Abstract
Microsporidia are long-known parasitic organisms of almost every animal group, including invertebrates and vertebrates. Microsporidia emerged as important opportunistic pathogens in humans when AIDS became pandemic and, more recently, have also increasingly been detected in otherwise immunocompromised patients, including organ transplant recipients, and in immunocompetent persons with corneal infection or diarrhea. Two species causing rare infections in humans, Encephalitozoon cuniculi and Brachiola vesicularum, had previously been described from animal hosts (vertebrates and insects, respectively). However, several new microsporidial species, including Enterocytozoon bieneusi, the most prevalent human microsporidian causing human immunodeficiency virus-associated diarrhea, have been discovered in humans, raising the question of their natural origin. Vertebrate hosts are now identified for all four major microsporidial species infecting humans (E. bieneusi and the three Encephalitozoon spp.), implying a zoonotic nature of these parasites. Molecular studies have identified phenotypic and/or genetic variability within these species, indicating that they are not uniform, and have allowed the question of their zoonotic potential to be addressed. The focus of this review is the zoonotic potential of the various microsporidia and a brief update on other microsporidia which have no known host or an invertebrate host and which cause rare infections in humans.
INTRODUCTION
Microsporidia are an exceptionally diverse group of organisms, comprising more than 1,200 species which parasitize a wide variety of invertebrate and vertebrate hosts. These organisms have long been known to be causative agents of economically important diseases in insects (silk worms and honey bees) (14), fish (179, 256), and mammals (rabbits, fur-bearing animals, and laboratory rodents) (37), and they emerged as important opportunistic pathogens when AIDS became pandemic (320). Thus, the question of whether animal reservoirs are the sources of human infections is reasonable.
The focus of this review is to discuss the most recent perceptions on the zoonotic potential of the various microsporidia with proven vertebrate hosts. Furthermore, we provide a brief update on other microsporidia which have no known vertebrate host or an invertebrate host and cause rare infections in humans.
The Organisms
Microsporidia are unicellular, obligate intracellular eukaryotes. Their life cycle includes a proliferative merogonic stage, followed by a sporogonic stage resulting in characteristically small (1 to 4 μm), environmentally resistant, infective spores (Fig. 1) (95). The spores contain a long, coiled tubular extrusion apparatus (“polar tube”), which distinguishes microsporidia from all other organisms and has a crucial role in host cell invasion: Upon extrusion from the spore, it injects the sporoplasm along with its nucleus into the cytoplasm of a new host cell after piercing the plasmalemma of the host cell or the membrane of the phagosomes containing the endocytosed spores (58, 106).
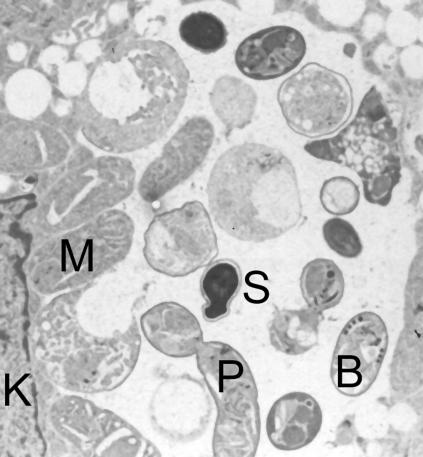
FIG. 1.
Electron micrograph of the developmental stages of the microsporidian species Encephalitozoon cuniculi in a host cell-derived vacuole in in vitro-cultivated human fibroblast cells. K, nucleus of host cell; M, meront; P, sporont, which divides into two sporoblasts; B, sporoblast (2 μm in length), with cross sections of the polar tube; S, mature spore.
Before the onset of the AIDS pandemic, only eight cases of human microsporidial infections had been reported (reviewed in reference 320). In most cases, species identification of the causative agents was not conclusive. In 1985, as early as 2 years after the identification of human immunodeficiency virus (HIV) as the causative agent of AIDS, the microsporidial species Enterocytozoon bieneusi was discovered in HIV-infected patients with chronic diarrhea (76). Subsequently, several new genera and species of microsporidia were found to be important opportunistic pathogens in humans, infecting virtually every organ in the body and a broad spectrum of cell types (217) (Table 1).
TABLE 1.
Microsporidial species infecting humans
| Species | Discovery
|
No. of confirmed reported patients
|
Site(s) of infection (reference[s]) | Animal host(s) | |||
|---|---|---|---|---|---|---|---|
| Host | Yr | Reference(s) | Immuno- compromiseda | Immuno- competentb | |||
| Enterocytozoon bieneusi | Human | 1985 | 76 | >1,000 | <20 | Intestine, biliary tract, respiratory tract (322) | Vertebrates |
| Encephalitozoon hellem | Human | 1991 | 78 | <50 | 3 | Eye, respiratory tract, urinary tract, systemic infection (322) | Birds |
| Encephalitozoon intestinalis (originally named Septata intestinalis) | Human | 1993 | 30, 139 | <200 | 2 | Intestine, biliary tract, respiratory tract, bone, skin, systemic infection (322) | Mammals |
| Encephalitozoon cuniculi | Rabbit | 1923 | 170 | <20 | —c | Systemic infection, eye, respiratory tract, urinary tract, liver, peritoneum, brain (322) | Mammals |
| Vittaforma corneae (originally named Nosema corneum) | Human | 1990 | 65, 258 | 1 | 3 | Eye, urinary tract (75, 101, 231) | Unknown |
| Vittaforma-liked | Human | 2003 | 278 | 22 | 3 | Intestine (278) | Unknown |
| Pleistophora ronneafiei (originally named Pleistophora sp.) | Human | 1985 | 32, 169 | 1e | — | Muscle (169) | Unknown |
| Trachipleistophora hominis | Human | 1996 | 145 | 1 | 1 | Muscle, eye (100, 231) | Unknown |
| Trachipleistophora anthropophthera | Human | 1998 | 305 | 3 | — | Systemic infection, eye (151, 335) | Unknown |
| Brachiola algerae (originally named Nosema algerae) | Mosquito | 1970 | 304 | 1f | 1 | Eye, muscle (61, 307) | Mosquito |
| Brachiola connori (originally named Nosema connori) | Human | 1974 | 33, 273 | 1g | — | Systemic infection (273) | Unknown |
| Brachiola vesicularum | Human | 1998 | 33 | 1 | — | Muscle (33) | Unknown |
| Nosema ocularum | Human | 1991 | 31 | — | 1 | Eye (31) | Unknown |
| Microsporidium ceylonensis | Human | 1973 | 11, 12, 36 | 1 (unknown) | Eye (12) | Unknown | |
| Microsporidium africanum | Human | 1981 | 223 | 1 (unknown) | Eye (223) | Unknown | |
HIV-seropositive persons, AIDS patients, and organ transplant recipients.
Immunocompetent, otherwise healthy.
Two patients with unknown immunostatus, presumably cellular immunodeficiency (see Table 4).
PCR/sequencing results only, needs confirmation.
Cellular immunodeficiency (HIV antibody negative).
Patient was taking immunosuppressive agents for rheumatoid arthritis for decades.
Thymic aplasia.
The most common microsporidial infections in humans are due to E. bieneusi and Encephalitozoon intestinalis. Both species have been found worldwide, mainly in HIV-infected patients with chronic diarrhea but also in immunocompetent persons with acute, self-limited diarrhea. Encephalitozoon cuniculi and Encephalitozoon hellem have been diagnosed, with very few exceptions, in immunocompromised patients and as causing local (e.g., ocular) or disseminated infections. Other rare microsporidial species infecting immunodeficient patients include Vittaforma corneae (formerly Nosema corneum), Pleistophora ronneafiei, Trachipleistophora spp., and Brachiola spp. Furthermore, V. corneae, Trachipleistophora hominis, Brachiola algerae, Nosema ocularum, Microsporidium ceylonensis, and Microsporidium africanum have been described in single cases as agents of ocular infections in immunocompetent persons.
Due to the administration of antiretroviral combination therapy, which restores immunity in HIV-infected persons, the number of clinically manifest microsporidial infections has markedly decreased in affluent countries (322). However, it is estimated that two-thirds of all HIV-infected persons live in sub-Saharan Africa, where antiretroviral therapy is not widely available due to the costs, and consequently, opportunistic complications continue to cause severe morbidity and mortality. Indeed, a recent study showed that 13% of HIV-positive diarrheic adults in Mali were positive for E. bieneusi, which thus was the most prevalent intestinal parasite in this African country (10). Furthermore, microsporidial infections are increasingly being diagnosed in affluent countries in immunosuppressed patients who undergo organ transplantation (39, 115, 119, 130, 132, 156, 167, 197, 200, 228, 229, 244, 260, 283), as well as causing ocular infections in nonimmunocompromised persons (47, 171, 206, 259, 274, 284).
Diagnostic Techniques
Considerable progress has been made in improving the repertoire of techniques for detection of microsporidia. Previously, diagnosis was based on laborious electron-microscopic examinations because of the small size of the organisms. The introduction of staining techniques allowed routine, light-microscopic diagnosis of microsporidial spores, at least to the genus level (319). Diagnosis to the species level is achieved by using antibodies (polyclonal or monoclonal) and by molecular methods based on the PCR (reviewed in references 116, 322, and 327). This latter sensitive and specific method has, in addition, the intrinsic advantage that upon further analysis of the PCR products with various methods (restriction fragment length polymorphism, SSCP, or sequencing), identification at the subspecies level (strains or genotypes) can be achieved (86, 154).
Serologic tests have been useful in detecting antibodies of E. cuniculi in several species of animals, but the value of detecting antibodies against Encephalitozoon spp. in humans has been controversial because of possible nonspecificity of the tests when spore walls are used as the antigen (322). By employing recombinant antigens of the polar tube of E. cuniculi, a high specificity was recently demonstrated, and the development of appropriate serodiagnostic tools seems feasible (298). No tests are available for the serodiagnosis of E. bieneusi.
Many but not all microsporidia infecting humans can be continuously cultivated in vitro in various cell lines (184, 306). This facilitates investigations of their basic biology (102, 127) and also allows for easy assessment of drugs (80) or disinfection schemes (118, 147, 150, 173), which has become an issue since human-pathogenic microsporidia have been discovered in surface waters (57, 89, 90, 103, 150, 255, 272).
Phylogeny
Investigations on the basic biology have unearthed highly exceptional characteristics of the microsporidia. Although they are true eukaryotes (i.e., they possess a typical eukaryotic nucleus, endomembrane system, and cytoskeleton), they also display molecular and cytological characteristics reminiscent of prokaryotes, including features of the translational apparatus, genome size (which is in the range of that of bacteria), and lack of recognizable mitochondria, peroxisomes, and typical Golgi membranes (reviewed in reference 189). Because of their prokaryotic features, microsporidia were initially classified within the Archezoa, together with other amitochondriate organisms (Giardia, trichomonads, and Entamoeba) which were thought to have evolved prior to the acquisition of mitochondria by endosymbiosis and consequently to represent the most primitive eukaryotes (42). However, the genome sequence of E. cuniculi revealed that it contains genes related to some mitochondrial functions, implying that microsporidia have retained a mitochondrion-derived organelle (152). Indeed, tiny organelles with double membranes could be demonstrated by using antibodies against a mitochondrial protein (Hsp70) in the human microsporidial parasite T. hominis (330).
Furthermore, sophisticated phylogenetic analyses revealed that the microsporidia evolved from within the fungi, being most closely related to the zygomycetes (43, 155). Microsporidia share additional features with fungi, e.g., the presence of chitin (although chitin is also found in other phyla, e.g., mollusks) and trehalose, similarities between the cell cycles, and the organization of certain genes (35, 211). Therefore, microsporidia are nowadays considered to be highly derived fungi that underwent substantial genetic and functional losses resulting in one of the smallest eukaryotic genomes described to date.
The placement of microsporidia among the fungi might have implications for the discovery of new therapeutic strategies. Although microsporidiosis in general can be successfully treated with albendazole and fumagillin, therapy for the most prevalent species, E. bieneusi, is difficult (129, 204). Indeed, a few studies have demonstrated that inhibitors of chitin synthase enzymes are effective against microsporidia (19, 270).
Natural History
A fundamental question that arose with the discovery of new microsporidial species in humans was that of their natural origin. The phylogram generated with small subunit ribosomal RNA (ssrRNA) gene sequences of microsporidia infecting humans (Fig. 2) illustrates their polyphyletic nature. Of particular interest is the fact that the closest relatives of three species infecting humans and belonging to the genera Trachipleistophora and Vittaforma are microsporidia that infect insects, and it is tempting to speculate that the insects might serve as reservoirs for these microsporidia. Indeed, another microsporidian of arthropod origin, Brachiola (formerly Nosema) algerae, was demonstrated to be a causative agent in human infections (61).
FIG. 2.
Dendrogram generated from the small subunit ribosomal RNA (ssrRNA) gene of microsporidian species identified in humans (underlined) and selected other species (Kimura's distance, unweighted pair group method of analysis). Known animal hosts are indicated in brackets; the brewer's yeast Saccharomyces cerevisiae serves as an outgroup. No corresponding gene sequences are known for the human-infecting microsporidian species Pleistophora ronneafiei, Trachipleistophora anthropophthera, Brachiola (formerly Nosema) connori, B. vesicularum, Nosema ocularum, Microsporidium ceylonensis, and M. africanum (Table 1).
The two new species of the genus Encephalitozoon, E. intestinalis and E. hellem, are very closely related to the widespread parasite of mammals E. cuniculi. The most prevalent species, E. bieneusi, is most closely related to a fish pathogen. For all four major microsporidial species infecting humans (E. bieneusi and the three Encephalitozoon spp.), animal hosts are known (Table 1; Fig. 2) implying a zoonotic nature of these parasites. Molecular studies have identified phenotypic and/or genetic variability within these species, indicating that they are not uniform. Whereas the significance of this variability remains largely unknown for E. hellem and E. intestinalis, strain variation in E. bieneusi and E. cuniculi provided new insights into the biology, origin and distribution of these parasites and has allowed the question of their zoonotic potential to be addressed.
ENTEROCYTOZOON BIENEUSI
There are two genera in the family Enterocytozoonidae: (i) Nucleospora, with the two characterized species N. salmonis, an intranuclear microsporidian of salmonid fish (87), and N. secunda, a parasite of a warm-water African fish (180), and (ii) Enterocytozoon, with E. bieneusi, infecting the cytoplasm of enterocytes and other epithelial cells in humans and mammals (76).
E. bieneusi, the most common microsporidial species known to cause human disease, was first described as an HIV-associated opportunistic intestinal pathogen in 1985 and was morphologically characterized using electron microscopy (76). In 1996, morphologically identical spores were detected in feces of pigs (74), and subsequently they also were detected in fecal samples and intestinal tissue of other mammals.
Infections in Humans
Several hundred HIV-infected patients with chronic diarrhea attributed to this organism have been reported from all over the world. The prevalence of E. bieneusi infections among HIV-infected patients reached up to 50% as documented by selected studies in Table 2. Human infections are well documented in all inhabited continents. In most studies, prevalences were significantly higher in patients with chronic diarrhea (92, 99, 128, 271, 324, 332). The prevalences presented in Table 2, however, do not allow for comparative analyses because there were considerable differences with regard to the selection of the patient groups, the patients' characteristics (age, sex, sociodemographic data, degree of immunodeficiency, and clinical features), and the specimens investigated (biopsies or stool samples). Furthermore, the improvements of diagnostic methods achieved over the last 15 years have to be considered.
TABLE 2.
Selected studies on prevalence rates of E. bieneusi in HIV-infected persons
| Geographic area | Specimen; diagnostic methoda | No. of patients examined; patients' characteristics | Prevalence (%) | Yr (reference[s]) |
|---|---|---|---|---|
| Africa | ||||
| Cameroon (Yaunde) | Stool; LM | 66; chronic diarrhea | 9b | 1997 (241) |
| Niger (Niame) | Stool; LM | 60; 41 with diarrhea | 7 | 1993 (27) |
| Zimbabwe (Harare) | Stool; LM | 129; hospitalized with diarrhea | 13 | 1995 (300) |
| Zimbabwe | Formalin-fixed stool; PCR | 74; 45 with diarrhea | 46 | 1997 (41) |
| Zambia (Lusaka) | Stool; LM | 69; chronic diarrhea | 23 | 1995 (91) |
| Mali (Bamako) | Stool; LM, partially confirmed by TEM | 88; 80% with chronic diarrhea | 32 | 1997 (185) |
| Tanzania | Stool; LM, TEM | 86; chronic diarrhea | 3 | 1999 (44) |
| Zimbabwe (Harare) | Stool; LM, PCR | 88; diarrhea longer than 1 week | 18 (LM), 51 (PCR) | 1999 (133) |
| Mali (Bamako) | Stool; LM, IFAT, PCR | 61; diarrhea | 13.1 | 2002 (10) |
| Americas | ||||
| United States (Washington, D.C.) | Intestinal biopsies; EM, TEM | 67; chronic unexplained diarrhea | 30 | 1990 (218) |
| United States (Texas) | Duodenal biopsies; TEM | 55; chronic diarrhea | 33 | 1993 (227) |
| 51; without chronic diarrhea | 25 | |||
| United States (Atlanta, Ga.) | Stool; LM | 65; diarrhea | 11 | 1993 (128) |
| 65; without diarrhea | 2 | |||
| United States (New York) | Intestinal biopsies; TEM | 34; AIDS patients | 44b | 1994 (160, 161) |
| 194; diarrhea | 39b | |||
| United States (New York) | Duodenal biopsies; PCR, confirmation by TEM | 68; diarrhea | 37 | 1996 (62) |
| 43; without diarrhoea | 2.3 | |||
| United States (California) | Stool; LM | 8,439; diarrhea, yr 1993, 1994, 1995, 1996. | 8.8, 9.7, 6.6, 2.9 | 1998 (53) |
| Brazil (Fortaleza) | Stool; LM | 79; with diarrhea | 6b | 1994 (332) |
| 82; without diarrhea | 1b | |||
| Brazil (Rio de Janeiro) | Stool; LM | 13; chronic unexplained diarrhea | 46b | 1996 (25) |
| Brazil (Rio de Janeiro) | Stools, duodenal or ileal biopsies | 40; chronic diarrhea | 27.5 | 2000 (24) |
| Peru (Lima) | Stool; LM | 2672; diarrhea | 3.9 | 2003 (275) |
| Australasia | ||||
| Australia (New South Wales) | Duodenal biopsies; LM | 109; chronic diarrhea | 29 | 1993 (99) |
| confirmed by EM | 71; without diarrhea | 1.4 | ||
| Australia (Victoria) | Stool; LM, TEM | 139; diarrhea | 3.5 | 1993 (239) |
| Thailand | Stool; LM, TEM | 66; chronic diarrhea | 33.3 | 1998 (313) |
| Thailand (Bangkok) | Stool; LM; TEM | 288; diarrhea | 11 | 2001 (317) |
| Thailand | Stool; LM, TEM | 95; children with diarrhea | 25.3 | 2002 (312) |
| India | Stool; LM | 120; diarrhea | 2.5 | 2002 (199) |
| Europe | ||||
| The Netherlands | Duodenal biopsies; LM partially confirmed by TEM | 55; unexplained diarrhea 38: without diarrhea | 27b 3b | 1991 (92) |
| The Netherlands | Stool; LM | 143; diarrhea | 7.7 | 1993 (301) |
| France | Duodenal biopsies; LM | 66; chronic diarrhea | 2 | 1993 (56) |
| France (Paris) | Stool, intestinal biopsies; LM | 18; chronic unexplained diarrhea | 50 | 1993 (203) |
| France (Nice) | Stool; LM | 46; chronic diarrhea | 24 | 1995 (16) |
| Italy (Apulia) | Stool; LM | 56; diarrhea | 2b | 1995 (187) |
| Italy | Intestinal biopsies; EM, TEM | 72; chronic diarrhea | 4.2 | 1996 (309) |
| Germany (Cologne) | Intestinal biopsies; PCR, Southern hybridization | 46; diarrhea | 22 | 1996 (110) |
| Germany (Hamburg) | Stool; LM | 50; diarrhea, hospitalized patients | 32 | 1998 (271) |
| 47; without diarrhea | 4 | |||
| England (London) | Intestinal biopsies; LM, EM | 59; diarrhea | 14b | 1991 (221) |
| England (northwest) | Stool, intestinal biopsies; LM confirmed by TEM | 63; diarrhea | 14 | 1995 (166) |
| Spain (Madrid) | Stool; LM, confirmation by PCR | 48 children; chronic diarrhea | 2 | 1997 (69) |
| Sweden (Stockholm) | Duodenal biopsies; LM | 72; abdominal symptoms of unknown cause | 3b | 1998 (281) |
| Switzerland | Stool; LM partially confirmed | 164; chronic diarrhea (1992-1994) | 10.7 | 1999 (324) |
| by TEM and PCR | 156; chronic diarrhea (1994-1996) | 5.3 | ||
| 949; without diarrhea | 0.4 | |||
| Portugal | Stool; LM, PCR | 215; diarrhea | 42.8c | 2001 (98) |
LM, light microscopy; TEM, transmission electron microscopy.
Intestinal microsporidia, species not stated.
A total of 92 samples were positive for microsporidia; 20 of 69 isolates that were further characterized by PCR were E. bieneusi, and 49 were E. intestinalis.
A few studies from affluent countries indicate that the prevalence of E. bieneusi in HIV-infected patients is decreasing (53, 324). Recent studies have shown that administration of antiretroviral combination therapy can result in remission of HIV-associated intestinal microsporidiosis (40, 54, 120, 198, 214). A decrease of 50% in E. bieneusi cases in Switzerland was also interpreted as being associated with antiretroviral therapy (324).
Although predominantly described among adults suffering from immunodeficiency due to HIV infection, E. bieneusi infections were also reported from HIV-negative patients who were immunocompromised due to an underlying disease or due to therapeutic immunosuppression when undergoing organ transplantation (119, 130, 197, 228, 229, 260, 318). Furthermore, a few E. bieneusi infections in HIV-negative, immunocompetent, and otherwise healthy persons that were associated with self-limited diarrhea were reported, mostly in the context of traveler's diarrhea in Europe (9, 71, 114, 181, 182, 209, 242, 268, 282, 314) but also in single cases in Africa (44, 131). Hence, E. bieneusi was detected by PCR in stool samples from 7 of 148 travelers with diarrhea returning to Germany (209). A recent study performed in Spain revealed that 8 of 47 (17%) geriatric persons with diarrhea were infected with E. bieneusi (182), and it was speculated that age-related diminishment of the immunological capacities might predispose elderly persons to microsporidial infections. On the other hand, no data so far indicate that children might be more susceptible to E. bieneusi infections (300).
