Abstract
Background
Against the backdrop of increasing population aging, the uncertainty and irreversibility of climate change have a significant impact on the health and healthcare burden of the elderly. However, it remains uncertain whether the multi-tiered medical insurance system disproportionately influences the health impacts of climate risks.
Methods
Using data from the China Health and Retirement Longitudinal Study (CHARLS) from 2011 to 2020, matched with urban climate risk variables, we employ a multi-dimensional panel fixed effects model and an instrumental variable model to examine the impact of climate risks on the health of the middle-aged and elderly, while also investigating the unequal effects of the multi-tiered medical insurance system.
Results
Climate risks significantly worsened the self-reported health of the middle-aged and elderly (β = 0.073, P = 0.089), and increased both total medical costs (β = 2.570, P = 0.012) and out-of-pocket expenses (β = 2.652, P = 0.003). Notably, the increases in hospitalization costs (β = 0.721, P = 0.004) and out-of-pocket hospitalization expenses (β = 0.706, P = 0.036) are particularly prominent. The current multi-tiered medical insurance system results in unequal impacts of climate risks on health and medical costs. Specifically, urban employee medical insurance and commercial medical insurance effectively improve the health outcomes of elderly individuals affected by climate risks. Urban residents’ medical insurance significantly reduces both total medical costs and out-of-pocket expenses for the elderly, whereas the new rural cooperative medical insurance shows no significant mitigating effect. Additionally, there is no evidence to suggest that the integration of urban and rural resident medical insurance can reduce the medical burden on rural elderly populations caused by climate risks. Our long-term projections indicate that, under both the SSP245 and SSP585 scenarios, the increase in elderly healthcare costs due to climate risks is irreversible. However, restrictive climate policies would yield significant health benefits, potentially reducing per capita medical costs for the elderly by nearly 50%.
Conclusions
The decentralized multi-tier medical insurance system leads to significant inequality in the health impacts of climate risks. Our study emphasizes the critical role of reforming the existing social medical insurance system and implementing climate policies to protect the health of elderly populations.
Keywords: Climate risks, Middle-aged and elderly populations, Healthcare costs, Climate policies
Introduction
Since the industrial and post-industrial eras, global economic growth has led to high-pollution and high-emission activities, resulting in increased climate instability and a higher frequency of extreme weather events [1]. Climate change, characterized primarily by global warming, and its governance have become central topics of current research. On a global scale, by 2020, the average global temperature had increased by approximately 1.15 °C compared to the period 1850–1900, with recent years accounting for about 15% of the temperature rise observed over the past three centuries [2]. Extreme climate-related disasters are increasing worldwide, with the intensity, frequency, and geographic extent of extreme events such as heatwaves, floods, droughts, and storms rapidly rising. China is a highly sensitive and significantly affected region for climate change. In recent years, the frequency of extreme weather events has increased, affecting wider areas, with greater intensity. Record-breaking events and unforeseen sudden occurrences have also become more common. The frequency of regional extreme heavy rainfall, widespread heatwaves, prolonged extreme droughts, and high-impact cold waves has risen, prompting widespread public concern and ongoing discussion.
The health impacts of various extreme climate events associated with climate risks are significant, with some studies identifying climate risk as the greatest threat to global public health [3]. Current research exploring the relationship between climate risks and health primarily focuses on the following areas: First, many studies use extreme heat as a proxy for climate risk to analyze its negative impact on individuals’ physical or mental health [4–6]. These studies confirm the causal relationship between extreme heat and individual health by defining different temperature ranges or calculating the cumulative number of hot days. Among them, the health issues of vulnerable groups such as the elderly and infants have received particular attention. In the short term, studies have shown that increased exposure to higher temperature ranges and the rising number of hot days significantly drive the probability and mortality rate of cardiovascular and other diseases among the elderly in the current period [7]. Regarding mental health, studies have found that extreme climate events lead the elderly to engage in more sedentary activities and experience a decline in sleep quality, which increases the likelihood of developing mental health issues such as depression and anxiety [8]. However, the health risks associated with extreme climate events are not limited to the short term. In the long run, the sudden occurrence of disasters like extreme temperatures has a cumulative and progressive effect on health. Studies indicate that, under the dual pressures of an aging population and increasing climate change uncertainty, the prevalence of chronic diseases among the elderly is expected to rise in the future [9]. Moreover, the health risks caused by extreme climate events may also be transmitted across generations. Studies have found that exposure to extreme temperatures during pregnancy not only worsens the mother’s health but also leads to poorer health outcomes for the offspring when they reach reproductive age [10, 11].
Second, extreme climate events are driving a continuous increase in public health expenditures and individual healthcare costs. From the perspective of public health expenditures, the uncertainties associated with extreme climate events may increase short-term emergency medical service costs and long-term maintenance expenses for the public sector, thereby putting greater pressure on government fiscal balance and sustainability [12, 13]. The increasing frequency of extreme climate events forces governments at all levels to factor in rising climate-related healthcare costs and the implementation of adaptive climate policies when preparing fiscal expenditure budgets. Moreover, as climate risks evolve, public demand for public sector health expenditures continues to grow. In terms of individual healthcare costs, studies have shown that both extreme heat and extreme cold significantly increase healthcare expenses for middle-aged and elderly individuals. However, exposure to extreme heat results in higher medical costs compared to exposure to extreme cold [14]. Some scholars have also estimated the long-term impact of extreme climate events on individuals’ out-of-pocket healthcare expenses. While these estimates cover different time periods and geographic areas, the consistent conclusion is that climate risks have a significant long-term effect on out-of-pocket costs [10, 15].
It is noteworthy that, although climate risks negatively affect individual health and healthcare costs, the current multi-tiered medical insurance system may result in inequalities. China has established a preliminary multi-tiered social medical insurance system, covering approximately 1.3 billion people. The scope of social basic medical insurance includes urban employee basic medical insurance (UEMI), urban resident basic medical insurance(URMI), and the new rural cooperative medical insurance (NRCMI). These basic medical insurance schemes cover urban employed populations, urban non-employed populations, and rural populations, each operating independently with distinct boundaries. Given the significant household registration characteristics of China’s social basic medical insurance [16, 17], the effectiveness of the multi-tiered insurance system may vary considerably. On one hand, in response to climate change risks, the multi-tiered medical insurance system may provide basic protection for individual health, acting as a “safety net” [18]. Such as, the basic medical insurance system can effectively improve the basic healthcare rights of impoverished and vulnerable groups. On the other hand, the current medical insurance system may have a “pro-rich” effect. In particular, the traditional model, based on household registration for insurance enrollment, per capita contributions, and unclear coverage boundaries, results in issues such as inequitable funding, limited coverage capacity, and significant disparities in benefits [19, 20]. As a result, differentiated insurance benefits may lead to unequal health impacts of climate risks on middle-aged and elderly populations.
To address the potential inequities caused by the fragmented multi-tiered medical insurance system, the Chinese government issued a healthcare reform document in 2016, aiming to gradually integrate URMI and the NRCMI across the country. The core elements of the urban-rural medical insurance integration (URMII) focus on unified departmental management, funding policies, coverage scope, benefits, insurance catalog, designated service providers, and fund management [21, 22]. At the same time, the central government has instructed local governments at all levels to promptly clarify integration plans and deployments, and to develop specific integration strategies tailored to regional differences. During the implementation of integration, governments at all levels typically adopt a “single system with multiple levels” approach to insurance contributions and benefit services, based on provincial or municipal coordination. The main integration goal is to ensure that contribution and benefit levels are similar to those of the NRCMI and URMI after integration. There are varying conclusions in current research regarding the effects of URMII. Some studies indicate that the integration of urban-rural medical insurance has effectively improved the health levels of urban and rural residents, particularly benefiting rural populations and residents in western China [23]. Additionally, research from a provincial coordination perspective has demonstrated the positive impact of URMII on the mobile population [24]. However, some studies have found that, after implementing the URMII plan, China did not reduce the inequality in healthcare payments between urban and rural households in the short term. The actual outcomes have fallen short of the expected goals [25, 26].
