Abstract
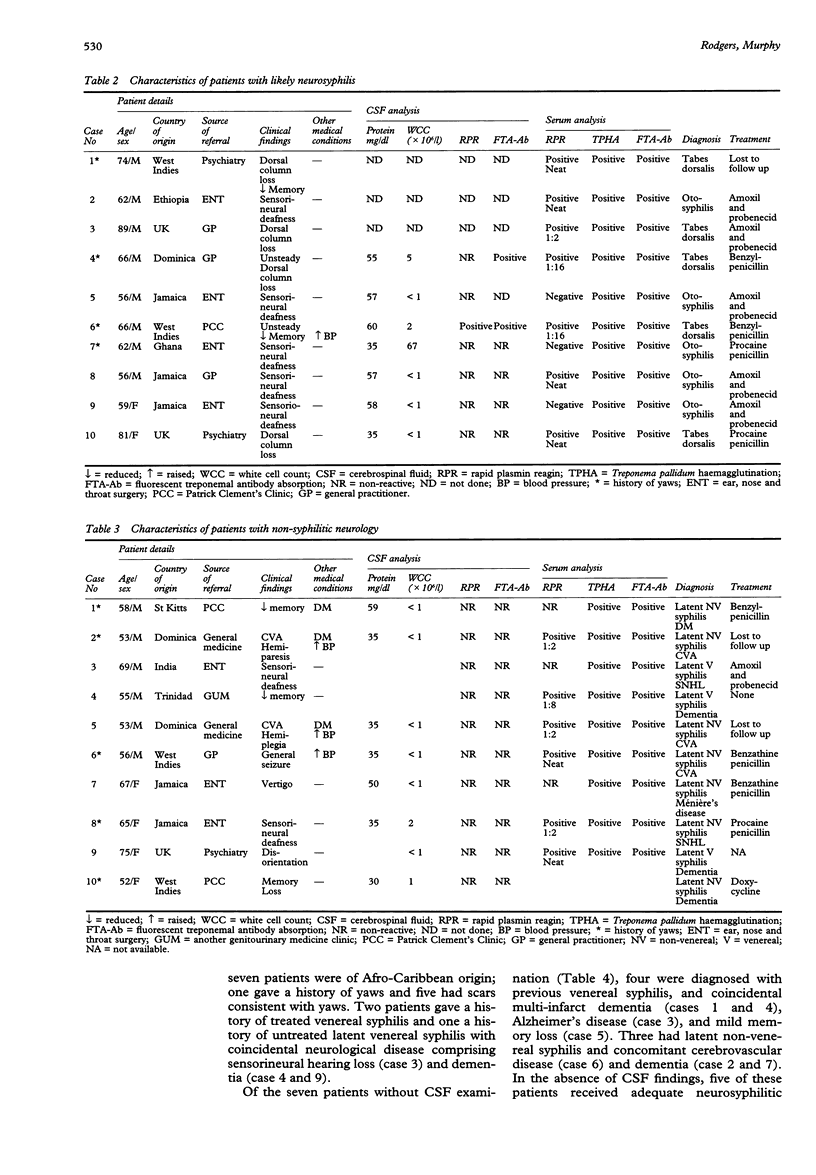
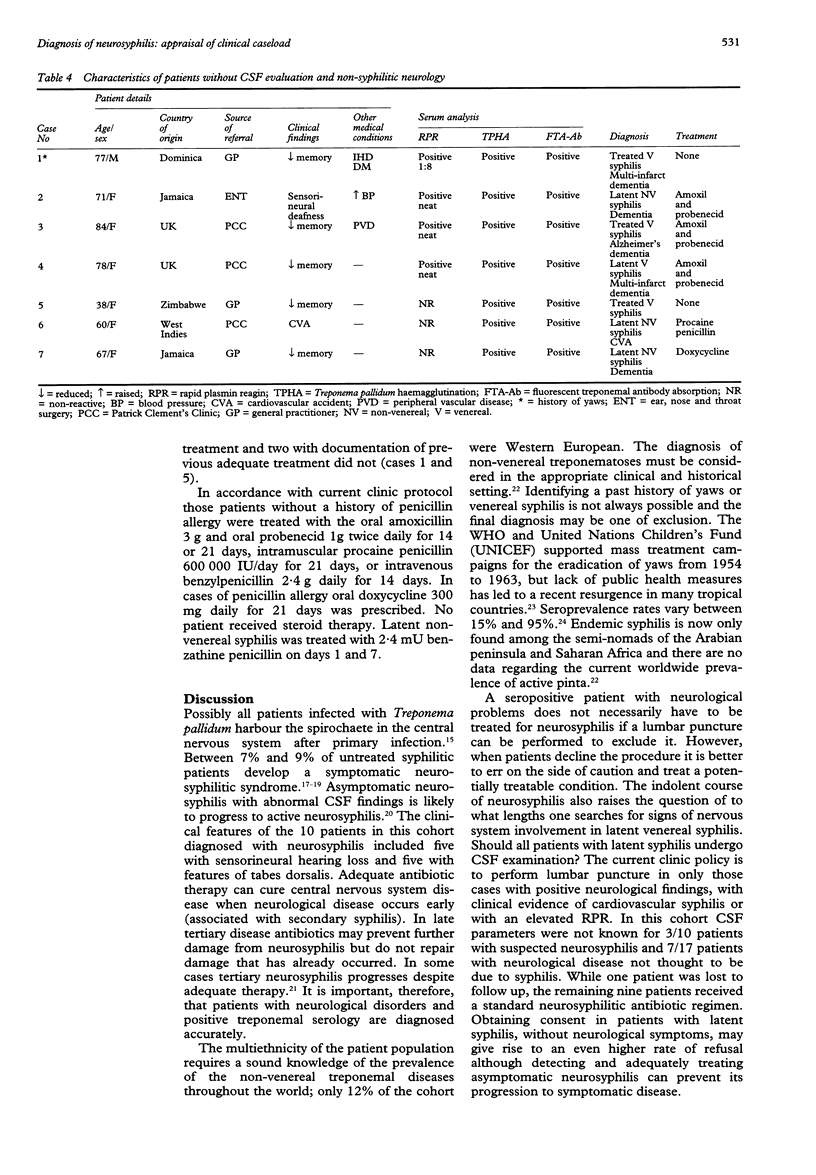
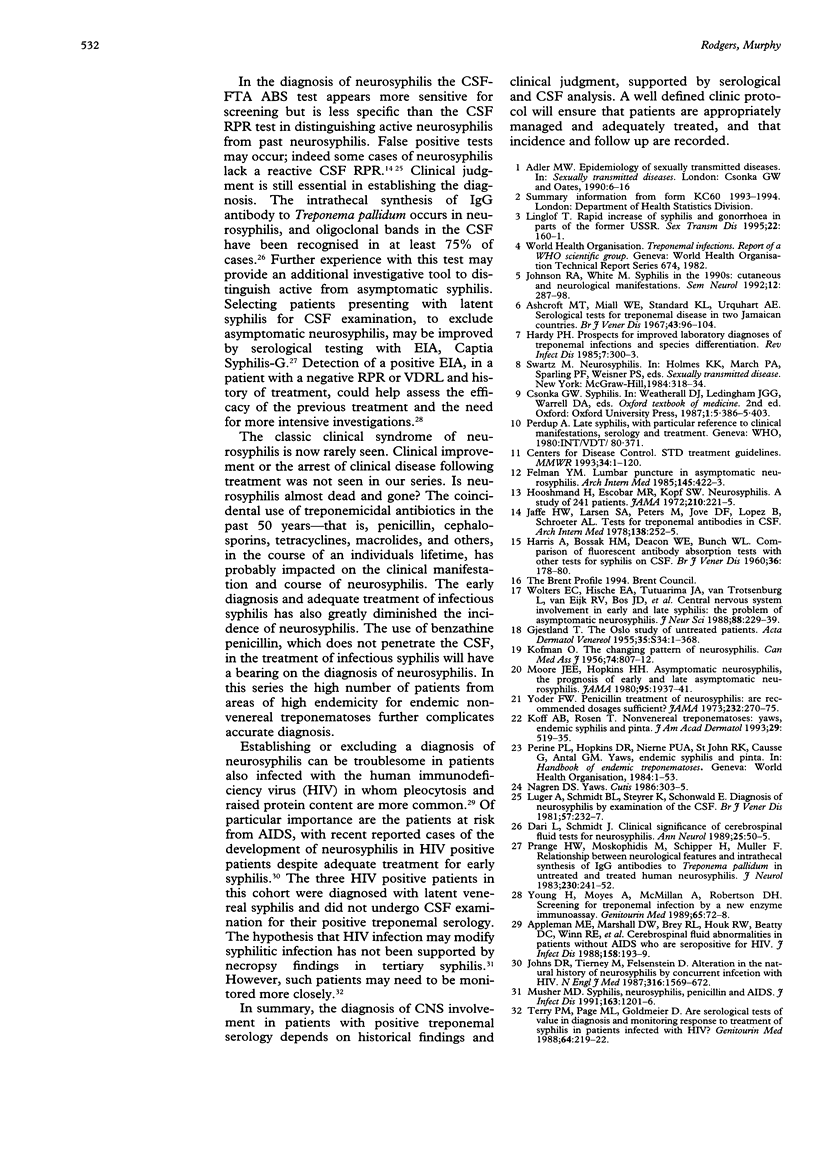
OBJECTIVES: To review the management of a cohort of patients with positive treponemal serology and psychiatric and/or neurological disorders. METHODS: A retrospective case note review of 172 patients with positive treponemal serology attending the Patrick Clement's Clinic, Central Middlesex Hospital between December 1990 and November 1995 was performed. RESULTS: 101 men and 71 women were new attenders diagnosed with positive treponemal serology. A neurological problem was identified in 27 patients (12 women and 15 men) with psychiatric and/or neurological disorders, of whom 20 (six women and 14 men) underwent investigation of the cerebrospinal fluid (CSF). With the medical history and results of CSF-RPR and FTA tests, white cell count (WCC), and total protein level in the CSF, 10 patients (eight men and two women) were diagnosed with likely neurosyphilis and 17 with neurological disorders not thought to be caused by syphilis. The clinical features in those having neurosyphilis were sensorineural hearing loss (n = 5) and tabes dorsalis (n = 5). In the seven patients diagnosed with neurosyphilis who underwent CSF examination one patient had a reactive CSF-FTA, elevated protein, and elevated WCC; one patient had a reactive CSF-FTA and RPR with elevated protein; the total protein only was elevated in three