Over the last decade, evidence has accumulated that E. bieneusi might also persist as an asymptomatic infection in immunocompetent humans. E. bieneusi was recovered in 8 of 990 stool samples from African children who were not considered HIV positive, suggesting enteric carriage among immunocompetent persons in tropical countries (27). Asymptomatic infections in children were reported in another study from Africa (44) and in a study from Asia, where not only healthy orphans (5.9%) but also child-care workers (1.9%) were infected (213). In all these studies, light microscopy, partly combined with transmission electron microscopy for confirmation of positive cases, was the diagnostic method, which might not be sensitive enough to detect subclinical infections under all circumstances. Therefore, more sensitive diagnostic tools such as PCR are required to elucidate the question of whether this parasite is a common organism of the human intestinal flora, causing severe disease only under immunodeficiency, or whether zoonotic transmission is of considerable importance (see below).
Infections in Animals
Eleven years after its discovery as a human pathogen, E. bieneusi was for the first time detected in animals, namely, in pigs (74), and a prevalence of 35% was determined by PCR in a subsequent investigation (26) of 109 randomly selected pigs from 22 farms located in different parts of Switzerland. A significantly (P ≤ 0.05) higher occurrence of E. bieneusi was found in weaned piglets. The feces of three infected pigs, which did not show any clinical signs, were examined weekly by PCR, revealing excretion of E. bieneusi spores in 67% of the samples. Hence, E. bieneusi seems to be a common parasite in asymptomatic pigs. The low pathogenicity of E. bieneusi for pigs was further substantiated by the lack of intestinal lesions in immunosuppressed and immunocompetent gnotobiotic piglets experimentally infected with E. bieneusi of human or macaque origin (159). This study, however, demonstrated that immunosuppression of piglets did lead to an increased excretion of spores.
Subsequent studies have confirmed the occurrence of E. bieneusi in pigs with high prevalence (32%) (29) and also in calves (9.5 to 11.5%) (237, 243, 277). The parasite has also been detected in cats (72, 191), dogs (182, 191), a goat (182), a llama (72), a variety of species of wild fur-bearing mammals (beavers, foxes, muskrats, otters, and raccoons) (72, 276), hedgehogs (A. Mathis, unpublished data), and, recently, nonmammalian hosts (chickens and pigeons) (233; M. Haro et al., unpublished data [GenBank accession number AY668953]).
Natural infections with E. bieneusi were documented in captive monkeys, namely, rhesus macaques. Prevalences were 16.7% (n = 131) in normal, asymptomatic animals, in which the infection persisted for 262 days, and 33.8% (n = 53) in animals which were experimentally infected with the simian immunodeficiency virus (186). A screening of 42 wild monkeys from Central Africa (Cameroon) by microscopy and PCR did not yield a single E. bieneusi-positive result (225).
Animal Models
For various reasons including mass production of the parasite for basic research, development of diagnostic tools, drug screening, and studies on disease pathogenesis, an animal model of enterocytozoonosis is desirable. E. bieneusi of human origin has been established in immunocompromised rhesus monkeys (126, 293), immunosuppressed gnotobiotic piglets (159), Sprague-Dawley rats (2), and New Zealand rabbits (3). In all animals, only chronic asymptomatic infections were observed, similar to the infections in naturally infected, immunocompetent pigs (26). Many attempts to establish E. bieneusi in immunocompetent and immunodeficient mice were unsuccessful (83). Hence, all hitherto-described experimental animal models appear not to be adequate to mimic the pathological intestinal situation in HIV-infected patients.
Molecular Epidemiology
Analyses of the single internal transcribed spacer of the rRNA genes (ITS) have revealed that there is considerable genetic variation within E. bieneusi isolates of human and animal origins, and more than 50 genotypes have so far been described based on subtle differences within this 243-bp sequence. An overview of human-infecting genotypes is provided in Table 3. In contrast to the situation with microsporidia of the genus Encephalitozoon (see below), no other genetic markers are available. However, classification of isolates of E. cuniculi and E. hellem based on ITS sequences has largely been confirmed by data for other genetic loci. Nevertheless, additional independent markers for E. bieneusi are highly desirable in order to clarify the genetic structure of the parasite's populations.
TABLE 3.
Enterocytozoon bieneusi genotypes in humans: number of described cases and animal hosts
| E. bieneusi genotype designation | No. of reported human cases (reference)
|
Animal host, genotype designation (reference[s]) | |
|---|---|---|---|
| HIV-infected or otherwise immunocompromised patients | Immunocompetent patients | ||
| Genotypes identified in independent studies | |||
| A | 3 (235), 3 (26), 1 (193), 32 (275) | ||
| B, I | 3 (235), 8 (26), 66 (174), 2 (193), 11 (240) | ||
| C, II | 2 (235), 2 (26), 1 (transplant recipient) (260), 9 (174), 7 (transplant recipient) (174), | 1 (174) | |
| 1 (lymphoma) (174), 1 (72) | |||
| D | 1 (236), 9 (275), 1 (240) | Macaque (45, 126); pig, EBITS9 (29); wildlife, WL8 (29, 45, 276) | |
| IV | 9 (174), 1 (transplant recipient), (174), 1 (myeloma) (174), 18 (275), 1 (240) | 1 (174), 10 (children with diarrhea, immunostatus not determined; estimated to be 18-29% among these children) (292) | Cat, K (72); cattle, BEB5 (72, 277) |
| Genotypes identified in single studies | |||
| Q (identical to C, II but with 2 nt insertion) | 1 (72) | ||
| III | 3 (174) | ||
| V | 1 (174) | ||
| Peru3 | 1 (275) | ||
| Peru4 | 1 (275) | Pig, EbpC (26); pig E (237); wildlife, WL13 (276) | |
| Peru5 | 3 (275) | Wildlife, WL11 (276) | |
| Peru6 | 1 (275) | ||
| Peru7 | 8 (275) | ||
| Peru8 | 4 (275) | ||
| Peru10 | 3 (275) | ||
| Peru11 | 6 (275) | ||
Five different ITS genotypes of E. bieneusi infecting humans have been confirmed in independent studies and another 12 were discovered in single studies, with one of these studies accounting for eight of these novel genotypes (275). Limited information is available on the geographic distribution of human-derived genotypes of E. bieneusi. Except for the above-mentioned eight genotypes identified in a study in South America (275), all other genotypes have been found in Europe, where most of the studies aiming at genotyping this parasite have been conducted (26, 72, 174, 235, 240). In additions, genotypes A, B, D, and IV have been identified in HIV-infected patients from South America and the United States (193, 275). In single studies from Asia and Africa, genotype A was found in 20 asymptomatic children in Thailand (I. Subrungruang et al., unpublished data [GenBank accession numbers AY357185 to AY357404]) and genotype IV in children with diarrhea in Uganda (292).
Of all 17 human-infecting E. bieneusi genotypes identified so far, four seem to have a zoonotic potential, as they have also been discovered in vertebrate hosts (Table 3). For the three genotypes A, B, and C, which account for the overwhelming number of isolates from humans, no animal host is known, and one might speculate that it is simply a matter of time until such hosts will be identified. On the other hand, several lines of evidence suggest that there is a certain degree of host specificity, at least for some of the E. bieneusi genotypes. First, a dendrogram based on ITS sequences of human-infecting E. bieneusi genotypes (confirmed in independent studies) and selected genotypes with animal hosts reveals a clustering of genotypes according to host species, although this grouping is not absolute (Fig. 3). Interestingly, the eight novel E. bieneusi genotypes recently identified in a single study of HIV patients (275) (Table 3) cluster within the branch containing all other human-derived genotypes (for a detailed dendrogram, see reference 275).
FIG. 3.
Dendrogram of ITS sequences of human-infecting E. bieneusi genotypes (confirmed in independent studies) and selected genotypes with animal hosts. All sequences are deposited in GenBank with the same designations (Kimura's distance, unweighted pair group method of analysis).
Further evidence for some degree of host specificity originates from experimental animal models using immunodeficient or immunosuppressed animals (see above). With E. bieneusi of human origin, only chronic asymptomatic infections which do not appropriately mimic the pathological intestinal situation in HIV-infected patients were observed in rhesus monkeys, rats, piglets, and rabbits (see above), and many attempts to establish human-derived E. bieneusi in immunodeficient mice were unsuccessful (83). A minor role of animals as sources of human infections is also substantiated by epidemiological data (see below).
Taken together, the picture of E. bieneusi with respect to its zoonotic potential is reminiscent of that of another intestinal parasite, Giardia lamblia, which comprises zoonotic as well as nonzoonotic genotypes (205).
Sources of Human Infections and Transmission
Extensive intestinal and rare respiratory tract involvement as described for patients with disseminated E. bieneusi infections suggest that different modes of transmission are possible, including the fecal-oral or oral-oral route, inhalation of aerosols, or ingestion of food contaminated with fecal material. In addition, direct human-to-human transmission is substantiated by studies that implicate male homosexuality or having an HIV-infected cohabitant as risk factors for acquiring intestinal microsporidiosis (148, 316). Person-to-person transmission was also suggested in a study which revealed that 9 of 13 infected orphans, who were HIV negative, were confined to two houses, whereas HIV-positive children inhabiting another house were not infected (213).
The detection of E. bieneusi in immunocompetent human carriers indicates that this parasite, or at least some of its genotypes, could naturally persist in the human population. Infections in organ transplant recipients or otherwise immunocompromised HIV-negative patients as well as in immunocompetent individuals were probably unrelated to direct contact with infected patients with AIDS.
No seasonal variation was obvious in the prevalence of human intestinal microsporidiosis in Brazil, as had been found for the intestinal parasite Cryptosporidium parvum (332). Despite differences in climate and sociodemographic factors, similar results were obtained in a study in southern California investigating 8,439 HIV-infected patients over a period of 4 years (53). In both studies it was suggested that contaminated drinking water was not likely to be the major source of microsporidial infections. However, other investigators have suggested that water contact may be an independent risk factor for enterocytozoonosis. In a prospective case-control study including 30 HIV-infected patients with intestinal microsporidiosis (28 with E. bieneusi infection and 2 with E. intestinalis infection) and 56 HIV-infected controls (148), “swimming in a pool” during the preceding 12 months was identified as one of three risk factors for intestinal microsporidiosis (besides male homosexuality and a CD4 lymphocyte count of ≤100/mm3). Other factors, such as consumption of different sorts of beverages or undercooked food, exposure to animals (cats, dogs, birds, bees, or fish), or recreational activities (swimming in freshwater or in the sea, trips abroad in the past 36 months, or visits to the countryside) were found not to be related to infection risk (148). Another study done in the United States included 12 HIV-infected patients with intestinal microsporidiosis and 54 CD4-matched controls. Risk factors for the acquisition of microsporidia were different kinds of water contacts (recreational swimming in rivers and lakes, drinking unfiltered tap water, or use of humidifiers) and close contact with another HIV-infected person (316). Lastly, a study investigating an urban cohort of HIV-infected patients revealed occupational contact with water or use of a hot tub or spa as risk factors for acquiring intestinal microsporidiosis (64), whereas contact with companion animals was not related to infection risk.
Infection risk associated with traveling was suggested for E. bieneusi infections of HIV-infected and noninfected travelers in one study (55) but not in another one (64). A comparative study on diarrheic HIV-infected patients from the Paris area (France), including 26 patients with intestinal microsporidial infection (species not determined) and 28 patients with cryptosporidiosis, revealed that trips to tropical countries were strongly associated only with microsporidial infections (55). It is not known whether particular factors are associated with microsporidial transmission in tropical countries where HIV-negative adult and children were found to be infected (27).
Detection of E. bieneusi and confirmation to the species level was achieved by PCR and subsequent sequence analysis of part of the ssrRNA gene in surface water but not in groundwater samples (89, 272) and recently, by species-specific PCR, also in zebra mussels from a river (123). Contamination of surface water may be from discharged domestic wastewater or from animal sources. As no genotyping was performed in these studies, the potential infection risk for humans from such sources needs further clarification.
ENCEPHALITOZOON
Three species of the genus Encephalitozoon have been identified as human pathogens: (i) E. cuniculi, which has a wide host range among mammals (37) and a worldwide distribution in domestic rabbits and is found in distinct geographic areas in carnivores and monkeys; (ii) E. hellem, which was distinguished from E. cuniculi in 1991 (78) and which has been reported in a few cases in avian hosts in the United States and Indonesia; and (iii) E. intestinalis (originally designated Septata intestinalis), which first was described in 1993 (30) and which was diagnosed in feces of farm animals in Mexico and in gorillas in Africa.
All three species have spores that are morphologically indistinguishable. Intraspecies genetic variation has so far been described for E. cuniculi and E. hellem. In E. cuniculi, three strains (I, II, and III) are recognized, which, according to the host of the originally characterized isolates, are also designated “rabbit strain,” “mouse strain,” and “dog strain.” The fourth known species from this genus, E. lacertae (37, 162), was identified in reptiles only and is most closely related to E. cuniculi.
ENCEPHALITOZOON CUNICULI
Infections in Humans
The first Encephalitozoon infection reported in humans, in 1959 (195), as well as a few subsequent cases were diagnosed based on spore morphology only. Therefore, these cases cannot unambiguously be attributed to E. cuniculi, as species differentiation was not possible at that time. Recent findings of E. cuniculi infections, as determined by immunological and/or molecular methods, in several patients (HIV infected, undergoing organ transplantation, or with idiopathic CD4+ T-lymphocytopenia) from Europe and from the United States prove the infectivity of E. cuniculi for immunodeficient humans (Table 4).
TABLE 4.
Single cases of human infections due to E. cuniculi confirmed by molecular analyses
| Immune status and country | Clinical manifestations | Site(s) of infection and/or specimen | E. cuniculi strain | Yr | Reference(s) |
|---|---|---|---|---|---|
| HIV-infected patients | |||||
| United Kingdom | Abdominal pain, anorexia, nausea, vomiting, fever, cough, renal failure | Kidney, urine | III | 1994 | 1, 141, 143 |
| United States | Fever, cough, emesis, insomnia, sinus congestion, severe dry eyes, blurred vision | Urine, sputum | III | 1995 | 63, 66, 85 |
| Germany | Keratoconjunctivitis, sinusitis, rhinitis | Urine, sputum stool, nasal discharge, duodenal biopsy | NDa | 1995 | 111 |
| Switzerland | Headache, visual impairment, cognitive impairment, nausea, vomiting | Cerebrospinal fluid, stool, sputum, urine | I | 1997 | 321 |
| United States | Dizziness, fever, nausea, abdominal pain, diarrhea | Adrenal glands, kidneys, brain, heart, trachea, urinary bladder, spleen, lymph nodes | III | 1997 | 196 |
| Switzerland | None | Urine | I | 1997 | 192 |
| Mexico | Pneumonitis, otitis media | Urine, respiratory specimen, stool | III | 1997 | 73, 192 |
| Switzerland | None | Urine | I | 1997 | 73, 192 |
| Switzerland | Conjunctivitis, sinusitis, seizure disorder | Urine | I | 1997 | 192 |
| Switzerland | Renal insufficiency, leucocyturia, erythrocyturia | Urine | I | 1997 | 192 |
| Switzerland | None | Urine, respiratory specimen | I | 1997 | 192 |
| Italy | Chronic sinusitis, bilateral keratoconjunctivitis | Nasal epithelium | I | 1998 | 238 |
| France | Visual impairment | Cerebrospinal fluid, urine, sputum, stool, duodenal biopsy | ND | 2000 | 105 |
| Chile | Cough, fever | Bronchoalveolar lavage, transbronchial biopsy | ND (IIIb) | 2001 | 328 |
| Spain | Fever, asthenia, abdominal pain, diarrhea | Stool, urine, sputum | III | 2001 | 68 |
| Italy | Fever, myalgia, poor general condition | Kidney, liver, lymph nodes, spleen, adrenal medulla, brain, ovary | III | 2002 | 288 |
| HIV-negative patients, immunocompromised (undergoing organ transplantation) | |||||
| Canada | Fever, keratoconjunctivitis, allograft tenderness, | Urine, stool, sputum, conjunctival scrapings | III | 2002 | 200 |
| Mexico | Cough, fever, diarrhea, thoracic pain, extreme weakness | Liver, kidney | III | 2003 | 115 |
| United States | Respiratory distress | Lung biopsy | III | 2004 | 283 |
| HIV-negative patients, otherwise immunocompromisedc | |||||
| Switzerland | Iris tumor | Tumor biopsy | I | 2005 | 158 |
ND, not determined.
E. cuniculi strain III deduced from clinical and epidemiological findings (see the text).
Idiopathic CD4+ T-lymphocytopenia.
In seroepidemiological studies with enzyme-linked immunosorbent assay (ELISA) and the indirect fluorescent-antibody test (IFAT) using spore antigens of E. cuniculi or parasite cell suspensions, prevalences of up to 42% have been reported for patients with a history of tropical diseases or a stay in tropical countries and for patients with renal diseases, psychiatric disorders, or neurological disorders (15, 142, 146, 261). Despite Western blot analysis, which potentially increases the specificity of the ELISA (146), it is uncertain whether detection of antibodies to E. cuniculi reflects true infections or antigen exposure without establishment of the parasite, cross-reactivity, or reactions due to polyclonal B-cell stimulation, particularly in patients with tropical diseases. More recent studies (50, 121, 135, 165, 224, 302) suffered from the same methodological limitations. However, all these serological studies suggest that human exposure to microsporidia may be common but without clinical significance. In a very recent serodiagnostic study of an immunocompetent laboratory worker who was accidentally infected with E. cuniculi when drops containing spores were spilled in his eyes, cross-reactivity of his serum with spore walls of E. hellem and E. intestinalis was demonstrated. However, only little cross-reactivity was observed when recombinant polar tube proteins of these parasites were used as antigens (298).
Infections in Animals
Beyond the numerous reports of E. cuniculi infections in rabbits, carnivores, and monkeys (see below), the parasite was identified as the causative agent of placentitis and abortion in a horse (220). Serological investigations (IFAT) revealed antibodies against E. cuniculi in goats and cattle (51, 136), but, as outlined above, the test specificity was not ascertained.
Rabbits.
Encephalitozoonosis in laboratory and pet rabbits is of clinical significance worldwide. E. cuniculi usually causes chronic infections which can persist asymptomatically for years. Severe neurological disease due to granulomatous encephalitis can occur unrelated to the age and sex of the animals (210) (Fig. 4). Until microsporidian-negative rabbit colonies were established, encephalitozoonosis was an important confounding variable in rabbit-based biomedical research on a variety of diseases (reviewed in reference 315).
FIG. 4.
Rabbit with torticollis (head tilt) due to cerebral infection with E. cuniculi.
In the past, high prevalences of encephalitozoonosis were recorded for laboratory rabbit colonies (37, 315), but these infections can be controlled by serological screening and high hygienic standards. On the other hand, the disease is still highly endemic in the pet rabbit population. In seroepidemiological surveys in Switzerland and the United Kingdom, specific antibodies against E. cuniculi spores were detected in 7.5% (n = 292) and 23% (n = 26) of healthy rabbits and in 85% (n = 72) and 71% (n = 65) of rabbits (mainly kept as pets) with neurological symptoms or with direct contact with symptomatic animals (74, 137, 210), respectively.
In rabbits, horizontal transmission by ingestion of spores is regarded to occur most frequently, but intrauterine infection has also been documented (13, 37). After experimental oral infections of rabbits, regular spore excretion in the urine was observed between days 38 and 63 postinfection and later intermittently at very low density (59). Spore excretion was reported in 9 of 11 symptomatic rabbits (60), indicating that such animals may play an important epidemiological role.
Based upon serological evidence, it was suggested that wild rabbits (Oryctolagus cuniculus) represent the natural host of E. cuniculi (331). Other studies revealed seroprevalences of 3.9% among 204 wild European rabbits in France (46) and 25% in the wild rabbit population in Western Australia (285). To our knowledge, E. cuniculi infections have so far not been reported for other free ranging lagomorphs.
Rodents.
E. cuniculi has been diagnosed in the past in numerous cases as a common parasite of laboratory rodents such as mice, rats, hamsters, and guinea pigs (reviewed in references 37 and 315), but nowadays, with high hygienic standards for the maintenance of laboratory rodents being applied, infections with microsporidia should no longer be a significant problem in these animals. On the other hand, rodent models have gained more attention for immunological research in the field of microsporidiosis (reviewed in reference 77).
Information about the possible significance of microsporidiosis in rodents kept as pet animals and about the epidemiology of microsporidiosis in wild rodents is scarce. Until 1986, only three reports of E. cuniculi infections in wild rats from Japan and the United Kingdom had been published (37). Recently, we isolated E. cuniculi strain II (“mouse strain”) from one of 30 wild rats (Rattus norvegicus) caught in the city of Zurich, Switzerland (212) (Table 5).
TABLE 5.
Hosts and geographical distribution of Encephalitozoon cuniculi strains
| E. cuniculi straina | Host | Geographic area (no. of isolates) | Reference(s) |
|---|---|---|---|
| I (“rabbit strain”) | Rabbit | Switzerland (21), United States (3), Germany (1), Australia (1), Italy (1), Japan (1) | 86, 113, 153, 192, 210; P. Deplazes and A. Mathis, unpublished data. |
| Human | Switzerland (6), Italy (1), United States (1) | 73, 238, 321, 334 | |
| II (“mouse strain”) | Mouse | Czech Republic (1), United Kingdom (1), United States (1) | 86, 334 |
| Wild rat | Switzerland (1) | 212 | |
| Blue fox | Norway (8), Finland (1) | 8, 190 | |
| III (“dog strain”) | Dog | United States (10), South Africa (1) | 86, 141, 264 |
| Prosimian |
As determined by the number of 5′-GTTT-3′ repeats in the ITS (86).
In wild mice, specific antibodies against E. cuniculi spores were found in Iceland in 4% and 9% of Apodemus sylvaticus and Mus musculus animals, respectively (140). The authors suggested that mice are a potential “reservoir” of E. cuniculi for arctic foxes and feral minks. Indeed, recent molecular characterization of E. cuniculi isolates from Norway and Finland (8, 190) revealed that all foxes originating from four different farms were infected with strain II (“mouse strain”) of E. cuniculi (see “Molecular Epidemiology” below).
Carnivores.
The clinical manifestation of canine encephalitozoonosis is an encephalitis-nephritis syndrome which had previously been confused with canine distemper (23). Encephalitozoonosis in domestic dogs, which is caused by strain III (“dog strain”) of E. cuniculi, has been described from Tanzania, South Africa, and the United States (23, 37, 252, 264).