In summary, existing research has discussed the negative impacts of climate risks on individual health and healthcare costs from different perspectives, but there is room for further exploration. First, current research primarily estimates climate risks using extreme temperatures as a proxy variable, such as using heat indicators to represent extreme weather, while overlooking the effects of other types of climate risks. Specifically, in China, extreme high-temperature days typically occur in the temperate and subtropical regions during the summer and autumn. Relying solely on heat indicators to measure climate risk may introduce spatial and temporal biases compared to actual conditions. Second, existing research on the threats posed by climate change to public health in China has not incorporated the impact of the multi-tiered medical insurance system into the analytical framework. This is particularly important for middle-aged and elderly populations, for whom participation in effective health insurance is a key factor in ensuring basic living standards and health outcomes. Differentiated medical benefits may have varying moderating effects on climate risks, yet this issue has not been addressed in existing research. Third, while existing studies have estimated the relationship between extreme temperatures and long-term individual healthcare costs, these predictions may significantly underestimate the actual impact of climate risks. Additionally, many of these studies use relatively short time frames for their estimates.
Based on this, our study uses five waves of data from the CHARLS between 2011 and 2020, paired with city-level indicators, to estimate the impact of climate risks on the health and healthcare costs of the middle-aged and elderly population. The marginal contributions of our research are primarily in the following areas: First, we employed a multidimensional composite climate risk indicator. Unlike studies that use single-dimensional extreme climate indicators, we utilized daily-level temperature and precipitation data at the city level. Based on standards published by China’s climate industry, we estimated the annual average number of extreme high-temperature, low-temperature, precipitation, and drought days in the sample cities as proxies for the composite climate risk indicator. This approach allows our study to accurately estimate the actual impact of climate change, enriching the research on the relationship between climate change and health costs. Second, we incorporate the multi-tiered medical insurance system into our research framework. Specifically, we examine whether participation in different types of social basic medical insurance and the URMII policies have unequal effects on mitigating the health and healthcare costs of middle-aged and elderly populations due to climate risks. These findings contribute to the development of targeted social medical insurance reform measures and health protection strategies for the middle-aged and elderly population in the context of both climate change and demographic aging, thereby filling a gap in existing research. Finally, we provide a long-term forecast of the relationship between climate risk changes and healthcare costs for the middle-aged and elderly population. We use future climate projections based on different climate policy intensities and shared socio- economic scenarios, combined with the temperature control targets of future climate policies, to estimate the long-term trends in healthcare costs for the middle-aged and elderly population caused by climate risks.
The structure of this study is as follows: “Theoretical analysis” section describes how climate risk affects health factors. “Methods and data” section introduces the methods and data variables used in our research. “Results” section presents the empirical results and tests related to climate risks and health variables. “The long-term impact of climate risk on medical costs” section estimates the long-term impact of climate risks on healthcare costs. “Discussion” section provides the discussion. “Conclusion” section concludes the study.
Theoretical analysis
By introducing the health production function, we theoretically explain how climate risks affect individual health and healthcare costs. The health production function suggests that an individual’s health outcome (H) depends on health inputs (I), external environment (E), and a set of individual characteristics (C). Therefore, the health outcome can be expressed as Eq. (1):
 |
1 |
In this context, f represents the health production function, which satisfies the conditions of ∂H/∂I > 0, ∂H/∂E > 0. Assuming that R denotes climate risks, such as extreme heat or heavy rainfall, which can disrupt the external environment E, the health outcome H can be expressed as Eq. (2):
 |
2 |
In this case, the external environment E is a function of climate risk R. By taking the partial derivative of Eq. (2) with respect to R, we obtain:
 |
3 |
Since climate risk R negatively impacts the external environment E, leading to ∂E/∂R < 0, which further results in ∂H/∂R < 0, it can be concluded that an increase in climate risk will reduce individual health outcomes. Considering healthcare cost investment, as individuals aim to maximize their health level or minimize health losses, the health cost function C(I) is incorporated into the model:
 |
4 |
In this case, C(I) represents the cost function of health investment, which satisfies ∂C/∂X > 0, while L(H) is the utility function of health loss, which satisfies ∂L/∂H < 0. By considering the first-order condition, we obtain:
 |
5 |
When climate risk R increases, individual health deteriorates. As a response, individuals will increase their investment in health inputs I to mitigate health damage.
 |
6 |
When health levels decline, utility decreases, leading to ∂2L/∂H2 < 0. Since ∂H/∂R > 0, we can derive:
 |
7 |
Based on Eq. (7), when climate risk R increases, individuals will increase their health investment I to reduce health losses. Further considering health costs (HC), it consists of two components:
 |
8 |
Here, C(I(R)) represents the medical costs caused by climate risks, while D(H(R)) reflects the costs associated with early retirement and other expenses due to deteriorating health. By taking the derivative of Eq. (8) with respect to R, we obtain:
 |
9 |
In this case, ∂I/∂R > 0, and ∂D/∂H > 0. We can derive:
 |
10 |
According to Eq. (10), when climate risk R increases, individual healthcare costs will rise. Considering the individual’s health utility U over the entire life cycle, health investment H is incorporated into the life-cycle health utility function:
 |
11 |
Here, U represents the individual’s health utility over the entire life cycle, p is the discount rate, and u (H) is the health utility function. By taking the derivative of Eq. (11) with respect to R, we obtain:
 |
12 |
Therefore, when climate risk R increases, an individual’s health utility over the entire life cycle will decrease.
Methods and data
Data sources
The data consists of two parts. The first part of the data includes micro-level data on individual health status and healthcare costs, derived from the CHARLS, conducted jointly by Wuhan University and Peking University from 2011 to 2020. The choice of CHARLS is based on two reasons: First, CHARLS collects high-quality micro-level data on households and individuals aged 45 and above in China, including key data required for our study, such as individual healthcare expenditures, medical insurance participation, and health status. Second, CHARLS allows matching data at the city level rather than the provincial level, enabling us to pair it with regional characteristics such as climate risks and economic development. This enhances the reliability of our research.
The second part of the data includes city-level climate and socio-economic indicators. The temperature and precipitation data used to calculate climate risk are sourced from daily observational data provided by the China National Meteorological Science Data Center (CNMSDC), with a spatial resolution of 0.5 × 0.5. We calculated a composite climate risk index based on the defined thresholds for various climate risks. Indicators such as economic development level and industrial characteristics are derived from the urban statistical yearbook. Additionally, we use per capita carbon emission intensity as an instrumental variable for the climate risk index to address the endogeneity issue. The raw carbon emission data is sourced from the annual indicators provided by the Global Atmospheric Research Emissions Database (EDGAR), formatted as raster data with a spatial resolution of 0.1 × 0.1. We used Arcgis to match this data with the sample city locations.