cases and the WCC elevated in one case. Nine of the 10 patients with neurosyphilis received adequate neurosyphilitic treatment; one patient was lost to follow up. CONCLUSIONS: The management of patients with positive treponemal serology and psychiatric and/or neurological disorders was consistent. Patients with suspected neurosyphilis or patients with neurological signs compatible with neurosyphilis (who did not undergo CSF examination) were treated with adequate neurosyphilitic therapy.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Appleman M. E., Marshall D. W., Brey R. L., Houk R. W., Beatty D. C., Winn R. E., Melcher G. P., Wise M. G., Sumaya C. V., Boswell R. N. Cerebrospinal fluid abnormalities in patients without AIDS who are seropositive for the human immunodeficiency virus. J Infect Dis. 1988 Jul;158(1):193–199. doi: 10.1093/infdis/158.1.193. [DOI] [PubMed] [Google Scholar]
- Ashcroft M. T., Miall W. E., Standard K. L., Urquhart A. E. Serological tests for treponemal disease in adults in two Jamaican communities. Br J Vener Dis. 1967 Jun;43(2):96–104. doi: 10.1136/sti.43.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARRIS A., BOSSAK H. M., DEACON W. E., BUNCH W. L., Jr Comparison of the fluorescent treponemal antibody test with other tests for syphilis on cerebrospinal fluids. Br J Vener Dis. 1960 Sep;36:178–180. doi: 10.1136/sti.36.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe H. W., Larsen S. A., Peters M., Jove D. F., Lopez B., Schroeter A. L. Tests for treponemal antibody in CSF. Arch Intern Med. 1978 Feb;138(2):252–255. [PubMed] [Google Scholar]
