Abstract
CS-023 (RO4908463, formerly R-115685) is a novel 1β-methylcarbapenem with 5-substituted pyrrolidin-3-ylthio groups, including an amidine moiety at the C-2 position. Its antibacterial activity was tested against 1,214 clinical isolates of 32 species and was compared with those of imipenem, meropenem, ceftazidime, ceftriaxone, ampicillin, amikacin, and levofloxacin. CS-023 exhibited a broad spectrum of activity against gram-positive and -negative aerobes and anaerobes, including methicillin-resistant Staphylococcus aureus (MRSA), methicillin-resistant Staphylococcus epidermidis, penicillin-resistant Streptococcus pneumoniae (PRSP), β-lactamase-negative ampicillin-resistant Haemophilus influenzae, and Pseudomonas aeruginosa. CS-023 showed the most potent activity among the compounds tested against P. aeruginosa and MRSA, with MICs at which 90% of isolates tested were inhibited of 4 μg/ml and 8 μg/ml, respectively. CS-023 was stable against hydrolysis by the β-lactamases from Enterobacter cloacae and Proteus vulgaris. CS-023 also showed potent activity against extended-spectrum β-lactamase-producing Escherichia coli. The in vivo efficacy of CS-023 was evaluated with a murine systemic infection model induced by 13 strains of gram-positive and -negative pathogens and a lung infection model induced by 2 strains of PRSP (serotypes 6 and 19). Against the systemic infections with PRSP, MRSA, and P. aeruginosa and the lung infections, the efficacy of CS-023 was comparable to those of imipenem/cilastatin and vancomycin (tested against lung infections only) and superior to those of meropenem, ceftriaxone, and ceftazidime (tested against P. aeruginosa infections only). These results suggest that CS-023 has potential for the treatment of nosocomial bacterial infections by gram-positive and -negative pathogens, including MRSA and P. aeruginosa.
Carbapenems, such as imipenem/cilastatin (3), panipenem/betamipron (7), and meropenem (27), are effective in patients with nosocomial infections, since they have an extremely wide antibacterial spectrum and strong activity against gram-positive and -negative aerobic and anaerobic bacteria, including many resistant pathogens. However, carbapenems do not show high activity against methicillin-resistant Staphylococcus aureus (MRSA), and the emergence of carbapenem-resistant pathogens has reduced the clinical efficacy of carbapenems (9). MRSA and Pseudomonas aeruginosa are major pathogens for patients who have nosocomial infections (11). Therefore, there is an urgent need for new antibacterial agents effective against such highly resistant pathogens.
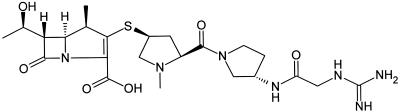
In the process of research for new carbapenem compounds with a broad spectrum, potent activity against MRSA as well as P. aeruginosa, and a longer half-life, we synthesized a novel 1β-methyl carbapenem, CS-023 (RO4908463, formerly R-115685), (-)-(4R,5S,6S)-3-[[(3S,5S)-5-[(S)-3-(2-guanidinoacetylamino)pyrrolidin-1-ylcarbonyl]-1-methylpyrrolidin-3-yl]thio]-6-[(R)-1-hydroxyethyl]-4-methyl-7-oxo-azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid (Fig. 1).
FIG. 1.
Chemical structure of CS-023 (RO4908463).
In this study, we investigated the in vitro and in vivo antibacterial activities of CS-023 in comparison with those of other carbapenems, i.e., imipenem and meropenem, parenteral cephems, i.e., ceftazidime and ceftriaxone, a penicillin, ampicillin, a quinolone, levofloxacin, and an aminoglycoside, amikacin.
(This work was presented in part at the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, Toronto, Canada, September 2000 [F-1230, F-1231, F-1232].)
MATERIALS AND METHODS
Antibiotics.
CS-023 was synthesized at Sankyo Research Laboratories, Tokyo, Japan. Imipenem, meropenem, ceftazidime, and ceftriaxone were obtained from the National Institute of Infectious Diseases, Tokyo, Japan. Levofloxacin was extracted at Sankyo from a commercial formula (Daiichi Pharmaceutical Co., Ltd., Tokyo, Japan). The following compounds were obtained commercially: cefotaxime (Chugai Pharmaceutical Co., Ltd., Tokyo, Japan); ampicillin (Meiji Seika Kaisha, Ltd., Tokyo, Japan); amikacin and imipenem/cilastatin (Banyu Pharmaceutical Co., Ltd., Tokyo, Japan); benzylpenicillin (Sigma-Aldrich Japan K.K., Tokyo, Japan); and cephaloridine, oxacillin, vancomycin, and cephalothin (Sigma-Aldrich Japan K.K.).
Bacterial strains.
The bacterial strains used in the susceptibility tests were isolated from clinical specimens in Japanese hospitals between 1996 and 2000 and were stored frozen at −80°C in our laboratory. Escherichia coli JM109 and its transformants harboring various extended-spectrum β-lactamase (ESBL) plasmids (22) were also used for susceptibility tests. The other strains used in this study were isolated from clinical specimens obtained between 1982 and 1996 and stored at −80°C in 10% skim milk until use.
Susceptibility tests.
MICs were determined with a standard microdilution broth method (14, 15). Mueller-Hinton broth (MHB) (Becton, Dickinson and Company) containing 25 mg of Ca2+ and 12.5 mg of Mg2+ per liter (cation-adjusted MHB) was used as a medium for all species of aerobes, except for cation-adjusted MHB supplemented with 5% lysed horse blood (Nippon Bio-Test Laboratories, Inc., Tokyo, Japan) for streptococci and Moraxella catarrhalis and cation-adjusted MHB supplemented with hemin (15 μg/ml; Sigma-Aldrich Japan K.K.), β-NAD (15 μg/ml; Sigma-Aldrich Japan K.K.), and yeast extract (5 mg/ml; Sigma-Aldrich Japan K.K.) for Haemophilus influenzae. The inoculum size of aerobes was 4 × 105 CFU/ml. The inoculated plates were incubated at 35°C for 20 to 24 h for Streptococcus pneumoniae and H. influenzae and for 16 to 20 h for other aerobic species. The MICs of oxacillin and benzylpenicillin were also determined to provide phenotypes for staphylococci and S. pneumoniae, respectively. Anaerobe Broth MIC (Becton, Dickinson and Company) was used for Propionibacterium acnes and Bacteroides fragilis. Anaerobe Broth MIC supplemented with 2% lysed horse blood was used for peptostreptococci. The inoculum size of anaerobes was approximately 1 × 106 CFU/ml. The inoculated plates were incubated at 35°C anaerobically for 48 h. The MIC was defined as the lowest concentration of compound that completely inhibited the viable growth of the organism in the microdilution wells.
Stability against β-lactamases.
β-Lactamase from Enterobacter cloacae (class C) was purchased from Sigma-Aldrich Japan K.K., and β-lactamase solution from Proteus vulgaris (class A) was from Wako Pure Chemical Industries, Ltd. (Osaka, Japan). The stability of antibiotics against β-lactamases was determined by the spectrophotometric assay described by Waley (25). Change in absorbance was monitored after addition of a test enzyme in a reaction mixture. The wavelengths (nm) used were as follows: CS-023, 300; imipenem, 300; meropenem, 300; ceftriaxone, 254; and cephalothin, 262. The relative velocity of hydrolysis was determined from 100 μM of the substrate concentration of each compound. The velocity is expressed as a relative value, assuming that of cephalothin to be 100.
Animals.
Male ddY (Japan SLC, Inc., Shizuoka, Japan) specific-pathogen-free mice were used in this study. All animal experiments were carried out according to the guidelines provided by the Institutional Animal Care and Use Committee of Sankyo Co., Ltd.
Murine systemic infection model.