Statistical analysis
The panel two-way fixed effects model is an effective method for estimating treatment effects with multi- individual, multi-time data. The time fixed effects account for shocks that vary over time but not across individuals, while individual fixed effects capture characteristics that vary across individuals but not over time [27]. Based on existing research, we establish a panel two-way fixed effects model to estimate the impact of climate risk on individual health and costs, as shown in Eq. (13):
 |
13 |
where, i represents the individual, and t represents time; Hea refers to a set of dependent variables, including self-reported health, total medical expenses, and out-of-pocket expenses; CR is the climate risk index; and X represents a set of control variables, including individual, household, and regional characteristics. β1 is the coefficient to be estimated. Additionally, it is considered that the cost of individual health maintenance may be related to economic factors, with regions experiencing better economic development generally having higher health maintenance costs. Furthermore, studies suggest that the industries driving economic growth are related to carbon emissions activities, which could lead to increased carbon emissions, thereby exacerbating climate risks [28]. Therefore, in this study, there may be a reverse causality between climate risk and health costs, necessitating the consideration of endogeneity issues. Drawing on existing research, we use climate policy uncertainty as an instrument for urban climate risk [29] to perform robustness checks. The instrumental variable regression model is given by the following equation:
 |
14 |
 |
15 |
where, IV represents the instrument for climate risk;  the coefficient from the first-stage regression;
the coefficient from the first-stage regression;  is the coefficient from the second-stage regression. To investigate whether the multi-tiered medical insurance system effectively moderates the impact of climate risk on self-reported health and medical expenses, we establish a moderation model to examine whether differentiated insurance participation plays a moderating role. The moderation effect model is shown in Eq. (16):
is the coefficient from the second-stage regression. To investigate whether the multi-tiered medical insurance system effectively moderates the impact of climate risk on self-reported health and medical expenses, we establish a moderation model to examine whether differentiated insurance participation plays a moderating role. The moderation effect model is shown in Eq. (16):
 |
16 |
where, Ins represents a set of moderating variables, including participation in UEMI, URMI, NRCMI, commercial medical insurance (CMI), and whether the city has implemented the URMII policy.
Variable selection
The dependent variables are health status and medical expenses. Health status is measured using self-reported health (self_hea), while medical expenses are represented by total medical costs (lncost) and out-of-pocket expenses (lnselfcost). The self-reported health status is derived from the individual health survey in CHARLS. Respondents answer using categories such as “very good,” “good,” “fair,” “poor,” and “very poor,” with scores ranging from 1 to 5. A higher score indicates worse self-reported health. Medical expenses are represented by total medical costs and out-of-pocket costs. Specifically, total medical costs are the sum of inpatient and outpatient costs, while out-of-pocket costs include the sum of inpatient and outpatient out-of-pocket expenses. The data on medical expenses related to inpatient and outpatient services come from the micro-survey of CHARLS.
The independent variable is the climate risk index (lnCR). Existing research indicates that climate risk primarily manifests as the uncertainty and shocks caused by various extreme climate events. In line with previous studies, we use the annual number of days of four types of extreme climate events—extreme high temperatures, extreme low temperatures, extreme precipitation, and extreme drought-to represent the urban climate risk index. Specifically, following existing research, we standardize the annual occurrence days of the four extreme climate events and calculate their average as the climate risk index. For defining the thresholds of different types of extreme climate events, we referred to the standards issued by China’s climate sector. We use percentiles to determine the extreme thresholds. This involves selecting the extreme and second extreme values of the corresponding indicators within the climate reference period, constructing a sample sequence, and using the 5th and 95th percentiles as the extreme thresholds. Additionally, compared to methods that define threshold ranges, using the annual occurrence days as a climate risk measure has the advantage of incorporating the impacts of different types of climate events into the same model for estimation. The calculation process for the climate risk index is shown in the following formula (17):
 |
17 |
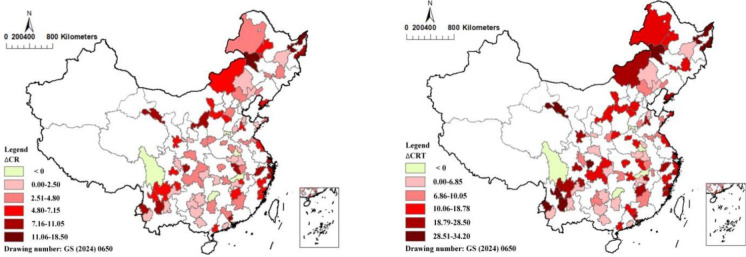
where, HTit and LTit represent the number of extreme high and low temperature days, respectively, in city i in year t; EPit and EDit represent the number of extreme precipitation and drought days, respectively, in city i in year t; To account for potential biases in the calculation of these indicators, we further use the cumulative number of extreme climate event days for different types of climate risks as alternative variables for robustness checks. As shown in Fig. 1, the climate risk index for the sample cities from 2011 to 2020 generally increased under different measurement methods, indicating that the climate risk in cities has been gradually increasing during the study period.
Fig. 1.
Change of climate risk in sample cities during 2011–2020 (L: ∆CR, R: ∆CRT)
The control variables include individual characteristics, family characteristics, and socio-economic traits of the region to which the respondent belongs. Individual characteristics include gender, marital status (married), retirement status (retire), education level (edu), chronic disease status (chr), age, life satisfaction (sat), BMI (bmi), and sleep duration (sleep); Family characteristics include per-capita income(lnincome), household size (size), household registration type (reg); Socio-economic characteristics include economic development level and industrial structure, represented by per capita GDP (pregdp) and the share of the tertiary sector in total output (ind_str).
The moderating variables include whether the individual participates in UEMI, URMI, NRCMI, CMI, and whether they have experienced the URMII policies.
Table 1 reports the descriptive statistics for the full sample, urban sample, and rural sample. All climate risk and regional characteristic indicators in the study are matched based on city codes and the CHARLS data. The core variables of interest are individual health status and medical expenditures. After excluding outliers and missing values, the final balanced panel dataset consists of 3,135 samples. According to Table 1, the average total medical expenses and out-of-pocket costs for rural residents are slightly higher than those of urban residents. The overall mean self-assessed health score for the full sample is 2.98 (close to 3), indicating that the general health status is moderate, with rural residents reporting slightly better self-assessed health than urban residents. Additionally, the gender distribution is 46.10% male and 53.90% female. The proportions of urban and rural households are 67.77% and 32.23%, respectively. The proportion of married individuals is 77.43%, while 12.59% are retired and 53.5% are aged 60 or older. Of the sample, 90.54% are enrolled in public basic health insurance, and only 5.53% have purchased commercial medical insurance.
Table 1.
