Abstract
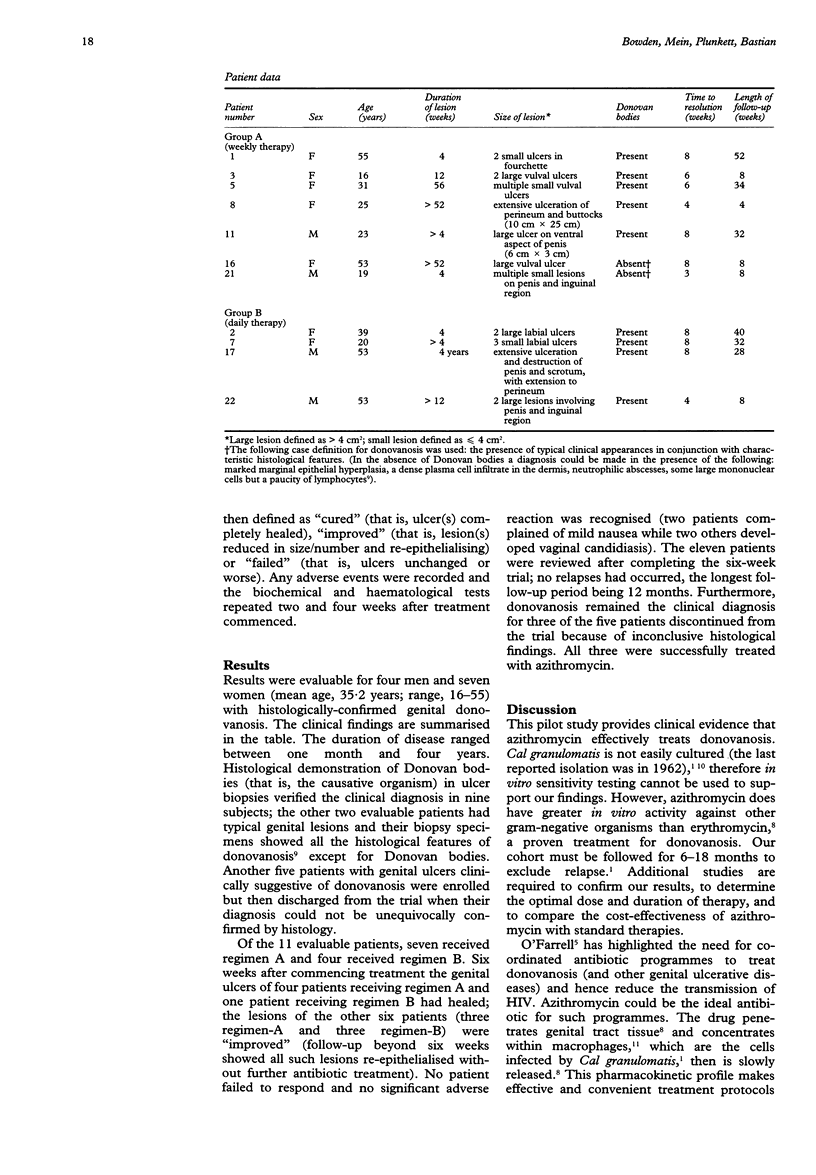
OBJECTIVES: To determine the effectiveness of azithromycin, an azalide antibiotic with long tissue half-life, in a pilot study of patients with genital donovanosis in the Northern Territory, Australia. DESIGN: Patients with histologically confirmed donovanosis were randomised to receive one of two open-label azithromycin dosage regimens: Regimen A--1.0 g once weekly for 4 weeks; or Regimen B--500 mg daily for 7 days. Patients were assessed at 6 weeks and classified as either "cured", "improved" or "failed". RESULTS: Seven patients received regimen A and 4 received regimen B. Six weeks after commencing treatment the genital ulcers of four patients receiving regimen A and one patient receiving regimen B had healed; the lesions of the other six patients (3 in each regimen) were "improved". No patient failed to respond and no significant adverse reaction was recognised. The eleven patients were reviewed after completing the six-week trial; all lesions had re-epithelialised without further antibiotic treatment, no relapses had occurred, the longest follow-up period being seven months. A further 17 patients with donovanosis who were unable to meet the entry criteria were also treated successfully with azithromycin during the study period. CONCLUSIONS: This is the first time that azithromycin has been shown to have clinical activity against donovanosis. Poor compliance with prolonged courses of antibiotics is one of the major barriers to control of the disease. Intermittent or short-course therapy, made possible by the long tissue half-life of the drug, could facilitate control of donovanosis in endemic populations if the high cost of medication can be addressed.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bowden F. J., Farmer B., Bullen J., Chamberlain V., Bastian I. Azithromycin and syphilis. Genitourin Med. 1995 Jun;71(3):196–197. doi: 10.1136/sti.71.3.196-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDBERG J. Studies on granuloma inguinale. V. Isolation of a bacterium resembling Donovania granulomatis from the faeces of a patient with granuloma inguinale. Br J Vener Dis. 1962 Jun;38:99–102. doi: 10.1136/sti.38.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladue R. P., Bright G. M., Isaacson R. E., Newborg M. F. In vitro and in vivo uptake of azithromycin (CP-62,993) by phagocytic cells: possible mechanism of delivery and release at sites of infection. Antimicrob Agents Chemother. 1989 Mar;33(3):277–282. doi: 10.1128/aac.33.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merianos A., Gilles M., Chuah J. Ceftriaxone in the treatment of chronic donovanosis in central Australia. Genitourin Med. 1994 Apr;70(2):84–89. doi: 10.1136/sti.70.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Farrell N. Global eradication of donovanosis: an opportunity for limiting the spread of HIV-1 infection. Genitourin Med. 1995 Feb;71(1):27–31. doi: 10.1136/sti.71.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters D. H., Friedel H. A., McTavish D. Azithromycin. A review of its antimicrobial activity, pharmacokinetic properties and clinical efficacy. Drugs. 1992 Nov;44(5):750–799. doi: 10.2165/00003495-199244050-00007. [DOI] [PubMed] [Google Scholar]
- Richens J. The diagnosis and treatment of donovanosis (granuloma inguinale). Genitourin Med. 1991 Dec;67(6):441–452. doi: 10.1136/sti.67.6.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sehgal V. N., Shyamprasad A. L., Beohar P. C. The histopathological diagnosis of donovanosis. Br J Vener Dis. 1984 Feb;60(1):45–47. doi: 10.1136/sti.60.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdon M. S., Handsfield H. H., Johnson R. B. Pilot study of azithromycin for treatment of primary and secondary syphilis. Clin Infect Dis. 1994 Sep;19(3):486–488. doi: 10.1093/clinids/19.3.486. [DOI] [PubMed] [Google Scholar]
- Wasserheit J. N. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992 Mar-Apr;19(2):61–77. [PubMed] [Google Scholar]