In domestic cats, only three cases of E. cuniculi infections have been reported (37, 178). In captive carnivores, disseminated infections similar to those found in dogs occurred in fox cubs (215). This disease, which is still a major problem and causes heavy losses of blue foxes in northern European countries (5), is caused by strain II (“mouse strain”) of E. cuniculi (190).
Outbreaks of encephalitozoonosis in carnivores in zoos were previously reviewed (37). Few data are available about the disease in wild carnivores. Encephalitozoon-like organisms were detected by light microscopy in brain tissues from a wild hand-reared red fox (Vulpes vulpes) with neurological symptoms from the United Kingdom (331) and from captive wild dog (Lycaon pictus) pups which died of a fatal disease resembling canine distemper 13 days after vaccination with a live attenuated strain of canine distemper virus (303). Serological investigations with ELISA revealed no seropositive animals in 86 wild red foxes from Switzerland (210). In Iceland, seroprevalences were 12% among 372 wild arctic foxes (Alopex lagopus) and 8% in feral mink (Mustela vison) (140). Histopathological findings for a seropositive fox pup with a neurological disorder which died 2 days after capture were consistent with encephalitozoonosis described for farmed foxes. The authors suggested that encephalitozoonosis contributed to the decline of the arctic fox population size by depressing fetal and pup survival and that mice may represent a potential reservoir for microsporidia (140). Indeed, in Greenland, where rodents are absent from the diet of these arctic foxes, none of 230 foxes investigated had antibodies to E. cuniculi (7).
In all mentioned reports of encephalitozoonosis in wild carnivores (140, 303, 331), Encephalitozoon-like organisms were detected by light microscopy only. Therefore, species and strain determinations were not conclusive.
In dogs and foxes, encephalitozoonosis is being perpetuated in the population by horizontal and vertical transmission (23, 201). Dogs and foxes infected by ingestion of spores showed moderate clinical symptoms, and the chronically infected animals represented the main source of infections for the offspring. In fur farms, food contaminated with spores from infected rodents or rabbits was assumed to be a possible source of infection for foxes and minks (140, 215).
Monkeys.
Disseminated natural infections resulting in high morbidity and severe encephalitis caused by Encephalitozoon-like organism have been reported for stillborn and young squirrel monkeys (Saimiri sciureus) in the United States (28, 337). Although parasite identification was based on electron microscopy only, which does not allow one to distinguish E. cuniculi from E. hellem, the neuropathological symptoms strongly suggested that E. cuniculi was the species involved. Only recently, strain III (“dog strain”) of E. cuniculi was identified in tamarin colonies (Saguinus imperator, Oedipomidas oedipus, and Leontopithecus rosalia rosalia) in two zoos in Europe, causing severe disseminated infection with high mortality in infants (134, 234, 329).
In experimental infections of vervet monkeys with dog-derived E. cuniculi isolates, transmission from infected infants to their nursing dams as well as transplacental transmission was established (297). In naturally infected monkeys, transplacental transmission was shown by the presence of multifocal granulomatous encephalitis with invasion of the brain by Encephalitozoon in stillborn monkeys or monkeys only a few days old, as well as by the reported placentitis in an animal and the isolation of Encephalitozoon-like parasites from placental tissue of a baboon (reviewed in reference 37). The hypothesis that animals with silent infections can perpetuate the disease in a colony is supported by a serological survey of a squirrel monkey colony over 3 years. More than half of these 250 animals tested positive at least once, and asymptomatic young animals were also seropositive (251). Export of such seropositive asymptomatic animals represents a high risk for the introduction of the parasite in other colonies, as was recently observed in an Emperor tamarin colony in Europe (134). So far, no sources of infection have been elucidated for E. cuniculi infections in monkeys, and it is not known whether this microsporidial species is prevalent in free-living monkeys.
In contrast to natural infections causing neonatal death or lethal infections in young monkeys, experimental infections of immunocompetent monkeys with dog- or rabbit-derived isolates resulted in asymptomatic infections (84, 254, 297). Therefore, many factors, including host species, E. cuniculi strain, age and immune status of the host, and mode of transmission (e.g., intrauterine or oral), may influence the outcome of infections in monkeys.
Molecular Epidemiology
In E. cuniculi, the existence of three strains (I, II, and III; also named “rabbit strain,” “mouse strain,” and “dog strain”) was established using immunological and molecular methods (86). The repeated element 5′-GTTT-3′ in the ITS is a reliable and widely used genetic marker: strain I contains three such repeats, strain II contains two repeats, and strain III contains four repeats. A recent multilocus analysis yielded additional markers for the three strains, namely, the genes coding for the polar tube protein and spore wall protein 1 (333). This strain differentiation helped to elucidate the complex epidemiological situation of E. cuniculi infections in different hosts and in different parts of the world.
Table 5 shows the host species and the geographical origins of those E. cuniculi isolates which were determined to the strain level and for which comprehensive information about the host animal was available. These data confirm earlier observations which suggested from circumstantial evidence that different strains of E. cuniculi with different host preferences might exist in nature (reviewed in reference 37). Strain II (“mouse strain”) was identified in rodents (mouse and rat) and in farmed blue foxes, supporting the hypothesis that mice are a reservoir of E. cuniculi for blue foxes (140). All E. cuniculi isolates from rabbits characterized so far belong to strain I (“rabbit strain”), and all isolates from dogs belong to strain III (“dog strain”).
Dogs indeed seem to be susceptible to strain III only. In Switzerland, where strain I (“rabbit strain”) is highly prevalent in the rabbit population (210) and strain II (“mouse strain”) was detected in a rat (212), no positive antibody reactions were detected by ELISA in 104 healthy dogs and in 108 dogs with neurological disorders (210). E. cuniculi strain II is known to have a remarkable pathogenicity for the blue fox and mink in Norway (6, 37), but encephalitozoonosis of dogs has not been reported from Norway, and a recent serological survey with 1,104 canine serum samples revealed no indications for an infection (6). The absence of canine encephalitozoonosis in Europe indicates that strains I and II of E. cuniculi do not play a significant role as pathogens in the dog population.
Host preference of the strains is further substantiated by the observations that strain II (“mouse strain”) was recently identified from a wild rat in an area in Switzerland (212) where strain I (“rabbit strain”) of E. cuniculi is highly endemic in pet rabbits and that, vice versa, a considerable number of rabbits from all over Switzerland all were infected with strain I but never with strain II. It is unlikely that strains I and II simply are epidemiologically separated, as E. cuniculi-positive rabbits were identified from stables where rodents were freely roaming.
On the other hand, a strict host specificity of the strains was not demonstrated under experimental conditions (reviewed in reference 192). E. cuniculi strains II (“mouse strain”) and III (“dog strain”), for example, were also infective to rabbits that were given spores from an in vitro culture by oral administration (192; P. Deplazes, unpublished data).
The strains of E. cuniculi seem to differ in their geographical distributions. Hence, strain II has so far been identified in Europe only, strain I infects rabbits from at least three continents (America, Australia, and Europe), and strain III was identified in dogs in America and South Africa. Strain III was recently identified for the first time in Europe in tamarin colonies from zoos (134, 234, 329). However, it was suggested in one of these cases that this infection had been imported with ancestor animals originating from the United States and has been perpetuated in the population by transplacental infections (134). A potential for spreading of this imported strain to the autochthonous carnivore population in the future has to be considered.
Immunocompromised humans were found to be infected with strain I (“rabbit strain”) in Europe and with strain III (“dog strain”) in the Americas (Table 5). In Europe, too, several HIV-infected patients were diagnosed to be infected with E. cuniculi strain III (Table 4), but no travel histories for these patients were provided.
Sources of Human Infections and Transmission
It is unlikely that E. cuniculi is a natural pathogen in humans, and its zoonotic origin is evident. Indeed did two of the six patients from Switzerland, all of whom were infected with E. cuniculi strain I (“rabbit strain”), recall exposure to rabbits in the past (192, 321). Two patients from the United States who were infected with strain III (“dog strain”) did own a pet dog, but microsporidial infection in the animals was not proven (85, 283). Seroconversion in one of three children exposed to puppies with overt encephalitozoonosis has been reported (79). In another case of an E. cuniculi infection in an HIV-infected person where no material was available for genotyping, strain III (“dog strain”) was suspected to be the causative agent based on geographical (Chile) and clinical reasons and on the fact that the patient had a high risk of exposure as she was working as a pet dog groomer (328). Patient-to-patient transmission was considered to be unlikely in the only study to date investigating several patients, because these patients neither knew each other nor had obvious personal contacts such as hospitalization at the same time (73, 192).
As spores of E. cuniculi are highly resistant in the environment and can survive several months under humid conditions (172, 311) direct contact with infected animals or humans is not required, and waterborne infections seem feasible. However, none of the two E. cuniculi strains found in humans have so far been detected in surface waters, in contrast to the case for strain II (“mouse strain”), which in a single study was identified by PCR in one of a total 50 samples from Switzerland (A. Mathis, unpublished data).
ENCEPHALITOZOON HELLEM
Infections in Humans
E. hellem has so far been diagnosed in around 50 HIV-infected persons in a relatively few countries: Most cases were reported from the United States (52, 78, 81, 248-250, 308). E. hellem was diagnosed in European patients from Italy (247), Switzerland (73, 109, 323), Germany (109), and the United Kingdom (144) and in one case in Africa (Tanzania) (75).
It is not clear whether epidemiological factors are responsible for a restricted distribution of this microsporidian or whether the relatively difficult identification of this species by immunological or molecular methods hampers its detection. E. hellem causes disseminated and ocular infections in HIV-positive patients, but asymptomatic infections of the respiratory tract have also been described (245). To our knowledge, E. hellem has so far been identified on two occasions in nonimmunosuppressed and HIV-seronegative patients, namely, from bronchoalveolar lavage of a patient with a simultaneous Mycobacterium tuberculosis coinfection (246) and in fecal samples from two diarrheic travelers returning from Singapore, who were coinfected with E. bieneusi (209) as diagnosed by PCR and confirmed by sequencing.
Infections in Animals
Before the description of E. hellem in 1991 (78), Encephalitozoon-like microsporidia were described on several occasions from psittacine birds (parrots). With the exception of a peach-faced lovebird from Australia, all cases were from birds kept in aviaries in the United States (37, 216, 230). Molecular analyses recently allowed identification of E. hellem in psittacine birds in the United States as the etiological agent of lethal infections in budgerigar chicks (Melopsittacus undulatus) in an aviary (20), in tissues from two eclectus parrots (Eclectus roratus) (226), and in droppings of a clinically normal peach-faced lovebird (Agapornis roseicollis) (267). The first detection of E. hellem in a wild psittacine bird was demonstrated by molecular analyses of spores from the intestinal contents of a yellow-streaked lory (Chalopsitta scintillata) captured on Aru Island (Indonesia) (279). However, microsporidial infections have been reported from nonpsittacine birds in the last few years. Horned puffin (Fratercula corniculata) chicks, which were caught in Alaska and which suffered a high mortality rate in quarantine at a zoo, were found to be infected with nonspecified microsporidian-like organisms (287). An intestinal microsporidiosis was diagnosed postmortem in a clinically normal ostrich (Struthio camelus) in Texas (125), and the causative agent was identified as E. hellem (263). Several species of wild, migratory hummingbirds from California, which suffered from enteritis, were infected with E. hellem (262). Finally, the parasite was diagnosed in a Gouldian finch from a flock with high nestling mortalities in Australia (38). A single epidemiological survey reported a prevalence of 25% of 198 clinically normal lovebirds from three flocks (265).
Experimental inoculations have resulted in disseminated infections in athymic nude mice (266). In an attempt to assess whether avian species with close contacts with humans can serve as hosts of E. hellem, young chickens and turkey poults (3 to 5 days of age) were inoculated by gastric gavage with 107 spores (97). All birds remained asymptomatic, and no microsporidia were detected by microscopy in fecal smears and in histological specimens of the intestine. However, PCR, which was shown to be considerably more sensitive for detection of microsporidia in feces than microscopy (96), was positive with fecal material from chicks only. Taken together, these results suggest that several avian species might serve as asymptomatic carriers of E. hellem.
The means of transmission of E. hellem infections in birds remain unexplored. As spores were found in kidney and intestine, spore excretion probably occurs with feces (20, 37, 216, 279). Black and colleagues (20) observed severe outbreaks of encephalitozoonosis with high mortality in young chicks, whereas adult birds in the same aviary appeared unaffected. In several reports, avian microsporidiosis leading to high morbidity and mortality was observed shortly after birds were brought into a new environment (37, 279, 287). These observations suggest that latent infections as observed with E. cuniculi in other animals also occur in adult birds and that the stress of translocation may reduce the degree of resistance to this infection. Immunosuppressive viral infections such as that with the psittacine beak and feather disease virus were found in two unrelated cases of lethal microsporidiosis in eclectus parrots (226), and a significant correlation was identified between shedding of E. hellem spores and psittacine beak and feather disease virus infection of lovebirds (265).
Molecular Epidemiology
Comparable to the situation in E. cuniculi, different genotypes as assessed by the sequence of the ITS were identified in E. hellem (194). Genotype 1, which represents the overwhelming number of E. hellem isolates characterized so far, was determined for isolates from several patients from the United States (153, 310, 333) and from Europe (109, 333) and for one E. hellem isolate each from a parrot caught in the wild in Indonesia (279) and from a psittacine bird from the United States (267). Genotypes 2 and 3 (194) and 2b (333), which differ from each other only by short insertions, consist of human-derived E. hellem isolates from Switzerland (three isolates) and Tanzania (one isolate) (194, 333). Differences among the E. hellem genotypes were also detected by Western blot analysis, but there was no absolute match between genotype and antigen profile. Indeed, karyotyping (17, 70) and multilocus analyses targeting coding (polar tube protein gene and ssrRNA gene) and noncoding (intergenic spacer) loci identified a least six different human-derived genotypes (138, 222, 333). From all these analyses, it appears that E. hellem isolates from the United States and from Europe are different populations. No isolates from birds have as yet been subjected to this more detailed genetic analysis; therefore, the biological and epidemiological significance of these findings remains to be elucidated.
Sources of Human Infections and Transmission
To our knowledge no epidemiological studies to demonstrate risk factors for E. hellem infections have been conducted, and the parasite has never been identified in surface waters. However, it is worth noting that some patients with ocular microsporidiosis owned or were exposed to pet birds (112, 219, 336). The identification of E. hellem as etiological cause of severe renal and intestinal infections in parrots and the excretion of spores in feces indicate that birds are a potential, but yet unproven, source of zoonotic infections. Once introduced into a susceptible human population, transmission of spores from person to person might be of importance. In HIV-infected patients with disseminated E. hellem infections, spores were isolated from sputum, nasal secretions, sinus aspirate, and urine (219, 323). The occurrence of upper and lower respiratory tract infections suggests that this species can be transmitted via the aerosol route (248, 323). Furthermore, oral or ocular autoinoculation, perhaps by contaminated fingers, may occur (249). For drug addicts, a hematogenous mode of transmission with contaminated syringes has been suggested but was not proven (117).
ENCEPHALITOZOON INTESTINALIS
Infections in Humans
E. intestinalis is the second most prevalent microsporidial species infecting humans. Infections in HIV-positive patients have been reported from the Americas (62, 208, 257), from Europe (21, 98, 107, 175, 177, 202, 271, 280, 299, 325), from Australia (88, 168, 208), and from Africa (10, 122, 157, 167). Most reports are descriptions of single case; in a few studies larger groups were examined, and prevalences for E. intestinalis were 7.3% for 68 AIDS patients with diarrhea from the United States (62), 2% for 97 consecutive HIV-infected patients in Germany (271), 3% for 75 patients with chronic diarrhea from Zambia (157), and 0.9% for 320 patients with chronic diarrhea in Switzerland (324). A study investigating 216 AIDS patients with gastrointestinal complaints in Portugal revealed 92 patients being positive for microsporidia by microscopy (trichrome stain, uvitex, and calcofluor; prevalence, 42.8%). Of the positive specimens, 69 were further investigated by species-specific PCR, resulting in the diagnosis of E. intestinalis in 49 of them and of E. bieneusi in 20 (98). When 63 stool samples from HIV-infected patients with diarrhea from England were investigated by the calcofluor method, no E. intestinalis infections were found, whereas in 9 samples (14.3%) E. bieneusi was detected (166). Similarly, no E. intestinalis infections were detected in 61 HIV-positive persons from Mali (Africa) by using a monoclonal antibody, but 8 (13.1%) were positive for E. bieneusi (10).
Two studies have proposed that double infections with E. bieneusi and E. intestinalis might occur. Five such double infections were identified in 10 cases of E. intestinalis infections in AIDS patients as proven by PCR on biopsy material (109). van Gool and colleagues (299), when attempting to cultivate E. bieneusi from four stool samples from biopsy-proven patients, surprisingly ended up with cultures of E. intestinalis in all four cases. They suggested that this microsporidian might be more common than suspected; however, laboratory contamination of the cultures cannot be excluded.
E. intestinalis had been identified in two HIV-negative travelers with diarrhea (232). In a cross-sectional survey of two rural villages in Mexico, a monoclonal antibody (3B6) which recognizes E. intestinalis, E. hellem, E. cuniculi, and the other microsporidial species Nosema and Vairimorpha spp., but neither Enterocytozoon bieneusi nor yeast from stool sample (93), was used to investigate 255 persons. Twenty (7.8%) of them were positive, with 21% of 70 households having at least one member who was positive (94). Indications for high prevalences in immunocompetent persons were also found in another study (302). Using serologic techniques with E. intestinalis as antigens, high seroprevalences among 300 Dutch blood donors (8%) and 276 pregnant French women (5%) were found. However, the tests used were not strictly specific for E. intestinalis but presumably were genus specific.
Infections in Animals
Experimentally infected wild-type mice were shown to excrete spores intermittently and in low numbers (4), a situation that is reminiscent of the one with E. bieneusi infections in pigs (26). In a survey using the monoclonal antibody 3B6 (which is not E. intestinalis specific; see above) in IFAT, fecal samples from domestic animals from a rural area in central Mexico were investigated, resulting in 19 (11%) of 172 mammalian and 16 of 99 avian samples being positive. Transmission electron microscopy on specimens from mammals revealed microsporidian-like structures. PCR using a contamination-prone protocol (with a cloned E. intestinalis target sequence as positive control) was done several months later on total DNA extracted from the formalin-fixed specimens, which generally is considered not to be suitable for sensitive detection due to time-dependent, formalin-induced degradation of DNA (149, 291). Six of the eight investigated fecal samples from goat, pig, cow, dog, and donkey were positive for E. intestinalis but negative when tested with primers specific for E. cuniculi and E. hellem (22).
Such a high prevalence in animals has not been confirmed in other studies. In a recent study, by employing microscopy and PCR on nonfixed material, low prevalences (3%) of E. intestinalis were identified in free-ranging gorillas and in people who share gorilla habitats in Uganda (122). Hence, a zoonotic potential was suggested, but further studies are needed to investigate whether E. intestinalis indeed is a common pathogen of a wide variety of (domestic) animals and whether animal-borne E. intestinalis is epidemiologically related to the human disease.
Molecular Epidemiology
In contrast to the situation in other human-infecting Encephalitozoon species, for which distinct strains with differences in their biology and epidemiology were identified, E. intestinalis seems to be a very homogenous species. Analysis of five human-derived isolates revealed only minor differences in sodium dodecyl sulfate-polyacrylamide gel electrophoresis and Western blot profiles (67). Whereas isolates from both E. cuniculi and E. hellem show considerable intraspecies variability in their karyotypes (17, 18, 70, 269), isolates of E. intestinalis displayed identical karyotypes when analyzed by pulsed-field gel electrophoresis (17). No variation of the ITS sequences was detected in 16 isolates of E. intestinalis (82, 176).
Sources of Human Infections and Transmission
Modes of transmission of E. intestinalis spores are uncertain. Considering the various sites of infections (intestinal, respiratory, and ocular) (108) and spore release into the environment via stool, transmission via the fecal-oral route, by inhalation, or by contaminated fingers seems plausible. Waterborne infection, at least focally, can be suspected, as the parasite was identified by sequence analysis of PCR amplicons from surface water and groundwater (89, 286), from 6 of 12 investigated samples of source water used for consumption (90), and recently, by species-specific PCR, also in zebra mussels from a river (123). Case-control studies indeed demonstrated that contact with water might be a risk factor for acquiring intestinal microsporidiosis (E. bieneusi and E. intestinalis), but either microsporidial species were not specified or E. bieneusi was the predominant one (see “E. bieneusi: Sources of Human Infections and Transmission” above).
OTHER MICROSPORIDIA
Several microsporidial species have been identified in rare cases of patients with ocular infections, myopathies, intestinal infections, or disseminated infections (Table 1). We briefly discuss the features of those microsporidia for which ultrastructural and/or molecular information is available. With the exception of B. algerae, which infects mosquitoes, no host other than humans is known for these species.
Vittaforma spp.
Vittaforma corneae (258), which originally was designated Nosema corneum (253), was the first human-derived microsporidial isolate which could be established in an in vitro culture. Up to now, four cases of human infections are on record, three of them related to eye infections in immunocompetent patients from the United States and Europe (101, 231, 253) and one presenting as an urinary tract infection in a patient with AIDS living in Africa, who had a concurrent infection with E. hellem (75). Phylogenetic analysis based on rRNA gene sequences (Fig. 2) revealed arthropod-infecting species as being most closely related to V. corneae and the human-infecting E. bieneusi as a close taxonomic relative. Although no common natural hosts of Vittaforma have yet been identified, these microsporidia seem to be ubiquitous. Investigations of surface waters in the United States and in Europe by PCR and sequencing revealed gene sequences with highest scores of identity (91 to 98%) with V. corneae in, e.g., seven of eight samples analyzed (89, 104). The Vittaforma-like organisms (96% identity with V. cornea) identified in feces from 25 diarrheic patients (22 HIV positive and 3 HIV negative) in Portugal (278) might therefore simply reflect intestinal passages of microsporidial spores.
Pleistophora spp.
Three cases of myositis in immunodeficient patients were identified as being caused by Pleistophora spp. (49, 124, 169). The correct taxonomic position of the organisms in two of the cases (49, 124) was not possible but it was assumed (48) that they belong to the subsequently described genus Trachipleistophora (see below). Ultrastructural analysis of the third isolate (169) allowed its classification as the new species Pleistophora ronneafiei (32).
