Abstract
Background
Refraction disorders are the leading cause of visual impairment worldwide. This study investigates the global burden and trends of refraction disorders from 1990 to 2021, with projections extending to 2050.
Methods
Data on prevalence and disability-adjusted life years (DALYs) for refraction disorders, along with their 95% uncertainty intervals (UIs), were obtained from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021. The study provides a comprehensive analysis of the epidemiology of refraction disorders at global, regional, and national levels. It examines trends from 1990 to 2021 from multiple dimensions, including overall and localized changes. Burden decomposition was performed to assess contributions from population size, age structure, and epidemiological changes. Cross-country inequalities were quantified using standard health equity methods recommended by the World Health Organization. Future changes in the burden of refraction disorders were also projected through 2050.
Results
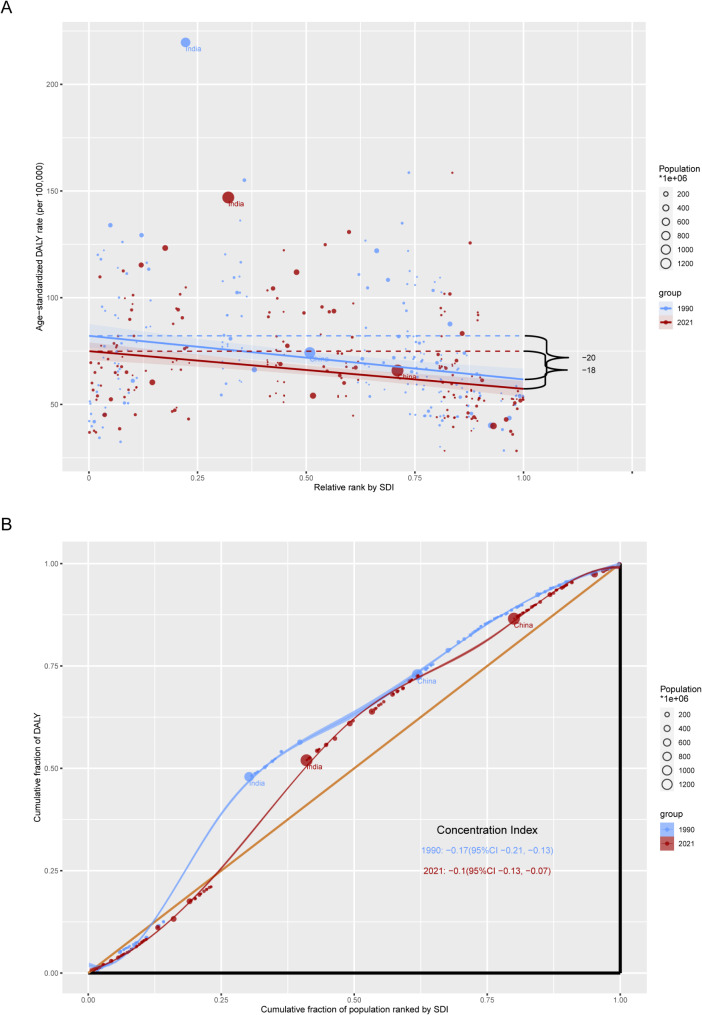
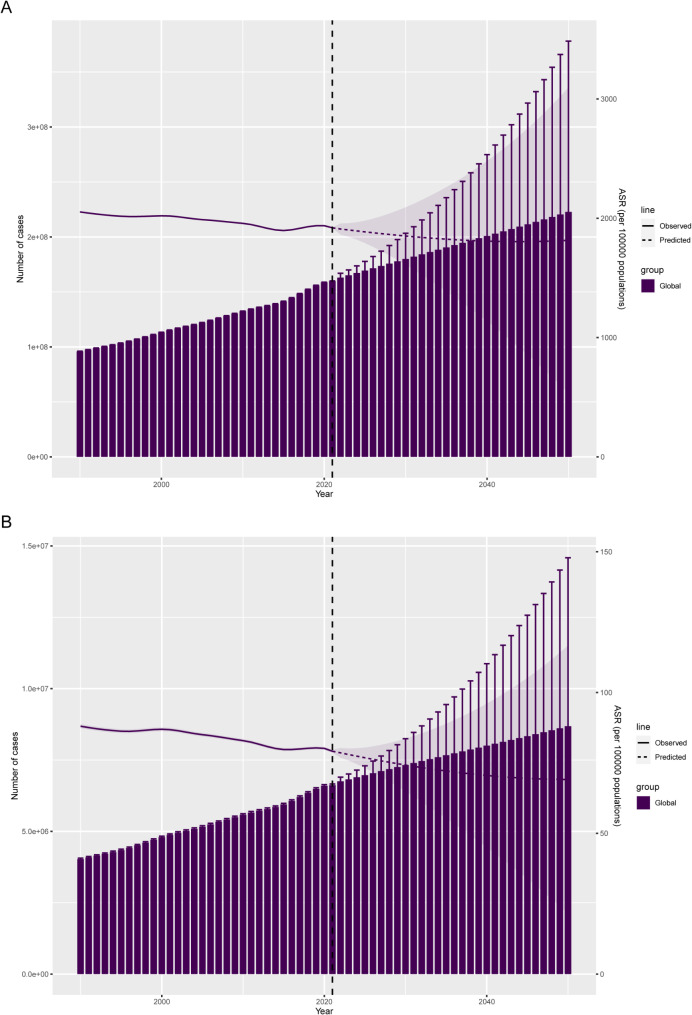
According to GBD 2021 estimates, there were 159,765,917 prevalent cases (95% UI: 142,526,915–178,698,348) and 6,618,600 DALYs (95% UI: 4,599,082–9,528,676) due to refraction disorders globally in 2021. From 1990 to 2021, prevalence and DALYs rates demonstrated a steady decline, although prevalence numbers, incidence numbers, and rates were consistently higher among females compared to males. Decomposition analysis showed that aging, population growth, and epidemiological changes contributed 36.25%, 76.92%, and − 13.18%, respectively, to changes in the age-standardized prevalence rate (ASR). The concentration index declined from − 0.17 (95% CI: −0.21 to − 0.13) in 1990 to − 0.10 (95% CI: −0.13 to − 0.07) in 2021, indicating a reduction in SDI-related inequalities. By 2050, the ASR for prevalence and DALYs is projected to decline to 1815.27 (95% UI: 534.15–3096.40) and 69.11 (95% UI: 21.45–116.77), respectively.
Conclusion
The global burden of refraction disorders decreased significantly from 1990 to 2021 and is expected to decline further by 2050. Females continue to experience a greater burden compared to males. Population growth emerged as the primary driver of changes in the ASR of prevalence and DALYs. While countries with low socio-demographic index (SDI) face a disproportionately high burden, SDI-related inequalities have gradually lessened over time.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-22440-w.