Describes and statistics
| Variables | Full sample | Urban | Rural | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Min | Max | N | Mean | Min | Max | N | Mean | Min | Max | |
| lncost | 3,135 | 17.17 | 5.298 | 23.14 | 2,130 | 17.02 | 5.298 | 23.14 | 1,005 | 17.44 | 11.59 | 23.04 |
| lnselfcost | 3,135 | 15.36 | 5.192 | 22.92 | 2,130 | 15.30 | 5.192 | 21.51 | 1,005 | 15.50 | 10.98 | 22.92 |
| self_hea | 3,135 | 2.980 | 1.000 | 5.000 | 2,130 | 2.922 | 1.000 | 5.000 | 1,005 | 3.098 | 1.000 | 5.000 |
| lnCR | 3,135 | 3.282 | 2.416 | 4.259 | 2,130 | 3.264 | 2.416 | 3.962 | 1,005 | 3.319 | 2.416 | 4.259 |
| lnCRT | 3,135 | 4.668 | 3.803 | 5.646 | 2,130 | 4.650 | 3.803 | 5.349 | 1,005 | 4.706 | 3.803 | 5.646 |
| lnincome | 3,135 | 8.412 | 4.605 | 11.98 | 2,130 | 9.124 | 4.805 | 11.98 | 1,005 | 8.081 | 4.605 | 9.098 |
| married | 3,135 | 0.865 | 0.000 | 1.000 | 2,130 | 0.863 | 0.000 | 1.000 | 1,005 | 0.867 | 0.000 | 1.000 |
| retire | 3,135 | 0.125 | 0.000 | 1.000 | 2,130 | 0.042 | 0.000 | 1.000 | 1,005 | 0.303 | 0.000 | 1.000 |
| sat | 3,135 | 3.196 | 1.000 | 5.000 | 2,130 | 0.794 | 1.000 | 5.000 | 1,005 | 3.336 | 0.000 | 5.000 |
| lnage | 3,135 | 4.112 | 3.807 | 4.595 | 2,130 | 4.118 | 3.806 | 4.595 | 1,005 | 4.114 | 3.807 | 4.585 |
| edu | 3,135 | 1.967 | 1.000 | 4.000 | 2,130 | 1.804 | 1.000 | 4.000 | 1,005 | 1.142 | 1.000 | 4.000 |
| reg | 3,135 | 0.678 | 0.000 | 1.000 | 2,130 | 1.000 | 1.000 | 1.000 | 1,005 | 0.000 | 0.000 | 0.000 |
| chr | 3,135 | 0.777 | 0.000 | 1.000 | 2,130 | 0.781 | 0.000 | 1.000 | 1,005 | 0.776 | 0.000 | 1.000 |
| lnbmi | 3,135 | 3.159 | 1.684 | 7.769 | 2,130 | 3.146 | 1.684 | 7.769 | 1,005 | 3.187 | 2.563 | 7.423 |
| sleep | 3,135 | 6.163 | 0.156 | 24.00 | 2,130 | 6.177 | 0.156 | 23.00 | 1,005 | 6.120 | 0.156 | 24.00 |
| size | 3,135 | 3.212 | 1.000 | 16.00 | 2,130 | 3.213 | 1.000 | 16.00 | 1,005 | 3.189 | 1.000 | 15.00 |
| gender | 3,135 | 0.461 | 0.000 | 1.000 | 2,130 | 0.470 | 0.000 | 1.000 | 1,005 | 0.452 | 0.000 | 1.000 |
| lnind_str | 3,135 | 3.730 | 3.140 | 4.287 | 2,130 | 3.777 | 3.140 | 4.287 | 1,005 | 3.710 | 3.140 | 4.273 |
| lnpregdp | 3,135 | 10.56 | 8.842 | 13.05 | 2,130 | 10.59 | 8.862 | 13.05 | 1,005 | 10.73 | 8.842 | 12.13 |
| UEMI | 3,135 | 0.482 | 0.000 | 1.000 | 2,130 | 0.502 | 0.000 | 1.000 | 1,005 | 0.193 | 0.000 | 1.000 |
| URMI | 2,130 | 0.734 | 0.000 | 1.000 | 2,130 | 0.734 | 0.000 | 1.000 | 1,005 | 0.000 | 0.000 | 0.000 |
| NRCMI | 1,005 | 0.752 | 0.000 | 1.000 | 2,130 | 0.000 | 0.000 | 0.000 | 1,005 | 0.752 | 0.000 | 1.000 |
| CMI | 3,135 | 0.022 | 0.000 | 1.000 | 2,130 | 0.035 | 0.000 | 1.000 | 1,005 | 0.016 | 0.000 | 1.000 |
Results
The impact of climate risks on the health and healthcare costs
After controlling for individual, household, and regional characteristics, as well as implementing a two-way fixed effects model, the baseline regression results are presented in (Table 2). The results indicate that, with regard to self-reported health, climate risks significantly exacerbate the respondents’ health conditions (self_hea), with an estimated coefficient of 0.073 (significant at the 10% level). This suggests that as climate risks increase, the health damages caused to the middle-aged and elderly population by extreme weather events become more severe. Regarding healthcare costs, the results show that climate risks significantly increase the costs associated with health maintenance. Specifically, when climate risk increases by 1%, individuals’ total medical costs (lncost) and out-of-pocket expenses (lnselfcost) will rise by 2.570% and 2.652%, respectively. It can be observed that the increase in urban climate risk significantly exacerbates the non-health conditions and healthcare costs of the middle-aged and elderly population, which is consistent with existing research findings. Previous studies have shown that the disaster impacts of climate risks are uncertain and difficult to effectively prevent, significantly increasing the health damages and healthcare costs individuals are exposed to [14, 30].
Table 2.
The impact of climate risks on individual health and cost of healthcare
| Variables | self_hea | lncost | lnselfcost | |||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| lnCR | 0.046 | 0.073* | 1.545*** | 2.570** | 1.345*** | 2.652*** |
| (0.033) | (0.043) | (0.531) | (0.995) | (0.468) | (0.852) | |
| lnincome | −0.092 | −1.117 | −0.451 | |||
| (0.087) | (2.082) | (1.685) | ||||
| married | 0.112** | 1.704** | 1.688*** | |||
| (0.047) | (0.846) | (0.549) | ||||
| retire | −0.007 | −0.277 | 0.436 | |||
| (0.057) | (0.738) | (0.823) | ||||
| sat | 0.132*** | −0.115 | −0.146 | |||
| (0.014) | (0.211) | (0.282) | ||||
| lnage | −0.897 | 66.54 | 71.47* | |||
| (1.426) | (44.74) | (41.51) | ||||
| edu | −0.034 | −7.730*** | −6.710*** | |||
| (0.068) | (0.603) | (1.016) | ||||
| reg | 0.029 | −0.124 | −0.127 | |||
| (0.035) | (0.119) | (0.144) | ||||
| chr | −0.109*** | −1.823** | −0.715 | |||
| (0.035) | (0.850) | (0.683) | ||||
| lnbmi | 0.087 | 3.145 | −2.883 | |||
| (0.125) | (5.181) | (4.576) | ||||
| sleep | 0.028*** | −0.115 | −0.121 | |||
| (0.005) | (0.190) | (0.209) | ||||
| size | −0.007 | 0.051 | 0.032 | |||
| (0.007) | (0.142) | (0.111) | ||||
| gender | −0.403 | −1.302 | −1.503 | |||
| (0.392) | (1.278) | (2.011) | ||||
| constant | 2.811*** | 6.526 | 11.74*** | −245.5* | 10.74*** | −257.9** |
| (0.116) | (5.929) | (1.812) | (118.4) | (1.596) | (175.6) | |
| con_s | No | Yes | No | Yes | No | Yes |
| year | Yes | Yes | Yes | Yes | Yes | Yes |
| ind_l | Yes | Yes | Yes | Yes | Yes | Yes |
| obs | 3,095 | 3,095 | 3,095 | 3,095 | 3,135 | 3,135 |
| R2 | 0.003 | 0.071 | 0.046 | 0.310 | 0.034 | 0.319 |
*, **, and *** represent significance at the 10%, 5%, and 1% levels, respectively. The values in parentheses are clustered robust standard errors at the city level
A possible explanation for this is that, on the one hand, the increase in climate risks directly threatens and harms individuals’ physical or mental health, especially among vulnerable groups such as the elderly, who are more sensitive to external environmental shocks. Studies have shown that the occurrence of extreme heat and other climate events is significantly positively correlated with the incidence of underlying diseases and the increased mortality risk among the elderly population [31]. Additionally, climate risks may reduce outdoor activities and social interactions, which can increase the likelihood of psychological conditions such as anxiety and depression in older adults [32]. On the other hand, climate risks are associated with higher medical costs. Sudden extreme climate events often lead to an increase in defensive behaviors and hospitalization rates, which consequently raises healthcare costs and health expenditures for the middle-aged and elderly population [15].
Based on the above findings, we decompose the total medical costs and out-of-pocket costs for the middle-aged and elderly population. The total costs include inpatient (lninc_cost) and outpatient costs (lnout_cost), while out-of-pocket costs include inpatient (lnself_inp) and outpatient self-paid expenses (lnself_out). Table 3 presents the results of the disaggregated regressions. It can be seen that climate risk leads to a 0.721% increase in lninc_cost (significant at the 1% level), and a 0.706% increase in lnself_inp (significant at the 5% level). As for outpatient costs, the estimated results for both lnout_cost and lnself_out are not statistically significant, indicating that climate risk does not significantly increase the medical expenses for the elderly in outpatient settings. Furthermore, we examine whether climate risk has differential impacts on inpatient and outpatient behaviors. The results show that the number of inpatient days (lnnum_inp) for the elderly significantly increases by 0.238% (significant at the 10% level), while there is no significant effect on the number of outpatient visits (lnnum_out) in the same period. These findings suggest that the health damage caused by climate risk for the elderly may be more likely to translate into direct physiological harm, thereby increasing medical costs associated with inpatient care. This contrasts with studies that consider only extreme heat as a proxy for climate risk, as the health damage caused by extreme heat may have a gradual cumulative effect, unlike sudden disasters such as extreme precipitation, which typically cause more immediate and acute harm [33, 34].
