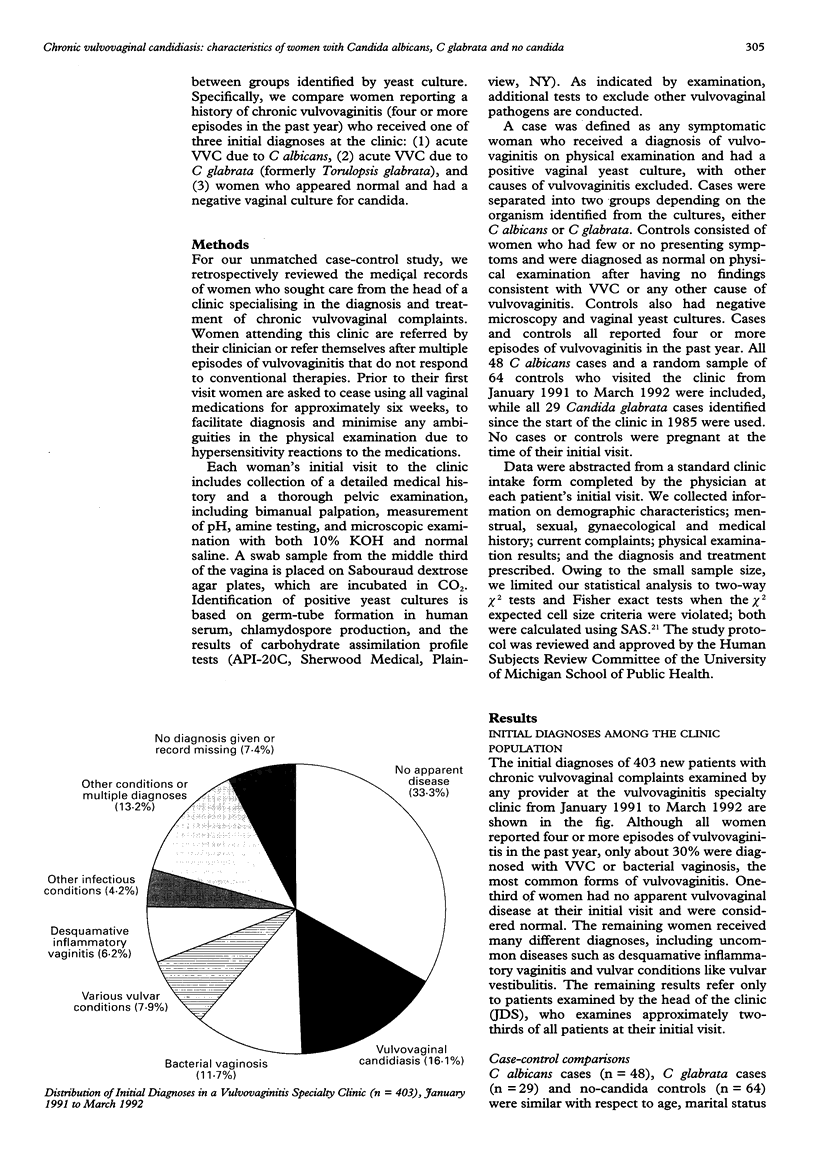
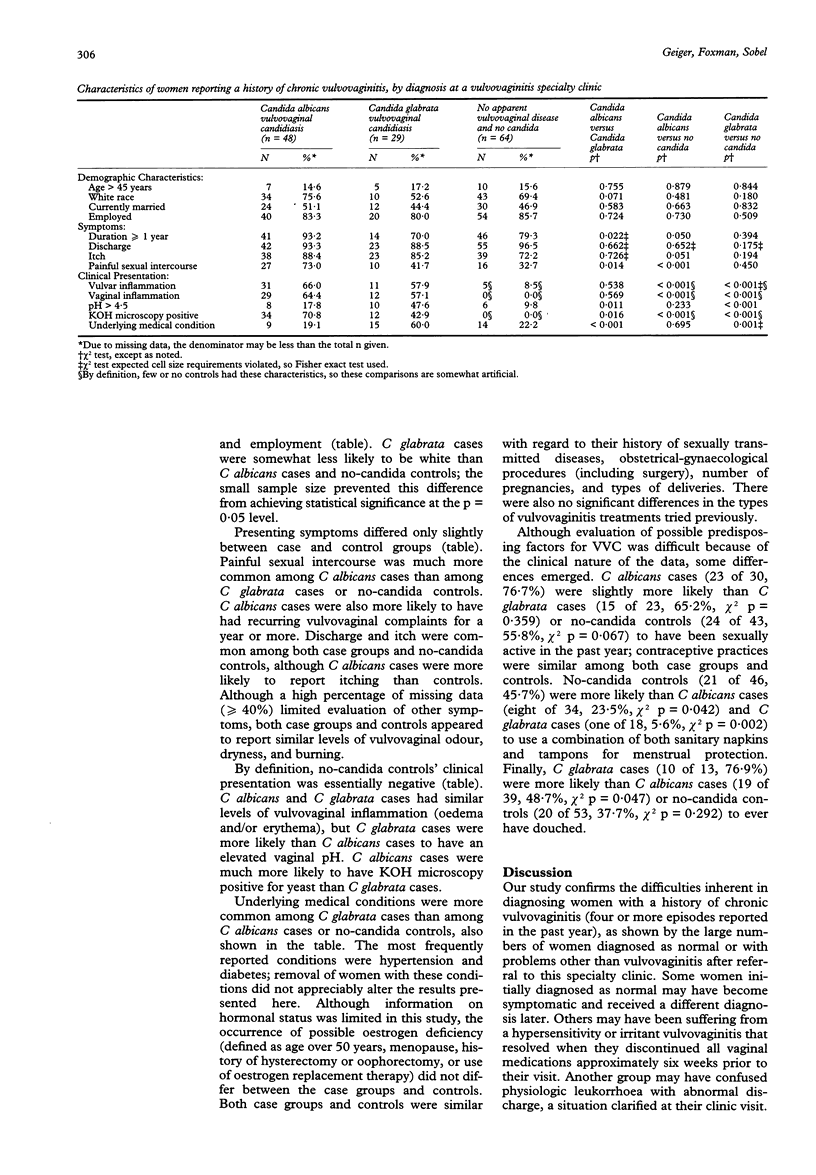
INTRODUCTION--Although as many as 5% of all women complain of chronic vulvovaginitis, little is known about these women. They may often be misdiagnosed and the role of vaginal yeast culture in diagnosing vulvovaginal candidiasis (VVC) among them has not been clearly defined. METHODS--To address these deficiencies, we tabulated initial diagnoses among new patients and conducted a medical record-based, unmatched case-control study among women reporting a history of chronic vulvovaginitis (four or more episodes in the past year) at a vulvovaginitis specialty clinic. Clinical presentation and medical history were compared for women who had a positive vaginal yeast culture for either Candida albicans or C glabrata, or who had a negative culture. RESULTS--One-third of the women had no apparent vulvovaginal disease at their initial visit. All women reported similar symptoms, except for an increased prevalence of painful sexual intercourse in women with C albicans (chi 2 p = 0.014 versus women with C glabrata and p < 0.001 versus women with no candida). Women with C glabrata were more likely to be non-white (chi 2 p = 0.071 compared with women with C albicans) and to report an underlying medical condition (chi 2 p < or = 0.001 versus both women with C albicans and women with no candida). Physical examination was normal only in women with no candida. C albicans cases were more likely to have positive potassium hydroxide microscopy (chi 2 p = 0.016) and a pH < or = 4.5 (chi 2 p = 0.011) than were C glabrata cases. CONCLUSIONS--These results suggest that reliance on symptoms and signs alone will result in significant misdiagnosis of chronic vulvovaginitis. Among women with VVC, subtle differences in clinical presentation do not reliably distinguish women with C albicans from those with C glabrata. Our study also indicates that vaginal yeast cultures, while not necessary for every patient, are valuable in confirming negative diagnoses, detecting microscopy false-negatives, and identifying non-C albicans isolates.