Pleistophora spp. have nearly exclusively lower (poikilothermic) vertebrate hosts, in particular fish and reptiles, but no other Pleistophora species has spores with the dimensions of P. ronneafiei, and hence a possible animal reservoir remains obscure.
Trachipleistophora spp.
Closer examination of a morphologically Pleistophora-like microsporidian isolated from an patient with AIDS with infection of skeletal muscle and also the nasal sinus cavities and conjunctiva (100) led to the establishment of the new genus and species Trachipleistophora hominis (145). Apart from this first case from Australia, T. hominis was identified in an immunocompetent African immigrant in the United Kingdom as causal agent of a stromal keratitis (231).
Phylogenetic analysis of T. hominis based on rRNA gene sequences revealed that its closest relationship is with species of the genus Vavraia, which are pathogenic to insects (48) (Fig. 2). T. hominis indeed could be readily propagated in mosquito larvae, and the spores produced were again infective for athymic mice. Furthermore, spores were transferred from infected adult mosquitoes to a feeding substrate (326). Insects being a potential source of T. hominis was substantiated by experimental infections of severe combined immunodeficient (SCID) mice. Whereas oral inoculation was ineffective for establishing an infection, injection of the parasites, mimicking insect stings, led to disseminated infections, including infection of urinary bladder, liver, and spleen but not the brain (163). Severe ocular and milder disseminated infections were also observed upon eye contamination with spores, providing a direct way of infection independent of insect bites.
A second species of this genus, Trachipleistophora anthropophthera, was differentiated based on ultrastructural features and clinical syndromes (305). In contrast to T. hominis infections in humans and in SCID mice, T. anthropophthera also infected the brain, as was reported for the first two infections in AIDS patients from the United States (335). This microsporidial species was identified in a single additional human case in an HIV-infected person from Thailand suffering from chronic keratitis, and the isolate was successfully cultivated in mouse fibroblast cells (151).
No genetic information allowing phylogenetic analysis is available for T. anthropophthera. Based on the common characteristic feature of bisporous sprorophorous vesicles, it was suggested that this species might be related to the genus Telomyxa, which infects insects (mayflies) (289).
Brachiola spp.
Brachiola algerae (183) (formerly Nosema algerae) is has long been known as a pathogen of different orders of insects, e.g., mosquitoes (304), and was a candidate agent for biological control of these insects (296). Within this context, it was evaluated in the 1970s whether B. algerae could pose a biohazard for mammalians when injected by a mosquito during a blood meal. Later, during the AIDS pandemic and before the first case of a human infection with this parasite was reported (307), the potential of B. algerae to infect immunocompromised vertebrates was assessed. Hence, this microsporidial species was shown to proliferate in mammalian cell lines, initially only at temperatures of below 37°C (294) but later also after adaptation to 37°C (207, 289). Intravenous injection of spores failed to induce infections in immunocompetent and immunocompromised mice, and subcutaneous injections led to limited development close to the infection site in extremities only (290, 295). Furthermore, ocular, but not oral, intraperitoneal, intramuscular, or subcutaneous, inoculation of SCID mice with spores of B. algerae led to severe infection of the liver as the only affected internal organ (164). It was concluded that an initial infection of the eye allowed the parasite to adapt to the conditions within the mammalian host and to spread to internal organs, presumably via macrophages.
In the first case of a human B. algerae infection, the parasite was isolated from the cornea of an immunocompetent patient (307), and the infection was resolved after appropriate treatment. In the second case (61), a deep-tissue infection in muscles in a patient with diabetes and rheumatoid arthritis was documented. The patient, who was HIV negative and who eventually died from a massive cerebrovascular infarcation, was taking immunosuppressive agents for rheumatoid arthritis. Diagnosis from muscle biopsies was confirmed by light and electron microscopy, by IFAT using rabbit antiserum against B. algerae, and by PCR and sequencing. Rather perplexing is the finding that the parasite isolate proliferated in RK13 (rabbit kidney) cells in vitro at 30°C but not at 37°C, a fact that was not further discussed by the authors.
Two further species of the genus Brachiola have been described based on ultrastructural features from single human infections: B. connori (33) (originally named Nosema connori [273]), causing disseminated infection in an immunologically compromised child (188, 273), and B. vesicularum, causing myositis in an AIDS patient (33). The validity of the latter species name was doubted, and it was suggested that B. vesicularum, for which no genetic information was provided, may be identical to B. algerae based on the ultrastructure of B. algerae when growing in human muscle fibroblasts at 38°C (289). However, examination of muscle biopsies from the above-mentioned B. algerae case (61) confirmed the existence of ultrastructural differences, implying that B. algerae and B. vesicularum indeed are different species (34).
Microsporidium spp.
Microsporidium ceylonensis.
In the original case report (12) of this ocular infection of a Tamil boy, spores were the only parasite stages identified, and it was suggested that either E. cuniculi, which had been confirmed as a human pathogen at that time (195), or Nosema helminthorum was the causative agent. The latter species, a parasite of tapeworms of goats, was suggested because the boy had suffered an injury of the affected eye when he had been gored by a goat. In a subsequent ultrastructural study published in 1998 (36), a generic classification of this isolate could not be achieved and it was named Microsporidium ceylonensis. The ultrastructural details identified should facilitate the recognition of this parasite in future cases.
Microsporidium africanum.
Microsporidial spores were identified in histiocystes of a corneal ulcer of an African woman (223), with a tentative identification as a Nosema sp. The isolate was later transferred to the collective group Microsporidium upon reexamination of the electron micrographs and was designated Microsporidium africanum (37). There are no clues whatsoever on other hosts of this species.
CONCLUDING REMARKS
Microsporidia are identified as parasitic organisms of almost every animal group, including numerous invertebrates and vertebrates. In humans, fewer than 10 human infections were reported until microsporidia had emerged as important opportunistic pathogens when AIDS became pandemic. Meanwhile, their significance has dramatically decreased in areas where antiretroviral combination therapy is available, but the prevalence of opportunistic infections in HIV-infected patients remains still high or is increasing in resource-poor countries. In affluent countries, the focus has shifted to microsporidial infections in otherwise immunocompromised patients, particularly organ transplant recipients, and in immunocompetent persons with cornea infection. Human microsporidial infections might be underdiagnosed due to the difficulties of detection.
The sources of most microsporidia infecting humans and modes of transmission are still uncertain. Because microsporidial spores are released into the environment via stool, urine, and respiratory secretions, possible sources of infection may be persons or animals infected with microsporidia. Furthermore, because some microsporidia infecting humans are morphologically identical to organisms known in animal reservoirs, the question arose as to whether these intracellular parasites are of zoonotic origin. Molecular techniques have been applied to address this question, but at present, conclusive results are available for only a few microsporidial species.
Using genetic analyses, the zoonotic potential has clearly been documented for several Encephalitozoon species including E. cuniculi and E. intestinalis, which infects mammals and humans, as well as E. hellem, which infects birds and humans. Epidemiological evidence, however, is lacking because the number of reported human infections is still low.
Most animal and human isolates of E. bieneusi, the most prevalent human microsporidian, causing mainly severe and chronic HIV-associated diarrhea, are genetically distinct. Nevertheless, identical E. bieneusi genotypes were found in mammals and in a few human patients, suggesting that zoonotic transmission is possible. The molecular results strongly support the hypothesis that most human-infecting E. bieneusi genotypes are “human adapted” and not zoonotic.
Because other microsporidial species are only very rarely found even in severely immunocompromised humans, it appears likely that humans do not represent a major parasite reservoir. Although the natural hosts have not been found yet for several of these rare human pathogens, an arthropod or fish host reservoir might be considered.
Ingestion of microsporidial spores is the most probable mode of acquisition, and it is assumed that infection is most likely transmitted either directly from human to human via the fecal-oral route or indirectly via water or food. Although some epidemiological studies indicated the possibility of human-to-human or waterborne infections, convincing epidemiological results are still lacking. Transmission by the aerosol route has also been considered, because spores have been found in respiratory specimens of patients with Encephalitozoon spp. or E. bieneusi infection.
Patients who have severe cellular immunodeficiency appear to be at highest risk of developing microsporidial disease, but little is known about immunity to microsporidial infection. It is not understood whether microsporidial infection in these patients is primarily a reactivation of latent infection acquired before the state of suppressed immunity or whether microsporidial disease is caused by recently acquired infection.
Based on the scarce current epidemiological knowledge concerning transmission of microsporidia, no recommendations to prevent infections can be suggested.
Acknowledgments
Work on microsporidia in the authors' groups was supported by grants from the Swiss National Science Foundation (3200-049751.96/1 and 3237399.93).
REFERENCES
- 1.Aarons, E. J., D. Woodrow, W. S. Hollister, E. U. Canning, N. Francis, and B. G. Gazzard. 1994. Reversible renal failure caused by a microsporidian infection. AIDS 8:1119-1121. [DOI] [PubMed] [Google Scholar]
- 2.Accoceberry, I., J. Carriere, M. Thellier, S. Biligui, M. Danis, and A. Datry. 1997. Rat model for the human intestinal microsporidian Enterocytozoon bieneusi. J. Eukaryot. Microbiol. 44:83S. [DOI] [PubMed] [Google Scholar]
- 3.Accoceberry, I., P. Greiner, M. Thellier, A. Achbarou, S. Biligui, M. Danis, and A. Datry. 1997. Rabbit model for human intestinal microsporidia. J. Eukaryot. Microbiol. 44:82S. [DOI] [PubMed] [Google Scholar]
- 4.Achbarou, A., C. Ombrouck, T. Gneragbe, F. Charlotte, L. Renia, I. Desportes-Livage, and D. Mazier. 1996. Experimental model for human intestinal microsporidiosis in interferon gamma receptor knockout mice infected by Encephalitozoon intestinalis. Parasite Immunol. 18:387-392. [DOI] [PubMed] [Google Scholar]
- 5.Akerstedt, J. 2002. An indirect ELISA for detection of Encephalitozoon cuniculi infection in farmed blue foxes (Alopex lagopus). Acta Vet. Scand. 43:211-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akerstedt, J. 2003. Serological investigation of canine encephalitozoonosis in Norway. Parasitol. Res. 89:49-52. [DOI] [PubMed] [Google Scholar]
- 7.Akerstedt, J., and C. M. Kapel. 2003. Survey for Encephalitozoon cuniculi in arctic foxes (Alopex lagopus) in Greenland. J. Wildl. Dis. 39:228-232. [DOI] [PubMed] [Google Scholar]
- 8.Akerstedt, J., K. Nordstoga, A. Mathis, E. Smeds, and P. Deplazes. 2002. Fox encephalitozoonosis: isolation of the agent from an outbreak in farmed blue foxes (Alopex lagopus) in Finland and some hitherto unreported pathologic lesions. J. Vet. Med. B 49:400-405. [DOI] [PubMed] [Google Scholar]
- 9.Albrecht, H., and I. Sobottka. 1997. Enterocytozoon bieneusi infection in patients who are not infected with human immunodeficiency virus. Clin. Infect. Dis. 25:344. [DOI] [PubMed] [Google Scholar]
- 10.Alfa Cisse, O., A. Ouattara, M. Thellier, I. Accoceberry, S. Biligui, D. Minta, O. Doumbo, I. Desportes-Livage, M. A. Thera, M. Danis, and A. Datry. 2002. Evaluation of an immunofluorescent-antibody test using monoclonal antibodies directed against Enterocytozoon bieneusi and Encephalitozoon intestinalis for diagnosis of intestinal microsporidiosis in Bamako (Mali). J. Clin. Microbiol. 40:1715-1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ashton, N., C. Cook, and F. Clegg. 1976. Encephalitozoonosis (nosematosis) causing bilateral cataract in a rabbit. Br. J. Ophthalmol. 60:618-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashton, N., and P. A. Wirasinha. 1973. Encephalitozoonosis (nosematosis) of the cornea. Br. J. Ophthalmol. 57:669-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baneux, P. J., and F. Pognan. 2003. In utero transmission of Encephalitozoon cuniculi strain type I in rabbits. Lab. Anim. 37:132-138. [DOI] [PubMed] [Google Scholar]
- 14.Becnel, J. J., and T. G. Andreadis. 1999. Microsporidia in insects, p. 1-6. In M. Wittner (ed.), The microsporidia and microsporidiosis. ASM Press, Washington, D.C.
- 15.Bergquist, N. R., G. Stintzing, L. Smedman, T. Waller, and T. Andersson. 1984. Diagnosis of encephalitozoonosis in man by serological tests. Br. Med. J. 24:902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernard, E., M. Carles, C. Pradier, C. Boissy, P. M. Roger, X. Hebuterne, V. Mondain, J. F. Michiels, Y. Le Fichoux, and P. Dellamonica. 1995. Persistent diarrhea in HIV infected patients: role of Enterocytozoon bieneusi. Presse Med. 24:671-674. [PubMed] [Google Scholar]
- 17.Biderre, C., E. U. Canning, G. Metenier, and C. P. Vivares. 1999. Comparison of two isolates of Encephalitozoon hellem and E. intestinalis (Microspora) by pulsed field gel electrophoresis. Eur. J. Protistol. 35:194-196. [Google Scholar]
- 18.Biderre, C., A. Mathis, P. Deplazes, R. Weber, G. Metenier, and C. P. Vivares. 1999. Molecular karyotype diversity in the microsporidian Encephalitozoon cuniculi. Parasitology 118:439-445. [DOI] [PubMed] [Google Scholar]
- 19.Bigliardi, E., A. M. Bernuzzi, S. Corona, S. Gatti, M. Scaglia, and L. Sacchi. 2000. In vitro efficacy of nikkomycin Z against the human isolate of the microsporidian species Encephalitozoon hellem. Antimicrob. Agents Chemother. 44:3012-3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black, S. S., L. A. Steinohrt, D. C. Bertucci, L. B. Rogers, and E. S. Didier. 1997. Encephalitozoon hellem in budgerigars (Melopsittacus undulatus). Vet. Pathol. 34:189-198. [DOI] [PubMed] [Google Scholar]
- 21.Boldorini, R., G. Monga, A. Tosoni, E. S. Didier, M. Nebuloni, G. Costanzi, G. Mazzucco, and J. M. Orenstein. 1998. Renal Encephalitozoon (Septata) intestinalis infection in a patient with AIDS. Post-mortem identification by means of transmission electron microscopy and PCR. Virchows Arch. 432:535-539. [DOI] [PubMed] [Google Scholar]
- 22.Bornay-Llinares, F. J., A. J. da Silva, H. Moura, D. A. Schwartz, G. S. Visvesvara, N. J. Pieniazek, A. Cruz-Lopez, P. Hernandez-Jauregui, J. Guerrero, and F. J. Enriquez. 1998. Immunologic, microscopic, and molecular evidence of Encephalitozoon intestinalis (Septata intestinalis) infection in mammals other than humans. J. Infect. Dis. 178:820-826. [DOI] [PubMed] [Google Scholar]
- 23.Botha, W. S., A. F. Van Dellen, and C. G. Stewart. 1979. Canine encephalitozoonosis in South Africa. J. S. Afr. Vet. Assoc. 50:135-144. [PubMed] [Google Scholar]
- 24.Brasil, P., D. B. de Lima, D. D. de Paiva, M. S. Lobo, F. C. Sodre, S. P. Silva, E. V. Villela, E. J. Silva, J. M. Peralta, M. Morgado, and H. Moura. 2000. Clinical and diagnostic aspects of intestinal microsporidiosis in HIV-infected patients with chronic diarrhea in Rio de Janeiro, Brazil. Rev. Inst. Med. Trop. Sao Paulo 42:299-304. [DOI] [PubMed] [Google Scholar]
- 25.Brasil, P., F. C. Sodre, T. Cuzzi-Maya, M. C. Gutierrez, H. Mattos, and H. Moura. 1996. Intestinal microsporidiosis in HIV-positive patients with chronic unexplained diarrhea in Rio de Janeiro, Brazil: diagnosis, clinical presentation and follow-up. Rev. Inst. Med. Trop. Sao Paulo 38:97-102. [DOI] [PubMed] [Google Scholar]
- 26.Breitenmoser, A. C., A. Mathis, E. Burgi, R. Weber, and P. Deplazes. 1999. High prevalence of Enterocytozoon bieneusi in swine with four genotypes that differ from those identified in humans. Parasitology 118:447-453. [DOI] [PubMed] [Google Scholar]
- 27.Bretagne, S., F. Foulet, W. Alkassoum, J. Fleury-Feith, and M. Develoux. 1993. Prevalence of Enterocytozoon bieneusi spores in the stool of AIDS patients and African children not infected by HIV. Bull. Soc. Pathol. Exot. 86:351-357. [PubMed] [Google Scholar]
- 28.Brown, R. J., D. K. Hinkle, W. P. Trevethan, J. L. Kupper, and A. E. McKee. 1973. Nosematosis in a squirrel monkey (Saimiri sciureus). J. Med. Primatol. 2:114-123. [DOI] [PubMed] [Google Scholar]
- 29.Buckholt, M. A., J. H. Lee, and S. Tzipori. 2002. Prevalence of Enterocytozoon bieneusi in swine: an 18-month survey at a slaughterhouse in Massachusetts. Appl. Environ. Microbiol. 68:2595-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cali, A., D. P. Kotler, and J. M. Orenstein. 1993. Septata intestinalis n. g., n. sp., an intestinal microsporidian associated with chronic diarrhea and dissemination in AIDS patients. J. Eukaryot. Microbiol. 40:101-112. [DOI] [PubMed] [Google Scholar]
- 31.Cali, A., D. M. Meisler, C. Y. Lowder, R. Lembach, L. Ayers, P. M. Takvorian, I. Rutherford, D. L. Longworth, J. M. Mahon, and R. T. Bryan. 1991. Corneal microsporidioses: characterization and identification. J. Protozool. 38:215s-217s. [PubMed] [Google Scholar]
- 32.Cali, A., and P. M. Takvorian. 2003. Ultrastructure and development of Pleistophora ronneafiei n. sp., a microsporidium (Protista) in the skeletal muscle of an immune-compromised individual. J. Eukaryot. Microbiol. 50:77-85. [DOI] [PubMed] [Google Scholar]
- 33.Cali, A., P. M. Takvorian, S. Lewin, M. Rendel, C. S. Sian, M. Wittner, H. B. Tanowitz, E. Keohane, and L. M. Weiss. 1998. Brachiola vesicularum, n. g., n. sp., a new microsporidium associated with AIDS and myositis. J. Eukaryot. Microbiol. 45:240-251. [DOI] [PubMed] [Google Scholar]
- 34.Cali, A., L. M. Weiss, and P. M. Takvorian. 2004. An analysis of the microsporidian genus Brachiola, with comparisons of human and insect isolates of Brachiola algerae. J. Eukaryot. Microbiol. 51:678-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Canning, E. U. 1988. Nuclear division and chromosome cycle in microsporidia. Biosystems 21:333-340. [DOI] [PubMed] [Google Scholar]
- 36.Canning, E. U., A. Curry, J. Vavra, and R. E. Bonshek. 1998. Some ultrastructural data on Microsporidium ceylonensis, a cause of corneal microsporidiosis. Parasite 5:247-254. [DOI] [PubMed] [Google Scholar]
- 37.Canning, E. U., and J. Lom. 1986. The microsporidia of vertebrates. Academic Press, London, United Kingdom.