Table 3.
Effects of climate risks on inpatient and outpatient costs
| Variables | lninc_cost | lnself_inp | lnnum_inp | lnout_cost | lnself_out | lnnum_out |
|---|---|---|---|---|---|---|
| (7) | (8) | (9) | (10) | (11) | (12) | |
| lnCR | 0.721*** | 0.706** | 0.238* | 0.027 | 0.054 | 0.043 |
| (0.246) | (0.344) | (0.134) | (0.291) | (0.284) | (0.230) | |
| constant | 3.120 | −79.04 | −13.30 | −14.81 | −27.68 | −32.57 |
| (54.88) | ( 67.15) | (28.88) | (47.75) | (52.93) | (52.72) | |
| con_s | Yes | Yes | Yes | Yes | Yes | Yes |
| year | Yes | Yes | Yes | Yes | Yes | Yes |
| ind_l | Yes | Yes | Yes | Yes | Yes | Yes |
| obs | 3,013 | 3,135 | 3,135 | 3105 | 3,135 | 3,135 |
| R2 | 0.114 | 0.074 | 0.042 | 0.071 | 0.057 | 0.062 |
*, **, and *** represent significance at the 10%, 5%, and 1% levels, respectively. The values in parentheses are clustered robust standard errors at the city level
Robustness test
Table 4 reports the results of four robustness checks. First, the measure of urban climate risk is altered. This study uses the cumulative number of annual extreme climate events as a substitute for the average measure, addressing potential biases in the latter. Second, regional characteristic variables are included. Building on the baseline regression results, we examine the impact of urban economic development and industrial structure on self-rated health and healthcare costs for the middle-aged and elderly population. Third, we conduct an instrumental variable regression. The climate policy uncertainty is used as an instrumental variable for urban climate risk, overcoming potential bidirectional causality that could lead to estimation bias between the explanatory and outcome variables. Since the number of instrumental variables is equal to the number of endogenous variables, the issue of over-identification does not arise. We perform tests for weak instruments and under-identification. The results in Table 4 show that the F-statistics for the first-stage regressions are all greater than 10, and the Cragg-Donald Wald F-statistics exceed the critical value at the 10% significance level. This indicates a strong correlation between climate policy uncertainty and climate risk. The p-values of the LM statistic are all 0.000, leading to the rejection of the under-identification hypothesis. Therefore, our instrumental variables are identified. Fourth, we consider individual-level clustered robust standard errors and regional fixed effects. We perform the test using clustered robust standard errors at the individual level, which assume that health variables for individual samples exhibit autocorrelation only over time. Additionally, based on the regional division standards set by the National Bureau of Statistics of China, we categorize the sample regions into East China, Central China, Northeast, Northwest, North China, Southwest, and South China, taking into account factors such as geographic location, climate conditions, and economic development. This generates regional fixed effects to control for the impact of unchanging regional characteristics on individual health across all time periods. As shown in Table 4, even when these factors are considered, the estimation results remain significant. The results confirming the robustness and reliability of the estimates from Eq. (13).
Table 4.
Robustness test
| Variables | Proxy variable | Regional variable | ||||
|---|---|---|---|---|---|---|
| self_hea | lncost | lnselfcost | self_hea | lncost | lnselfcost | |
| lnCR | 0.083** | 2.735*** | 2.700*** | 0.084** | 2.591*** | 2.611*** |
| (0.041) | (0.974) | (0.768) | (0.042) | (0.917) | (0.949) | |
| constant | 4.275 | −420.2** | −383.1** | 4.004 | −282.3 | −249.5 |
| (5.470) | (202.7) | ( 206.8) | (6.754) | (170.1) | (163.9) | |
| con_s | Yes | Yes | Yes | Yes | Yes | Yes |
| year | Yes | Yes | Yes | Yes | Yes | Yes |
| ind_l | Yes | Yes | Yes | Yes | Yes | Yes |
| R2 | 0.091 | 0.381 | 0.362 | 0.115 | 0.330 | 0.323 |
| obs | 3,135 | 3,095 | 3,135 | 3,135 | 3,095 | 3,135 |
| Instrumental variable | Individual cluster | |||||
|---|---|---|---|---|---|---|
| self_hea | lncost | lnselfcost | self_hea | lncost | lnselfcost | |
| lnCR | 0.356*** | 5.514*** | 4.633*** | 0.093** | 2.792*** | 2.913*** |
| (0.120) | (1.186) | (1.142) | (0.037) | (0.906) | (0.898) | |
| constant | 2.562** | 29.71*** | 38.20** | 5.324 | −417.3*** | −440.2*** |
| (0.573) | (5.457) | (16.19) | (6.131) | (171.6) | (160.9) | |
| con_s | Yes | Yes | Yes | Yes | Yes | Yes |
| year | Yes | Yes | Yes | Yes | Yes | Yes |
| ind_l | Yes | Yes | Yes | Yes | Yes | Yes |
| reg_l | No | No | No | Yes | Yes | Yes |
| F | 655.5 | 51.14 | 44.93 | |||
| C_D Wald | 692.8 | 58.01 | 51.28 | |||
| LM (p) | 0.000 | 0.000 | 0.000 | |||
| R2 | 0.047 | 0.081 | 0.231 | 0.082 | 0.350 | 0.348 |
| obs | 3,135 | 3,095 | 3,135 | 3,135 | 3,095 | 3,135 |
*, **, and *** represent significance at the 10%, 5%, and 1% levels, respectively. The values in parentheses are clustered robust standard errors at the city level. For the instrumental variable regression, we report only the results from the second stage
The moderating effect of the multi-tier health insurance system
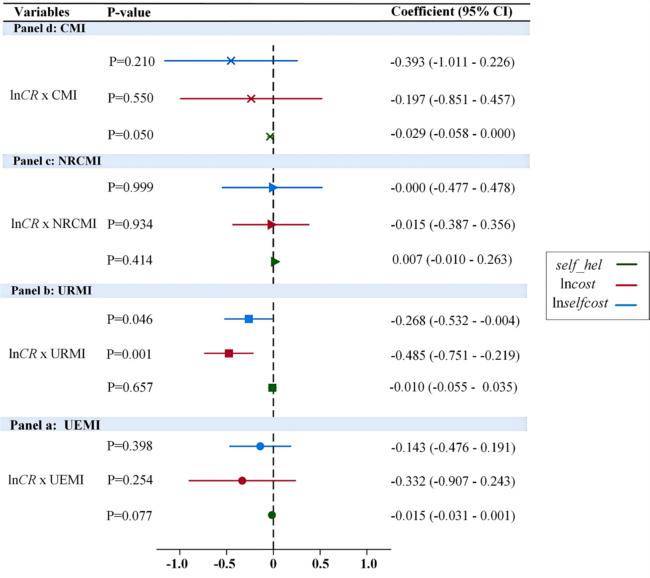
To examine whether changes in self-assessed health and healthcare costs among the elderly due to climate risks are influenced by participation in different types of medical insurance, this study analyzes the interaction between differentiated insurance participation and climate risk. Specifically, we considered the impact of three types of public medical insurance and commercial insurance: UEMI, URMI, NRCMI, and CMI. Figure 2 presents the moderating effects of different types of medical insurance. The results show (Panel a) that the interaction term between UEMI and climate risk has a coefficient of −0.015 (significant at the 10% level), indicating that participation in UEMI helps reduce the health damages (self_hea) caused by climate risks for the elderly. However, for both total medical costs (lncost) and out-of- pocket expenses (lnselfcost), the interaction term coefficients are not significant, suggesting that UEMI participation does not significantly reduce healthcare expenditures resulting from climate risks.