Keywords: Refraction disorders, Global burden of disease, Prevalence, Disability-adjusted life years
Background
Refraction disorders, such as myopia, hyperopia, and astigmatism, are complex ocular conditions with multifactorial origins, though their exact causes remain unclear [1]. These disorders affect a significant portion of the global population, representing the leading cause of visual impairment and the second leading cause of blindness after cataracts [2]. The consequences of uncorrected refractive error (URE) are substantial, as socioeconomic factors like poverty and limited access to healthcare often hinder timely correction. Additionally, URE can exacerbate economic challenges for affected individuals and their families [3]. Vision impairment (VI) from URE has wide-reaching social and economic repercussions, restricting educational and employment opportunities for individuals and communities. For instance, Varma et al. estimated that 8.4 million adults in the United States experienced VI from URE (20/40 or worse), with another 0.29 million cases of blindness due to URE [4]. The prevalence of URE is expected to double by 2050 in the U.S., with over 10% prevalence in 15 states. Among Americans aged ≥ 50 years, approximately 1 in 8 experiences near-VI worse than 20/40 [5]. Globally, by 2050, an estimated 1.8 billion people are projected to suffer vision loss from refraction disorders [6]. Smith et al. reported that UREs result in a global economic loss of $269 billion annually due to reduced productivity [7].
Fortunately, VI from refractive disorders is largely preventable. More than 90% of such cases can be avoided through existing cost-effective interventions [8]. The year 2020 marked the culmination of VISION 2020: The Right to Sight, a global initiative to eliminate avoidable blindness, in which refractive disorders were identified as one of five priority conditions [9]. Building on this, the World Health Organization set a global target of a 40% increase in effective refractive error coverage by 2030, established at the 73rd World Health Assembly [10].
Despite these efforts, refractive disorders remain a significant global health challenge, particularly in low-income and remote areas [11, 12]. For instance, in Nigeria, URE was closely linked to poverty, with eyeglass usage being three times lower in poorer households [13]. Factors such as nonwhite ethnicity, older age, lower educational attainment, lack of private health insurance, and poverty are associated with a higher risk of near-VI [5]. The Global Burden of Disease (GBD) study provides valuable data on the prevalence and trends of refractive disorders across diverse regions, enabling assessments of disease burden based on factors like geography, age, gender, and socio-demographic index (SDI). Leveraging data from GBD 2021, this study seeks to provide an updated and comprehensive analysis of the burden, trends, and inequalities associated with refractive disorders [14]. It aims to offer critical insights to inform targeted prevention strategies and improve outcomes for affected populations.
Method
Data acquisition
The 2021 GBD study provides an extensive analysis of health loss related to 369 diseases, injuries, and impairments, as well as 88 risk factors, across 204 countries and territories. This study leverages the latest epidemiological data and refined standard methods to ensure reliable findings [15]. Advanced techniques are used in the GBD database to handle missing data and adjust for confounding factors. Further details on the study’s design and methodology are available in previous GBD literature [16]. For this analysis, we extracted prevalence and disability-adjusted life years (DALYs), along with their 95% uncertainty intervals (UIs), for refraction disorders from the GBD 2021 dataset. DALYs are calculated by summing years lived with disability (YLDs) and years of life lost due to premature death. For refraction disorders specifically, DALYs equal YLDs, per GBD 2021 definitions [17]. We also used the SDI, a composite indicator of a country’s development level based on fertility, education, and income levels [18]. With SDI values ranging from 0 to 1, we categorized countries and regions into five SDI levels (low to high) to examine the relationship between the burden of refraction disorders and socioeconomic development.
Burden description
In 2021, a comprehensive analysis was conducted to quantify the national burden of refraction disorders, focusing on their prevalence and associated DALYs. This study also investigated demographic factors affecting the impact of refraction disorders, assessing burden distribution across age groups and genders.
Joinpoint regression analysis
The Joinpoint regression model, commonly used in epidemiology for trend analysis, was applied here to assess temporal trends in the prevalence of refraction disorders at global, continental, and national levels. This model identifies significant trend changes in time-series data, facilitating calculations of annual percent change (APC) with corresponding 95% confidence intervals (CI) over specified periods. Additionally, the average annual percent change (AAPC) was calculated to provide an overview of trends from 1990 to 2021.
Age-period-cohort analysis
We used the age-period-cohort model to analyze trends in prevalence and DALYs for refraction disorders. The age-period-cohort model, often employed to assess trends in chronic disease metrics, explores age, period, and cohort effects to describe disease trends and predict future trajectories. Given the inherent linear relationship among these three factors (period = age + cohort), estimating parameters can be challenging. This study addressed this by developing estimable age-period-cohort parameters and functions without imposing constraints on the model parameters. The model was implemented using R tools, with detailed methods described in prior literature [19–22]. Prevalence and DALYs data for refraction disorders from GBD 2021, along with population data, were used as inputs. Data for 20 age groups (0–4, 5–9,…, 95+) and six time periods (1992–1996, 1997–2001,…, 2017–2021) were structured to represent age and period-specific trends. The model calculated age-period-cohort in age-specific prevalence and DALYs, with a randomly selected reference group for the cohort [23]. Relative risk was used to estimate age-specific incidence ratios, and statistical significance was assessed using the Wald χ2 test (P < 0.05). All analyses were conducted in R (version 4.2.1).
Decomposition analysis
Decomposition analysis was used to quantify how changes in age structure, population size, and epidemiology contribute to overall trends. This method helps highlight heterogeneity in demographic and epidemiological patterns [24]. Using Das Gupta’s decomposition method [25], we examined changes in age structure (reflecting population aging), population size (reflecting population growth), and epidemiological factors (reflecting incidence and mortality rates) for refraction disorders burden from 1990 to 2021 [26].
Cross-country inequality analysis
Monitoring health inequalities is essential for evidence-based health planning, helping inform policies to address disparities. In this study, we used the slope index of inequality and concentration index to assess inequalities in refraction disorders burden across countries [27, 28]. The slope index of inequality was derived by regressing national DALY rates against a relative position scale linked to sociodemographic development, while the concentration index was calculated from the area under the Lorenz curve, constructed using the cumulative distribution of DALYs and the cumulative population distribution ranked by SDI [25].
Predictive analysis
To inform public health policy and resource allocation, we conducted a prediction analysis of the future burden of refraction disorders. Using the Bayesian age-period-cohort (BAPC) model with integrated nested Laplace approximation (INLA), which offers improved coverage and precision over traditional APC models, we projected the global burden of refraction disorders to 2050 [28]. INLA with BAPC model approximates marginal posterior distributions, which can avoid convergence issues and mixing problems associated with Bayesian methods that rely on Markov Chain Monte Carlo techniques [29].
Result
Global level
In 2021, refraction disorders continued to pose a substantial global health challenge, with an estimated prevalence of 159,765,917 cases (95% UI: 142,526,915–178,698,348). The age-standardized prevalence rate (ASPR) decreased from 2,053.56 per 100,000 individuals (95% UI: 1,835.31–2,275.8) in 1990 to 1,919.66 per 100,000 (95% UI: 1,715.24–2,135.28) in 2021 (Table 1; Fig. 1A). DALYs associated with refraction disorders reached 6,618,600 cases (95% UI: 4,599,082–9,528,676) in 2021. Furthermore, the age-standardized rate (ASR) of DALYs declined from 88.04 per 100,000 (95% UI: 62.19–125.15) in 1990 to 79.11 per 100,000 (95% UI: 54.94–114.14) in 2021 (Table 1; Fig. 1B).
Table 1.