Six strains of gram-positive pathogens, including MRSA and penicillin-resistant S. pneumoniae (PRSP), and seven strains of gram-negative pathogens were used in this study. Mice weighing 22 to 28 g were infected intraperitoneally with 0.2 ml of bacterial suspension. The bacterial suspensions, except for those of E. coli, Serratia marcescens, and P. aeruginosa, were mixed with hog stomach gastric mucin to a final concentration of 5% and used for inoculation. The challenge doses shown in Table 4 caused 100% mortality between the third and fifth days after infection. They ranged between 3 and 71 times the 50% lethal doses for all pathogens except for S. pneumoniae (140 to 200 50% lethal dose). CS-023, imipenem/cilastatin, meropenem, ceftriaxone, and ceftazidime, which was used only for gram-negative pathogens, were each administered subcutaneously as a 0.1-ml solution immediately and 4 h after infection. Four to seven doses utilizing serial twofold dilutions from 0.025 to 100 mg/kg of body weight were employed for each 50% effective dose (ED50) determination. Seven mice were used for each dose. After the inoculation, mortality of mice was recorded daily for 7 days. Values of ED50s and 95% confidence intervals were calculated by the probit method (1) from the survival rates on the seventh day after infection.
TABLE 4.
Protective effect of CS-023 on systemic infections in mice
| Organism (MIC of drug), Challenge dose (CFU/mouse) | Compound | MIC (μg/ml) | ED50a (mg/kg/dose) | 95% confidence interval (mg/kg/dose) |
|---|---|---|---|---|
| Methicillin-susceptible S. aureus Smithb (MIC of MPIPC,d 0.25 μg/ml), 1.3 × 107 | CS-023 | 0.12 | 0.97 | 0.61-1.5 |
| Imipenem/cilastatin | 0.016 | 0.20 | NCc | |
| Meropenem | 0.06 | 5.8 | 3.9-9.9 | |
| Ceftriaxone | 4 | 6.6 | NC | |
| Methicillin-susceptible S. aureus 560b (MIC of MPIPC, 1 μg/ml), 1.3 × 108 | CS-023 | 0.25 | 2.6 | 1.6-4.3 |
| Imipenem/cilastatin | 0.016 | 0.61 | 0.40-0.99 | |
| Meropenem | 0.12 | 39 | 27-58 | |
| Ceftriaxone | 4 | 8.8 | NC | |
| Methicillin-resistant S. aureus 507b (MIC of MPIPC, 32 μg/ml), 1.6 × 107 | CS-023 | 1 | 7.9 | 3.9-12 |
| Imipenem/cilastatin | 0.12 | 13 | 8.6-20 | |
| Meropenem | 2 | >100 | NC | |
| Ceftriaxone | 32 | 39 | 25-70 | |
| Methicillin-susceptible S. epidermidis 1392,b 4.8 × 108 | CS-023 | 0.06 | 0.76 | 0.47-1.1 |
| Imipenem/cilastatin | 0.016 | 0.16 | 0.10-0.24 | |
| Meropenem | 0.06 | 5.8 | 3.5-9.7 | |
| Ceftriaxone | 2 | 11 | NC | |
| Penicillin-susceptible S. pneumoniae 2132b (MIC of PCG,e 0.016 μg/ml), 1.4 × 102 | CS-023 | ≤0.008 | 0.10 | 0.071-0.16 |
| Imipenem/cilastatin | ≤0.008 | 0.042 | 0.010-0.075 | |
| Meropenem | 0.016 | 1.1 | 0.69-2.0 | |
| Ceftriaxone | 0.016 | 0.13 | 0.083-0.19 | |
| Ampicillin | 0.03 | 0.48 | 0.30-0.74 | |
| Penicillin-resistant S. pneumoniae 9605b (MIC of PCG, 4 μg/ml), 6.9 × 102 | CS-023 | 0.25 | 0.55 | 0.38-0.79 |
| Imipenem/cilastatin | 0.25 | 0.33 | 0.13-0.52 | |
| Meropenem | 0.5 | 3.9 | 2.0-6.4 | |
| Ceftriaxone | 1 | 2.1 | 1.2-4.9 | |
| Ampicillin | 4 | 7.9 | 4.9-14 | |
| E. coli 704, 5.9 × 107 | CS-023 | ≤0.008 | 1.2 | 0.82-2.5 |
| Imipenem/cilastatin | 0.12 | 4.9 | 3.3-10 | |
| Meropenem | 0.016 | 5.9 | NC | |
| Ceftazidime | 0.12 | 3.2 | NC | |
| Ceftriaxone | 0.03 | 0.33 | 0.19-0.63 | |
| C. freundii 1231,b 3.7 × 107 | CS-023 | 0.016 | 0.31 | 0.17-0.54 |
| Imipenem/cilastatin | 1 | 1.2 | 0.81-1.8 | |
| Meropenem | 0.016 | 1.2 | 0.41-2.0 | |
| Ceftazidime | 0.5 | 3.2 | 1.7-5.4 | |
| Ceftriaxone | 0.12 | 0.27 | 0.15-0.55 | |
| K. pneumoniae 866,b 6.4 × 106 | CS-023 | 0.016 | 0.67 | 0.46-1.0 |
| Imipenem/cilastatin | 0.25 | 1.8 | 1.2-2.7 | |
| Meropenem | 0.03 | 1.8 | 1.1-3.0 | |
| Ceftazidime | 0.25 | 0.46 | 0.29-0.79 | |
| Ceftriaxone | 0.25 | 0.11 | NC | |
| E. aerogenes 100,b 4.6 × 107 | CS-023 | 0.06 | 6.5 | 3.2-15 |
| Imipenem/cilastatin | 2 | 3.1 | 1.7-5.0 | |
| Meropenem | 0.06 | 31 | NC | |
| Ceftazidime | 0.12 | 3.1 | 1.5-5.0 | |
| Ceftriaxone | 0.06 | 2.5 | NC | |
| S. marcescens 1850, 6.9 × 107 | CS-023 | 0.016 | 1.1 | 0.61-6.7 |
| Imipenem/cilastatin | 0.12 | 9.4 | 4.8-74 | |
| Meropenem | 0.016 | 2.5 | 1.6-5.0 | |
| Ceftazidime | 0.12 | 0.68 | 0.32-25 | |
| Ceftriaxone | 0.25 | 0.054 | 0.030-55 | |
| P. mirabilis 1262,b 4.8 × 108 | CS-023 | 0.25 | 39 | 22-260 |
| Imipenem/cilastatin | 4 | >100 | NC | |
| Meropenem | 0.12 | >100 | NC | |
| Ceftazidime | 0.25 | 29 | 19-43 | |
| Ceftriaxone | 0.016 | 0.28 | 0.18-0.45 | |
| P. aeruginosa 1008, 2.0 × 107 | CS-023 | 0.12 | 0.95 | 0.42-4.8 |
| Imipenem/cilastatin | 1 | 0.73 | 0.50-1.1 | |
| Meropenem | 0.12 | 4.2 | 2.7-12 | |
| Ceftazidime | 2 | 58 | 38-110 | |
| Ceftriaxone | 128 | >100 | NC |
Groups of seven mice were challenged with bacterial suspension intraperitoneally, and the compounds were administered by the subcutaneous route immediately and 4 h postinfection.
5% mucin.
NC, not calculated.
MPIPC, oxacillin.
PCG, penicillin G.
Murine pneumonia model induced by PRSP.
PRSP 9601 (serotype 6) (MIC of benzylpenicillin, 4 μg/ml) and 10691 (serotype 19) (MIC of benzylpenicillin, 2 μg/ml) were used in this study. This infection model was constructed as described previously (5) with minor modification. Freshly grown colonies after overnight incubation on brain heart infusion agar (Becton, Dickinson and Company) supplemented with 5% defibrinated horse blood were suspended in heart infusion broth (Becton, Dickinson and Company) supplemented with 10% heat-inactivated horse serum at an optical density at 625 nm of 0.12 with a Miniphoto 518 spectrophotometer (Taitec Co., Ltd., Tokyo, Japan). The bacterial suspension was diluted 100-fold with fresh 10% heat-inactivated horse serum and incubated, with shaking, to yield an optical density at 625 nm of 0.12. This culture, which was in the exponential growth phase, was diluted 5-fold with the same medium and used for inoculation.