- 38.Carlisle, M. S., K. Snowden, J. Gill, M. Jones, P. O'Donoghue, and P. Prociv. 2002. Microsporidiosis in a Gouldian finch (Erythrura [Chloebia] gouldiae). Aust. Vet. J. 80:41-44. [DOI] [PubMed] [Google Scholar]
- 39.Carlson, J. R., L. Li, C. L. Helton, R. J. Munn, K. Wasson, R. V. Perez, B. J. Gallay, and W. E. Finkbeiner. 2004. Disseminated microsporidiosis in a pancreas/kidney transplant recipient. Arch. Pathol. Lab. Med. 128:e41-e43. [DOI] [PubMed] [Google Scholar]
- 40.Carr, A., D. Marriott, A. Field, E. Vasak, and D. A. Cooper. 1998. Treatment of HIV-1-associated microsporidiosis and cryptosporidiosis with combination antiretroviral therapy. Lancet 351:256-261. [DOI] [PubMed] [Google Scholar]
- 41.Carville, A., K. Mansfield, G. Widmer, A. Lackner, D. Kotler, P. Wiest, T. Gumbo, S. Sarbah, and S. Tzipori. 1997. Development and application of genetic probes for detection of Enterocytozoon bieneusi in formalin-fixed stools and in intestinal biopsy specimens from infected patients. Clin. Diagn. Lab. Immunol. 4:405-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cavalier-Smith, T. 1993. Kingdom protozoa and its 18 phyla. Microbiol. Rev. 57:953-994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cavalier-Smith, T. 1998. A revised six-kingdom system of life. Biol. Rev. Cambr. Philos. Soc. 73:203-266. [DOI] [PubMed] [Google Scholar]
- 44.Cegielski, J. P., Y. R. Ortega, S. McKee, J. F. Madden, L. Gaido, D. A. Schwartz, K. Manji, A. F. Jorgensen, S. E. Miller, U. P. Pulipaka, A. E. Msengi, D. H. Mwakyusa, C. R. Sterling, and L. B. Reller. 1999. Cryptosporidium, enterocytozoon, and cyclospora infections in pediatric and adult patients with diarrhea in Tanzania. Clin. Infect. Dis. 28:314-321. [DOI] [PubMed] [Google Scholar]
- 45.Chalifoux, L. V., A. Carville, D. Pauley, B. Thompson, A. A. Lackner, and K. G. Mansfield. 2000. Enterocytozoon bieneusi as a cause of proliferative serositis in simian immunodeficiency virus-infected immunodeficient macaques (Macaca mulatta). Arch. Pathol. Lab. Med. 124:1480-1484. [DOI] [PubMed] [Google Scholar]
- 46.Chalupsky, J., J. Vavra, J. C. Gaudin, P. Vandewalle, C. P. Arthur, M. Guenezan, and H. Launay. 1990. Mise en evidence serologique de la presence d'encephalitozoonose et de toxoplasmose chez le lapin de Garenne (Oryctolagus cuniculus) en France. Bull. Soc. Fr. Parasitol. 8:91-95. [Google Scholar]
- 47.Chan, C. M., J. T. Theng, L. Li, and D. T. Tan. 2003. Microsporidial keratoconjunctivitis in healthy individuals: a case series. Ophthalmology. 110:1420-1425. [DOI] [PubMed] [Google Scholar]
- 48.Cheney, S. A., N. J. Lafranchi-Tristem, and E. U. Canning. 2000. Phylogenetic relationships of Pleistophora-like microsporidia based on small subunit ribosomal DNA sequences and implications for the source of Trachipleistophora hominis infections. J. Eukaryot. Microbiol. 47:280-287. [DOI] [PubMed] [Google Scholar]
- 49.Chupp, G. L., J. Alroy, L. S. Adelman, J. C. Breen, and P. R. Skolnik. 1993. Myositis due to Pleistophora (Microsporidia) in a patient with AIDS. Clin. Infect. Dis. 16:15-21. [DOI] [PubMed] [Google Scholar]
- 50.Cislakova, L., and M. Halanova. 2003. Microsporidial infections in immunocompromised hospitalized patients. Cesk Epidemiol. Mikrobiol. Imunol. 52:81-83. [PubMed] [Google Scholar]
- 51.Cislakova, L., I. Literak, P. Balent, V. Hipikova, M. Levkutova, M. Travnicek, and A. Novotna. 2001. Prevalence of antibodies to Encephalitozoon cuniculi (microsporidia) in angora goats—a potential risk of infection for breeders. Ann. Agric. Environ. Med. 8:289-291. [PubMed] [Google Scholar]
- 52.Conners, M. S., T. S. Gibler, and R. N. Van Gelder. 2004. Diagnosis of microsporidia keratitis by polymerase chain reaction. Arch. Ophthalmol. 122:283-284. [DOI] [PubMed] [Google Scholar]
- 53.Conteas, C. N., O. G. Berlin, M. J. Lariviere, S. S. Pandhumas, C. E. Speck, R. Porschen, and T. Nakaya. 1998. Examination of the prevalence and seasonal variation of intestinal microsporidiosis in the stools of persons with chronic diarrhea and human immunodeficiency virus infection. Am. J. Trop. Med. Hyg. 58:559-561. [DOI] [PubMed] [Google Scholar]
- 54.Conteas, C. N., O. G. Berlin, C. E. Speck, S. S. Pandhumas, M. J. Lariviere, and C. Fu. 1998. Modification of the clinical course of intestinal microsporidiosis in acquired immunodeficiency syndrome patients by immune status and anti-human immunodeficiency virus therapy. Am. J. Trop. Med. Hyg. 58:555-558. [DOI] [PubMed] [Google Scholar]
- 55.Cornet, M., S. Romand, J. Warszawski, and P. Bouree. 1996. Factors associated with microsporidial and cryptosporidial diarrhea in HIV infected patients. Parasite 3:397-401. [DOI] [PubMed] [Google Scholar]
- 56.Cotte, C., M. Rabodonirina, M. A. Piens, M. Perreard, M. Mojon, and C. Trepo. 1993. Prevalence of intestinal protozoans in French patients infected with AIDS. J. Aquir. Immune Defic. Syndr. 6:1024-1029. [PubMed] [Google Scholar]
- 57.Cotte, L., M. Rabodonirina, F. Chapuis, F. Bailly, F. Bissuel, C. Raynal, P. Gelas, F. Persat, M. A. Piens, and C. Trepo. 1999. Waterborne outbreak of intestinal microsporidiosis in persons with and without human immunodeficiency virus infection. J. Infect. Dis. 180:2003-2008. [DOI] [PubMed] [Google Scholar]
- 58.Couzinet, S., E. Cejas, J. Schittny, P. Deplazes, R. Weber, and S. Zimmerli. 2000. Phagocytic uptake of Encephalitozoon cuniculi by nonprofessional phagocytes. Infect. Immun. 68:6939-6945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cox, J. C., R. C. Hamilton, and H. D. Attwood. 1979. An investigation of the route and progression of Encephalitozoon cuniculi infection in adult rabbits. J. Protozool. 26:260-265. [DOI] [PubMed] [Google Scholar]
- 60.Cox, J. C., and N. B. Walden. 1972. Presumptive diagnosis of Nosema cuniculi in rabbits by immunofluorescence. Res. Vet. Sci. 13:595-597. [PubMed] [Google Scholar]
- 61.Coyle, C. M., L. M. Weiss, L. V. Rhodes III, A. Cali, P. M. Takvorian, D. F. Brown, G. S. Visvesvara, L. Xiao, J. Naktin, E. Young, M. Gareca, G. Colasante, and M. Wittner. 2004. Fatal myositis due to the microsporidian Brachiola algerae, a mosquito pathogen. N. Engl. J. Med. 351:42-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Coyle, C. M., M. Wittner, D. P. Kotler, C. Noyer, J. M. Orenstein, H. B. Tanowitz, and L. M. Weiss. 1996. Prevalence of microsporidiosis due to Enterocytozoon bieneusi and Encephalitozoon (Septata) intestinalis among patients with AIDS-related diarrhea: determination by polymerase chain reaction to the microsporidian small-subunit rRNA gene. Clin. Infect. Dis. 23:1002-1006. [DOI] [PubMed] [Google Scholar]
- 63.Croppo, G. P., G. S. Visvesvara, G. J. Leitch, S. Wallace, and M. A. De Groote. 1997. Western blot and immunofluorescence analysis of a human isolate of Encephalitozoon cuniculi established in culture from the urine of a patient with AIDS. J. Parasitol. 83:66-69. [PubMed] [Google Scholar]
- 64.Dascomb, K., T. Frazer, R. A. Clark, P. Kissinger, and E. Didier. 2000. Microsporidiosis and HIV. J. Acquir. Immune Defic. Syndr. 24:290-292. [DOI] [PubMed] [Google Scholar]
- 65.Davis, R. M., R. L. Font, M. S. Keisler, and J. A. Shadduck. 1990. Corneal microsporidiosis. A case report including ultrastructural observations. Ophthalmology 97:953-957. [PubMed] [Google Scholar]
- 66.De Groote, M. A., G. Visvesvara, M. L. Wilson, N. J. Pieniazek, S. B. Slemenda, A. J. DaSilva, G. J. Leitch, R. T. Bryan, and R. Reves. 1995. PCR and culture confirmation of disseminated Encephalitozoon cuniculi in a patient with AIDS: successful therapy with albendazole. J. Infect. Dis. 171:1375-1378. [DOI] [PubMed] [Google Scholar]
- 67.Del Aguila, C., G. P. Croppo, H. Moura, A. J. Da Silva, G. J. Leitch, D. M. Moss, S. Wallace, S. B. Slemenda, N. J. Pieniazek, and G. S. Visvesvara. 1998. Ultrastructure, immunofluorescence, Western blot, and PCR analysis of eight isolates of Encephalitozoon (Septata) intestinalis established in culture from sputum and urine samples and duodenal aspirates of five patients with AIDS. J. Clin. Microbiol. 36:1201-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.del Aguila, C., H. Moura, S. Fenoy, R. Navajas, R. Lopez-Velez, L. Li, L. Xiao, G. J. Leitch, A. da Silva, N. J. Pieniazek, A. A. Lal, and G. S. Visvesvara. 2001. In vitro culture, ultrastructure, antigenic, and molecular characterization of Encephalitozoon cuniculi isolated from urine and sputum samples from a Spanish patient with AIDS. J. Clin. Microbiol. 39:1105-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.del Aguila, C., R. Navajas, D. Gurbindo, J. T. Ramos, M. J. Mellado, S. Fenoy, M. A. Munoz Fernandez, M. Subirats, J. Ruiz, and N. J. Pieniazek. 1997. Microsporidiosis in HIV-positive children in Madrid (Spain). J. Eukaryot. Microbiol. 44:84S-85S. [DOI] [PubMed] [Google Scholar]
- 70.Delarbre, S., S. Gatti, M. Scaglia, and M. Drancour. 2001. Genetic diversity in the microsporidian Encephalitozoon hellem demonstrated by pulsed-field gel electrophoresis. J. Eukaryot. Microbiol. 48:471-474. [DOI] [PubMed] [Google Scholar]
- 71.Deluol, A. M., J. L. Poirot, F. Heyer, P. Roux, D. Levy, and W. Rozenbaum. 1994. Intestinal microsporidiosis: about clinical characteristics and laboratory diagnosis. J. Eukaryot. Microbiol. 41:33S. [PubMed] [Google Scholar]
- 72.Dengjel, B., M. Zahler, W. Hermanns, K. Heinritzi, T. Spillmann, A. Thomschke, T. Loscher, R. Gothe, and H. Rinder. 2001. Zoonotic potential of Enterocytozoon bieneusi. J. Clin. Microbiol. 39:4495-4499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Deplazes, P., A. Mathis, R. Baumgartner, I. Tanner, and R. Weber. 1996. Immunologic and molecular characterization of Encephalitozoon-like microsporidia isolated from humans and rabbits indicate that Encephalitozoon cuniculi is a zoonotic parasite. Clin. Infect. Dis. 22:557-559. [DOI] [PubMed] [Google Scholar]
- 74.Deplazes, P., A. Mathis, C. Muller, and R. Weber. 1996. Molecular epidemiology of Encephalitozoon cuniculi and first detection of Enterocytozoon bieneusi in faecal samples of pigs. J. Eukaryot. Microbiol. 43:93S. [DOI] [PubMed] [Google Scholar]
- 75.Deplazes, P., A. Mathis, M. van Saanen, A. Iten, R. Keller, I. Tanner, M. P. Glauser, R. Weber, and E. U. Canning. 1998. Dual microsporidial infection due to Vittaforma corneae and Encephalitozoon hellem in a patient with AIDS. Clin. Infect. Dis. 27:1521-1524. [DOI] [PubMed] [Google Scholar]
- 76.Desportes, I., Y. Le Charpentier, A. Galian, F. Bernard, B. Cochand-Priollet, A. Lavergne, P. Ravisse, and R. Modigliani. 1985. Occurrence of a new microsporidian: Enterocytozoon bieneusi n.g., n. sp., in the enterocytes of a human patient with AIDS. J. Protozool. 32:250-254. [DOI] [PubMed] [Google Scholar]
- 77.Didier, E. S. 2000. Immunology of microsporidiosis. Contrib. Microbiol. 6:193-208. [DOI] [PubMed] [Google Scholar]
- 78.Didier, E. S., P. J. Didier, D. N. Friedberg, S. M. Stenson, J. M. Orenstein, R. W. Yee, F. O. Tio, R. M. Davis, C. Vossbrinck, N. Millichamp, and J. A. Shadduck. 1991. Isolation and characterization of a new human microsporidian, Encephalitozoon hellem (n. sp.), from three AIDS patients with keratoconjunctivitis. J. Infect. Dis. 163:617-621. [DOI] [PubMed] [Google Scholar]
- 79.Didier, E. S., P. J. Didier, K. F. Snowden, and J. A. Shadduck. 2000. Microsporidiosis in mammals. Microb. Infect. 2:709-720. [DOI] [PubMed] [Google Scholar]
- 80.Didier, E. S., J. A. Maddry, C. D. Kwong, L. C. Green, K. F. Snowden, and J. A. Shadduck. 1998. Screening of compounds for antimicrosporidial activity in vitro. Folia Parasitol. 45:129-139. [PubMed] [Google Scholar]
- 81.Didier, E. S., L. B. Rogers, A. D. Brush, S. Wong, V. Traina-Dorge, and D. Bertucci. 1996. Diagnosis of disseminated microsporidian Encephalitozoon hellem infection by PCR-Southern analysis and successful treatment with albendazole and fumagillin. J. Clin. Microbiol. 34:947-952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Didier, E. S., L. B. Rogers, J. M. Orenstein, M. D. Baker, C. R. Vossbrinck, T. Van Gool, R. Hartskeerl, R. Soave, and L. M. Beaudet. 1996. Characterization of Encephalitozoon (Septata) intestinalis isolates cultured from nasal mucosa and bronchoalveolar lavage fluids of two AIDS patients. J. Eukaryot. Microbiol. 43:34-43. [DOI] [PubMed] [Google Scholar]
- 83.Didier, E. S., K. F. Snowden, and J. A. Shadduck. 1998. Biology of microsporidian species infecting mammals. Adv. Parasitol. 40:283-320. [DOI] [PubMed] [Google Scholar]
- 84.Didier, E. S., P. W. Varner, P. J. Didier, A. M. Aldras, N. J. Millichamp, M. Murphey-Corb, R. Bohm, and J. A. Shadduck. 1994. Experimental microsporidiosis in immunocompetent and immunodeficient mice and monkeys. Folia Parasitol. 41:1-11. [PubMed] [Google Scholar]
- 85.Didier, E. S., G. S. Visvesvara, M. D. Baker, L. B. Rogers, D. C. Bertucci, M. A. De Groote, and C. R. Vossbrinck. 1996. A microsporidian isolated from an AIDS patient corresponds to Encephalitozoon cuniculi III, originally isolated from domestic dogs. J. Clin. Microbiol. 34:2835-2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Didier, E. S., C. R. Vossbrinck, M. D. Baker, L. B. Rogers, D. C. Bertucci, and J. A. Shadduck. 1995. Identification and characterization of three Encephalitozoon cuniculi strains. Parasitology 111:411-421. [DOI] [PubMed] [Google Scholar]
- 87.Docker, M. F., M. L. Kent, D. M. L. Hervio, J. S. Khattra, L. M. Weiss, A. Cali, and R. H. Devlin. 1997. Ribosomal DNA sequence of Nucleospora salmonis Hedrick, Groff and Baxa, 1991 (Microsporea: Enterocytozoonidae): implications for phylogeny and nomenclature. J. Eukaryot. Microbiol. 44:55-60. [DOI] [PubMed] [Google Scholar]
- 88.Dore, G. J., D. J. Marriott, M. C. Hing, J. L. Harkness, and A. S. Field. 1995. Disseminated microsporidiosis due to Septata intestinalis in nine patients infected with the human immunodeficiency virus: response to therapy with albendazole. Clin. Infect. Dis. 21:70-76. [DOI] [PubMed] [Google Scholar]
- 89.Dowd, S. E., C. P. Gerba, and I. L. Pepper. 1998. Confirmation of the human-pathogenic microsporidia Enterocytozoon bieneusi, Encephalitozoon intestinalis, and Vittaforma corneae in water. Appl. Environ. Microbiol. 64:3332-3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dowd, S. E., D. John, J. Eliopolus, C. P. Gerba, J. Naranjo, R. Klein, B. Lopez, M. de Mejia, C. E. Mendoza, and I. L. Pepper. 2003. Confirmed detection of Cyclospora cayetanesis, Encephalitozoon intestinalis and Cryptosporidium parvum in water used for drinking. J. Water Health 1:117-123. [PubMed] [Google Scholar]
- 91.Drobniewski, F., P. Kelly, A. Carew, B. Ngwenya, N. Luo, C. Pankhurst, and M. Farthing. 1995. Human microsporidiosis in African AIDS patients with chronic diarrhea. J. Infect. Dis. 171:515-516. [DOI] [PubMed] [Google Scholar]
- 92.Eeftinck Schattenkerk, J. K. M., T. Van Gool, R. J. Van Ketel, J. F. W. M. Bartelsman, C. L. Kuiken, W. J. Terpstra, and P. Reiss. 1991. Clinical significance of small-intestinal microsporidiosis in HIV-1-infected individuals. Lancet 337:895-898. [DOI] [PubMed] [Google Scholar]
- 93.Enriquez, F. J., O. Ditrich, J. D. Palting, and K. Smith. 1997. Simple diagnosis of Encephalitozoon sp. microsporidial infections by using a panspecific antiexospore monoclonal antibody. J. Clin. Microbiol. 35:724-729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Enriquez, F. J., D. Taren, A. Cruz-Lopez, M. Muramoto, J. D. Palting, and P. Cruz. 1998. Prevalence of intestinal encephalitozoonosis in Mexico. Clin. Infect. Dis. 26:1227-1229. [DOI] [PubMed] [Google Scholar]
- 95.Fayer, R. 2004. Infectivity of microsporidia spores stored in seawater at environmental temperatures. J. Parasitol. 90:654-657. [DOI] [PubMed] [Google Scholar]
- 96.Fayer, R., M. Santin, and R. Palmer. 2003. Comparison of microscopy and PCR for detection of three species of Encephalitozoon in feces. J. Eukaryot. Microbiol. 50:572-573. [DOI] [PubMed] [Google Scholar]
- 97.Fayer, R., M. Santin, R. Palmer, and X. Li. 2003. Detection of Encephalitozoon hellem in feces of experimentally infected chickens. J. Eukaryot. Microbiol. 50:574-575. [DOI] [PubMed] [Google Scholar]
- 98.Ferreira, F. M., L. Bezerra, M. B. Santos, R. M. Bernardes, I. Avelino, and M. L. Silva. 2001. Intestinal microsporidiosis: a current infection in HIV-seropositive patients in Portugal. Microb. Infect. 3:1015-1019. [DOI] [PubMed] [Google Scholar]
- 99.Field, A. S., M. C. Hing, S. T. Milliken, and D. J. Marriott. 1993. Microsporidia in the small intestine of HIV-infected patients. a new diagnostic technique and a new species. Med. J. Aust. 158:390-394. [PubMed] [Google Scholar]
- 100.Field, A. S., D. J. Marriott, S. T. Milliken, B. J. Brew, E. U. Canning, J. G. Kench, P. Darveniza, and J. L. Harkness. 1996. Myositis associated with a newly described microsporidian, Trachipleistophora hominis, in a patient with AIDS. J. Clin. Microbiol. 34:2803-2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Font, R. L., G. W. Su, and A. Y. Matoba. 2003. Microsporidial stromal keratitis. Arch. Ophthalmol. 121:1045-1047. [DOI] [PubMed] [Google Scholar]
- 102.Foucault, C., and M. Drancourt. 2000. Actin mediates Encephalitozoon intestinalis entry into the human enterocyte-like cell line, Caco-2. Microb. Pathog. 28:51-58. [DOI] [PubMed] [Google Scholar]
- 103.Fournier, S., S. Dubrou, O. Liguory, F. Gaussin, M. Santillana-Hayat, C. Sarfati, J. M. Molina, and F. Derouin. 2002. Detection of microsporidia, cryptosporidia and Giardia in swimming pools: a one-year prospective study. FEMS Immunol. Med. Microbiol. 33:209-213. [DOI] [PubMed] [Google Scholar]
- 104.Fournier, S., O. Liguory, M. Santillana-Hayat, E. Guillot, C. Sarfati, N. Dumoutier, J. Molina, and F. Derouin. 2000. Detection of microsporidia in surface water: a one-year follow-up study. FEMS Immunol. Med. Microbiol. 29:95-100. [DOI] [PubMed] [Google Scholar]
- 105.Fournier, S., O. Liguory, C. Sarfati, F. David-Ouaknine, F. Derouin, J. M. Decazes, and J. M. Molina. 2000. Disseminated infection due to Encephalitozoon cuniculi in a patient with AIDS: case report and review. HIV Med. 1:155-161. [DOI] [PubMed] [Google Scholar]
- 106.Franzen, C. 2004. Microsporidia: how can they invade other cells? Trends Parasitol. 20:275-279. [DOI] [PubMed] [Google Scholar]
- 107.Franzen, C., R. Kuppers, A. Muller, B. Salzberger, G. Fatkenheuer, B. Vetten, V. Diehl, and M. Schrappe. 1996. Genetic evidence for latent Septata intestinalis infection in human immunodeficiency virus-infected patients with intestinal microsporidiosis. J. Infect. Dis. 173:1038-1040. [DOI] [PubMed] [Google Scholar]
- 108.Franzen, C., and A. Muller. 2001. Microsporidiosis: human diseases and diagnosis. Microb. Infect. 3:389-400. [DOI] [PubMed] [Google Scholar]
- 109.Franzen, C., A. Muller, P. Hartmann, P. Hegener, M. Schrappe, V. Diehl, G. Fatkenheuer, and B. Salzberger. 1998. Polymerase chain reaction for diagnosis and species differentiation of microsporidia. Folia Parasitol. 45:140-148. [PubMed] [Google Scholar]
- 110.Franzen, C., A. Muller, P. Hegener, P. Hartmann, B. Salzberger, B. Franzen, V. Diehl, and G. Fatkenheuer. 1996. Polymerase chain reaction for microsporidian DNA in gastrointestinal biopsy specimens of HIV-infected patients. AIDS 10:F23-F27. [DOI] [PubMed] [Google Scholar]
- 111.Franzen, C., D. A. Schwartz, G. S. Visvesvara, A. Muller, A. Schwenk, B. Salzberger, G. Fatkenheuer, P. Hartmann, G. Mahrle, V. Diehl, et al. 1995. Immunologically confirmed disseminated, asymptomatic Encephalitozoon cuniculi infection of the gastrointestinal tract in a patient with AIDS. Clin. Infect. Dis. 21:1480-1484. [DOI] [PubMed] [Google Scholar]
- 112.Friedberg, D. N., S. M. Stenson, J. M. Orenstein, P. M. Tierno, and N. C. Charles. 1990. Microsporidial keratoconjunctivitis in acquired immunodeficiency syndrome. Arch. Ophthalmol. 108:504-508. [DOI] [PubMed] [Google Scholar]
- 113.Furuya, K. 2002. Genotyping of Encephalitozoon cuniculi isolates found in Hokkaido. Jpn. J. Infect. Dis. 55:128-130. [PubMed] [Google Scholar]
- 114.Gainzarain, J. C., A. Canut, M. Lozano, A. Labora, F. Carreras, S. Fenoy, R. Navajas, N. J. Pieniazek, A. J. da Silva, and C. del Aguila. 1998. Detection of Enterocytozoon bieneusi in two human immunodeficiency virus-negative patients with chronic diarrhea by polymerase chain reaction in duodenal biopsy specimens and review. Clin. Infect. Dis. 27:394-398. [DOI] [PubMed] [Google Scholar]
- 115.Gamboa-Dominguez, A., J. De Anda, J. Donis, F. Ruiz-Maza, G. S. Visvesvara, and H. Diliz. 2003. Disseminated Encephalitozoon cuniculi infection in a Mexican kidney transplant recipient. Transplantation 75:1898-1900. [DOI] [PubMed] [Google Scholar]
- 116.Garcia, L. S. 2002. Laboratory identification of the microsporidia. J. Clin. Microbiol. 40:1892-1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gatti, S., L. Sacchi, S. Novati, S. Corona, A. M. Bernuzzi, H. Moura, N. J. Pieniazek, G. S. Visvesvara, and M. Scaglia. 1997. Extraintestinal microsporidiosis in AIDS patients: clinical features and advanced protocols for diagnosis and characterization of the isolates. J. Eukaryot. Microbiol. 44:79S. [DOI] [PubMed] [Google Scholar]
- 118.Gerba, C. P., K. R. Riley, N. Nwachuku, H. Ryu, and M. Abbaszadegan. 2003. Removal of Encephalitozoon intestinalis, calicivirus, and coliphages by conventional drinking water treatment. J. Environ. Sci. Health A 38:1259-1268. [DOI] [PubMed] [Google Scholar]
- 119.Goetz, M., S. Eichenlaub, G. R. Pape, and R. M. Hoffmann. 2001. Chronic diarrhea as a result of intestinal microsposidiosis in a liver transplant recipient. Transplantation 71:334-337. [DOI] [PubMed] [Google Scholar]
- 120.Goguel, J., C. Katlama, C. Sarfati, C. Maslo, C. Leport, and J. M. Molina. 1997. Remission of AIDS-associated intestinal microsporidiosis with highly active antiretroviral therapy. AIDS 11:1658-1659. [PubMed] [Google Scholar]
- 121.Gomez Morales, M. A., C. Atzori, A. Ludovisi, P. Rossi, and E. Pozio. 1995. Opportunistic and non-opportunistic parasites in HIV-positive and negative patients with diarrhoea in Tanzania. Trop. Med. Parasitol. 46:109-114. [PubMed] [Google Scholar]