The case number and ASR of prevalence and dalys for refraction disorders in 1990 and 2021 by SDI quintiles and GBD regions
| Location | Prevalence (95% uncertainty interval) | DALYs (95% uncertainty interval) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases (1990) |
ASR (1990) |
Cases (2021) |
ASR (2021) |
Cases (1990) |
ASR (1990) |
Cases (2021) |
ASR (2021) |
||
| Global (both sex) | 95978319 (86236197–106044403) | 2053.56 (1835.31–2275.8) | 159765917 (142526915–178698348) | 1919.66 (1715.24–2135.28) | 4029084 (2821217–5812174) | 88.04 (62.19–125.15) | 6618600 (4599082–9528676) | 79.11 (54.94–114.14) | |
| Global (female) | 50828803 (45686966–56154379) | 2122.71 (1898.65–2359.66) | 85542335 (76384917–95629800) | 2010.3 (1795.38–2236.72) | 2135778 (1498780–3063246) | 90.52 (63.93–128.48) | 3549323 (2475790–5089344) | 82.63 (57.5–118.94) | |
| Global (male) | 45149517 (40528116–49979248) | 1988.64 (1779.77–2199.85) | 74223582 (66109341–83068548) | 1828.35 (1631.82–2032.97) | 1893306 (1319889–2748928) | 85.73 (60.55–122.05) | 3069277 (2123253–4439332) | 75.52 (52.31–109.24) | |
| High SDI | 11796392 (10574699–12980520) | 1266.1 (1134.08–1396.02) | 16532003 (14744586–18239386) | 1286.91 (1153.4–1412.4) | 460957 (314571–669985) | 48.76 (32.95–71.39) | 651929 (453966–929362) | 48.7 (32.87–71.33) | |
| High-middle SDI | 18429393 (16515827–20423165) | 1781.54 (1594–1976.58) | 27421792 (24305264–30943682) | 1717.63 (1535.02–1903.64) | 748735 (523143–1078997) | 72.61 (50.9–104.27) | 1136033 (792645–1626121) | 69.3 (47.99–100.28) | |
| Middle SDI | 30450445 (27410659–33726613) | 2222.7 (1989.98–2471.07) | 54543247 (48754426–61052227) | 2083.27 (1863.56–2310.25) | 1306760 (908852–1882212) | 99.52 (71.24–139.67) | 2311240 (1613507–3308195) | 87.81 (61.48–126.06) | |
| Low-middle SDI | 27847244 (24958860–30907719) | 3469.56 (3090.76–3878.16) | 46004885 (40990725–51552083) | 2774.05 (2453.7–3115.98) | 1191346 (834617–1705275) | 155.73 (110.68–218.15) | 1886272 (1297734–2736015) | 115.82 (80.26–165.83) | |
| Low SDI | 7378532 (6606296–8197508) | 2338.79 (2086.21–2609.68) | 15155638 (13499747–16856286) | 2062.51 (1826.09–2328.2) | 318437 (222737–452158) | 107.51 (77.31–149.99) | 629029 (435086–910576) | 89.83 (62.97–126.44) | |
| Andean Latin America | 857004 (769940–947111) | 2733.78 (2448.24–3024.76) | 1711240 (1539436–1893867) | 2642.66 (2381.51–2927.88) | 33925 (22875–49853) | 113.29 (78.18–164.54) | 66855 (45187–97656) | 103.92 (70.64–151.08) | |
| Australasia | 283175 (254230–311935) | 1372.15 (1232.94–1524.83) | 458789 (408260–506019) | 1370.99 (1223.5–1526.15) | 10426 (7097–15435) | 50.09 (34.07–74.3) | 17272 (11889–25063) | 49.73 (33.15–73.88) | |
| Caribbean | 596665 (531840–662766) | 1831.48 (1639.68–2029.86) | 854693 (761320–954030) | 1717.08 (1531.96–1909.93) | 23031 (15497–34081) | 72.39 (49.28–106.48) | 33093 (22425–49070) | 65.96 (44.48–97.75) | |
| Central Asia | 1068170 (955419–1188286) | 1826.84 (1619.37–2049.87) | 1599533 (1409713–1804634) | 1746.41 (1546.44–1964.81) | 39882 (26628–59063) | 69.16 (46.84–101.42) | 59718 (40061–88841) | 65.59 (44.25–97.47) | |
| Central Europe | 1763264 (1554068–1997193) | 1282.96 (1137.58–1436.73) | 2044563 (1782705–2326908) | 1259.82 (1114.76–1410.88) | 62153 (41054–91617) | 45.19 (29.83–67) | 72485 (48717–105660) | 44.5 (29.49–65.52) | |
| Central Latin America | 3173170 (2840150–3534416) | 2412.28 (2160.22–2667.54) | 5734174 (5118445–6344218) | 2226.69 (1990.96–2459.71) | 131636 (90119–189569) | 106.26 (74.75–152.23) | 240347 (166816–349851) | 93.6 (65.18–135.81) | |
| Central Sub-Saharan Africa | 534501 (473470–600708) | 1706.33 (1515.21–1921.43) | 1391685 (1239630–1546248) | 1741.79 (1548.33–1952.78) | 19134 (12715–28438) | 63.79 (43.85–92.54) | 49849 (32874–74546) | 64.98 (44.13–94.29) | |
| East Asia | 15325817 (13678032–17105161) | 1557.41 (1387.6–1731.54) | 27707612 (24235005–31689353) | 1456.79 (1291.02–1629.15) | 708410 (507328–982029) | 73.35 (53.26–100.85) | 1264468 (893967–1758611) | 64.98 (46–91.1) | |
| Eastern Europe | 5691994 (5078235–6394207) | 2241.99 (2007.75–2503.35) | 5992338 (5304238–6778118) | 2188.17 (1961.21–2444.5) | 206374 (138674–303154) | 81.17 (54.56–120.6) | 214816 (143055–316878) | 78.06 (52.35–115.98) | |
| Eastern Sub-Saharan Africa | 1436051 (1282887–1589453) | 1121.13 (1014.05–1235.77) | 3244072 (2869561–3609905) | 1068.75 (958.13–1188.04) | 65472 (46025–93093) | 56.42 (41.36–77.58) | 143294 (100041–205828) | 51.29 (36.68–71.99) | |
| High-income Asia Pacific | 2122794 (1903099–2348266) | 1189.5 (1071.02–1307.36) | 2769221 (2466596–3070249) | 1192.53 (1070.1–1310.75) | 83451 (56730–121337) | 46.26 (31.31–67.56) | 113455 (79621–161746) | 45.78 (31.03–67.33) | |
| High-income North America | 3080307 (2766556–3406529) | 1051.17 (935.58–1165.51) | 4279805 (3813432–4707427) | 1065.69 (950.02–1181.34) | 118905 (80870–173610) | 39.97 (26.92–58.58) | 165979 (114395–239719) | 39.69 (26.6–58.45) | |
| North Africa and Middle East | 6586898 (5939819–7292767) | 2386.92 (2147.7–2636.84) | 12976695 (11647714–14349490) | 2280.95 (2040.24–2514.18) | 276369 (189259–403521) | 106.87 (75.37–151.65) | 539124 (370628–782669) | 97.01 (67.72–139.63) | |