Experimental pneumonia was induced by each strain in mice weighing 25 to 32 g. Mice were anesthetized lightly by intravenous injection of ketamine hydrochloride (Sankyo, Co., Ltd., Tokyo, Japan), at 12.5 mg/kg, and 75 μl of bacterial suspension (approximately 106 CFU) was inoculated through the nares into the lungs. CS-023, imipenem/cilastatin meropenem, ceftazidime, ceftriaxone, and vancomycin were each administered subcutaneously as 0.1-ml solutions 18, 26, 42, and 50 h after infection at doses of 0.4, 2, and 10 mg/kg. Seven mice were used for each dose. The therapeutic efficacy was defined as the reduction in viable cell numbers in the lungs of infected mice. Mice were sacrificed by CO2 asphyxiation, and lungs were removed 66 h after infection. The lungs were homogenized in 5 ml of saline, and the homogenates were diluted 10-fold serially with saline. One hundred microliters of the diluent was spread onto 5% defibrinated horse blood plates and incubated at 37°C for 24 h. The viable cell numbers were determined by counting the colonies on the plates. The viable cell numbers were converted into common logarithms, and the mean values and standard errors of each group were calculated. The detection limit for lungs infected with each strain was 1.7 in log10 CFU per set of lungs.
Pharmacokinetic studies.
Pharmacokinetic study was performed using uninfected mice of the same strain as that used for the in vivo model. Mice (n = 3) were exsanguinated, and blood samples were collected by cardiopuncture with a heparinized syringe at 0.13, 0.25, 0.5, 1.0, 1.5, and 2 h after subcutaneous administration of antibiotics at 20 mg/kg. After centrifugation of the heparinized blood samples, the plasma was immediately separated and diluted with an equal volume of 500 mM 3-morpholinopropanesulfonic acid buffer (pH 7.0). Antibiotic concentrations in plasma were determined by the paper disk diffusion method, using Bacillus subtilis ATCC 6633 as the bioassay indicator (10). Standard curves were constructed with mouse plasma. For CS-023, assay validation indicated linearity (r2 value of 0.9959) in the range of 0.625 to 40 μg/ml, intra-assay bias ranged from 0.6 to 17.1%, and the coefficient of variation (CV) ranged from 3.7 to 8.6%, indicating acceptable accuracy and precision. The limit of quantitation was 0.625 μg/ml with a bias of 17.1% and a CV of 5.4%. For imipenem, assay validation indicated linearity (r2 value of 0.9990) in the range of 0.313 to 40 μg/ml, intra-assay bias ranged from 1.4 to 13.5%, and the CV ranged from 4.1 to 9.0%, indicating acceptable accuracy and precision. The limit of quantitation was 0.313 μg/ml with a bias of 8.5% and a CV of 4.8%. For meropenem, assay validation indicated linearity (r2 value of 0.9993) in the range of 0.313 to 40 μg/ml, intra-assay bias ranged from 1.8 to 8.3%, and the CV ranged from 2.3 to 11.1%, indicating acceptable accuracy and precision. The limit of quantitation was 0.313 μg/ml with a bias of 1.9% and a CV of 9.2%. For ceftriaxone, assay validation indicated linearity (r2 value of 0.9974) in the range of 0.625 to 40 μg/ml, intra-assay bias ranged from 0.3 to 14.8%, and the CV ranged from 6.8 to 14.4%, indicating acceptable accuracy and precision. The limit of quantitation was 0.625 μg/ml with a bias of 7.1% and a CV of 6.9%. For ceftazidime, assay validation indicated linearity (r2 value of 0.9925) in the range of 1.25 to 40 μg/ml, intra-assay bias ranged from 2.5 to 17.0%, and the CV ranged from 3.8 to 11.7%, indicating acceptable accuracy and precision. The limit of quantitation was 1.25 μg/ml with a bias of 17.0% and a CV of 11.7%. The pharmacokinetic parameters of the concentration in plasma were calculated by one-compartment analysis with the WinNonlin program (Scientific Consulting, Inc.).
Statistical analysis.
The statistical significance of the difference between the numbers of viable organisms recovered from the lungs of each treated group and those for the untreated control group was evaluated by a nonparametric Williams' test. A difference between the treated group and the untreated control group was considered to be statistically significant if the P value was <0.05.
RESULTS
Antibacterial activity.
The antibacterial activity of CS-023 was determined against 1,214 clinical isolates of 32 species (19 to 149 strains for each species) in comparison with those of imipenem, meropenem, ceftazidime, ceftriaxone, ampicillin, amikacin, and levofloxacin. Table 1 summarizes the MIC ranges and MICs at which 50% and 90% (MIC90) of the clinical isolates were inhibited. CS-023 exhibited a broad antibacterial spectrum against gram-positive and -negative aerobes and anaerobes.
TABLE 1.
Activities of CS-023 against Japanese clinical isolates
| Organism (no. of strains) | Compound | MIC (μg/ml)a
|
||
|---|---|---|---|---|
| Range | 50% | 90% | ||
| Methicillin-susceptiblebS. aureus (48) | CS-023 | 0.06-0.25 | 0.12 | 0.12 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03-0.25 | 0.06 | 0.12 | |
| Ceftriaxone | 1-8 | 2 | 4 | |
| Ampicillin | ≤0.03->32 | 1 | >32 | |
| Amikacin | 0.25-16 | 2 | 8 | |
| Levofloxacin | ≤0.03-0.5 | 0.12 | 0.12 | |
| Methicillin-resistantcS. aureus (52) | CS-023 | 0.12-32 | 4 | 8 |
| Imipenem | ≤0.03->32 | 32 | >32 | |
| Meropenem | 0.12->32 | 16 | 32 | |
| Ceftriaxone | 4->32 | >32 | >32 | |
| Ampicillin | 16->32 | 32 | >32 | |
| Amikacin | 0.5->32 | 8 | 32 | |
| Levofloxacin | 0.12->32 | 4 | >32 | |
| Methicillin-susceptibledS. epidermidis (48) | CS-023 | ≤0.03-0.06 | ≤0.03 | 0.06 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03-0.12 | 0.06 | 0.12 | |