- 122.Graczyk, T. K., J. Bosco-Nizeyi, A. J. da Silva, I. N. Moura, N. J. Pieniazek, M. R. Cranfield, and H. D. Lindquist. 2002. A single genotype of Encephalitozoon intestinalis infects free-ranging gorillas and people sharing their habitats in Uganda. Parasitol. Res. 88:926-931. [DOI] [PubMed] [Google Scholar]
- 123.Graczyk, T. K., D. B. Conn, F. Lucy, D. Minchin, L. Tamang, L. N. Moura, and A. J. DaSilva. 2004. Human waterborne parasites in zebra mussels (Dreissena polymorpha) from the Shannon River drainage area, Ireland. Parasitol. Res. 93:385-391. [DOI] [PubMed] [Google Scholar]
- 124.Grau, A., M. E. Valls, J. E. Williams, D. S. Ellis, M. J. Muntane, and C. Nadal. 1996. Myositis caused by Pleistophora in a patient with AIDS. Med. Clin. 107:779-781. [PubMed] [Google Scholar]
- 125.Gray, M. L., M. Puette, and K. S. Latimer. 1998. Microsporidiosis in a young ostrich (Struthio camelus). Avian Dis. 42:832-836. [PubMed] [Google Scholar]
- 126.Green, L. C., P. J. Didier, L. C. Bowers, and E. S. Didier. 2004. Natural and experimental infection of immunocompromised rhesus macaques (Macaca mulatta) with the microsporidian Enterocytozoon bieneusi genotype D. Microb. Infect. 6:996-1002. [DOI] [PubMed] [Google Scholar]
- 127.Green, L. C., P. J. Didier, and E. S. Didier. 1999. Fractionation of sporogonial stages of the microsporidian Encephalitozoon cuniculi by Percoll gradients. J. Eukaryot. Microbiol. 46:434-438. [DOI] [PubMed] [Google Scholar]
- 128.Grohmann, G. S., R. I. Glass, H. G. Pereira, S. S. Monroe, A. W. Hightower, R. Weber, and R. T. Bryan. 1993. Enteric viruses and diarrhea in HIV-infected patients. N. Engl. J. Med. 329:14-20. [DOI] [PubMed] [Google Scholar]
- 129.Gross, U. 2003. Treatment of microsporidiosis including albendazole. Parasitol. Res. 90:S14-S18. [DOI] [PubMed] [Google Scholar]
- 130.Guerard, A., M. Rabodonirina, L. Cotte, O. Liguory, M. A. Piens, S. Daoud, S. Picot, and J. L. Touraine. 1999. Intestinal microsporidiosis occurring in two renal transplant recipients treated with mycophenolate mofetil. Transplantation 68:699-707. [DOI] [PubMed] [Google Scholar]
- 131.Gumbo, T., I. T. Gangaidzo, S. Sarbah, A. Carville, S. Tzipori, and P. M. Wiest. 2000. Enterocytozoon bieneusi infection in patients without evidence of immunosuppression: two cases from Zimbabwe found to have positive stools by PCR. Ann. Trop. Med. Parasitol. 94:699-702. [DOI] [PubMed] [Google Scholar]
- 132.Gumbo, T., R. E. Hobbs, C. Carlyn, G. Hall, and C. M. Isada. 1999. Microsporidia infection in transplant patients. Transplantation 67:482-484. [DOI] [PubMed] [Google Scholar]
- 133.Gumbo, T., S. Steedman, I. T. Gangaidzo, Y. Ortega, C. R. Sterling, A. Carville, S. Tzipori, and P. Wiest. 1999. Intestinal parasites in patients with diarrhea and human immunodeficiency virus infection in Zimbabwe. AIDS 13:819-821. [DOI] [PubMed] [Google Scholar]
- 134.Guscetti, F., A. Mathis, J. M. Hatt, and P. Deplazes. 2003. Overt fatal and chronic subclinical Encephalitozoon cuniculi microsporidiosis in a colony of captive emperor tamarins (Saguinus imperator). J. Med. Primatol. 32:111-119. [DOI] [PubMed] [Google Scholar]
- 135.Halanova, M., L. Cislakova, A. Valencakova, P. Balent, J. Adam, and M. Travnicek. 2003. Serological screening of occurrence of antibodies to Encephalitozoon cuniculi in humans and animals in eastern Slovakia. Ann. Agric. Environ. Med. 10:117-120. [PubMed] [Google Scholar]
- 136.Halanova, M., V. Letkova, V. Macak, M. Stefkovic, and M. Halan. 1999. The first finding of antibodies to Encephalitozoon cuniculi in cows in Slovakia. Vet. Parasitol. 82:167-171. [DOI] [PubMed] [Google Scholar]
- 137.Harcourt-Brown, F. M., and H. K. Holloway. 2003. Encephalitozoon cuniculi in pet rabbits. Vet. Rec. 152:427-431. [DOI] [PubMed] [Google Scholar]
- 138.Haro, M., C. Del Aguila, S. Fenoy, and N. Henriques-Gil. 2003. Intraspecies genotype variability of the microsporidian parasite Encephalitozoon hellem. J. Clin. Microbiol. 41:4166-4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hartskeerl, R. A., T. Van Gool, A. R. J. Schuitema, E. S. Didier, and W. J. Terpstra. 1995. Genetic and immunological characterization of the microsporidian Septata intestinalis Cali, Kotler and Orenstein, 1993: reclassification to Encephalitozoon intestinalis. Parasitology 110:277-285. [DOI] [PubMed] [Google Scholar]
- 140.Hersteinsson, P., E. Gunnarsson, S. Hjartardottir, and K. Skirnisson. 1993. Prevalence of Encephalitozoon cuniculi antibodies in terrestrial mammals in Iceland, 1986 to 1989. J. Wildl. Dis. 29:341-344. [DOI] [PubMed] [Google Scholar]
- 141.Hollister, W. A., E. U. Canning, and C. L. Anderson. 1996. Identification of microsporidia causing human disease. J. Eukaryot. Microbiol. 43:104S-105S. [DOI] [PubMed] [Google Scholar]
- 142.Hollister, W. S., and E. U. Canning. 1987. An enzyme-linked immunosorbent assay (ELISA) for detection of antibodies to Encephalitozoon cuniculi and its use in determination of infections in man. Parasitology 94:209-219. [DOI] [PubMed] [Google Scholar]
- 143.Hollister, W. S., E. U. Canning, N. I. Colbourn, and E. J. Aarons. 1995. Encephalitozoon cuniculi isolated from the urine of an AIDS patient, which differs from canine and murine isolates. J. Eukaryot. Microbiol. 42:367-372. [DOI] [PubMed] [Google Scholar]
- 144.Hollister, W. S., E. U. Canning, N. I. Colbourn, A. Curry, and C. J. N. Lacey. 1993. Characterization of Encephalitozoon hellem (Microspora) isolated from the nasal mucosa of a patient with AIDS. Parasitology 107:351-358. [DOI] [PubMed] [Google Scholar]
- 145.Hollister, W. S., E. U. Canning, E. Weidner, A. S. Field, J. Kench, and D. J. Marriott. 1996. Development and ultrastructure of Trachipleistophora hominis n. g., n. sp. after in vitro isolation from an AIDS patient and inoculation into athymic mice. Parasitology 112:143-154. [DOI] [PubMed] [Google Scholar]
- 146.Hollister, W. S., E. U. Canning, and A. Willcox. 1991. Evidence for widespread occurrence of antibodies to Encephalitozoon cuniculi (Microspora) in man provided by ELISA and other serological tests. Parasitology 102:33-43. [DOI] [PubMed] [Google Scholar]
- 147.Huffman, D. E., A. Gennaccaro, J. B. Rose, and B. W. Dussert. 2002. Low- and medium-pressure UV inactivation of microsporidia Encephalitozoon intestinalis. Water Res. 36:3161-3164. [DOI] [PubMed] [Google Scholar]
- 148.Hutin, Y. J., M. N. Sombardier, O. Liguory, C. Sarfati, F. Derouin, J. Modai, and J. M. Molina. 1998. Risk factors for intestinal microsporidiosis in patients with human immunodeficiency virus infection: a case-control study. J. Infect. Dis. 178:904-907. [DOI] [PubMed] [Google Scholar]
- 149.Inadome, Y., and M. Noguchi. 2003. Selection of higher molecular weight genomic DNA for molecular diagnosis from formalin-fixed material. Diagn. Mol. Pathol. 12:231-236. [DOI] [PubMed] [Google Scholar]
- 150.Johnson, C. H., M. M. Marshall, L. A. DeMaria, J. M. Moffet, and D. G. Korich. 2003. Chlorine inactivation of spores of Encephalitozoon spp. Appl. Environ. Microbiol. 69:1325-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Juarez, S. I., A. Ichinose, S. Jongwutiwes, T. Yanagi, and H. Kanbara. 2003. A species of microsporidium isolated from an HIV-infected patient and identified as Trachipleistophora anthropophthera by transmission electron microscopy. J. Eukaryot. Microbiol. 50:576. [DOI] [PubMed] [Google Scholar]
- 152.Katinka, M. D., S. Duprat, E. Cornillot, G. Metenier, F. Thomarat, G. Prensier, V. Barbe, E. Peyretaillade, P. Brottier, P. Wincker, F. Delbac, H. El Alaoui, P. Peyret, W. Saurin, M. Gouy, J. Weissenbach, and C. P. Vivares. 2001. Genome sequence and gene compaction of the eukaryote parasite Encephalitozoon cuniculi. Nature 414:450-453. [DOI] [PubMed] [Google Scholar]
- 153.Katiyar, S. K., G. S. Visvesvara, and T. D. Edlind. 1995. Comparison of ribosomal RNA sequences from amitochondrial protozoa: implications for processing, mRNA binding and paromomycin susceptibility. Gene 152:27-33. [DOI] [PubMed] [Google Scholar]
- 154.Katzwinkel-Wladarsch, S., P. Deplazes, R. Weber, T. Löscher, and H. Rinder. 1997. Comparison of polymerase chain reaction with light microscopy for detection of microsporidia in clinical specimens. J. Clin. Microbiol. 16:7-10. [DOI] [PubMed] [Google Scholar]
- 155.Keeling, P. J. 2003. Congruent evidence from alpha-tubulin and beta-tubulin gene phylogenies for a zygomycete origin of microsporidia. Fungal Genet. Biol. 38:298-309. [DOI] [PubMed] [Google Scholar]
- 156.Kelkar, R., P. S. Sastry, S. S. Kulkarni, T. K. Saikia, P. M. Parikh, and S. H. Advani. 1997. Pulmonary microsporidial infection in a patient with CML undergoing allogeneic marrow transplant. Bone Marrow Transplant. 19:179-182. [DOI] [PubMed] [Google Scholar]
- 157.Kelly, P., G. McPhail, B. Ngwenya, N. Luo, A. H. Karew, C. Pankhurst, F. Drobniewski, and M. Farthing. 1994. Septata intestinalis: a new microsporidian in Africa. Lancet 344:271-272. [DOI] [PubMed] [Google Scholar]
- 158.Kodjikian, L., J. G. Garweg, M. Nguyen, T. Schaffner, P. Deplazes, and S. Zimmerli. 2005. Intraocular microsporidiosis due to Encephalitozoon cuniculi in a patient with idiopathic CD4+ T-lymphocytopenia. Int. J. Med. Microbiol. 294:529-533. [DOI] [PubMed] [Google Scholar]
- 159.Kondova, I., K. Mansfield, M. A. Buckholt, B. Stein, G. Widmer, A. Carville, A. Lackner, and S. Tzipori. 1998. Transmission and serial propagation of Enterocytozoon bieneusi from humans and rhesus macaques in gnotobiotic piglets. Infect. Immun. 66:5515-5519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kotler, D. P., T. T. Giang, M. L. Garro, and J. M. Orenstein. 1994. Light microscopic diagnosis of microsporidiosis in patients with AIDS. Am. J. Gastroenterol. 89:540-544. [PubMed] [Google Scholar]
- 161.Kotler, D. P., and J. M. Orenstein. 1994. Prevalence of intestinal microsporidiosis in HIV-infected individuals referred for gastroenterological evaluation. Am. J. Gastroenterol. 89:1998-2002. [PubMed] [Google Scholar]
- 162.Koudela, B., E. S. Didier, L. B. Rogers, D. Modry, and S. Kucerova. 1998. Intestinal microsporidiosis in African skink Mabuya perrotetii. Folia Parasitol. 45:149-155. [PubMed] [Google Scholar]
- 163.Koudela, B., J. Vavra, and E. U. Canning. 2004. Experimental infection of severe combined immunodeficient (SCID) mice with the human microsporidian Trachipleistophora hominis. Parasitology 128:377-384. [DOI] [PubMed] [Google Scholar]
- 164.Koudela, B., G. S. Visvesvara, H. Moura, and J. Vavra. 2001. The human isolate of Brachiola algerae (Phylum Microspora): development in SCID mice and description of its fine structure features. Parasitology 123:153-162. [DOI] [PubMed] [Google Scholar]
- 165.Kucerova-Pospisilova, Z., and O. Ditrich. 1998. The serological surveillance of several groups of patients using antigens of Encephalitozoon hellem and E. cuniculi antibodies to microsporidia in patients. Folia Parasitol. 45:108-112. [PubMed] [Google Scholar]
- 166.Kyaw, T., A. Curry, V. Edwards-Jones, J. Craske, and B. K. Mandal. 1997. The prevalence of Enterocytozoon bieneusi in acquired immunodeficiency syndrome (AIDS) patients from the north west of England: 1992-1995. Br. J. Biomed. Sci. 54:186-191. [PubMed] [Google Scholar]
- 167.Latib, M. A., M. D. Pascoe, M. S. Duffield, and D. Kahn. 2001. Microsporidiosis in the graft of a renal transplant recipient. Transplant. Int. 14:274-277. [DOI] [PubMed] [Google Scholar]
- 168.Leder, K., N. Ryan, D. Spelman, and S. M. Crowe. 1998. Microsporidial disease in HIV-infected patients: a report of 42 patients and review of the literature. Scand. J. Infect. Dis. 30:331-338. [DOI] [PubMed] [Google Scholar]
- 169.Ledford, D. K., M. D. Overman, A. Gonzalvo, A. Cali, S. W. Mester, and R. F. Lockey. 1985. Microsporidiosis myositis in a patient with the acquired immunodeficiency syndrome. Ann. Intern. Med. 102:628-630. [DOI] [PubMed] [Google Scholar]
- 170.Levaditi, C., S. Nicolau, and R. Schoen. 1923. Eine Mikrosporidie, Encephalitozoon cuniculi, als Erreger der epizootischen Encephalitis des Kaninchens. Schweiz. Med. Wochenschr. 6:149-151. [Google Scholar]
- 171.Lewis, N. L., I. C. Francis, G. S. Hawkins, and M. T. Coroneo. 2003. Bilateral microsporidial keratoconjunctivitis in an immunocompetent non-contact lens wearer. Cornea 22:374-376. [DOI] [PubMed] [Google Scholar]
- 172.Li, X., R. Palmer, J. M. Trout, and R. Fayer. 2003. Infectivity of microsporidia spores stored in water at environmental temperatures. J. Parasitol. 89:185-188. [DOI] [PubMed] [Google Scholar]
- 173.Li, X., J. M. Trout, M. C. Jenkins, R. Palmer, and R. Fayer. 2002. Effects of gamma radiation on viability of Encephalitozoon spores. J. Parasitol. 88:812-813. [DOI] [PubMed] [Google Scholar]
- 174.Liguory, O., F. David, C. Sarfati, F. Derouin, and J. M. Molina. 1998. Determination of types of Enterocytozoon bieneusi strains isolated from patients with intestinal microsporidiosis. J. Clin. Microbiol. 36:1882-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liguory, O., F. David, C. Sarfati, A. R. Schuitema, R. A. Hartskeerl, F. Derouin, J. Modai, and J. M. Molina. 1997. Diagnosis of infections caused by Enterocytozoon bieneusi and Encephalitozoon intestinalis using polymerase chain reaction in stool specimens. AIDS 11:723-726. [DOI] [PubMed] [Google Scholar]
- 176.Liguory, O., S. Fournier, C. Sarfati, F. Derouin, and J. M. Molina. 2000. Genetic homology among thirteen Encephalitozoon intestinalis isolates obtained from human immunodeficiency virus-infected patients with intestinal microsporidiosis. J. Clin. Microbiol. 38:2389-2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lippert, U., J. Schottelius, and C. Manegold. 2003. Disseminated microsporidiosis (Encephalitozoon intestinalis) in a patient with HIV infection. Dtsch. Med. Wochenschr. 128:1769-1772. [DOI] [PubMed] [Google Scholar]
- 178.Lobo, M. L., A. Teles, M. B. da Cunha, J. Henriques, A. M. Lourenco, F. Antunes, and O. Matos. 2003. Microsporidia detection in stools from pets and animals from the zoo in Portugal: a preliminary study. J. Eukaryot. Microbiol. 50:581-582. [DOI] [PubMed] [Google Scholar]
- 179.Lom, J. 2002. A catalogue of described genera and species of microsporidians parasitic in fish. Syst. Parasitol. 53:81-99. [DOI] [PubMed] [Google Scholar]
- 180.Lom, J., and I. Dykova. 2002. Ultrastructure of Nucleospora secunda n.sp. (Microsporidia), parasite of enterocytes of Nothobranchius rubripinnis. Eur. J. Protistol. 38:19-27. [Google Scholar]
- 181.Lopez-Velez, R., M. C. Turrientes, C. Garron, P. Montilla, R. Navajas, S. Fenoy, and C. del Aguila. 1999. Microsporidiosis in travelers with diarrhea from the tropics. J. Travel Med. 6:223-227. [DOI] [PubMed] [Google Scholar]
- 182.Lores, B., C. del Aguila, and C. Arias. 2002. Enterocytozoon bieneusi (microsporidia) in faecal samples from domestic animals from Galicia, Spain. Mem. Inst. Oswaldo Cruz 97:941-945. [DOI] [PubMed] [Google Scholar]
- 183.Lowman, P. M., P. M. Takvorian, and A. Cali. 2000. The effects of elevated temperatures and various time-temperature combinations on the development of Brachiola (Nosema) algerae n. comb. in mammalian cell culture. J. Eukaryot. Microbiol. 47:221-234. [DOI] [PubMed] [Google Scholar]
- 184.Ludovisi, A., P. Rossi, A. M. Onori, and E. Pozio. 1998. In vitro growth on different cell lines of four microsporidial species infecting humans. Folia Parasitol. 45:329-331. [PubMed] [Google Scholar]
- 185.Maiga, I., O. Doumbo, M. Dembele, H. Traore, I. Desportes-Livage, I. Hilmarsdottir, E. Giboyau, L. Maiga, L. Kassambara, Y. el Fakhry, A. Datry, M. Gentilini, and E. Pichard. 1997. Human intestinal microsporidiosis in Bamako (Mali): the presence of Enterocytozoon bieneusi in HIV seropositive patients. Santé 7:257-262. [PubMed] [Google Scholar]
- 186.Mansfield, K. G., A. Carville, D. Hebert, L. Chalifoux, D. Shvetz, K. C. Lin, S. Tzipori, and A. A. Lackner. 1998. Localization of persistent Enterocytozoon bieneusi infection in normal rhesus macaques (Macaca mulatta) to the hepatobiliary tree. J. Clin. Microbiol. 36:2336-2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Marangi, A., P. Maggi, M. A. Panaro, G. Angarano, G. Pastore, S. Lisi, C. Romanelli, and O. Brandonisio. 1995. Intestinal microsporidiosis in AIDS patients with diarrhoeal illness in Apulia (south Italy). New Microbiol. 18:435-439. [PubMed] [Google Scholar]
- 188.Margileth, A. M., A. J. Strano, R. Chandra, R. Neafie, M. Blum, and R. M. McCully. 1973. Disseminated nosematosis in an immunologically compromised infant. Arch. Pathol. 95:145-150. [PubMed] [Google Scholar]
- 189.Mathis, A. 2000. Microsporidia: emerging advances in understanding the basic biology of these unique organisms. Int. J. Parasitol. 30:795-804. [DOI] [PubMed] [Google Scholar]
- 190.Mathis, A., J. Akerstedt, J. Tharaldsen, O. Odegaard, and P. Deplazes. 1996. Isolates of Encephalitozoon cuniculi from farmed blue foxes (Alopex lagopus) from Norway differ from isolates from Swiss domestic rabbits (Oryctolagus cuniculus). Parasitol. Res. 82:727-730. [DOI] [PubMed] [Google Scholar]
- 191.Mathis, A., A. C. Breitenmoser, and P. Deplazes. 1999. Detection of new Enterocytozoon genotypes in faecal samples of farm dogs and a cat. Parasite 6:189-193. [DOI] [PubMed] [Google Scholar]
- 192.Mathis, A., M. Michel, H. Kuster, C. Muller, R. Weber, and P. Deplazes. 1997. Two Encephalitozoon cuniculi strains of human origin are infectious to rabbits. Parasitology 114:29-35. [DOI] [PubMed] [Google Scholar]
- 193.Mathis, A., W. Ndiritu, R. C. A. Thompson, E. S. Didier, U. Müller-Doblies, and P. Deplazes. 2000. Genetic heterogeneity and host specificity of the microsporidian Enterocytozoon bieneusi. Acta Parasitol. 45:190. [Google Scholar]
- 194.Mathis, A., I. Tanner, R. Weber, and P. Deplazes. 1999. Genetic and phenotypic intraspecific variation in the microsporidian Encephalitozoon hellem. Int. J. Parasitol. 29:767-770. [DOI] [PubMed] [Google Scholar]
- 195.Matsubayashi, M., T. Koike, I. Mikata, H. Takei, and S. Hagiwara. 1959. A case of Encephalitozoon-like body infection in man. Arch. Pathol. 67:181-187. [PubMed] [Google Scholar]
- 196.Mertens, R. B., E. S. Didier, M. C. Fishbein, D. C. Bertucci, L. B. Rogers, and J. M. Orenstein. 1997. Encephalitozoon cuniculi microsporidiosis: infection of the brain, heart, kidneys, trachea, adrenal glands, and urinary bladder in a patient with AIDS. Mod. Pathol. 10:68-77. [PubMed] [Google Scholar]
- 197.Metge, S., J. T. Van Nhieu, D. Dahmane, P. Grimbert, F. Foulet, C. Sarfati, and S. Bretagne. 2000. A case of Enterocytozoon bieneusi infection in an HIV-negative renal transplant recipient. Eur. J. Clin. Microbiol. Infect. Dis. 19:221-223. [DOI] [PubMed] [Google Scholar]
- 198.Miao, Y. M., F. M. Awad-El-Kariem, C. Franzen, D. S. Ellis, A. Muller, H. M. Counihan, P. J. Hayes, and B. G. Gazzard. 2000. Eradication of cryptosporidia and microsporidia following successful antiretroviral therapy. J. Acquir. Immune Defic. Syndr. 25:124-129. [DOI] [PubMed] [Google Scholar]
- 199.Mohandas, K., R. Sehgal, A. Sud, and N. Malla. 2002. Prevalence of intestinal parasitic pathogens in HIV-seropositive individuals in Northern India. Jpn. J. Infect. Dis. 55:83-84. [PubMed] [Google Scholar]
- 200.Mohindra, A. R., M. W. Lee, G. Visvesvara, H. Moura, R. Parasuraman, G. J. Leitch, L. Xiao, J. Yee, and R. del Busto. 2002. Disseminated microsporidiosis in a renal transplant recipient. Transplant. Infect. Dis. 4:102-107. [DOI] [PubMed] [Google Scholar]
- 201.Mohn, S. F., K. Nordstoga, J. Krogsrud, and A. Helgebostad. 1974. Transplacental transmission of Nosema cuniculi in the blue fox (Alopex lagopus). Acta Pathol. Microbiol. Scand. B 82:299-300. [DOI] [PubMed] [Google Scholar]
- 202.Molina, J.-M., E. Oksenhendler, B. Beauvais, C. Sarfati, A. Jaccard, F. Derouin, and J. Modai. 1995. Disseminated microsporidiosis due to Septata intestinalis in patients with AIDS: clinical features and response to albendazole therapy. J. Infect. Dis. 171:245-249. [DOI] [PubMed] [Google Scholar]
- 203.Molina, J. M., C. Sarfati, B. Beauvais, M. Lemann, A. Lesourd, F. Ferchal, I. Casin, P. Lagrange, R. Modigliani, and F. Derouin. 1993. Intestinal microsporidiosis in human immunodeficiency virus-infected patients with chronic unexplained diarrhea: prevalence and clinical and biologic features. J. Infect. Dis. 167:217-221. [DOI] [PubMed] [Google Scholar]
- 204.Molina, J. M., M. Tourneur, C. Sarfati, S. Chevret, A. de Gouvello, J. G. Gobert, S. Balkan, F. Derouin, and Agence Nationale de Recherches sur le SIDA 090 Study Group. 2002. Fumagillin treatment of intestinal microsporidiosis. N. Engl. J. Med. 346:1963-1969. [DOI] [PubMed] [Google Scholar]
- 205.Monis, P. T., and R. C. Thompson. 2003. Cryptosporidium and Giardia-zoonoses: fact or fiction? Infect. Genet. Evol. 3:233-244. [DOI] [PubMed] [Google Scholar]
- 206.Moon, S. J., P. M. Mann, and A. Y. Matoba. 2003. Microsporidial keratoconjunctivitis in a healthy patient with a history of LASIK surgery. Cornea 22:271-272. [DOI] [PubMed] [Google Scholar]
- 207.Moura, H., A. J. da Silva, I. N. S. Moura, D. A. Schwartz, G. Leitch, S. Wallace, N. J. Pieniazek, R. A. Wirtz, and G. S. Visvesvara. 1999. Characterization of Nosema algerae isolates after continuous cultivation in mammalian cells at 37 degrees C. J. Eukaryot. Microbiol. 46:14S-16S. [PubMed] [Google Scholar]
- 208.Moura, H., F. C. Sodre, F. J. Bornay-Llinares, G. J. Leitch, T. Navin, S. Wahlquist, R. Bryan, I. Meseguer, and G. S. Visvesvara. 1999. Detection by an immunofluorescence test of Encephalitozoon intestinalis spores in routinely formalin-fixed stool samples stored at room temperature. J. Clin. Microbiol. 37:2317-2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Muller, A., R. Bialek, A. Kamper, G. Fatkenheuer, B. Salzberger, and C. Franzen. 2001. Detection of microsporidia in travelers with diarrhea. J. Clin. Microbiol. 39:1630-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Müller, C. 1998. Untersuchungen zur Diagnostik, Biologie und Verbreitung von Microsporidien bei Kaninchen und anderen Tierarten. Dissertation. University of Zürich, Zürich, Switzerland.