Fig. 2.
The unequal impact of a multi-tier healthcare system
Regarding URMI, the results in Fig. 2 (Panel b) indicate that the interaction term between URMI and climate risk has no significant effect on the self-assessed health of the elderly, as the coefficient is not statistically significant. However, it significantly reduces the total medical costs (lncost) and out-of-pocket expenses (lnselfcost) caused by climate risk, with regression coefficients of −0.485 (significant at the 1% level) and − 0.268 (significant at the 5% level), respectively. This result suggests that although participation in URMI does not alleviate the health damage caused by climate risks, it plays a positive role in reducing healthcare costs associated with climate risks. As for NRCMI, the results in Fig. 2 (Panel c) show that the interaction term between NRCMI and climate risk has no significant impact on both self-assessed health (self_hea) and medical costs for the elderly, with the regression coefficients being statistically insignificant. This suggests that participation in NRCMI has no noticeable effect on mitigating the health damage or healthcare costs resulting from climate risk.
Additionally, unlike public social insurance, we examine whether participation in CMI moderates the health and cost impacts of climate risk. According to the regression results in Fig. 2 (Panel d), the interaction term between CMI and climate risk has a significant negative coefficient of −0.029 (at the 5% level) for self-assessed health (self_hea), indicating that purchasing CMI effectively mitigates the health damage caused by climate risks. However, for total medical costs (lncost) and out-of-pocket expenses (lnselfcost), the interaction term coefficients are not significant, suggesting that purchasing CMI does not reduce the medical expenses incurred by the elderly due to climate risk.
Based on the above findings, our results suggest that the multi-tiered healthcare insurance system has a significant differential impact on alleviating the health and medical costs of middle-aged and elderly populations affected by climate risk. Both social basic medical insurance and commercial insurance exhibit a “pro-wealthy” rather than “pro-poor” characteristic, which aligns with similar findings in existing literature [35, 36]. Specifically, participation in UEMI and CMI effectively mitigated the health damage caused by climate risk, improving the self-assessed health (self_hea) of the elderly. URMI, on the other hand, significantly reduced total medical costs (lncost) and out-of-pocket expenses (lnselfcost) for the elderly, while NRCMI had no significant effect on reducing these costs associated with climate risk.
Further analysis is conducted using Eq. (16) to examine whether the IURMI can eliminate the inequality caused by multi-tiered insurance participation. Considering the policy implementation goals, as previously mentioned, various provinces and cities have gradually introduced corresponding supporting measures and specific integration plans since the integration objective was proposed. These measures aim to reduce the disparity between urban basic healthcare insurance and the new rural cooperative medical system, improve healthcare service efficiency, and expand the scope of insurance reimbursements and covered services. We define the policy treatment variable based on the specific implementation timeline of URMII schemes in each city or province for examination. To investigate whether URMII can effectively mitigate the negative impacts of climate risks on middle-aged and elderly individuals with rural household registration, we analyze the rural household registration sample.
In Table 5, the interaction term between the policy treatment variable and climate risk (lnCR x URMII) is not statistically significant across different regression results. This indicates that, it has not alleviated the inequality inherent in the multi-tiered healthcare insurance system. One possible reason is that a significant proportion of the elderly rural population is either self-employed or unemployed, and their labor capacity rapidly declines with age, leading to greater health deterioration [37]. While the URMII has improved rural residents’ access to medical services, the incidence of disease significantly increases with age due to the greater health deterioration in elderly populations. This is particularly true for elderly rural residents, who are highly vulnerable to negative impacts from climate risks and other environmental changes [38]. This significantly counteracts the potential alleviating effect of the URMII on the medical burdens of elderly rural populations. Secondly, the differences in economic development, medical resource allocation, population aging structure, and variations in healthcare policies between urban and rural areas have led to differences in the definitions, operational models, reimbursement scopes, and insurance catalogs under the unified healthcare system. Based on the above findings, health insurance integration has not reduced the health costs caused by climate risks for middle-aged and older adults with rural household registration.
Table 5.
The moderating effect of URMII
| Variables | self_hel | lncost | lnselfcost | |||
|---|---|---|---|---|---|---|
| lnCR | 0.032 | 0.025 | 0.919 | 0.401 | 0.717 | 0.526 |
| (0.057) | (0.050) | (0.923) | (1.032) | (0.878) | (0.825) | |
| lnCR x URMII | 0.013 | 0.009 | 0.990 | 0.748 | 0.859 | 0.468 |
| (0.009) | (0.009) | (0.141) | (0.605) | (0.601) | (0.593) | |
| constant | 2.976*** | −2.078 | 13.77*** | −86.44 | 13.00*** | −56.90 |
| (0.203) | (3.657) | ( 3.159) | (124.3) | (2.943) | (127.9) | |
| con_s | No | Yes | No | Yes | No | Yes |
| year | Yes | Yes | Yes | Yes | Yes | Yes |
| ind_l | Yes | Yes | Yes | Yes | Yes | Yes |
| obs | 0.004 | 0.501 | 0.145 | 0.297 | 0.085 | 0.233 |
| R2 | 1,005 | 1,005 | 1,005 | 1,005 | 1,005 | 1,005 |
*, **, and *** represent significance at the 10%, 5%, and 1% levels, respectively. The values in parentheses are clustered robust standard errors at the city level
The long-term impact of climate risk on medical costs
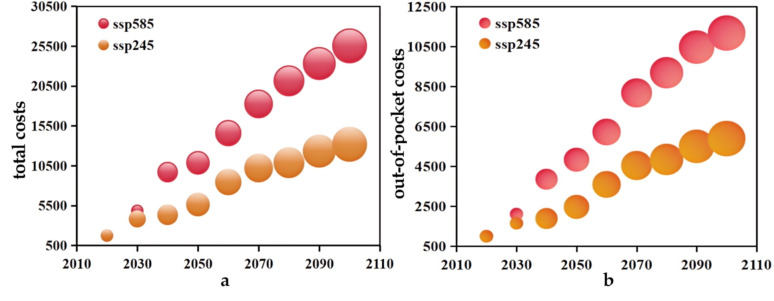
With the dual challenges of escalating global climate risks and China’s aging population, it is foreseeable that an increasing number of elderly individuals will face the threats posed by climate risks in the future [39]. As a result, we have estimated the long-term impact of climate risks on healthcare costs for the elderly population. We employed a climate model along with two scenarios based on shared socioeconomic pathways, provided by the NASN Earth Exchange Global Daily Downscaled Projections (NEX-GDDP-CMIP6), to estimate the dynamic changes in future climate risks for cities. The CMIP6 dataset includes retrospective climate forecast data from 1950 to 2014 and future daily climate projections from 2015 to 2100, covering indicators such as near-surface average temperature, precipitation, and wind speed, all with a spatial resolution of 0.25 × 0.25 [40]. Additionally, we use SSP585 and SSP245 to represent two shared socioeconomic pathways. SSP585 represents a worst-case climate change scenario without climate policy constraints, while SSP245 reflects a more realistic intermediate pathway, representing global climate change under effective climate policy interventions [41]. We use Arcgis to match future climate projections under the two scenarios with the sample cities, both temporally and spatially. Then, we extract annual indicators from the daily observations to estimate the dynamic changes in climate risk. In alignment with global temperature control targets, our estimation covers the period from 2020 to 2100, with 2020 as the baseline year, and estimates are made at 10-year intervals. The model for long-term estimation of health costs for the middle-aged and elderly population is as follows (18):
 |
18 |
where, ΔHelits represents the change in medical expenses for individual i at time t under scenario s; ΔCRitjs represents the change in climate risk for the city of individual i in year j of the t-th decade under scenario s; θ1 represents the estimated coefficient of climate risk on the healthcare costs for middle-aged and elderly individuals after considering the instrumental variables, which is estimated using Eq. (15).