| Ceftriaxone | 0.5-4 | 1 | 2 | |
| Ampicillin | ≤0.03->32 | 0.12 | 8 | |
| Amikacin | 0.12-8 | 0.5 | 1 | |
| Levofloxacin | 0.06-4 | 0.25 | 0.5 | |
| Methicillin-resistanteS. epidermidis (49) | CS-023 | ≤0.03-8 | 0.5 | 4 |
| Imipenem | ≤0.03-32 | 0.12 | 8 | |
| Meropenem | 0.12-32 | 1 | 8 | |
| Ceftriaxone | 1->32 | 16 | >32 | |
| Ampicillin | 0.06->32 | 8 | >32 | |
| Amikacin | 0.06->32 | 2 | 16 | |
| Levofloxacin | 0.12->32 | 2 | 16 | |
| S. haemolyticus (30) | CS-023 | ≤0.03-4 | 0.12 | 1 |
| Imipenem | ≤0.03-32 | ≤0.03 | 0.25 | |
| Meropenem | ≤0.03-16 | 0.25 | 4 | |
| Ceftriaxone | 0.5->32 | 8 | 32 | |
| Ampicillin | ≤0.03->32 | 8 | 32 | |
| Amikacin | 0.06-8 | 0.25 | 2 | |
| Levofloxacin | 0.06-32 | 0.12 | 8 | |
| S. pyogenes (25) | CS-023 | ≤0.03 | ≤0.03 | ≤0.03 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ceftriaxone | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ampicillin | ≤0.03 | ≤0.03 | ≤0.03 | |
| Amikacin | 32->32 | >32 | >32 | |
| Levofloxacin | 0.25-8 | 0.5 | 2 | |
| S. agalactiae (25) | CS-023 | ≤0.03-0.06 | ≤0.03 | 0.06 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03-0.06 | 0.06 | 0.06 | |
| Ceftriaxone | ≤0.03-0.12 | 0.06 | 0.06 | |
| Ampicillin | 0.06-0.12 | 0.12 | 0.12 | |
| Amikacin | >32 | >32 | >32 | |
| Levofloxacin | 0.5-1 | 1 | 1 | |
| S. oralis (25) | CS-023 | ≤0.03-4 | ≤0.03 | 2 |
| Imipenem | ≤0.03-2 | ≤0.03 | 2 | |
| Meropenem | ≤0.03-4 | ≤0.03 | 2 | |
| Ceftriaxone | ≤0.03->32 | 0.12 | 4 | |
| Ampicillin | ≤0.03-32 | 0.12 | 8 | |
| Amikacin | 16->32 | >32 | >32 | |
| Levofloxacin | 1-2 | 1 | 2 | |
| S. mitis (24) | CS-023 | ≤0.03-4 | ≤0.03 | 1 |
| Imipenem | ≤0.03-2 | ≤0.03 | 1 | |
| Meropenem | ≤0.03-4 | ≤0.03 | 1 | |
| Ceftriaxone | ≤0.03-4 | 0.06 | 4 | |
| Ampicillin | ≤0.03-16 | 0.12 | 16 | |
| Amikacin | 8->32 | 32 | >32 | |
| Levofloxacin | 0.5-32 | 1 | 32 | |
| S. sanguis (19) | CS-023 | ≤0.03-0.25 | ≤0.03 | 0.25 |
| Imipenem | ≤0.03-0.12 | ≤0.03 | 0.06 | |
| Meropenem | ≤0.03-0.5 | ≤0.03 | 0.25 | |
| Ceftriaxone | ≤0.03-0.5 | 0.12 | 0.5 | |
| Ampicillin | ≤0.03-2 | 0.06 | 1 | |
| Amikacin | 16->32 | >32 | >32 | |
| Levofloxacin | 0.5-8 | 1 | 2 | |
| Penicillin-susceptiblefS. pneumoniae (60) | CS-023 | ≤0.03 | ≤0.03 | ≤0.03 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ceftriaxone | ≤0.03-0.5 | 0.12 | 0.5 | |
| Ampicillin | ≤0.03-0.06 | ≤0.03 | ≤0.03 | |
| Amikacin | 8->32 | >32 | >32 | |
| Levofloxacin | 0.25-1 | 0.5 | 0.5 | |
| Penicillin-intermediategS. pneumoniae (42) | CS-023 | ≤0.03-0.25 | 0.06 | 0.12 |
| Imipenem | ≤0.03-0.25 | 0.06 | 0.12 | |
| Meropenem | ≤0.03-0.5 | 0.12 | 0.25 | |
| Ceftriaxone | ≤0.03-0.5 | 0.5 | 0.5 | |
| Ampicillin | ≤0.03-2 | 0.5 | 2 | |
| Amikacin | 16->32 | 32 | >32 | |
| Levofloxacin | 0.25-1 | 0.5 | 0.5 | |
| Penicillin-resistanthS. pneumoniae (47) | CS-023 | 0.06-0.5 | 0.12 | 0.25 |
| Imipenem | 0.06-0.5 | 0.25 | 0.5 | |
| Meropenem | 0.25-0.5 | 0.5 | 0.5 | |
| Ceftriaxone | 0.5-4 | 0.5 | 0.5 | |
| Ampicillin | 0.5-8 | 2 | 4 | |
| Amikacin | 32->32 | >32 | >32 | |
| Levofloxacin | 0.5-2 | 0.5 | 1 | |
| E. faecalis (25) | CS-023 | 0.25-8 | 2 | 8 |
| Imipenem | 0.5-2 | 1 | 2 | |
| Meropenem | 2-16 | 4 | 16 | |
| Ceftriaxone | 2->32 | >32 | >32 | |
| Ampicillin | 0.5->32 | 1 | 2 | |
| Amikacin | 32->32 | >32 | >32 | |
| Levofloxacin | 0.5->32 | 2 | >32 | |
| E. faecium (24) | CS-023 | 2->32 | >32 | >32 |
| Imipenem | 0.5->32 | >32 | >32 | |
| Meropenem | 8->32 | >32 | >32 | |
| Ceftriaxone | >32 | >32 | >32 | |
| Ampicillin | 2->32 | >32 | >32 | |
| Amikacin | 32->32 | >32 | >32 | |
| Levofloxacin | 2->32 | >32 | >32 | |
| P. asaccharolyticus (21) | CS-023 | ≤0.03 | ≤0.03 | ≤0.03 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ceftriaxone | ≤0.03-1 | ≤0.03 | 0.5 | |
| Levofloxacin | 0.5->32 | 2 | 32 | |
| P. anaerobius (25) | CS-023 | ≤0.03-4 | 0.12 | 2 |
| Imipenem | ≤0.03-1 | ≤0.03 | 0.5 | |
| Meropenem | ≤0.03-2 | 0.12 | 2 | |
| Ceftriaxone | 0.06-8 | 0.25 | 4 | |
| Levofloxacin | 0.12-32 | 0.25 | 32 | |
| P. magnus (25) | CS-023 | ≤0.03-0.06 | ≤0.03 | ≤0.03 |
| Imipenem | ≤0.03-0.06 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03-0.12 | ≤0.03 | ≤0.03 | |
| Ceftriaxone | ≤0.03-8 | 2 | 8 | |
| Levofloxacin | 0.06->32 | 2 | >32 | |
| P. acnes (25) | CS-023 | ≤0.03-0.12 | ≤0.03 | 0.12 |
| Imipenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Meropenem | ≤0.03-0.5 | ≤0.03 | 0.5 | |
| Ceftriaxone | ≤0.03-0.5 | 0.12 | 0.5 | |
| Levofloxacin | 0.12-0.5 | 0.25 | 0.5 | |
| M. catarrhalis (25) | CS-023 | ≤0.03 | ≤0.03 | ≤0.03 |
| Imipenem | ≤0.03-0.12 | 0.06 | 0.06 | |
| Meropenem | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ceftazidime | 0.06-0.25 | 0.06 | 0.12 | |
| Ceftriaxone | 0.06-2 | 0.5 | 1 | |
| Ampicillin | 0.5-32 | 8 | 16 | |
| Amikacin | 0.5-2 | 0.5 | 1 | |
| Levofloxacin | ≤0.03 | ≤0.03 | ≤0.03 | |
| Ampicillin-susceptibleiH. influenzae (65) | CS-023 | ≤0.03-0.5 | ≤0.03 | 0.25 |
| Imipenem | 0.12-4 | 0.5 | 0.5 | |
| Meropenem | ≤0.03-0.5 | ≤0.03 | 0.25 | |
| Ceftazidime | ≤0.03-8 | 0.06 | 0.5 | |
| Ceftriaxone | ≤0.03-0.5 | ≤0.03 | 0.25 | |
| Ampicillin | 0.12-2 | 0.5 | 2 | |
| Amikacin | 2-16 | 8 | 16 | |
| Levofloxacin | ≤0.03-0.5 | ≤0.03 | ≤0.03 | |
| β-lactamase-negative ampicillin-resistantjH. influenzae (11) | CS-023 | ≤0.03-0.5 | 0.12 | 0.25 |
| Imipenem | 0.25-4 | 0.5 | 4 | |
| Meropenem | ≤0.03-0.5 | 0.25 | 0.25 | |
| Ceftazidime | 0.12-0.5 | 0.25 | 0.25 | |
| Ceftriaxone | 0.12-0.25 | 0.12 | 0.25 | |
| Ampicillin | 4 | 4 | 4 | |