| Oceania | 112742 (100089–126892) | 2595.06 (2253.14–2965.26) | 259189 (226992–291462) | 2518.86 (2183.35–2876.59) | 3656 (2353–5560) | 83.02 (53.33–126.54) | 8294 (5272–12522) | 79.66 (50.59–121.23) | |
| South Asia | 32081349 (28516567–36037814) | 4446.18 (3962.59–5006.29) | 55485190 (49062021–62842997) | 3397.67 (2991.52–3859.72) | 1391910 (972604–1965521) | 201.54 (144.62–281.61) | 2285352 (1576821–3281211) | 141.73 (98.52–201.42) | |
| Southeast Asia | 7178590 (6390500–8012839) | 1838.75 (1644.85–2042.66) | 11320903 (10179658–12496512) | 1633.62 (1470.42–1800.88) | 288187 (193142–422905) | 77.89 (53.77–111.99) | 451649 (305473–661764) | 65.31 (44.11–95.59) | |
| Southern Latin America | 967604 (869171–1072960) | 1978.74 (1782.79–2187.75) | 1363645 (1215905–1512654) | 1893.73 (1692.83–2098.87) | 36046 (23944–53479) | 74.15 (49.72–109.58) | 50358 (34087–74033) | 68.76 (45.66–101.75) | |
| Southern Sub-Saharan Africa | 602786 (538259–663849) | 1568.84 (1402.08–1742.35) | 1059805 (938589–1177798) | 1535.31 (1361.35–1716.51) | 25596 (17847–36935) | 70.29 (50.26–97.95) | 44575 (31164–64303) | 66.2 (46.92–93.48) | |
| Tropical Latin America | 4067963 (3650308–4493560) | 2968.45 (2679.31–3262.59) | 6759436 (6077276–7435843) | 2810.82 (2524.81–3085.81) | 160632 (108646–237288) | 122.13 (84.37–177.31) | 272422 (186998–398263) | 112.22 (77–163.19) | |
| Western Europe | 6730264 (6031222–7394682) | 1600.58 (1437.43–1763.41) | 8083424 (7223640–8953331) | 1564.83 (1401.07–1733.45) | 268013 (185734–388314) | 61.9 (42.03–90.52) | 323694 (226166–466150) | 59.23 (39.76–87.31) | |
| Western Sub-Saharan Africa | 1717211 (1540538–1895977) | 1199.13 (1073.99–1329.43) | 4669907 (4157775–5186404) | 1350.54 (1202.95–1519.49) | 75876 (52404–108277) | 57.78 (41.61–80.8) | 201501 (138395–290933) | 63.29 (44.79–89.46) | |
Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years; SDI, sociodemographic index; GBD, Global Burden of Diseases, Injuries, and Risk Factors Study
Fig. 1.
Global distribution of refraction disorders disease burden in 2021. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
Regional level
In 2021, the ASPR of refraction disorders varied significantly across regions and SDI levels. The highest ASPR was observed in regions with a low-middle SDI, reaching 2,774.05 per 100,000 (95% UI: 2,453.7–3,115.98) (Table 1; Fig. 1A). In contrast, high-SDI regions reported the lowest ASPR at 1,286.91 per 100,000 (95% UI: 1,153.4–1,412.4) (Table 1; Fig. 1A). Geographically, South Asia exhibited the highest ASPR at 3,397.67 per 100,000 (95% UI: 2,991.52–3,859.72), followed by Tropical Latin America at 2,810.82 per 100,000 (95% UI: 2,524.81–3,085.81) (Table 1). On the other hand, High-income North America recorded the lowest ASPR at 1,065.69 per 100,000 (95% UI: 950.02–1,181.34) (Table 1).
The age-standardized DALY rate for refraction disorders was also highest in low-middle SDI regions, at 115.82 per 100,000 (95% UI: 80.26–165.83), and lowest in high-SDI regions, at 48.7 per 100,000 (95% UI: 32.87–71.33) (Table 1; Fig. 1C). Among geographic regions, South Asia had the highest age-standardized DALY rate at 141.73 per 100,000 (95% UI: 98.52–201.42), whereas High-income North America reported the lowest rate at 39.69 per 100,000 (95% UI: 26.6–58.45) (Table 1).
National level
The ASPR of refraction disorders in 2021 varied widely, ranging from approximately 700 to 4,000 per 100,000 individuals. Countries with the highest ASPR included Oman (4,007.19 per 100,000; 95% UI: 3,604.72–4,429.02), India (3,495.7 per 100,000; 95% UI: 3,079.16–3,974.25), Paraguay (3,407.02 per 100,000; 95% UI: 3,100.74–3,724.79), Peru (3,196.68 per 100,000; 95% UI: 2,875.97–3,553.96), and Saudi Arabia (3,015.33 per 100,000; 95% UI: 2,762.64–3,293.38) (Fig. 1A, Supplementary Table S1). Conversely, the lowest ASPR values were observed in Sweden (706.37 per 100,000; 95% UI: 613.59–797.73), Barbados (748.8 per 100,000; 95% UI: 665.92–830.7), Somalia (754.16 per 100,000; 95% UI: 682.41–822.67), Uganda (790.76 per 100,000; 95% UI: 702.69–884.3), and Burundi (805.99 per 100,000; 95% UI: 711.57–897.96) (Fig. 1A, Supplementary Table S1).
Similarly, the age-standardized DALY rates for refraction disorders ranged from 28 to 230 per 100,000 population. The highest rates were recorded in Oman (158.56 per 100,000; 95% UI: 108.57–231.4), India (146.97 per 100,000; 95% UI: 102.34–207.98), Iran (Islamic Republic of) (130.81 per 100,000; 95% UI: 93.78–182.09), Saudi Arabia (125.68 per 100,000; 95% UI: 86.99–178.6), and Peru (124.86 per 100,000; 95% UI: 85.14–180.98) (Fig. 1B, Supplementary Table S1). In contrast, the lowest age-standardized DALY rates were found in Sweden (28.3 per 100,000; 95% UI: 19.14–40.94), Barbados (28.38 per 100,000; 95% UI: 19.09–41.64), Taiwan (Province of China) (35.98 per 100,000; 95% UI: 23.44–54.17), Somalia (36.92 per 100,000; 95% UI: 26.54–50.89), and Burundi (36.96 per 100,000; 95% UI: 26.22–51.79) (Fig. 1B, Supplementary Table S1).