Figure 3 presents the estimated results for the average medical total medical costs (a) and out-of-pocket costs (b). It is evident that both out-of-pocket costs and total medical costs increase significantly under both the SSP585 and SSP245 scenarios. Specifically, under the SSP585 scenario, by the end of this century, per capita out-of-pocket costs and total medical costs for the elderly population due to climate risk are projected to reach 25,523 CNY and 11,171 CNY, respectively. While the cost increase in the SSP585 scenario may diverge significantly from actual outcomes, it represents the worst-case scenario for climate change. In contrast, the SSP245 scenario, which is more realistic, shows a more moderate growth in climate risk-induced medical costs for the elderly. By the end of the century, per capita total medical costs and out-of-pocket costs are projected to increase to 13,191 CNY and 5,882 CNY, respectively, reflecting an average increase of 7 to 10 times. Furthermore, these results across different scenarios highlight the health benefits of implementing climate policies. In the SSP245 scenario, medical out-of-pocket and total costs for the elderly are reduced by nearly 50% compared to the SSP585 scenario.
Fig. 3.
The long-term impact of climate risk changes on medical costs
Discussion
Our study uses survey data from the CHARLS elderly population and city-level indicators, employing multidimensional panel fixed effects and instrumental variable estimation methods. We find that the rise in climate risk has a significant negative impact on the self-reported health status and medical costs of the middle-aged and elderly population. Specifically, climate risk significantly increased the total hospitalization costs (β = 0.721, P = 0.004) and out-of-pocket hospitalization expenses (β = 0.706, P = 0.036) for the middle-aged and elderly, but had no significant impact on outpatient total costs (β = 0.027, P = 0.941) or out-of-pocket outpatient expenses (β = 0.054, P = 0.790). This suggests that the health damage caused by climate risk for the elderly is more likely to manifest as direct physiological harm. The potential reasons for this include two factors: First, unlike previous studies that use extreme heat as a proxy for climate risk, health damage caused by extreme precipitation and other climate events tends to result in direct physical harm rather than cumulative health damage. Second, elderly people, as a vulnerable group, have weakened physical functions and immune systems, making them more sensitive to changes in the external climate environment. When extreme climate events occur, they may exacerbate underlying conditions such as cardiovascular diseases and respiratory illnesses, increasing the likelihood of hospitalization and thus raising hospitalization costs for the elderly population [42, 43].
Unlike previous studies, our findings highlight the heterogeneous moderating effects of multi-tier medical insurance participation on climate risk. In China, the multi-tiered social health insurance system covers nearly all groups, with an average participation rate of 95%. Specifically, for the elderly, participation in basic health insurance is a crucial safeguard for improving access to healthcare services. However, the household registration-based social medical insurance system also leads to inequalities in the utilization of medical services and the provision of benefits. Our estimations show that the inequality resulting from multi-tiered insurance participation manifests in the fact that both UEMI and URMI can effectively mitigate the health risks and medical costs associated with climate risk. However, for elderly people with rural household registration, participation in the NRCMI has not significantly alleviated the health damage and medical burden caused by climate risk. Furthermore, although the Chinese government began gradually promoting effective coordination of URMII at the provincial or municipal level in 2016, with the aim of reducing urban-rural disparities in healthcare utilization. Our estimation results indicate that the implementation of the URMII policy has had a limited impact in reducing health inequalities, resulting in persistent disparities in health and medical burdens between urban and rural elderly populations. According to the asset poverty theory, when an individual’s asset accumulation falls below a certain threshold over the long term, they are at risk of falling into a poverty trap. The URMII serves as a redistributive mechanism that compensates for the medical burdens faced by the elderly due to illness, providing a loss compensation effect. However, the increase in morbidity among the elderly caused by climate risks can lead to a surge in medical costs. Based on these findings, we recommend further unifying urban and rural health insurance premiums and service levels, and increasing the reimbursement benefits for rural residents’ medical insurance. Specifically for the rural elderly population, on the one hand, improving primary healthcare services, promoting the establishment of urban-rural medical collaboration mechanisms, and accelerating the extension of healthcare resources to rural areas are crucial to effectively addressing the health impacts of climate risks on rural seniors. On the other hand, implementing an adaptive health insurance system, exploring elderly allowances, and establishing a dynamic benefits adjustment mechanism are essential, alongside strict control over irrational increases in outpatient and inpatient medical expenses.
Our findings also highlight the importance of implementing restrictive climate policies for health benefits. We conducted long-term forecasts of healthcare costs for the elderly using two shared socioeconomic pathways, SSP585 and SSP245. Our results indicate that in both climate policy scenarios, the increase in healthcare costs due to climate risks is irreversible. However, in the SSP245 scenario, which represents a middle-of-the-road approach, healthcare costs for the elderly caused by climate risks are projected to be nearly 50% lower by the end of this century compared to the SSP585 scenario. This reduction in costs is significant, underscoring the necessity of implementing strict climate constraint policies. Therefore, given the public nature of climate risk changes, it is critical for governments to continuously develop and implement stringent climate governance policies, while aligning climate action with health maintenance objectives. However, it is important to note that our long-term forecast results are simple estimates based on linear relationships.
Our study inevitably has certain limitations. First, the Difference-in-Differences (DID) model provides a more precise assessment of the health impacts caused by climate risks. However, we ultimately chose to advance our study using a combination of ordinary least squares (OLS) and instrumental variable (IV) approaches. Extreme climate events typically occur in localized areas and are relatively short-lived, posing unavoidable challenges for causal identification using the DID model. Since climate risks often unfold over just a few days, such an analysis requires high-frequency daily data. Unfortunately, most publicly available micro-level survey data are collected annually, making it difficult to obtain daily-level data to support our analysis. Moreover, extreme climate events do not always occur consecutively, making it challenging to maintain temporal continuity. The intermittent nature of climate events weakens the identification strategy in the DID model, and this lack of continuity poses challenges for estimating treatment effects. Second, We have not conducted an in-depth discussion or elaboration on the relationships between climate risk and health inequality, as well as between the multi-tiered health insurance system and health inequality. Our study focuses solely on examining whether participation in a multi-tiered health insurance system contributes to the inequality in health damage caused by climate risks. Finally, our long-term forecasts of climate risks and healthcare cost changes are based on linear relationships, which may introduce some error in the predictions. In reality, the relationship between climate risks and healthcare costs is often a complex nonlinear one. Our predicted results are only a simple estimate of the long-term relationship between climate risks and healthcare costs. We hope that future research will refine these predictions further.
Conclusion
In summary, our study reveals the negative impact of climate risks on self-rated health and healthcare costs for the elderly population. Moreover, under the differentiated multi-tiered healthcare insurance system, the health impacts of climate risks show significant disparities based on household registration status. We also discuss the long-term impacts of climate risks, highlighting the significant health benefits of implementing climate policies. Our study provides insights into mitigating the health impacts of climate risks on the elderly and reducing the inequalities arising from the multi-tiered healthcare insurance system.
Acknowledgements
Not applicable.
Authors’ contributions
Conceptualization, H.Y; methodology, Y.Y., D.L; software, Y.Y., D.L; validation, Y.Y, D.L; formal analysis, Y.Y.; investigation,H.Y., D.L.; writing-original draft preparation, Y.Y.; writing-review and editing, H.Y., Y.Y; funding acquisition, H.Y. All authors read and approved the final manuscript.
Funding
This work is supported by “Health inequality related to air pollution: level measurement, policy evaluation and mechanism testing”, the National Natural Science Foundation of China (72274145).