| Amikacin | 2-8 | 4 | 8 | |
| Levofloxacin | ≤0.03 | ≤0.03 | ≤0.03 | |
| E. coli (25) | CS-023 | ≤0.03-0.12 | ≤0.03 | ≤0.03 |
| Imipenem | 0.06-0.5 | 0.12 | 0.25 | |
| Meropenem | ≤0.03-0.25 | ≤0.03 | ≤0.03 | |
| Ceftazidime | 0.06-2 | 0.25 | 1 | |
| Ceftriaxone | ≤0.03-2 | ≤0.03 | 0.25 | |
| Ampicillin | 2->32 | 4 | >32 | |
| Amikacin | 1-8 | 2 | 4 | |
| Levofloxacin | ≤0.03->32 | 0.12 | 2 | |
| C. freundii (25) | CS-023 | ≤0.03-0.06 | ≤0.03 | 0.06 |
| Imipenem | 0.06-1 | 0.12 | 1 | |
| Meropenem | ≤0.03-0.06 | ≤0.03 | 0.06 | |
| Ceftazidime | 0.06->32 | 0.25 | >32 | |
| Ceftriaxone | ≤0.03->32 | 0.12 | >32 | |
| Ampicillin | 16->32 | >32 | >32 | |
| Amikacin | 0.5-2 | 1 | 2 | |
| Levofloxacin | ≤0.03-1 | 0.06 | 0.5 | |
| K. pneumoniae (25) | CS-023 | ≤0.03-0.12 | ≤0.03 | 0.06 |
| Imipenem | 0.06-1 | 0.12 | 0.5 | |
| Meropenem | ≤0.03-0.06 | ≤0.03 | ≤0.03 | |
| Ceftazidime | 0.06-16 | 0.25 | 2 | |
| Ceftriaxone | ≤0.03-0.5 | 0.06 | 0.25 | |
| Ampicillin | 16->32 | >32 | >32 | |
| Amikacin | 0.5-2 | 1 | 2 | |
| Levofloxacin | ≤0.03-8 | 0.06 | 1 | |
| K. oxytoca (25) | CS-023 | ≤0.03-0.12 | ≤0.03 | 0.12 |
| Imipenem | 0.12-0.5 | 0.25 | 0.5 | |
| Meropenem | ≤0.03-0.12 | ≤0.03 | 0.12 | |
| Ceftazidime | 0.06-4 | 0.25 | 2 | |
| Ceftriaxone | ≤0.03->32 | 0.06 | >32 | |
| Ampicillin | 32->32 | >32 | >32 | |
| Amikacin | 0.5-4 | 1 | 2 | |
| Levofloxacin | ≤0.03-16 | ≤0.03 | 8 | |
| E. cloacae (25) | CS-023 | ≤0.03-2 | 0.06 | 1 |
| Imipenem | 0.25-4 | 0.5 | 1 | |
| Meropenem | ≤0.03-4 | 0.12 | 0.5 | |
| Ceftazidime | 0.12->32 | 32 | >32 | |
| Ceftriaxone | 0.12->32 | >32 | >32 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | 0.5-32 | 1 | 16 | |
| Levofloxacin | ≤0.03-16 | 0.5 | 4 | |
| E. aerogenes (25) | CS-023 | ≤0.03-0.12 | ≤0.03 | 0.06 |
| Imipenem | 0.5-2 | 1 | 2 | |
| Meropenem | ≤0.03-0.12 | ≤0.03 | 0.06 | |
| Ceftazidime | 0.06->32 | 0.25 | 32 | |
| Ceftriaxone | ≤0.03-32 | 0.12 | 16 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | 0.5-2 | 2 | 2 | |
| Levofloxacin | ≤0.03-0.12 | ≤0.03 | 0.06 | |
| S. marcescens (50) | CS-023 | ≤0.03->32 | 0.06 | 0.25 |
| Imipenem | 0.25->32 | 2 | 4 | |
| Meropenem | ≤0.03->32 | 0.06 | 0.25 | |
| Ceftazidime | ≤0.03->32 | 0.12 | 16 | |
| Ceftriaxone | ≤0.03->32 | 0.25 | >32 | |
| Ampicillin | 4->32 | >32 | >32 | |
| Amikacin | 1->32 | 2 | 8 | |
| Levofloxacin | ≤0.03->32 | 0.12 | 2 | |
| P. vulgaris (25) | CS-023 | 0.12-0.25 | 0.25 | 0.25 |
| Imipenem | 4-8 | 4 | 8 | |
| Meropenem | 0.06-0.25 | 0.12 | 0.12 | |
| Ceftazidime | 0.12-16 | 0.5 | 4 | |
| Ceftriaxone | 4->32 | >32 | >32 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | 1-16 | 2 | 4 | |
| Levofloxacin | ≤0.03-32 | ≤0.03 | 0.12 | |
| P. mirabilis (25) | CS-023 | ≤0.03-0.5 | 0.12 | 0.25 |
| Imipenem | 0.12-8 | 4 | 4 | |
| Meropenem | ≤0.03-0.5 | 0.12 | 0.12 | |
| Ceftazidime | 0.06->32 | 0.12 | 2 | |
| Ceftriaxone | ≤0.03-8 | ≤0.03 | 0.12 | |
| Ampicillin | 0.5->32 | 2 | >32 | |
| Amikacin | 1-16 | 4 | 4 | |
| Levofloxacin | ≤0.03-1 | 0.06 | 0.12 | |
| M. morganii (25) | CS-023 | ≤0.03-0.5 | 0.25 | 0.25 |
| Imipenem | 4-8 | 4 | 4 | |
| Meropenem | 0.06-0.25 | 0.25 | 0.25 | |
| Ceftazidime | 0.06->32 | 4 | >32 | |
| Ceftriaxone | ≤0.03->32 | 0.25 | 32 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | 1-8 | 2 | 4 | |
| Levofloxacin | ≤0.03-8 | ≤0.03 | 2 | |
| P. rettgeri (25) | CS-023 | 0.12-4 | 0.25 | 4 |
| Imipenem | 0.5-32 | 2 | 4 | |
| Meropenem | ≤0.03-4 | 0.12 | 0.25 | |
| Ceftazidime | 0.06->32 | >32 | >32 | |
| Ceftriaxone | ≤0.03->32 | 0.25 | 16 | |
| Ampicillin | 1->32 | >32 | >32 | |
| Amikacin | 0.25-32 | 2 | 16 | |
| Levofloxacin | ≤0.03->32 | 0.12 | 16 | |
| P. aeruginosa (total, 100) | CS-023 | 0.06-32 | 0.5 | 4 |
| Imipenem | 0.25-32 | 1 | 16 | |
| Meropenem | 0.06->32 | 0.5 | 16 | |
| Ceftazidime | 1->32 | 4 | 32 | |
| Ceftriaxone | 4->32 | >32 | >32 | |
| Ampicillin | 32->32 | >32 | >32 | |
| Amikacin | 0.5->32 | 4 | 16 | |
| Levofloxacin | 0.12->32 | 0.5 | 16 | |
| P. aeruginosa (MIC of IPM, ≤8) (79) | CS-023 | 0.06-16 | 0.25 | 1 |
| Imipenem | 0.25-8 | 1 | 4 | |
| Meropenem | 0.06-16 | 0.5 | 2 | |
| Ceftazidime | 1->32 | 2 | 16 | |
| Ceftriaxone | 4->32 | >32 | >32 | |
| Ampicillin | 32->32 | >32 | >32 | |
| Amikacin | 0.5->32 | 4 | 16 | |
| Levofloxacin | 0.12->32 | 0.5 | 4 | |
| P. aeruginosa (MIC of IPM, >8) (21) | CS-023 | 1-32 | 4 | 16 |
| Imipenem | 16-32 | 16 | 32 | |
| Meropenem | 1->32 | 8 | 32 | |
| Ceftazidime | 2->32 | 32 | >32 | |
| Ceftriaxone | 16->32 | >32 | >32 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | 0.5->32 | 4 | 16 | |
| Levofloxacin | 0.25->32 | 1 | 32 | |
| B. cepacia (25) | CS-023 | 4-32 | 32 | 32 |
| Imipenem | 1-32 | 8 | 16 | |
| Meropenem | 0.25-8 | 2 | 4 | |
| Ceftazidime | 2-8 | 4 | 8 | |
| Ceftriaxone | 8->32 | >32 | >32 | |
| Ampicillin | 4->32 | >32 | >32 | |
| Amikacin | 16->32 | >32 | >32 | |
| Levofloxacin | 1-32 | 4 | 8 | |
| S. maltophilia (25) | CS-023 | 0.5->32 | >32 | >32 |
| Imipenem | 32->32 | >32 | >32 | |
| Meropenem | 0.12->32 | >32 | >32 | |
| Ceftazidime | 2->32 | 32 | >32 | |
| Ceftriaxone | >32 | >32 | >32 | |
| Ampicillin | >32 | >32 | >32 | |
| Amikacin | >32 | >32 | >32 | |
| Levofloxacin | 0.5-32 | 1 | 4 | |
| B. fragilis (24) | CS-023 | ≤0.03-16 | 0.12 | 0.5 |
| Imipenem | ≤0.03-4 | 0.12 | 0.25 | |
| Meropenem | ≤0.03-16 | 0.12 | 0.25 | |
| Ceftazidime | 8->32 | 16 | >32 | |
| Ceftriaxone | 2->32 | 32 | >32 | |
| Levofloxacin | 1-32 | 2 | 8 | |
50% and 90%, MICs at which 50% and 90%, respectively, of the isolates are inhibited.