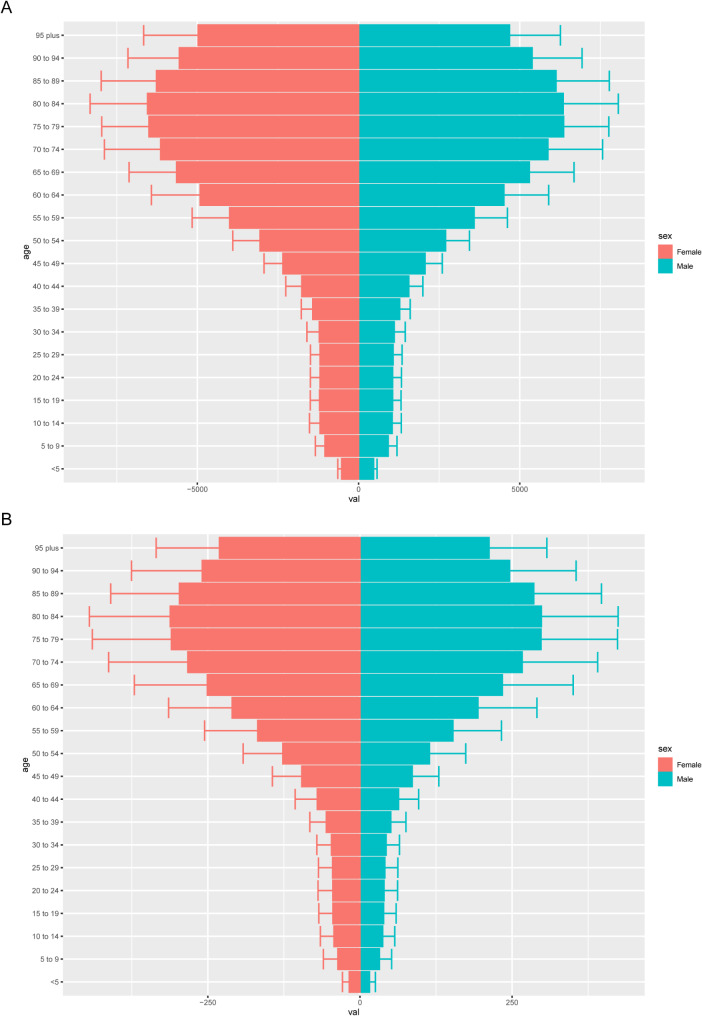
Age and sex patterns
In 2021, the lowest global age-standardized rates (ASRs) for both prevalence and DALYs of refraction disorders were observed in children under the age of 5 (Fig. 2A). Prevalence rates increased steadily with age, peaking at 80–84 years for females and 75–79 years for males, before gradually declining in both sexes (Fig. 2A). Across all age groups, females exhibited higher prevalence rates than males (Fig. 2A). Similarly, DALY rates peaked at 80–84 years for both sexes, with females consistently experiencing higher rates than males across all age groups (Fig. 2B).
Fig. 2.
Age- and sex-structured analysis of refraction disorders disease burden in 2021. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
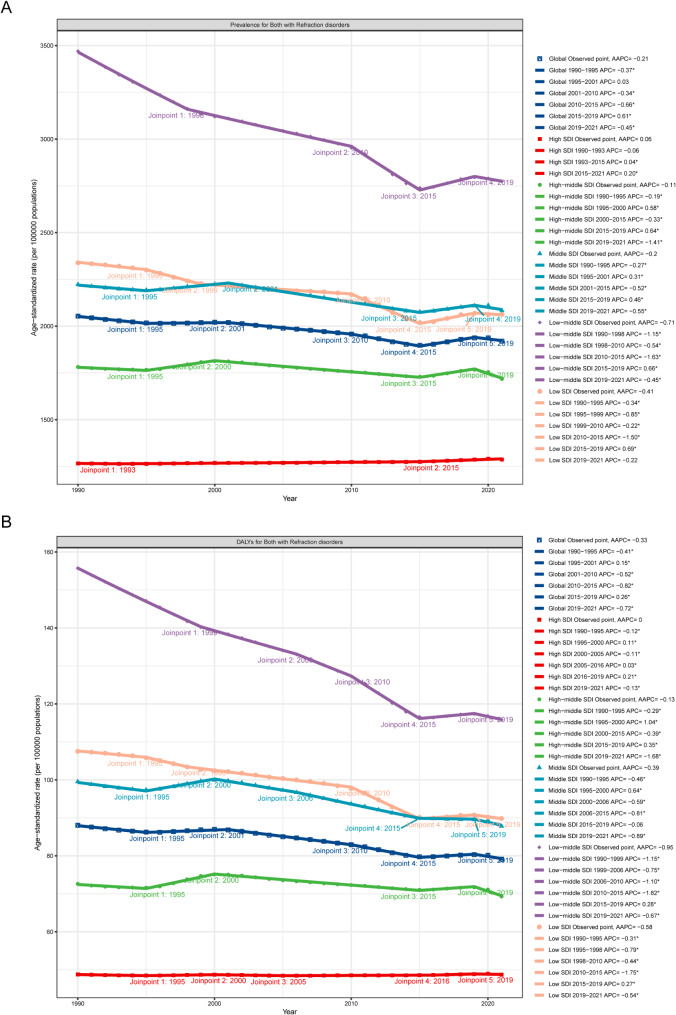
Overall temporal trends in gender and age structures
Between 1990 and 2021, both the prevalence and DALYs numbers showed a general increase across all groups. Throughout this period, females consistently exhibited higher prevalence and DALY numbers and rates compared to males (Fig. 3). Despite the rising numbers, a steady decline was observed in prevalence rates and DALY rates, with an AAPC of -0.21 (95% CI: -0.23–-0.19) and − 0.33 (95% CI: -0.36–-0.31), respectively (Fig. 3; Table 2).
Fig. 3.
Overall temporal trends in gender and age structures of refraction disorders disease burden from 1990 to 2021. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
Table 2.
Joinpoint regression analysis: trends in age-standardized prevalence, incidence, dalys rates (per 100,000 persons) of refraction disorders in global and 5 SDI regions, 1990–2021
| Location | Prevalence | DALYs | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | APC (95% CI) | P value | AAPC (95% CI) | Period | APC (95% CI) | P value | AAPC (95% CI) | ||
| Global | 1990–1995 | -0.37 (-0.4–-0.33) | < 0.001 | -0.21 (-0.23–-0.19) | 1990–1995 | -0.41 (-0.45–-0.36) | < 0.001 | -0.33 (-0.36–-0.31) | |
| 1995–2001 | 0.03 (0–0.07) | 0.079 | 1995–2001 | 0.15 (0.1–0.19) | < 0.001 | ||||
| 2001–2010 | -0.34 (-0.36–-0.32) | < 0.001 | 2001–2010 | -0.52 (-0.54–-0.5) | < 0.001 | ||||
| 2010–2015 | -0.66 (-0.72–-0.61) | < 0.001 | 2010–2015 | -0.82 (-0.88–-0.76) | < 0.001 | ||||
| 2015–2019 | 0.61 (0.52–0.7) | < 0.001 | 2015–2019 | 0.26 (0.17–0.35) | < 0.001 | ||||
| 2019–2021 | -0.45 (-0.62–-0.28) | < 0.001 | 2019–2021 | -0.72 (-0.9–-0.53) | < 0.001 | ||||
| High SDI | 1990–1993 | -0.06 (-0.2–0.08) | 0.398 | 0.06 (0.05–0.08) | 1990–1995 | -0.12 (-0.15–-0.1) | < 0.001 | 0 (-0.01–0.02) | |
| 1993–2015 | 0.04 (0.03–0.05) | < 0.001 | 1995–2000 | 0.11 (0.07–0.14) | < 0.001 | ||||
| 2015–2021 | 0.2 (0.15–0.25) | < 0.001 | 2000–2005 | -0.11 (-0.15–-0.08) | < 0.001 | ||||
| 2005–2016 | 0.03 (0.02–0.04) | < 0.001 | |||||||
| 2016–2019 | 0.21 (0.1–0.32) | 0.001 | |||||||
| 2019–2021 | -0.13 (-0.24–-0.02) | 0.02 | |||||||
| High-middle SDI | 1990–1995 | -0.19 (-0.24–-0.14) | < 0.001 | -0.11 (-0.13–-0.08) | 1990–1995 | -0.29 (-0.39–-0.2) | < 0.001 | -0.13 (-0.18–-0.09) | |
| 1995–2000 | 0.58 (0.51–0.66) | < 0.001 | 1995–2000 | 1.04 (0.9–1.18) | < 0.001 | ||||
| 2000–2015 | -0.33 (-0.34–-0.32) | < 0.001 | 2000–2015 | -0.39 (-0.41–-0.37) | < 0.001 | ||||
| 2015–2019 | 0.64 (0.53–0.75) | < 0.001 | 2015–2019 | 0.35 (0.13–0.57) | 0.003 | ||||
| 2019–2021 | -1.41 (-1.63–-1.18) | < 0.001 | 2019–2021 | -1.68 (-2.1–-1.25) | < 0.001 | ||||
| Middle SDI | 1990–1995 | -0.27 (-0.33–-0.21) | < 0.001 | -0.2 (-0.22–-0.17) | 1990–1995 | -0.46 (-0.51–-0.4) | 0 | -0.39 (-0.42–-0.36) | |
| 1995–2001 | 0.31 (0.25–0.37) | < 0.001 | 1995–2000 | 0.64 (0.56–0.72) | 0 | ||||
| 2001–2015 | -0.52 (-0.54–-0.51) | < 0.001 | 2000–2006 | -0.59 (-0.65–-0.53) | 0 | ||||