- 211.Müller, M. 1997. What are the microsporidia? Parasitol. Today 13:455-456. [DOI] [PubMed] [Google Scholar]
- 212.Muller-Doblies, U. U., K. Herzog, I. Tanner, A. Mathis, and P. Deplazes. 2002. First isolation and characterisation of Encephalitozoon cuniculi from a free-ranging rat (Rattus norvegicus). Vet. Parasitol. 107:279-285. [DOI] [PubMed] [Google Scholar]
- 213.Mungthin, M., R. Suwannasaeng, T. Naaglor, W. Areekul, and S. Leelayoova. 2001. Asymptomatic intestinal microsporidiosis in Thai orphans and child-care workers. Trans. R. Soc. Trop. Med. Hyg. 95:304-306. [DOI] [PubMed] [Google Scholar]
- 214.Nannini, E. C., and P. C. Okhuysen. 2002. HIV1 and the gut in the era of highly active antiretroviral therapy. Curr. Gastroenterol. Rep. 4:392-398. [DOI] [PubMed] [Google Scholar]
- 215.Nordstoga, K. 1972. Nosematosis in blue foxes. Nord. Vet. Med. 24:21-24. [PubMed] [Google Scholar]
- 216.Norton, J. H., and H. C. Prior. 1994. Microsporidiosis in a peach-faced lovebird (Agapornis roseicollis). Aust. Vet. J. 71:23-24. [DOI] [PubMed] [Google Scholar]
- 217.Orenstein, J. M. 2003. Diagnostic pathology of microsporidiosis. Ultrastruct. Pathol. 27:141-149. [DOI] [PubMed] [Google Scholar]
- 218.Orenstein, J. M., J. Chiang, W. Steinberg, P. D. Smith, H. Rotterdam, and D. P. Kotler. 1990. Intestinal microsporidiosis as a cause of diarrhea in human immunodeficiency virus-infected patients: a report of 20 cases. Hum. Pathol. 21:475-481. [DOI] [PubMed] [Google Scholar]
- 219.Orenstein, J. M., J. Seedor, D. N. Friedberg, S. S. M., P. M. Tierno, N. C. Charles, M. D. M., C. Y. Lowder, J. T. McMahon, D. L. Longworth, I. Rutherford, R. W. Yee, A. Martinez, F. Tio, and K. Held. 1990. Microsporidian keratoconjunctivitis in patients with AIDS. Morb. Mort. Wkly. Rep. 39:188-189. [PubMed] [Google Scholar]
- 220.Patterson-Kane, J. C., P. Caplazi, F. Rurangirwa, R. R. Tramontin, and K. Wolfsdorf. 2003. Encephalitozoon cuniculi placentitis and abortion in a quarterhorse mare. J. Vet. Diagn. Investig. 15:57-59. [DOI] [PubMed] [Google Scholar]
- 221.Peacock, C. S., C. Blanshard, D. G. Tovey, D. S. Ellis, and B. G. Gazzard. 1991. Histological diagnosis of intestinal microsporidiosis in patients with AIDS. J. Clin. Pathol. 44:558-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Peuvel, I., F. Delbac, G. Metenier, P. Peyret, and C. P. Vivares. 2000. Polymorphism of the gene encoding a major polar tube protein PTP1 in two microsporidia of the genus Encephalitozoon. Parasitology 121:581-587. [DOI] [PubMed] [Google Scholar]
- 223.Pinnolis, M., P. R. Egbert, R. L. Font, and F. C. Winter. 1981. Nosematosis of the cornea. Case report, including electron microscopic studies. Arch. Ophthalmol. 99:1044-1047. [DOI] [PubMed] [Google Scholar]
- 224.Pospisilova, Z., O. Ditrich, M. Stankova, and P. Kodym. 1997. Parasitic opportunistic infections in Czech HIV-infected patients—a prospective study. Cent. Eur. J. Public Health 5:208-213. [PubMed] [Google Scholar]
- 225.Pourrut, X., C. Sarfati, O. Liguory, R. Moyou-Somo, and F. Derouin. 2002. Search for Enterocytozoon bieneusi infection in wild monkeys in Cameroon. Trans. R. Soc. Trop. Med. Hyg. 96:56-57. [DOI] [PubMed] [Google Scholar]
- 226.Pulparampil, N., D. Graham, D. Phalen, and K. Snowden. 1998. Encephalitozoon hellem in two Eclectus parrots (Eclectus roratus): identification from archival tissues. J. Eukaryot. Microbiol. 45:651-655. [DOI] [PubMed] [Google Scholar]
- 227.Rabeneck, L., F. Gyorkey, R. M. Genta, P. Gyorkey, L. W. Foote, and J. M. Risser. 1993. The role of microsporidia in the pathogenesis of HIV-related chronic diarrhea. Ann. Intern. Med. 119:895-899. [DOI] [PubMed] [Google Scholar]
- 228.Rabodonirina, M., M. Bertocchi, I. Desportes-Livage, L. Cotte, H. Levrey, M. A. Piens, G. Monneret, M. Celard, J. F. Mornex, and M. Mojon. 1996. Enterocytozoon bieneusi as a cause of chronic diarrhea in a heart-lung transplant recipient who was seronegative for human immunodeficiency virus. Clin. Infect. Dis. 23:114-117. [DOI] [PubMed] [Google Scholar]
- 229.Rabodonirina, M., L. Cotte, S. Radenne, E. Besada, and C. Trepo. 2003. Microsporidiosis and transplantation: a retrospective study of 23 cases. J. Eukaryot. Microbiol. 50:583. [DOI] [PubMed] [Google Scholar]
- 230.Randall, C. J., S. Lees, R. J. Higgins, and N. H. Harcourt-Brown. 1986. Microsporidian infection in lovebirds (Agapornis spp.). Avian Pathol. 15:223-231. [DOI] [PubMed] [Google Scholar]
- 231.Rauz, S., S. Tuft, J. K. Dart, R. Bonshek, P. Luthert, and A. Curry. 2004. Ultrastructural examination of two cases of stromal microsporidial keratitis. J. Med. Microbiol. 53:775-781. [DOI] [PubMed] [Google Scholar]
- 232.Raynaud, L., F. Delbac, V. Broussolle, M. Rabodonirina, V. Girault, M. Wallon, G. Cozon, C. P. Vivares, and F. Peyron. 1998. Identification of Encephalitozoon intestinalis in travelers with chronic diarrhea by specific PCR amplification. J. Clin. Microbiol. 36:37-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Reetz, J., H. Rinder, A. Thomschke, H. Manke, M. Schwebs, and A. Bruderek. 2002. First detection of the microsporidium Enterocytozoon bieneusi in non-mammalian hosts (chickens). Int. J. Parasitol. 32:785-787. [DOI] [PubMed] [Google Scholar]
- 234.Reetz, J., M. Wiedemann, A. Aue, U. Wittstatt, A. Ochs, A. Thomschke, H. Manke, M. Schwebs, and H. Rinder. 2004. Disseminated lethal Encephalitozoon cuniculi (genotype III) infections in cotton-top tamarins (Oedipomidas oedipus)—a case report. Parasitol. Int. 53:29-34. [DOI] [PubMed] [Google Scholar]
- 235.Rinder, H., S. Katzwinkel-Wladarsch, and T. Loscher. 1997. Evidence for the existence of genetically distinct strains of Enterocytozoon bieneusi. Parasitol. Res. 83:670-672. [DOI] [PubMed] [Google Scholar]
- 236.Rinder, H., S. Katzwinkel-Wladarsch, A. Thomschke, and T. Loscher. 1998. Strain differentiation in microsporidia. Tokai J. Exp. Clin. Med. 23:433-437. [PubMed] [Google Scholar]
- 237.Rinder, H., A. Thomschke, B. Dengjel, R. Gothe, T. Loscher, and M. Zahler. 2000. Close genotypic relationship between Enterocytozoon bieneusi from humans and pigs and first detection in cattle. J. Parasitol. 86:185-188. [DOI] [PubMed] [Google Scholar]
- 238.Rossi, P., G. La Rosa, A. Ludovisi, A. Tamburini, M. A. Gomez Morales, and E. Pozio. 1998. Identification of a human isolate of Encephalitozoon cuniculi type I from Italy. Int. J. Parasitol. 28:1361-1366. [DOI] [PubMed] [Google Scholar]
- 239.Ryan, N. J., G. Sutherland, K. Coughlan, M. Globan, J. Doultree, J. Marshall, R. W. Baird, J. Pedersen, and B. Dwyer. 1993. A new trichome-blue stain for detection of microsporidial species in urine, stool, and nasopharyngeal specimens. J. Clin. Microbiol. 31:3264-3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Sadler, F., N. Peake, R. Borrow, P. L. Rowl, E. G. Wilkins, and A. Curry. 2002. Genotyping of Enterocytozoon bieneusi in AIDS patients from the north west of England. J. Infect. 44:39-42. [DOI] [PubMed] [Google Scholar]
- 241.Same-Ekobo, A., J. Lohoue, and A. Mbassi. 1997. A clinical and biological study of parasitic and fungal diarrhea in immunosuppressed patients in an urban and suburban area of Yaounde. Santé 7:349-354. [PubMed] [Google Scholar]
- 242.Sandfort, J., A. Hannemann, H. Gelderblom, K. Stark, R. l. Owen, and B. Ruf. 1994. Enterocytozoon bieneusi infection in an immunocompetent patient who had acute diarrhea and who was not infected with the human immunodeficiency virus. Clin. Infect. Dis. 19:514-516. [DOI] [PubMed] [Google Scholar]
- 243.Santin, M., J. M. Trout, and R. Fayer. 2004. Prevalence of Enterocytozoon bieneusi in post-weaned dairy calves in the eastern United States. Parasitol. Res. 93:287-289. [DOI] [PubMed] [Google Scholar]
- 244.Sax, P. E., J. D. Rich, W. S. Pieciak, and Y. M. Trnka. 1995. Intestinal microsporidiosis occurring in a liver transplant recipient. Transplantation 60:617-618. [DOI] [PubMed] [Google Scholar]
- 245.Scaglia, M., C. Bandi, S. Novati, S. Gatti, A. M. Bernuzzi, S. Corona, and L. Sacchi. 1998. Respiratory microsporidiosis due to Encephaliltozoon hellem: the first case report in an immunocompetent subject. Parasitol. Int. 47:203S. [Google Scholar]
- 246.Scaglia, M., S. Gatti, L. Sacchi, S. Corona, G. Chichino, A. M. Bernuzzi, G. Barbarini, G. P. Croppo, A. J. Da Silva, N. J. Pieniazek, and G. S. Visvesvara. 1998. Asymptomatic respiratory tract microsporidiosis due to Encephalitozoon hellem in three patients with AIDS. Clin. Infect. Dis. 26:174-176. [DOI] [PubMed] [Google Scholar]
- 247.Scaglia, M., L. Sacchi, G. P. Croppo, A. da Silva, S. Gatti, S. Corona, A. Orani, A. M. Bernuzzi, N. J. Pieniazek, S. B. Slemenda, S. Wallace, and G. S. Visvesvara. 1997. Pulmonary microsporidiosis due to Encephalitozoon hellem in a patient with AIDS. J. Infect. 34:119-126. [DOI] [PubMed] [Google Scholar]
- 248.Schwartz, D. A., R. T. Bryan, K. O. Hewan-Lowe, G. S. Visvesvara, R. Weber, A. Cali, and P. Angritt. 1992. Disseminated microsporidiosis (Encephalitozoon hellem) and acquired immunodeficiency syndrome. Autopsy evidence for respiratory acquisition. Arch. Pathol. Lab. Med. 116:660-668. [PubMed] [Google Scholar]
- 249.Schwartz, D. A., G. S. Visvesvara, M. C. Diesenhouse, R. Weber, R. L. Font, L. A. Wilson, G. Corrent, O. N. Serdarevic, D. F. Rosberger, P. C. Keenen, H. E. Grossniklaus, K. Hewan-Lowe, and R. T. Bryan. 1993. Pathologic features and immunofluorescent antibody demonstration of ocular microsporidiosis (Encephalitozoon hellem) in seven patients with acquired immunodeficiency syndrome. Am. J. Ophthalmol. 115:285-292. [DOI] [PubMed] [Google Scholar]
- 250.Schwartz, D. A., G. S. Visvesvara, G. J. Leitch, L. Tashjian, M. Pollack, J. Holden, and R. T. Bryan. 1993. Pathology of symptomatic microsporidial (Encephalitozoon hellem) bronchiolitis in the acquired immunodeficiency syndrome: a new respiratory pathogen diagnosed from lung biopsy, bronchoalveolar lavage, sputum, and tissue culture. Hum. Pathol. 24:937-943. [DOI] [PubMed] [Google Scholar]
- 251.Shadduck, J. A., and G. Baskin. 1989. Serologic evidence of Encephalitozoon cuniculi infection in a colony of squirrel monkeys (Saimiri sciureus). Lab. Anim. Sci. 39:328-330. [PubMed] [Google Scholar]
- 252.Shadduck, J. A., R. Bendele, and G. T. Robinson. 1978. Isolation of the causative organism of canine encephalitozoonosis. Vet. Pathol. 15:449-460. [DOI] [PubMed] [Google Scholar]
- 253.Shadduck, J. A., R. A. Meccoli, R. Davis, and R. L. Font. 1990. Isolation of a microsporidian from a human patient. J. Infect. Dis. 162:773-776. [DOI] [PubMed] [Google Scholar]
- 254.Shadduck, J. A., W. T. Watson, S. P. Pakes, and A. Cali. 1979. Animal infectivity of Encephalitozoon cuniculi. J. Parasitol. 65:123-129. [PubMed] [Google Scholar]
- 255.Sharma, S., P. Sachdeva, and J. S. Virdi. 2003. Emerging water-borne pathogens. Appl. Microbiol. Biotechnol. 61:424-428. [DOI] [PubMed] [Google Scholar]
- 256.Shaw, R. W. 1999. Fish microsporidia, p. 447-501. In M. Wittner (ed.), Microsporidia and microsporidiosis. ASM Press, Washington, D.C.
- 257.Sheikh, R. A., T. P. Prindiville, S. Yenamandra, R. J. Munn, and B. H. Ruebner. 2000. Microsporidial AIDS cholangiopathy due to Encephalitozoon intestinalis: case report and review. Am. J. Gastroenterol. 95:2364-2371. [DOI] [PubMed] [Google Scholar]
- 258.Silveira, H., and E. U. Canning. 1995. Vittaforma corneae n. comb. for the human microsporidium Nosema corneum Shadduck, Meccoli, Davis & Font, 1990, based on its ultrastructure in the liver of experimentally infected athymic mice. J. Eukaryot. Microbiol. 42:158-165. [DOI] [PubMed] [Google Scholar]
- 259.Silverstein, B. E., E. T. Cunningham, Jr., T. P. Margolis, V. Cevallos, and I. G. Wong. 1997. Microsporidial keratoconjunctivitis in a patient without human immunodeficiency virus infection. Am. J. Ophthalmol. 124:395-396. [DOI] [PubMed] [Google Scholar]
- 260.Sing, A., K. Tybus, J. Heesemann, and A. Mathis. 2001. Molecular diagnosis of an Enterocytozoon bieneusi human genotype C infection in a moderately immunosuppressed human immunodeficiency virus seronegative liver-transplant recipient with severe chronic diarrhea. J. Clin. Microbiol. 39:2371-2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Singh, M., G. J. Kane, L. Mackinlay, I. Quaki, E. H. Yap, B. C. Ho, L. C. Ho, and K. C. Lim. 1982. Detection of antibodies to Nosema cuniculi (Protozoa: Microsporidia) in human and animal sera by the indirect fluorescent antibody technique. Southeast Asian J. Trop. Med. Public Health 13:110-113. [PubMed] [Google Scholar]
- 262.Snowden, K., B. Daft, and R. W. Nordhausen. 2001. Morphological and molecular characterization of Encephalitozoon hellem in hummingbirds. Avian Pathol. 30:251-255. [DOI] [PubMed] [Google Scholar]
- 263.Snowden, K., and K. Logan. 1999. Molecular identification of Encephalitozoon hellem in an ostrich. Avian Dis. 43:779-782. [PubMed] [Google Scholar]
- 264.Snowden, K., K. Logan, and E. S. Didier. 1999. Encephalitozoon cuniculi strain III is a cause of encephalitozoonosis in both humans and dogs. J. Infect. Dis. 180:2086-2088. [DOI] [PubMed] [Google Scholar]
- 265.Snowden, K. F. 2004. Zoonotic microsporidia from animals and arthropods with a discussion of human infections, p. 123-134. In D. S. Lindsay and L. M. Weiss (ed.), Opportunistic infections: toxoplasma, sarcocystis, and microsporidia, vol. 9. Kluwer Academic Publishers, Boston, Mass.