- Johns D. R., Tierney M., Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immunodeficiency virus. N Engl J Med. 1987 Jun 18;316(25):1569–1572. doi: 10.1056/NEJM198706183162503. [DOI] [PubMed] [Google Scholar]
- Johnson R. A., White M. Syphilis in the 1990s: cutaneous and neurologic manifestations. Semin Neurol. 1992 Dec;12(4):287–298. doi: 10.1055/s-2008-1041185. [DOI] [PubMed] [Google Scholar]
- KOFMAN O. The changing pattern of neurosyphilis. Can Med Assoc J. 1956 May 15;74(10):807–812. [PMC free article] [PubMed] [Google Scholar]
- Koff A. B., Rosen T. Nonvenereal treponematoses: yaws, endemic syphilis, and pinta. J Am Acad Dermatol. 1993 Oct;29(4):519–538. doi: 10.1016/0190-9622(93)70217-h. [DOI] [PubMed] [Google Scholar]
- Linglöf T. Rapid increase of syphilis and gonorrhea in parts of the former USSR. Sex Transm Dis. 1995 May-Jun;22(3):160–161. doi: 10.1097/00007435-199505000-00005. [DOI] [PubMed] [Google Scholar]
- Luger A., Schmidt B. L., Steyrer K., Schonwald E. Diagnosis of neurosyphilis by examination of the cerebrospinal fluid. Br J Vener Dis. 1981 Aug;57(4):232–237. doi: 10.1136/sti.57.4.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musher D. M. Syphilis, neurosyphilis, penicillin, and AIDS. J Infect Dis. 1991 Jun;163(6):1201–1206. doi: 10.1093/infdis/163.6.1201. [DOI] [PubMed] [Google Scholar]