| 2015–2019 | 0.46 (0.33–0.59) | < 0.001 | 2006–2015 | -0.81 (-0.84–-0.78) | 0 | ||||
| 2019–2021 | -0.55 (-0.81–-0.28) | < 0.001 | 2015–2019 | -0.06 (-0.19–0.07) | 0.321 | ||||
| 2019–2021 | -0.89 (-1.14–-0.64) | 0 | |||||||
| Low-middle SDI | 1998–2010 | -0.54 (-0.56–-0.52) | < 0.001 | -0.71 (-0.75–-0.68) | 1990–1999 | -1.15 (-1.17–-1.13) | < 0.001 | -0.95 (-0.98–-0.92) | |
| 2010–2015 | -1.63 (-1.72–-1.53) | < 0.001 | 1999–2006 | -0.75 (-0.79–-0.71) | < 0.001 | ||||
| 2015–2019 | 0.66 (0.5–0.81) | < 0.001 | 2006–2010 | -1.1 (-1.22–-0.98) | < 0.001 | ||||
| 2019–2021 | -0.45 (-0.75–-0.15) | 0.006 | 2010–2015 | -1.82 (-1.9–-1.75) | < 0.001 | ||||
| 2015–2019 | 0.28 (0.16–0.4) | < 0.001 | |||||||
| 2019–2021 | -0.67 (-0.91–-0.42) | < 0.001 | |||||||
| Low SDI | 1990–1995 | -0.34 (-0.41–-0.27) | < 0.001 | -0.41 (-0.45–-0.37) | 1990–1995 | -0.31 (-0.38–-0.25) | < 0.001 | -0.58 (-0.62–-0.54) | |
| 1995–1999 | -0.85 (-1.01–-0.69) | < 0.001 | 1995–1998 | -0.79 (-1.08–-0.5) | < 0.001 | ||||
| 1999–2010 | -0.22 (-0.24–-0.19) | < 0.001 | 1998–2010 | -0.44 (-0.46–-0.42) | < 0.001 | ||||
| 2010–2015 | -1.5 (-1.6–-1.4) | < 0.001 | 2010–2015 | -1.75 (-1.84–-1.66) | < 0.001 | ||||
| 2015–2019 | 0.69 (0.53–0.85) | < 0.001 | 2015–2019 | 0.27 (0.12–0.42) | 0.001 | ||||
| 2019–2021 | -0.22 (-0.54–0.09) | 0.155 | 2019–2021 | -0.54 (-0.83–-0.25) | 0.001 | ||||
Abbreviations: SDI, sociodemographic index; DALYs, disability-adjusted life-years; annual percent change, APC; average annual percent change, AAPC
Temporal joinpoint analysis
Joinpoint regression analysis revealed a general downward trend in the global ASPR of refraction disorders from 1990 to 2021 (AAPC = -0.21; 95% CI: -0.23–-0.19; P < 0.001). However, a brief upward trend occurred from 2015 to 2019 (APC = 0.61; 95% CI: 0.52–0.7; P < 0.001) (Fig. 4A; Table 2). The most significant decrease in ASPR was observed between 2010 and 2015 (APC = -0.66; 95% CI: -0.72–-0.61; P < 0.001) (Fig. 4A; Table 2). Similarly, age-standardized DALY rates followed a downward trajectory from 1990 to 2021 (AAPC = -0.33; 95% CI: -0.36–-0.31; P < 0.001), with an increase observed between 2015 and 2018 (APC = 0.26; 95% CI: 0.17–0.35; P < 0.001).
Fig. 4.
Joinpoint regression analysis of the refraction disorders disease burden temporal trends, 1990–2021. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
An analysis of the five SDI regions showed a general downward trend in both ASPR and age-standardized DALY rates from 1990 to 2021 for the high-middle SDI, middle SDI, low-middle SDI, and low SDI regions (Fig. 4; Table 2). The low-middle SDI region experienced the most notable decline in both ASPR (AAPC = -0.71; 95% CI: -0.75–-0.68; P < 0.001) and age-standardized DALYs (AAPC = -0.95; 95% CI: -0.98–-0.92; P < 0.001). In contrast, the high SDI region showed a slight increase in ASPR (AAPC = 0.06; 95% CI: 0.05–0.08; P < 0.001), and the age-standardized DALY rates remained largely unchanged (AAPC = 0; 95% CI: -0.01–0.02; P < 0.001) from 1990 to 2021.
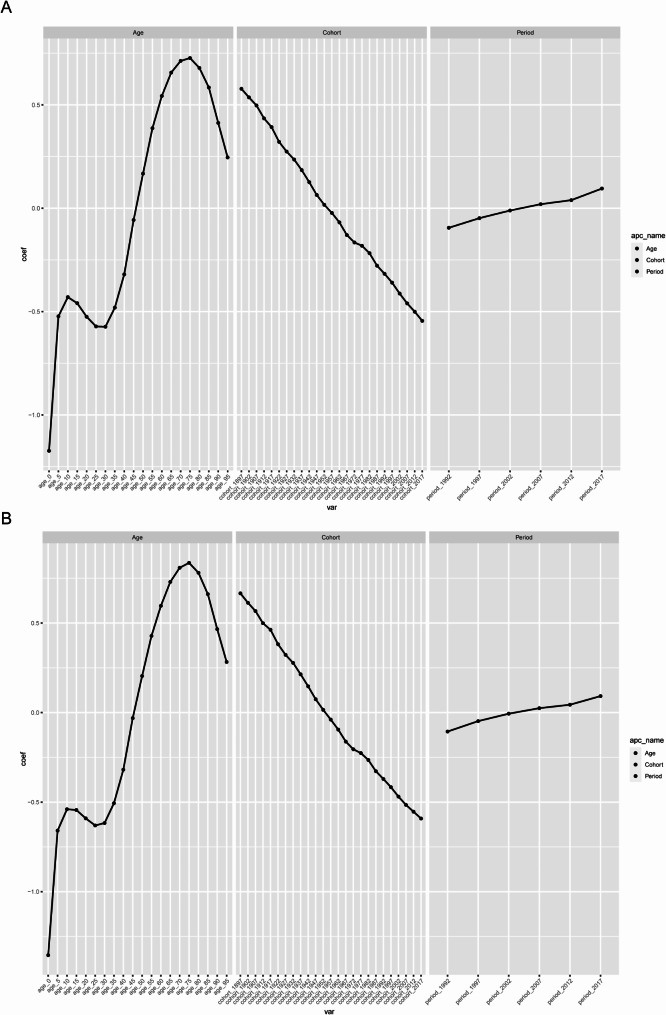
Age-period-cohort analysis
After adjusting for period and birth cohort effects, the age effect was found to significantly influence the risk of both refraction disorders prevalence and DALYs. The relative prevalence risk increased initially before 10–15 years, then declined up to 30–35 years, before rising again to the highest risk at ages 75–80, followed by a gradual decrease (Fig. 5A; Table 3). Similarly, the relative DALYs risk followed a similar pattern, rising before 10–15 years, falling up to 25–30 years, and then increasing again to the highest risk at ages 75–80, with a gradual decline thereafter (Fig. 5B; Table 3).