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arilla M. C., Carbonero J. L., Schneider J., Regúlez P., Quindós G., Pontón J., Cisterna R. Vulvovaginal candidiasis refractory to treatment with fluconazole. Eur J Obstet Gynecol Reprod Biol. 1992 Mar 23;44(1):77–80. doi: 10.1016/0028-2243(92)90317-r. [DOI] [PubMed] [Google Scholar]
- Berg A. O., Heidrich F. E., Fihn S. D., Bergman J. J., Wood R. W., Stamm W. E., Holmes K. K. Establishing the cause of genitourinary symptoms in women in a family practice. Comparison of clinical examination and comprehensive microbiology. JAMA. 1984 Feb 3;251(5):620–625. [PubMed] [Google Scholar]
- Bergman J. J., Berg A. O. How useful are symptoms in the diagnosis of Candida vaginitis? J Fam Pract. 1983 Mar;16(3):509–511. [PubMed] [Google Scholar]
- Bleker O. P., Folkertsma K., Dirks-Go S. I. Diagnostic procedures in vaginitis. Eur J Obstet Gynecol Reprod Biol. 1989 May;31(2):179–183. doi: 10.1016/0028-2243(89)90179-2. [DOI] [PubMed] [Google Scholar]
- Boquet-Jiménez E., Alvarez San Cristóbal A. Cytologic and microbiologic aspects of vaginal Torulopsis. Acta Cytol. 1978 Sep-Oct;22(5):331–334. [PubMed] [Google Scholar]
- Friedrich E. G., Jr Vaginitis. Am J Obstet Gynecol. 1985 Jun 1;152(3):247–251. doi: 10.1016/s0002-9378(85)80203-9. [DOI] [PubMed] [Google Scholar]
- Goldacre M. J., Milne L. J., Watt B., Loudon N., Vessey M. P. Prevalence of Yeast and fungi other than Candida albicans in the vagina of normal young women. Br J Obstet Gynaecol. 1981 Jun;88(6):596–600. doi: 10.1111/j.1471-0528.1981.tb01214.x. [DOI] [PubMed] [Google Scholar]
- Higashide K., Aman R., Yamamuro O. Clinical characteristics correlated with different fungi causing vulvovaginal mycosis. Mycoses. 1988 Apr;31(4):213-8, 223-5. [PubMed] [Google Scholar]
- Horowitz B. J., Giaquinta D., Ito S. Evolving pathogens in vulvovaginal candidiasis: implications for patient care. J Clin Pharmacol. 1992 Mar;32(3):248–255. doi: 10.1002/j.1552-4604.1992.tb03833.x. [DOI] [PubMed] [Google Scholar]