- 266.Snowden, K. F., E. S. Didier, J. M. Orenstein, and J. A. Shadduck. 1998. Animal models of human microsporidial infections. Lab. Anim. Sci. 48:589-592. [PubMed] [Google Scholar]
- 267.Snowden, K. F., K. Logan, and D. N. Phalen. 2000. Isolation and characterization of an avian isolate of Encephalitozoon hellem. Parasitology 121:9-14. [DOI] [PubMed] [Google Scholar]
- 268.Sobottka, I., H. Albrecht, J. Schottelius, C. Schmetz, M. Bentfeld, R. Laufs, and D. A. Schwartz. 1995. Self-limited traveller's diarrhea due to a dual infection with Enterocytozoon bieneusi and Cryptosporidium parvum in an immunocompetent HIV-negative child. Eur. J. Clin. Microbiol. Infect. Dis. 14:919-920. [DOI] [PubMed] [Google Scholar]
- 269.Sobottka, I., H. Albrecht, G. S. Visvesvara, N. J. Pieniazek, P. Deplazes, D. A. Schwartz, R. Laufs, and H. A. Elsner. 1999. Inter- and intra-species karyotype variations among microsporidia of the genus Encephalitozoon as determined by pulsed-field gel electrophoresis. Scand. J. Infect. Dis. 31:555-558. [DOI] [PubMed] [Google Scholar]
- 270.Sobottka, I., K. Bartscht, P. Schafer, T. Weitzel, J. Schottelius, N. Kock, and R. Laufs. 2002. In vitro activity of polyoxin D and nikkomycin Z against Encephalitozoon cuniculi. Parasitol. Res. 88:451-453. [DOI] [PubMed] [Google Scholar]
- 271.Sobottka, I., D. A. Schwartz, J. Schottelius, G. S. Visvesvara, N. J. Pieniazek, C. Schmetz, N. P. Kock, R. Laufs, and H. Albrecht. 1998. Prevalence and clinical significance of intestinal microsporidiosis in human immunodeficiency virus-infected patients with and without diarrhea in Germany: a prospective coprodiagnostic study. Clin. Infect. Dis. 26:475-480. [DOI] [PubMed] [Google Scholar]
- 272.Sparfel, J. M., C. Sarfati, O. Liguory, B. Caroff, N. Dumoutier, B. Gueglio, E. Billaud, F. Raffi, J. M. Molina, M. Miegeville, and F. Derouin. 1997. Detection of microsporidia and identification of Enterocytozoon bieneusi in surface water by filtration followed by specific PCR. J. Eukaryot. Microbiol. 44:78S. [DOI] [PubMed] [Google Scholar]
- 273.Sprague, V. 1974. Nosema connori n. sp., a microsporidian parasite of man. Trans. Am. Microsc. Soc. 93:400-403. [PubMed] [Google Scholar]
- 274.Sridhar, M. S., and S. Sharma. 2003. Microsporidial keratoconjunctivitis in a HIV-seronegative patient treated with debridement and oral itraconazole. Am. J. Ophthalmol. 136:745-746. [DOI] [PubMed] [Google Scholar]
- 275.Sulaiman, I. M., C. Bern, R. Gilman, V. Cama, V. Kawai, D. Vargas, E. Ticona, A. Vivar, and L. Xiao. 2003. A molecular biologic study of Enterocytozoon bieneusi in HIV-infected patients in Lima, Peru. J. Eukaryot. Microbiol. 50:591-596. [DOI] [PubMed] [Google Scholar]
- 276.Sulaiman, I. M., R. Fayer, A. A. Lal, J. M. Trout, F. W. Schaefer III, and L. Xiao. 2003. Molecular characterization of microsporidia indicates that wild mammals harbor host-adapted Enterocytozoon spp. as well as human-pathogenic Enterocytozoon bieneusi. Appl. Environ. Microbiol. 69:4495-4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Sulaiman, I. M., R. Fayer, C. Yang, M. Santin, O. Matos, and L. Xiao. 2004. Molecular characterization of Enterocytozoon bieneusi in cattle indicates that only some isolates have zoonotic potential. Parasitol. Res. 92:328-334. [DOI] [PubMed] [Google Scholar]
- 278.Sulaiman, I. M., O. Matos, M. L. Lobo, and L. Xiao. 2003. Identification of a new microsporidian parasite related to Vittaforma corneae in HIV-positive and HIV-negative patients from Portugal. J. Eukaryot. Microbiol. 50:586-590. [DOI] [PubMed] [Google Scholar]
- 279.Suter, C., A. Mathis, R. Hoop, and P. Deplazes. 1998. Encephalitozoon hellem infection in a yellow-streaked lory (Chalcopsitta scintillata) imported from Indonesia. Vet. Rec. 143:694-695. [PubMed] [Google Scholar]
- 280.Svedhem, V., M. Lebbad, B. Hedkvist, C. Del Aguila, P. Hedman, R. Larsson, R. Navajas, and A. Aust-Kettis. 2002. Disseminated infection with Encephalitozoon intestinalis in AIDS patients: report of 2 cases. Scand. J. Infect. Dis. 34:703-705. [DOI] [PubMed] [Google Scholar]
- 281.Svedhem, V., M. Lebbad, J. Struve, B. Veress, E. Andstrom, A. Aust-Kettis, and E. Linder. 1998. Microsporidia in duodenal biopsies from 72 HIV-infected patients with abdominal complaints. APMIS 106:535-538. [DOI] [PubMed] [Google Scholar]
- 282.Svenungsson, B., T. Capraru, B. Evengard, R. Larsson, and M. Lebbad. 1998. Intestinal microsporidiosis in a HIV-seronegative patient. Scand. J. Infect. Dis. 30:314-316. [DOI] [PubMed] [Google Scholar]
- 283.Teachey, D. T., P. Russo, J. M. Orenstein, E. S. Didier, C. Bowers, and N. Bunin. 2004. Pulmonary infection with microsporidia after allogeneic bone marrow transplantation. Bone Marrow Transplant. 33:299-302. [DOI] [PubMed] [Google Scholar]
- 284.Theng, J., C. Chan, M. L. Ling, and D. Tan. 2001. Microsporidial keratoconjunctivitis in a healthy contact lens wearer without human immunodeficiency virus infection. Ophthalmology 108:976-978. [DOI] [PubMed] [Google Scholar]
- 285.Thomas, C., M. Finn, L. Twigg, P. Deplazes, and R. Thompson. 1997. Microsporidia (Encephalitozoon cuniculi) in wild rabbits in Australia. Aust. Vet. J. 75:808-810. [DOI] [PubMed] [Google Scholar]
- 286.Thurston-Enriquez, J. A., P. Watt, S. E. Dowd, R. Enriquez, I. L. Pepper, and C. P. Gerba. 2002. Detection of protozoan parasites and microsporidia in irrigation waters used for crop production. J. Food Prot. 65:378-382. [DOI] [PubMed] [Google Scholar]
- 287.Tocidlowski, M. E., T. E. Cornish, M. R. Loomis, and M. K. Stoskopf. 1997. Mortality in captive wild-caught horned puffin chicks (Fratercula corniculata). J. Zoo Wildl. Med. 28:298-306. [PubMed] [Google Scholar]
- 288.Tosoni, A., M. Nebuloni, A. Ferri, S. Bonetto, S. Antinori, M. Scaglia, L. Xiao, H. Moura, G. S. Visvesvara, L. Vago, and G. Costanzi. 2002. Disseminated microsporidiosis caused by Encephalitozoon cuniculi III (dog type) in an Italian AIDS patient: a retrospective study. Mod. Pathol. 15:577-583. [DOI] [PubMed] [Google Scholar]
- 289.Trammer, T., G. Chioralia, W. A. Maier, and H. M. Seitz. 1999. In vitro replication of Nosema algerae (Microsporidia), a parasite of anopheline mosquitoes, in human cells above 36° C. J. Eukaryot. Microbiol. 46:464-468. [DOI] [PubMed] [Google Scholar]
- 290.Trammer, T., F. Dombrowski, M. Doehring, W. A. Maier, and H. M. Seitz. 1997. Opportunistic properties of Nosema algerae (Microspora), a mosquito parasite, in immunocompromised mice. J. Eukaryot. Microbiol. 44:258-262. [DOI] [PubMed] [Google Scholar]
- 291.Troll, H., H. Marti, and N. Weiss. 1997. Simple differential detection of Entamoeba histolytica and Entamoeba dispar in fresh stool specimens by sodium acetate-acetic acid-formalin concentration and PCR. J. Clin. Microbiol. 35:1701-1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Tumwine, J. K., A. Kekitiinwa, N. Nabukeera, D. E. Akiyoshi, M. A. Buckholt, and S. Tzipori. 2002. Enterocytozoon bieneusi among children with diarrhea attending Mulago Hospital in Uganda. Am. J. Trop. Med. Hyg. 67:299-303. [DOI] [PubMed] [Google Scholar]
- 293.Tzipori, S., A. Carville, G. Widmer, D. Kotler, K. Mansfield, and A. Lackner. 1997. Transmission and establishment of a persistent infection of Enterocytozoon bieneusi, derived from a human with AIDS, in simian immunodeficiency virus-infected rhesus monkeys. J. Infect. Dis. 175:1016-1020. [DOI] [PubMed] [Google Scholar]
- 294.Undeen, A. H. 1975. Growth of Nosema algerae in pig kidney cell cultures. J. Protozool. 22:107-110. [DOI] [PubMed] [Google Scholar]
- 295.Undeen, A. H., and N. E. Alger. 1976. Nosema algerae: infection of the white mouse by a mosquito parasite. Exp. Parasitol. 40:86-88. [DOI] [PubMed] [Google Scholar]
- 296.Undeen, A. H., and D. A. Dame. 1987. Measurement of the effect of microsporidian pathogens on mosquito larval mortality under artificial field conditions. J. Am. Mosq. Control Assoc. 3:91-93. [PubMed] [Google Scholar]
- 297.Van Dellen, A. F., C. G. Stewart, and W. S. Botha. 1989. Studies of encephalitozoonosis in vervet monkeys (Cercopithecus pygerythrus) orally inoculated with spores of Encephalitozoon cuniculi isolated from dogs (Canis familiaris). Onderstepoort J. Vet. Res. 56:1-22. [PubMed] [Google Scholar]
- 298.Van Gool, T., C. Biderre, F. Delbac, E. Wentink-Bonnema, R. Peek, and C. P. Vivares. 2004. Serodiagnostic studies in an immunocompetent individual infected with Encephalitozoon cuniculi. J. Infect. Dis. 189:2243-2249. [DOI] [PubMed] [Google Scholar]
- 299.Van Gool, T., E. U. Canning, H. Gilis, M. A. Van den Bergh Weerman, J. K. M. Eeftinck Schattenkerk, and J. Dankert. 1994. Septata intestinalis frequently isolated from stool of AIDS patients with a new cultivation method. Parasitology 109:281-289. [DOI] [PubMed] [Google Scholar]
- 300.Van Gool, T., E. Luderhoff, K. J. Nathoo, C. F. Kiire, J. Dankert, and P. R. Mason. 1995. High prevalence of Enterocytozoon bieneusi infections among HIV-positive individuals with persistent diarrhoea in Harare, Zimbabwe. Trans. R. Soc. Trop. Med. Hyg. 89:478-480. [DOI] [PubMed] [Google Scholar]
- 301.Van Gool, T., F. Snijders, P. Reiss, J. K. M. Eeftinck Schattenkerk, M. A. Van den Bergh Weerman, J. F. W. M. Bartelsman, J. J. M. Bruins, E. U. Canning, and J. Dankert. 1993. Diagnosis of intestinal and disseminated microsporidial infections in patients with HIV by a new rapid fluorescence technique. J. Clin. Pathol. 46:694-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Van Gool, T., J. C. Vetter, B. Weinmayr, A. Van Dam, F. Derouin, and J. Dankert. 1997. High seroprevalence of Encephalitozoon species in immunocompetent subjects. J. Infect. Dis. 175:1020-1024. [DOI] [PubMed] [Google Scholar]
- 303.Van Heerden, J., N. Bainbridge, R. E. Burroughs, and N. P. Kriek. 1989. Distemper-like disease and encephalitozoonosis in wild dogs (Lycaon pictus). J. Wildl. Dis. 25:70-75. [DOI] [PubMed] [Google Scholar]
- 304.Vavra, J., and A. H. Undeen. 1970. Nosema algerae n. sp. (Cnisospora, Microsporida), a pathogen in a laboratory colony of Anophales stephensi Liston (Diptera, Culicidae). J. Protozool. 17:240-249. [DOI] [PubMed] [Google Scholar]
- 305.Vavra, J., A. T. Yachnis, J. A. Shadduck, and J. M. Orenstein. 1998. Microsporidia of the genus Trachipleistophora—causative agents of human microsporidiosis: description of Trachipleistophora anthropophthera n. sp. (Protozoa: Microsporidia). J. Eukaryot. Microbiol. 45:273-283. [DOI] [PubMed] [Google Scholar]
- 306.Visvesvara, G. S. 2002. In vitro cultivation of microsporidia of clinical importance. Clin. Microbiol. Rev. 15:401-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Visvesvara, G. S., M. Belloso, H. Moura, A. J. Da Silva, I. N. Moura, G. J. Leitch, D. A. Schwartz, P. Chevez-Barrios, S. Wallace, N. J. Pieniazek, and J. D. Goosey. 1999. Isolation of Nosema algerae from the cornea of an immunocompetent patient. J. Eukaryot. Microbiol. 46:10S. [PubMed] [Google Scholar]
- 308.Visvesvara, G. S., G. J. Leitch, A. J. Da Silva, G. P. Croppo, H. Moura, S. Wallace, S. Slemenda, D. A. Schwartz, D. Moss, R. T. Bryan, and N. J. Pieniazek. 1994. Polyclonal and monoclonal antibody and PCR-amplified small-subunit rRNA identification of a microsporidian, Encephalitozoon hellem, isolated from an AIDS patient with disseminated infection. J. Clin. Microbiol. 32:2760-2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Voglino, M. C., G. Donelli, P. Rossi, A. Ludovisi, V. Rinaldi, F. Goffredo, R. Paloscia, and E. Pozio. 1996. Intestinal microsporidiosis in Italian individuals with AIDS. Ital. J. Gastroenterol. 28:381-386. [PubMed] [Google Scholar]
- 310.Vossbrinck, C. R., M. D. Baker, E. S. Didier, B. A. Debrunner Vossbrinck, and J. A. Shadduck. 1993. Ribosomal DNA sequences of Encephalitozoon hellem and Encephalitozoon cuniculi: species identification and phylogenetic construction. J. Eukaryot. Microbiol. 40:354-362. [DOI] [PubMed] [Google Scholar]
- 311.Waller, T. 1979. Sensitivity of Encephalitozoon cuniculi to various temperatures, disinfectants and drugs. Lab. Anim. 13:227-230. [DOI] [PubMed] [Google Scholar]
- 312.Wanachiwanawin, D., K. Chokephaibulkit, P. Lertlaituan, J. Ongrotchanakun, P. Chinabut, and K. Thakerngpol. 2002. Intestinal microsporidiosis in HIV-infected children with diarrhea. Southeast Asian J. Trop. Med. Public Health 33:241-245. [PubMed] [Google Scholar]
- 313.Wanachiwanawin, D., S. Manatsathit, P. Lertlaituan, K. Thakerngpol, and P. Suwanagool. 1998. Intestinal microsporidiosis in HIV infected patients with chronic diarrhea in Thailand. Southeast Asian J. Trop. Med. Public Health 29:767-771. [PubMed] [Google Scholar]
- 314.Wanke, C. A., P. DeGirolami, and M. Federman. 1996. Enterocytozoon bieneusi infection and diarrheal disease in patients who were not infected with human immunodeficiency virus: case report and review. Clin. Infect. Dis. 23:816-818. [DOI] [PubMed] [Google Scholar]
- 315.Wasson, K., and R. L. Peper. 2000. Mammalian microsporidiosis. Vet. Pathol. 37:113-128. [DOI] [PubMed] [Google Scholar]
- 316.Watson, D. R. A., D. Asmuth, and C. A. Wanke. 1996. Environmental risk factors for acquisation of microsporidia in HIV-infected persons. In Proceedings of the 34th Annual Meeting of the Infectious Diseases Society of America, New Orleans, La., p. 67. Infectious Diseases Society of America, New Orleans, La.
- 317.Waywa, D., S. Kongkriengdaj, S. Chaidatch, S. Tiengrim, B. Kowadisaiburana, S. Chaikachonpat, S. Suwanagool, A. Chaiprasert, A. Curry, W. Bailey, Y. Suputtamongkol, and N. J. Beeching. 2001. Protozoan enteric infection in AIDS related diarrhea in Thailand. Southeast Asian J. Trop. Med. Public Health 2:151-155. [PubMed] [Google Scholar]
- 318.Weber, R., and R. T. Bryan. 1994. Microsporidial infections in immunodeficient and immunocompetent patients. Clin. Infect. Dis. 19:517-521. [DOI] [PubMed] [Google Scholar]
- 319.Weber, R., R. T. Bryan, R. L. Owen, C. M. Wilcox, L. Gorelkin, and G. S. Visvesvara. 1992. Improved light-microscopical detection of Microsporidia spores in stool and duodenal aspirates. N. Engl. J. Med. 326:161-166. [DOI] [PubMed] [Google Scholar]
- 320.Weber, R., R. T. Bryan, D. A. Schwartz, and R. L. Owen. 1994. Human microsporidial infections. Clin. Microbiol. Rev. 7:426-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Weber, R., P. Deplazes, M. Flepp, A. Mathis, R. Baumann, B. Sauer, H. Kuster, and R. Luthy. 1997. Cerebral microsporidiosis due to Encephalitozoon cuniculi in a patient with human immunodeficiency virus infection. N. Engl. J. Med. 336:474-478. [DOI] [PubMed] [Google Scholar]
- 322.Weber, R., P. Deplazes, and D. Schwartz. 2000. Diagnosis and clinical aspects of human microsporidiosis. Contrib. Microbiol. 6:166-192. [DOI] [PubMed] [Google Scholar]
- 323.Weber, R., H. Kuster, G. S. Visvesvara, R. T. Bryan, D. A. Schwartz, and R. Lüthy. 1993. Disseminated microsporidiosis due to Encephalitozoon hellem: pulmonary colonization, microhematuria, and mild conjunctivitis in a patient with AIDS. Clin. Infect. Dis. 17:415-419. [DOI] [PubMed] [Google Scholar]
- 324.Weber, R., B. Ledergerber, R. Zbinden, M. Altwegg, G. E. Pfyffer, M. A. Spycher, J. Briner, L. Kaiser, M. Opravil, C. Meyenberger, M. Flepp, et al. 1999. Enteric infections and diarrhea in human immunodeficiency virus-infected persons: prospective community-based cohort study. Arch. Intern. Med. 159:1473-1480. [DOI] [PubMed] [Google Scholar]
- 325.Weber, R., B. Sauer, M. A. Spycher, P. Deplazes, R. Keller, R. Ammann, J. Briner, and R. Lüthy. 1994. Detection of Septata intestinalis in stool specimens and coprodiagnostic monitoring of successful treatment with albendazole. Clin. Infect. Dis. 19:342-345. [DOI] [PubMed] [Google Scholar]
- 326.Weidner, E., E. U. Canning, C. R. Rutledge, and C. L. Meek. 1999. Mosquito (Diptera: Culicidae) host compatibility and vector competency for the human myositic parasite Trachipleistophora hominis (phylum microspora). J. Med. Entomol. 36:522-525. [DOI] [PubMed] [Google Scholar]
- 327.Weiss, L. M. 2000. Molecular phylogeny and diagnostic approaches to microsporidia. Contrib. Microbiol. 6:209-235. [DOI] [PubMed] [Google Scholar]
- 328.Weitzel, T., M. Wolff, J. Dabanch, I. Levy, C. Schmetz, G. S. Visvesvara, and I. Sobottka. 2001. Dual microsporidial infection with Encephalitozoon cuniculi and Enterocytozoon bieneusi in an HIV-positive patient. Infection 29:237-239. [DOI] [PubMed] [Google Scholar]
- 329.Wenker, C. J., J.-M. Hatt, D. Ziegler, A. Mathis, I. Tanner, and P. Deplazes. 2002. Microsporidiosis (Encephalitozoon spp.) of new world primates—an emerging disease? A seroepidemiological, pathological and therapeutical survey in the Zurich zoo. In Proceedings of the 4th Scientific Meeting of the European Association of Zoo and Wildlife Vets, Heidelberg, Germany, p. 503-508. European Association of Zoo and Wildlife Vets, Heidelberg, Germany.
- 330.Williams, B. A., R. P. Hirt, J. M. Lucocq, and T. M. Embley. 2002. A mitochondrial remnant in the microsporidian Trachipleistophora hominis. Nature 418:865-869. [DOI] [PubMed] [Google Scholar]
- 331.Wilson, J. M. 1979. Encephalitozoon cuniculi in wild European rabbits and a fox. Res. Vet. Sci. 26:114. [PubMed] [Google Scholar]
- 332.Wuhib, T., T. M. Silva, R. D. Newman, L. S. Garcia, M. L. Pereira, C. S. Chaves, S. P. Wahlquist, R. T. Bryan, R. L. Guerrant, Q. Sousa Ade, et al. 1994. Cryptosporidial and microsporidial infections in human immunodeficiency virus-infected patients in northeastern Brazil. J. Infect. Dis. 170:494-497. [DOI] [PubMed] [Google Scholar]
- 333.Xiao, L., L. Li, H. Moura, I. Sulaiman, A. A. Lal, S. Gatti, M. Scaglia, E. S. Didier, and G. S. Visvesvara. 2001. Genotyping Encephalitozoon hellem isolates by analysis of the polar tube protein gene. J. Clin. Microbiol. 39:2191-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Xiao, L., L. Li, G. S. Visvesvara, H. Moura, E. S. Didier, and A. A. Lal. 2001. Genotyping Encephalitozoon cuniculi by multilocus analyses of genes with repetitive sequences. J. Clin. Microbiol. 39:2248-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Yachnis, A. T., J. Berg, A. Martinez-Salazar, B. S. Bender, L. Diaz, A. M. Rojiani, T. A. Eskin, and J. M. Orenstein. 1996. Disseminated microsporidiosis especially infecting the brain, heart, and kidneys. Report of a newly recognized pansporoblastic species in two symptomatic AIDS patients. Am. J. Clin. Pathol. 106:535-543. [DOI] [PubMed] [Google Scholar]
- 336.Yee, R. W., F. O. Tio, J. A. Martinez, K. S. Held, J. A. Shadduck, and E. S. Didier. 1991. Resolution of microsporidial epithelial keratopathy in a patient with AIDS. Ophthalmology 98:196-201. [DOI] [PubMed] [Google Scholar]
- 337.Zeman, D. H., and G. B. Baskin. 1985. Encephalitozoonosis in squirrel monkeys (Saimiri sciureus). Vet. Pathol. 22:24-31. [DOI] [PubMed] [Google Scholar]