Fig. 5.
The effects of age, period, and birth cohort on the relative risk of refraction disorders. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
Table 3.
RRs of refraction disorders prevalence and dalys for both sexes due to age, period, and birth cohort effects
| Factor | Prevalence | DALYs | |||
|---|---|---|---|---|---|
| RR (95% CI) | P | RR (95% CI) | P | ||
| Age (years) | |||||
| 0–4 | 0.309 (0.309–0.309) | < 0.001 | 0.258 (0.257–0.259) | < 0.001 | |
| 5–9 | 0.593 (0.592–0.593) | < 0.001 | 0.517 (0.516–0.519) | < 0.001 | |
| 10–14 | 0.65 (0.65–0.651) | < 0.001 | 0.583 (0.581–0.584) | < 0.001 | |
| 15–19 | 0.632 (0.631–0.632) | < 0.001 | 0.58 (0.579–0.582) | < 0.001 | |
| 20–24 | 0.592 (0.591–0.592) | < 0.001 | 0.554 (0.553–0.555) | < 0.001 | |
| 25–29 | 0.564 (0.564–0.565) | < 0.001 | 0.532 (0.531–0.534) | < 0.001 | |
| 30–34 | 0.564 (0.563–0.564) | < 0.001 | 0.54 (0.539–0.541) | < 0.001 | |
| 35–39 | 0.618 (0.618–0.619) | < 0.001 | 0.603 (0.602–0.604) | < 0.001 | |
| 40–44 | 0.726 (0.726–0.726) | < 0.001 | 0.727 (0.726–0.728) | < 0.001 | |
| 45–49 | 0.945 (0.944–0.945) | < 0.001 | 0.969 (0.968–0.971) | < 0.001 | |
| 50–54 | 1.182 (1.182–1.183) | < 0.001 | 1.226 (1.224–1.228) | < 0.001 | |
| 55–59 | 1.473 (1.472–1.473) | < 0.001 | 1.534 (1.532–1.537) | < 0.001 | |
| 60–64 | 1.721 (1.721–1.722) | < 0.001 | 1.815 (1.811–1.818) | < 0.001 | |
| 65–69 | 1.928 (1.927–1.928) | < 0.001 | 2.074 (2.07–2.078) | < 0.001 | |
| 70–74 | 2.039 (2.038–2.04) | < 0.001 | 2.244 (2.24–2.249) | < 0.001 | |
| 75–79 | 2.068 (2.067–2.069) | < 0.001 | 2.307 (2.302–2.313) | < 0.001 | |
| 80–84 | 1.971 (1.97–1.972) | < 0.001 | 2.183 (2.177–2.189) | < 0.001 | |
| 85–89 | 1.794 (1.792–1.795) | < 0.001 | 1.937 (1.931–1.944) | < 0.001 | |
| 90–94 | 1.511 (1.509–1.513) | < 0.001 | 1.593 (1.585–1.601) | < 0.001 | |
| 95–99 | 1.279 (1.276–1.281) | < 0.001 | 1.326 (1.314–1.339) | < 0.001 | |
| Period | |||||
| 1992–1996 | 0.91 (0.909–0.91) | < 0.001 | 0.899 (0.898–0.9) | < 0.001 | |
| 1997–2001 | 0.953 (0.953–0.953) | < 0.001 | 0.953 (0.952–0.954) | < 0.001 | |
| 2002–2006 | 0.989 (0.989–0.989) | < 0.001 | 0.994 (0.993–0.995) | < 0.001 | |
| 2007–2011 | 1.02 (1.02–1.02) | < 0.001 | 1.025 (1.024–1.026) | < 0.001 | |
| 2012–2016 | 1.04 (1.04–1.04) | < 0.001 | 1.045 (1.044–1.046) | < 0.001 | |
| 2017–2021 | 1.1 (1.1–1.1) | < 0.001 | 1.096 (1.095–1.097) | < 0.001 | |
| Birth cohort | |||||
| 1897–1901 | 1.782 (1.769–1.795) | < 0.001 | 1.946 (1.883–2.01) | < 0.001 | |
| 1902–1906 | 1.71 (1.705–1.715) | < 0.001 | 1.846 (1.821–1.871) | < 0.001 | |
| 1907–1911 | 1.644 (1.641–1.647) | < 0.001 | 1.763 (1.749–1.776) | < 0.001 | |
| 1912–1916 | 1.544 (1.543–1.546) | < 0.001 | 1.646 (1.637–1.656) | < 0.001 | |
| 1917–1921 | 1.481 (1.479–1.482) | < 0.001 | 1.588 (1.58–1.595) | < 0.001 | |
| 1922–1926 | 1.378 (1.377–1.38) | < 0.001 | 1.464 (1.458–1.471) | < 0.001 | |
| 1927–1931 | 1.315 (1.314–1.316) | < 0.001 | 1.38 (1.375–1.385) | < 0.001 | |
| 1932–1936 | 1.266 (1.265–1.267) | < 0.001 | 1.32 (1.315–1.324) | < 0.001 | |
| 1937–1941 | 1.203 (1.202–1.203) | < 0.001 | 1.238 (1.234–1.242) | < 0.001 | |
| 1942–1946 | 1.134 (1.134–1.135) | < 0.001 | 1.158 (1.154–1.161) | < 0.001 | |
| 1947–1951 | 1.066 (1.065–1.067) | < 0.001 | 1.077 (1.074–1.08) | < 0.001 | |
| 1952–1956 | 1.017 (1.016–1.017) | < 0.001 | 1.015 (1.013–1.018) | < 0.001 | |
| 1957–1961 | 0.978 (0.977–0.978) | < 0.001 | 0.962 (0.959–0.964) | < 0.001 | |
| 1962–1966 | 0.934 (0.933–0.934) | < 0.001 | 0.909 (0.907–0.911) | < 0.001 | |
| 1967–1971 | 0.878 (0.878–0.878) | < 0.001 | 0.85 (0.849–0.852) | < 0.001 | |
| 1972–1976 | 0.847 (0.847–0.848) | < 0.001 | 0.815 (0.813–0.816) | < 0.001 | |
| 1977–1981 | 0.834 (0.834–0.834) | < 0.001 | 0.798 (0.796–0.799) | < 0.001 | |
| 1982–1986 | 0.804 (0.804–0.805) | < 0.001 | 0.767 (0.766–0.769) | < 0.001 | |
| 1987–1991 | 0.757 (0.757–0.757) | < 0.001 | 0.721 (0.719–0.722) | < 0.001 | |
| 1992–1996 | 0.728 (0.728–0.728) | < 0.001 | 0.69 (0.689–0.691) | < 0.001 | |
| 1997–2001 | 0.698 (0.697–0.698) | < 0.001 | 0.659 (0.658–0.661) | < 0.001 | |
| 2002–2006 | 0.662 (0.661–0.662) | < 0.001 | 0.625 (0.624–0.627) | < 0.001 | |
| 2007–2011 | 0.631 (0.631–0.631) | < 0.001 | 0.597 (0.595–0.599) | < 0.001 | |
| 2012–2016 | 0.606 (0.606–0.607) | < 0.001 | 0.575 (0.573–0.577) | < 0.001 | |
| 2017–2021 | 0.58 (0.579–0.581) | < 0.001 | 0.553 (0.55–0.557) | < 0.001 |
Abbreviations: DALYs, disability-adjusted life-years; RR, relative risk; CI, confidence interval
After controlling for age and period effects, the birth cohort effect showed a significant influence on the risk of both refraction disorders prevalence and DALYs. The analysis indicated higher risks in earlier birth cohorts compared to later ones, with the relative risk (RR) steadily decreasing from the 1897–1901 cohort to the 2017–2021 cohort (Fig. 5; Table 3).