- Hurley R. Inveterate vaginal thrush. Practitioner. 1975 Dec;215(1290):753–756. [PubMed] [Google Scholar]
- Kaufman R. H., Hammill H. A. Vaginitis. Prim Care. 1990 Mar;17(1):115–125. [PubMed] [Google Scholar]
- O'Neill S., Howard J. Recurrent vulvovaginal candidiasis. A gynaecological enigma. Aust Fam Physician. 1989 Feb;18(2):99–102. [PubMed] [Google Scholar]
- Ott A. K., Ashman R. B. Modern perspectives on vaginal candidiasis. Aust Fam Physician. 1989 Jun;18(6):695–697. [PubMed] [Google Scholar]
- Redondo-Lopez V., Lynch M., Schmitt C., Cook R., Sobel J. D. Torulopsis glabrata vaginitis: clinical aspects and susceptibility to antifungal agents. Obstet Gynecol. 1990 Oct;76(4):651–655. [PubMed] [Google Scholar]
- Reed B. D., Huck W., Zazove P. Differentiation of Gardnerella vaginalis, Candida albicans, and Trichomonas vaginalis infections of the vagina. J Fam Pract. 1989 Jun;28(6):673–680. [PubMed] [Google Scholar]
- Reed B. D., Slattery M. L., French T. K. The association between dietary intake and reported history of Candida vulvovaginitis. J Fam Pract. 1989 Nov;29(5):509–515. [PubMed] [Google Scholar]
- Schaaf V. M., Perez-Stable E. J., Borchardt K. The limited value of symptoms and signs in the diagnosis of vaginal infections. Arch Intern Med. 1990 Sep;150(9):1929–1933. [PubMed] [Google Scholar]
- Siapco B. J., Kaplan B. J., Bernstein G. S., Moyer D. L. Cytodiagnosis of Candida organisms in cervical smears. Acta Cytol. 1986 Sep-Oct;30(5):477–480. [PubMed] [Google Scholar]
- Sobel J. D. Candidal vulvovaginitis. Clin Obstet Gynecol. 1993 Mar;36(1):153–165. doi: 10.1097/00003081-199303000-00021. [DOI] [PubMed] [Google Scholar]
- Summers P. R., Sharp H. T. The management of obscure or difficult cases of vulvovaginitis. Clin Obstet Gynecol. 1993 Mar;36(1):206–214. doi: 10.1097/00003081-199303000-00026. [DOI] [PubMed] [Google Scholar]
- White D. J., Johnson E. M., Warnock D. W. Management of persistent vulvo vaginal candidosis due to azole-resistant Candida glabrata. Genitourin Med. 1993 Apr;69(2):112–114. doi: 10.1136/sti.69.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]