MIC of oxacillin: 2 μg/ml or lower.
MIC of oxacillin: 4 μg/ml or higher.
MIC of oxacillin: 0.25 μg/ml or lower.
MIC of oxacillin: 0.5 μg/ml or higher.
MIC of benzylpenicillin: 0.06 μg/ml or lower.
MIC of benzylpenicillin: 0.12 to 1 μg/ml.
MIC of benzylpenicillin: 2 μg/ml or higher.
MIC of ampicillin: 2 μg/ml or lower.
MIC of ampicillin: 4 μg/ml or higher.
CS-023 showed highly potent activity against methicillin-susceptible S. aureus and methicillin-susceptible S. epidermidis, with MIC90s of ≤0.12 μg/ml. Imipenem showed the most potent activity among the reference compounds. Against MRSA, CS-023 was more active than the reference compounds, as indicated by a MIC90 fourfold or more lower than those of the reference compounds (MIC90 for MRSA, 8 μg/ml). Against methicillin-resistant Staphylococcus epidermidis, the MIC90s of CS-023, imipenem, and meropenem were 4, 8, and 8 μg/ml, respectively.
CS-023 showed high activity against most streptococci, including PRSP (MIC90s, ≤0.03 to 0.25 μg/ml) except for Streptococcus oralis and Streptococcus mitis. Its activity was comparable to or superior to those of the reference compounds. Although CS-023 exhibited potent activity against Enterococcus faecalis (MIC90, 8 μg/ml), it was less active than imipenem. All carbapenems were highly active against peptostreptococci.
CS-023 showed high activity against M. catarrhalis and ampicillin-susceptible H. influenzae, and the activity was comparable to that of meropenem. Against β-lactamase-negative ampicillin-resistant H. influenzae, CS-023 was as active as meropenem (MIC90, 0.25 μg/ml) and 16-fold more active than imipenem.
CS-023 showed consistently potent activity against the strains of the family Enterobacteriaceae, such as E. coli, Klebsiella spp., and Proteus spp., whose activities ranged from ≤0.03 to 1 μg/ml. The activity of CS-023 against the family Enterobacteriaceae except for Providencia rettgeri (MIC90, 4 μg/ml) was comparable to that of meropenem and stronger than that of imipenem. The activity of CS-023 was stronger than those of cephems against all members of the family Enterobacteriaceae tested, particularly against pathogens that commonly produce β-lactamases (e.g., Citrobacter freundii, Enterobacter spp., S. marcescens, and Morganella morganii).
CS-023 showed the most potent activity against P. aeruginosa (MIC90, 4 μg/ml), being fourfold more active than imipenem, meropenem, and levofloxacin. The MIC90s of CS-023, imipenem, and meropenem against Burkholderia cepacia were 32, 16, and 4 μg/ml, respectively. None of the carbapenems was highly potent against Stenotrophomonas maltophilia, although levofloxacin showed moderate activity. All carbapenems were highly active against B. fragilis.
Stability against β-lactamases.
Table 2 shows the stability of CS-023, imipenem, meropenem, and ceftriaxone against hydrolysis by β-lactamases from E. cloacae and P. vulgaris. CS-023, imipenem, and meropenem were quite stable against hydrolysis by both β-lactamases. Ceftriaxone was hydrolyzed by β-lactamase from P. vulgaris.
TABLE 2.
Stability of CS-023 to hydrolysis by β-lactamases
| Enzyme source | Relative rate of hydrolysisa
|
||||
|---|---|---|---|---|---|
| CS-023 | Imipenem | Meropenem | Ceftriaxone | Cephalothin | |
| E. cloacae | <0.10 | <0.10 | 0.12 | 0.51 | 100 |
| P. vulgaris | <0.10 | <0.10 | 0.13 | 58 | 100 |
Expressed as the percentage of hydrolysis of cephalothin.
Antibacterial activity of CS-023 against ESBL producers.
Table 3 shows the antibacterial activity of CS-023 and reference compounds against the host strain E. coli JM109 and its transformants (22), determined by the broth microdilution method. The MICs of CS-023 against transformants containing plasmids carrying TEM- and SHV-type ESBL genes were 0.016 μg/ml, showing that the magnitude of increase in MICs was two times that with the host. The MIC of CS-023 against the Toho-1 producers increased eight times, compared with that against the host, but was still as low as 0.06 μg/ml. Other carbapenems showed similar tendencies. The MICs of cephems and penicillins against TEM-3, -5, and -9, SHV-type ESBL, and Toho-1 producers increased more than 32 times compared with those against the host strain. The MICs of both amikacin and levofloxacin against all ESBL producers were uniform.
TABLE 3.
MICs of CS-023 and comparators against E. coli JM109 and its transformants having a plasmid encoding a β-lactamase gene
| Compound | MIC (μg/ml) against E. coli JM109 producing plasmid (β-lactamase type encoded):
|
|||||||
|---|---|---|---|---|---|---|---|---|
| None | pTEM-1 (TEM-1) | pTEM-2 (TEM-2) | pTEM-3 (TEM-3) | pTEM-5 (TEM-5) | pTEM-9 (TEM-9) | pSHV5a (SHV-12) | pMTY010 (Toho-1) | |
| CS-023 | 0.008 | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 | 0.06 |
| Imipenem | 0.06 | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 | 0.25 |
| Meropenem | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 | 0.06 |
| Cefotaxime | 0.06 | 0.06 | 0.06 | 16 | 4 | 4 | 8 | 16 |
| Ceftazidime | 0.25 | 0.25 | 0.5 | 32 | 64 | >128 | 64 | 64 |
| Ceftriaxone | 0.06 | 0.06 | 0.06 | >128 | 16 | 32 | 32 | >128 |
| Ampicillin | 4 | >128 | >128 | >128 | >128 | >128 | >128 | >128 |
| Amikacin | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0.5 |
| Levofloxacin | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 |
Efficacy against a murine systemic infection model.
Table 4, shows the protective effects of CS-023, imipenem/cilastatin, meropenem, ceftriaxone, and ceftazidime on a murine systemic infection model induced by a variety of pathogens. The protective effect of CS-023 was comparable to that of imipenem/cilastatin and stronger than those of the other compounds for infections induced by MRSA 507, PRSP 9605, and P. aeruginosa 1008. For the other gram-positive bacterial infections, its protective effect was comparable or inferior to that of imipenem/cilastatin and stronger than those of the other compounds evaluated. For the other gram-negative bacterial infections, its protective effect was generally less active than that of ceftriaxone and stronger than those of the other compounds evaluated.