Data availability
The China Health and Retirement Longitudinal Study (CHARLS) data can be accessed through the following link: https://charls.pku.edu.cn/.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hueholt DM, Barnes EA, Hurrell JW, et al. Speed of environmental change frames relative ecological risk in climate change and climate intervention scenarios. Nat Commun. 2024;15(1):3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang Y, Gillett NP, Monahan AH. Accounting for Pacific climate variability increases projected global warming. Nat Clim Chang. 2024;14(6):608–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendola P, Ha S. Beyond the infant in your arms: effects of climate change last for generations. Fertil Steril. 2022;118(2):224–9. [DOI] [PubMed] [Google Scholar]
- 4.Liu H, Tong M, Guo F, et al. Deaths attributable to anomalous temperature: a generalizable metric for the health impact of global warming. Environ Int. 2022;169:107520. [DOI] [PubMed] [Google Scholar]
- 5.Amondo EI, Kirui OK, Mirzabaev A. Health gender gap in Uganda: do weather effects and water play a role? Int J Equity Health. 2022;21(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meierrieks D. Weather shocks, climate change and human health. World Dev. 2021;138:105228. [Google Scholar]
- 7.Liao H, Zhang C, Burke PJ, et al. Extreme temperatures, mortality, and adaptation: evidence from the County level in China. Health Econ. 2023;32(4):953–69. [DOI] [PubMed] [Google Scholar]
- 8.Li X, Ye Z, Lang H, et al. Climate change and depressive disorders in middle-aged and older people in China: a quasi-experimental study. J Environ Psychol. 2023;92:102162. [Google Scholar]
- 9.Murage P, Macintyre HL, Heaviside C, et al. Future temperature-related mortality in the UK under climate change scenarios: impact of population ageing and bias-corrected climate projections. Environ Res. 2024;259:119565. [DOI] [PubMed] [Google Scholar]
- 10.Ai H, Tan X. The effects of exposure to high temperatures during pregnancy on adolescent mental health: evidence from China. China Econ Rev. 2023;80:101991. [Google Scholar]
- 11.Dasgupta S, Robinson EJZ. Climate, weather, and child health: quantifying health co-benefits. Environ Res Lett. 2024;19(8):084001. [Google Scholar]
- 12.Qi Y, Zhang H, Shao S. Valuing high temperature’s fiscal costs: evidence from China. Econ Anal Policy. 2024;81:134–52. [Google Scholar]
- 13.Chen Z, Zhang X, Chen F. Assessment of extreme temperature to fiscal pressure in China. Glob Environ Change. 2024;84:102797. [Google Scholar]
- 14.Yang Z, Yang B, Liu P, et al. Exposure to extreme climate decreases self-rated health score: large-scale survey evidence from China. Glob Environ Change. 2022;74:102514. [Google Scholar]
- 15.Hou J, Wang C, Wang H, et al. Effects of temperature on mental health: evidence and mechanisms from China. China Econ Rev. 2023;79:101953. [Google Scholar]
- 16.Dong B. The promotion of pooling level of basic medical insurance and participants’ health: impact effects and mediating mechanisms. Int J Equity Health. 2023;22(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang X, Chen X, Li L, et al. The impacts of basic medical insurance for urban-rural residents on the perception of social equity in China. Cost Eff Res Alloc. 2024;22(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huo J, Hu M, Li S. The impact of urban-rural medical insurance integration on medical impoverishment: evidence from China. Int J Equity Health. 2023;22(1):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dai L, Guo Y. The problem and countermeasures of the failure of the rural social security system to reduce poverty. Discov Sustain. 2024;5(1):54. [Google Scholar]
- 20.Ma X, Feng W, Shi C, et al. Association between the location of social medical insurance and social integration among China’s elderly rural migrants: a nationwide cross-sectional study. BMC Public Health. 2023;23(1):2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang J, Zhao D, Zhang X. China’s universal medical insurance scheme: progress and perspectives. BMC Global Public Health. 2024;2(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fu D, Liu L, Zhang X, et al. The relationship between urban and rural health insurance and the self-rated health of migrant workers in Southwest China. BMC Health Serv Res. 2021;21:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meng Y, Yu R, Bai H, et al. Evidence from the China family panel studies survey on the effect of integrating the basic medical insurance system for urban and rural residents on the health equity of residents: difference-in-differences analysis. JMIR Public Health Surveill. 2024;10:e50622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Chen W. Can provincial-pooling of urban and rural resident basic medical insurance improve the health performance of migrant population? Humanit Soc Sci Commun. 2024;11(1):1–11. [Google Scholar]
- 25.Hu H, Zhao L, Yong Y, et al. Medical insurance payment schemes and patient medical expenses: a cross-sectional study of lung cancer patients in urban China. BMC Health Serv Res. 2023;23(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ren W, Xing Y, Tarimo CS, et al. A study on the equity of self-rated health of older adults at the family level. Int J Equity Health. 2023;22(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miao K, Li K, Su L. Panel threshold models with interactive fixed effects. J Econ. 2020;219(1):137–70. [Google Scholar]
- 28.Liu Y, Zhang X, Shen Y. Technology-driven carbon reduction: analyzing the impact of digital technology on China’s carbon emission and its mechanism. Technol Forecast Soc Chang. 2024;200:123124. [Google Scholar]
- 29.Baker SR, Bloom N, Davis SJ. Measuring economic policy uncertainty. Q J Econ. 2016;131(4):1593–636. [Google Scholar]
- 30.Xiang R, Hou X, Li R. Health risks from extreme heat in China: evidence from health insurance. J Environ Manage. 2024;354:120300. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y, Yuan Y. Examining the non-linear association between ambient temperature and mental health of elderly adults in the community: evidence from Guangzhou, China. BMC Public Health. 2024;24(1):2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ning Z, Ma Y, He S, et al. The interactive effect of extreme weather events and PM2. 5 on respiratory health among the elderly: a case-crossover study in a high-altitude city. Int J Biometeorol. 2025;69(2):331–42. [DOI] [PubMed]
- 33.Bell JE, Brown CL, Conlon K, et al. Changes in extreme events and the potential impacts on human health. J Air Waste Manag Assoc. 2018;68(4):265–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang G, Ji Y, Chen C, et al. Effects of extreme precipitation on hospital visit risk and disease burden of depression in Suzhou, China. BMC Public Health. 2022;22(1):1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.He W. Social medical insurance integration and health care disparities in China: evidence from an administrative claim data set. Econ Anal Policy. 2023;79:20–39. [Google Scholar]
- 36.Ren Y, Zhou Z, Cao D, et al. Did the integrated urban and rural resident basic medical insurance improve benefit equity in China? Value Health. 2022;25(9):1548–58. [DOI] [PubMed] [Google Scholar]
- 37.Xu X, Yang H. Elderly chronic diseases and catastrophic health expenditure: an important cause of borderline poor families’ return to poverty in rural China. Humanit Soc Sci Commun. 2022;9(1):1–10. [Google Scholar]
- 38.Wen B, Su BB, Xue J, et al. Temperature variability and common diseases of the elderly in China: a National cross-sectional study. Environ Health. 2023;22(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Z, Gao S, Cai W, et al. Projections of heat-related excess mortality in China due to climate change, population and aging. Front Environ Sci Eng. 2023;17(11):132. [Google Scholar]
- 40.Thrasher B, Wang W, Michaelis A, et al. NASA global daily down scaled projections, CMIP6. Sci Data. 2022;9(1):262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yuan H, Ning L, Zhou J, et al. HiCPC: A new 10-km CMIP6 down scaled daily climate projections over China. Sci Data. 2024;11(1):1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McDermott-Levy R, Kolanowski AM, Fick DM, et al. Addressing the health risks of climate change in older adults. J Gerontol Nurs. 2019;45(11):21–9. [DOI] [PubMed] [Google Scholar]
- 43.Antal H, Bhutani S. Identifying linkages between climate change, urbanisation, and population ageing for understanding vulnerability and risk to older people: a review. Ageing Int. 2023;48(3):816–39. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The China Health and Retirement Longitudinal Study (CHARLS) data can be accessed through the following link: https://charls.pku.edu.cn/.