- Nagreh D. S. Yaws. Cutis. 1986 Nov;38(5):303–305. [PubMed] [Google Scholar]
- Prange H. W., Moskophidis M., Schipper H. I., Müller F. Relationship between neurological features and intrathecal synthesis of IgG antibodies to Treponema pallidum in untreated and treated human neurosyphilis. J Neurol. 1983;230(4):241–252. doi: 10.1007/BF00313700. [DOI] [PubMed] [Google Scholar]
- Terry P. M., Page M. L., Goldmeier D. Are serological tests of value in diagnosing and monitoring response to treatment of syphilis in patients infected with human immunodeficiency virus? Genitourin Med. 1988 Aug;64(4):219–222. doi: 10.1136/sti.64.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolters E. C., Hische E. A., Tutuarima J. A., van Trotsenburg L., van Eijk R. V., Bos J. D., Starink T. M., Emsbroek L. J., van der Helm H. J. Central nervous system involvement in early and late syphilis: the problem of asymptomatic neurosyphilis. J Neurol Sci. 1988 Dec;88(1-3):229–239. doi: 10.1016/0022-510x(88)90220-1. [DOI] [PubMed] [Google Scholar]
- Yoder F. W. Penicillin treatment of neurosyphilis. Are recommended dosages sufficient? JAMA. 1975 Apr 21;232(3):270–271. [PubMed] [Google Scholar]
- Young H., Moyes A., McMillan A., Robertson D. H. Screening for treponemal infection by a new enzyme immunoassay. Genitourin Med. 1989 Apr;65(2):72–78. doi: 10.1136/sti.65.2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]