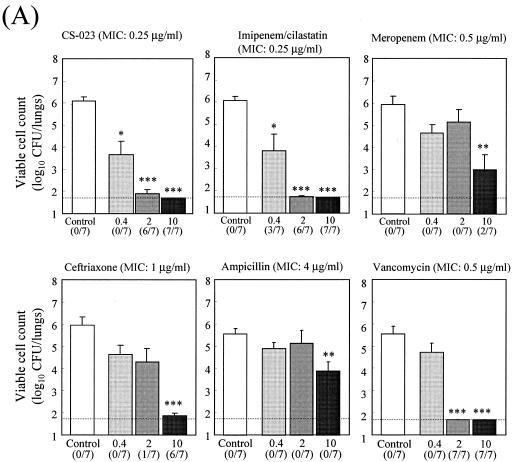
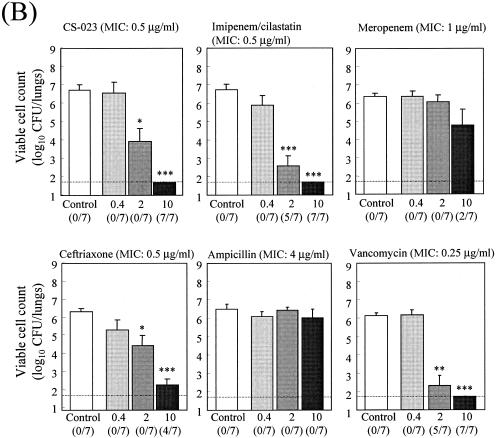
Efficacy against a murine pneumonia model induced by PRSP.
Fig. 2 shows the therapeutic efficacy of CS-023 and reference compounds with a pneumonia model induced by two PRSP strains. CS-023 exhibited dose-dependent efficacy against both infections at doses of 0.4, 2, and 10 mg/kg. CS-023 showed efficacy comparable with those of imipenem/cilastatin and vancomycin and stronger efficacy than those of the other compounds evaluated against a pneumonia model induced by PRSP 9601 (Fig. 2A). It showed significant reductions in viable cell counts in the lungs at doses of 0.4, 2, and 10 mg/kg. CS-023 showed efficacy comparable to those of imipenem/cilastatin and vancomycin and stronger efficacy than those of the other compounds evaluated against a pneumonia model induced by PRSP 10691 (Fig. 2B). It showed significant reductions in viable cell counts in the lungs at doses of 2 and 10 mg/kg.
FIG. 2.
Therapeutic efficacies of CS-023 and reference compounds against a pneumonia model induced by PRSP 9601 (A) and 10931 (B). Each column and bar represents the mean ± standard error, respectively (n = 7). The indicated doses of each compound were administered subcutaneously twice daily for 2 days beginning 18 h after infection, and the numbers of viable cells in the lungs of mice were determined 66 h after infection. The asterisks indicate a significant difference compared with the results for the control group (*, P < 0.05; **, P < 0.01; ***, P < 0.001). The dotted line indicates the detection limit. The numbers in parentheses indicate the numbers of culture-negative mice per group whose viable cell counts were below the detection limit.
Pharmacokinetics of compounds in plasma.
Table 5 shows the pharmacokinetic parameters of CS-023 and the reference compounds in plasma after a single subcutaneous administration at 20 mg/kg. The concentrations of CS-023 in plasma were higher than those of meropenem, almost similar to those of imipenem, and lower than those of the other compounds. The mean peak level (±standard error) of CS-023 was 20.0 ± 1.9 μg/ml at 0.25 h after administration. At 2 h, the concentration of CS-023 was below the detection limit. The half-life of CS-023 was 0.18 h, compared with 0.14 h for imipenem/cilastatin, 0.10 h for meropenem, 0.21 h for ceftazidime, and 0.83 h for ceftriaxone.
TABLE 5.
Pharmacokinetics of CS-023 in mouse plasmaa
| Compound | Tmax (h) | Cmax (μg/ml) | t1/2 | AUC0-2 (μg · h/ml) |
|---|---|---|---|---|
| CS-023 | 0.25 | 20.0 ± 1.9 | 0.18 | 12.7 |
| Imipenem/cilastatin | 0.25 | 24.9 ± 1.7 | 0.14 | 13.5 |
| Meropenem | 0.083 | 14.6 ± 2.1 | 0.10 | 6.70 |
| Ceftazidime | 0.25 | 30.9 ± 3.1 | 0.21 | 19.3 |
| Ceftriaxone | 0.25 | 45.4 ± 4.6 | 0.83 | 51.2 |
Abbreviations: Tmax, time to maximum concentration of compound in plasma; Cmax, maximum concentration of compound in plasma; t1/2, half-life; AUC0-2, area under the concentration-time curve from time zero to 2 h.
DISCUSSION
CS-023 showed potent antibacterial activity with a broad antibacterial spectrum that encompasses a wide range of gram-positive and -negative aerobic and anaerobic pathogens. Overall, CS-023 demonstrated in vitro activity comparable to that of imipenem against most isolates of gram-positive pathogens and similar to that of meropenem against gram-negative pathogens. These findings were consistent with the results obtained by using United States and European clinical isolates (6, 23). A characteristic of CS-023 is its improved activity against MRSA and P. aeruginosa compared with the other carbapenems tested. We have evaluated the stability against commercially available β-lactamases only in this study; however, CS-023 was very stable against two types of β-lactamases of Enterobacteriaceae, such as E. cloacae and P. vulgaris, compared with ceftriaxone. This suggests that the high stability of CS-023 against these β-lactamases is one reason for its potent activity against clinical isolates of the family Enterobacteriaceae. However, 1 of 50 clinical isolates of S. marcescens tested was resistant to carbapenems, including CS-023. Recently, newer β-lactamases hydrolyzing imipenem have been identified from clinical isolates of S. marcescens (17). The carbapenem-resistant S. marcescens strain used in this study might produce carbapenem-hydrolyzing β-lactamase. The stability of CS-023 against other groups of β-lactamases, such as metallo- and OXA-type β-lactamases, remains to be elucidated.
The MICs of parenteral cephems and penicillins tested against TEM- and SHV-type ESBL producers were increased more than 32 times over those against the host strain. The antibacterial activities of CS-023 and other carbapenems were virtually unchanged against the ESBL producers tested. This property is one of the advantages of CS-023 as well as other carbapenems over cephems and penicillins.
The therapeutic efficacy of CS-023 was comparable to that of imipenem/cilastatin in a systemic infection model induced by MRSA, PRSP, and P. aeruginosa. CS-023 also showed efficacy comparable to those of imipenem/cilastatin and vancomycin in a pneumonia model induced by two serotypes of PRSP. Plasma concentrations were different among the compounds tested. Since meropenem is unstable against mouse renal dehydropeptidase I (4, 24), the difference could be due to faster elimination than the other compounds evaluated. Ceftriaxone maintained a relatively high concentration and showed a long half-life, this result being consistent with that of a previous report (12). In the present study, the pharmacokinetics of each compound in uninfected mice was determined. The relationship between pharmacokinetic data and therapeutic efficacy was not evaluated, since the underlying infection may have a dramatic effect on systemic pharmacokinetics as well as distribution properties at the infected site depending on the compounds. However, therapeutic efficacy of CS-023 is considered to reflect the in vitro potent antibacterial activity of CS-023. One of the reasons for this would be the low level of protein binding of CS-023 in serum. The protein binding values of CS-023 were 17.6% and 9.5% in mouse and human sera, respectively (T. Shibayama et al., unpublished data). The protein binding values found for CS-023, imipenem (2%) (8), meropenem (33.8%) (21), and ceftazidime (17.9%) (16) have a similar tendency in mice, since protein binding values of less than 70% for β-lactams would have minimal impact on penetration (26). On the contrary, the protein binding of ceftriaxone in mice has been reported to be >80% (12). It is suggested that the effectiveness of CS-023 in mouse models results from its low level of protein binding.
Human plasma pharmacokinetics of CS-023 predicted a longer half-life than that of imipenem/cilastatin by the Detrick plot method (2), which is based on the allometric relationship between body weight and pharmacokinetic parameters, although mouse plasma pharmacokinetics of CS-023 was comparable to that of imipenem/cilastatin (20). This prediction was confirmed by demonstrating that CS-023 (1.5 to 2.1 h) showed a much longer half-life than imipenem/cilastatin (1.0 h) (13) and meropenem (0.9 h) (19) in a study with healthy male volunteers (18). These results suggest that CS-023 could show more-potent efficacy in clinical practice than it showed with the mouse model.
In conclusion, the new parenteral administered carbapenem CS-023 is considered to be an extremely promising compound for further evaluation. Its antibacterial activity would cover not only P. aeruginosa but also MRSA encountered in the treatment of nosocomial infections. Clinical studies on CS-023 are in progress globally in Japan, Europe, and the United States.
REFERENCES
- 1.Bliss, C. I. 1934. The method of probits. Science 79:38-39. [DOI] [PubMed] [Google Scholar]
- 2.Boxenbaum, H. 1984. Interspecies pharmacokinetic scaling and the evolutionary-comparative paradigm. Drug Metab. Rev. 15:1071-1121. [DOI] [PubMed] [Google Scholar]
- 3.Clissold, S. P., P. A. Todd, and D. M. Campoli-Richards. 1987. Imipenem/cilastatin. A review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy. Drugs 33:183-241. [DOI] [PubMed] [Google Scholar]
- 4.Edwards, J. R. 1995. Meropenem: a microbiological overview. J. Antimicrob. Chemother. 36(Suppl. A):1-17. [DOI] [PubMed] [Google Scholar]
- 5.Fukuoka, T., H. Kawada, A. Kitayama, T. Koga, M. Kubota, T. Harasaki, Y. Kamai, S. Ohya, H. Yasuda, M. Iwata, and S. Kuwahara. 1998. Efficacy of CS-834 against experimental pneumonia caused by penicillin-susceptible and -resistant Streptococcus pneumoniae in mice. Antimicrob. Agents Chemother. 42:23-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fukuoka, T., K. Puchler, J. Rennecke, and S. Kuwahara. 2000. In vitro activity of CS-023 against European clinical relevant bacterial isolates, abstr. F-326. In Abstracts of the 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology, Washington, D.C.
- 7.Goa, K. L., and S. Noble. 2003. Panipenem/betamipron. Drugs 63:913-925. [DOI] [PubMed] [Google Scholar]
- 8.Hamajima, K., H. Kobayashi, K. Kamei, M. Shibata, J. Horikoshi, and K. Hayase. 1985. Plasma levels and urinary excretion of imipenem and cilastatin sodium in dogs and rabbits. Chemotherapy (Tokyo) 33(Suppl. 4):315-328. [Google Scholar]
- 9.Hikida, M., S. Terashima, Y. Sato, R. Okamoato, and M. Inoue. 2001. Comparative antibacterial activity of carbapenems against P. aeruginosa (1). Jpn. J. Antibiot. 54:571-579. [PubMed] [Google Scholar]
- 10.Hisaoka, M., M. Ichikawa, and T. Terao. 1991. Microbiological assay method for the determination of panipenem concentration in body fluids. Chemotherapy (Tokyo) 39(Suppl. 3):190-196. [Google Scholar]
- 11.Kobayashi, Y., and T. Matsushima. 2003. Clinical analysis of patients requiring long-term mechanical ventilation of over three months: ventilator-associated pneumonia as a primary complication. Intern. Med. 42:25-32. [DOI] [PubMed] [Google Scholar]
- 12.Moine, P., E. Vallee, E. Azoulay-Dupuis, P. Bourget, J. P. Bedos, J. Bauchet, and J. J. Pocidalo. 1994. In vivo efficacy of a broad-spectrum cephalosporin, ceftriaxone, against penicillin-susceptible and -resistant strains of Streptococcus pneumoniae in a mouse pneumonia model. Antimicrob. Agents Chemother. 38:1953-1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakagawa, K., and M. Koyama. 1985. Imipenem, cilastatin sodium, imipenem/cilastatin sodium clinical phase I study. Chemotherapy (Tokyo) 33(Suppl. 4):357-378. [Google Scholar]
- 14.National Committee for Clinical Laboratory Standards. 1997. Methods for antimicrobial susceptibility testing of anaerobic bacteria, 4th ed., approved standard M11-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 15.National Committee for Clinical Laboratory Standards. 2000. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 5th ed., approved standard M7-A5. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 16.Okumura, K., H. Tsuiji, K. Takeda, I. Fukuda, T. Nagaki, M. Takano, K. Higo, and J. Kinami. 1983. Absorption, distribution metabolism and excretion of ceftazidime in mice, rats and rabbits. Chemotherapy (Tokyo) 31(Suppl. 3):188-198. [Google Scholar]
- 17.Osano, E., Y. Arakawa, R. Wacharotayankun, M. Ohta, T. Horii, H. Ito, F. Yoshimura, and N. Kato. 1994. Molecular characterization of an enterobacterial metallo β-lactamase found in a clinical isolate of Serratia marcescens that shows imipenem resistance. Antimicrob. Agents Chemother. 38:71-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rennecke, J., T. Hirota, T. Shibayama, Y. Matsushita, S. Kuwahara, K. Puchler, A. Ruhland, and B. Drewelow. 2002. Safety, tolerability, and pharmacokinetics (PK) of CS-023, a new parenteral carbapenem, in healthy male volunteers, abstr. F-327. In Abstracts of the 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology. Washington, D.C.
- 19.Saito, A. 1992. Pharmacokinetic study on meropenem. Chemotherapy (Tokyo) 40(Suppl. 1):276-282. [Google Scholar]
- 20.Shibayama, T., N. Matsushita, N. Kikuchi, K. Kawai, T. Hirota, and S. Kuwahara. 2000. R-115685, a novel parenteral carbapenem: pharmacokinetic and metabolism in laboratory animals, abstr. F-1233. In Abstracts of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology. Washington, D.C.
- 21.Sumita, Y., H. Nouda, E. Tada, T. Kohzuki, M. Kato, T. Okuda, and M. Fukasawa. 1992. Pharmacokinetics of meropenem, a new carbapenem antibiotic, parenterally administrated to laboratory animals. Chemotherapy (Tokyo) 40(Suppl. 1):123-131. [Google Scholar]
- 22.Takenouchi, T., Y. Ishii, and K. Yamaguchi. 2002. Properties of extended-spectrum β-lactamases constructed by site-directed mutagenesis. J. Infect. Chemother. 8:211-217. [DOI] [PubMed] [Google Scholar]
- 23.Thomson, K. S., and E. S. Moland. 2004. CS-023 (R-115685), a novel carbapenem with enhanced in vitro activity against oxacillin-resistant staphylococci and Pseudomonas aeruginosa. J. Antimicrob. Chemother. 54:557-562. [DOI] [PubMed] [Google Scholar]
- 24.Tsuji, M., Y. Ishii, A. Ohno, S. Miyazaki, and K. Yamaguchi. 1998. In vitro and in vivo antibacterial activities of S-4661, a new carbapenem. Antimicrob. Agents Chemother. 42:94-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waley, S. G. 1974. A spectrophotometric assay of β-lactamase action on penicillins. Biochem. J. 139:789-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wise, R., A. P. Gillett, B. Cadge, S. R. Durham, and S. Baker. 1980. The influence of protein binding upon tissue fluid levels of six beta-lactam antibiotics. J. Infect. Dis. 142:77-82. [DOI] [PubMed] [Google Scholar]
- 27.Wiseman, L. R., A. J. Wagstaff, R. N. Brogden, and H. M. Bryson. 1995. Meropenem. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs 50:73-101. [DOI] [PubMed] [Google Scholar]