When adjusting for age and birth cohort effects, the period effect also significantly impacted the risk of refraction disorders prevalence and DALYs. The period effect demonstrated an increasing trend, with a 1.21 and 1.22 times increase in RR for prevalence and DALYs risk, respectively, from the period 1992 to 2017. The highest risks for both incidence and prevalence were observed in the period 2017 (Fig. 5; Table 3).
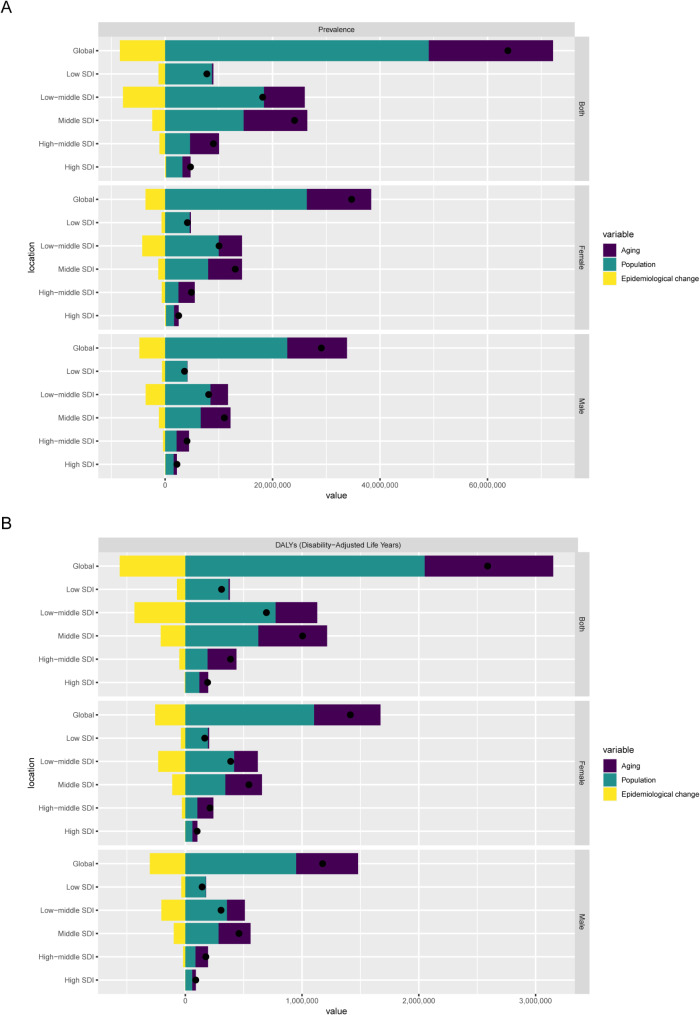
Decomposition analysis
Population growth and aging were the main drivers behind the global decrease in ASR of prevalence and DALYs (Fig. 6, Supplementary Table S2). Aging, population growth, and epidemiological changes contributed 36.25%, 76.92%, and − 13.18% to the global decrease in ASPR, respectively (Fig. 6A, Supplementary Table S2). Notably, the highest contributions from aging, population growth, and epidemiological changes were seen in the high-middle SDI region (60.05%), low SDI region (112.09%), and low-middle SDI region (-43.13%) (Supplementary Table S2). Similarly, these factors accounted for 42.51%, 79.17%, and − 21.68% of the global increase in age-standardized DALY rates, respectively (Fig. 6B, Supplementary Table S2). The most significant contributions were observed in the high-middle SDI region (63.99%), low SDI region (118.93%), and low-middle SDI region (-62.59%) (Supplementary Table S2). Notably, epidemiological changes had a negative impact on the decrease in ASPR, except in the high SDI region, and similarly, they negatively affected DALY decreases globally and across the five SDI regions.
Fig. 6.
Decomposition Analysis of refraction disorders disease burden in 2021. (A) The ASR of prevalence; (B) The ASR of DALYs. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
Cross-country inequality analysis
An analysis of age-standardized DALY rates across 204 countries revealed trends in SDI-associated inequalities in the burden of refraction disorders. According to the slope index of inequality, the DALYs per 100,000 population between countries with the highest and lowest SDI was − 20.42 (95% CI: −30.70–−10.14) in 1990, decreasing to − 17.65 (95% CI: −25.69–−9.60) in 2021, indicating a decline in absolute SDI-associated inequalities (Fig. 7A). The concentration curve lay above the diagonal line, signifying that the burden was disproportionately concentrated in countries with lower socioeconomic development levels (Fig. 7B). The concentration index, a measure of relative gradient inequality, was − 0.17 (95% CI: −0.21–−0.13) in 1990 and declined to − 0.10 (95% CI: −0.13–−0.07) in 2021, further confirming a reduction in relative SDI-associated inequalities (Fig. 7B).
Fig. 7.
Cross-country inequality analysis of refraction disorders in 1990 and 2021. (A) SDI-related health inequality regression; (B) concentration curves for the DALYs of refraction disorders worldwide. Abbreviations: SDI, sociodemographic index; DALYs, disability-adjusted life-years
Predictive analysis of refraction disorders burden to 2050
Predictive analysis results for refraction disorders indicated that by 2050, case numbers for prevalence and DALYs were projected to rise to 222768558.2 (95% UI: 67412657.71–378124458.8) and 8684314.99 (95% UI: 2768725.2–14599904.78) (Fig. 8, Table S3). However, the ASR for prevalence and DALYs were expected to decline to 1815.27 (95% UI: 534.15–3096.40) and 69.11 (95% UI: 21.45–116.77) (Fig. 8, Table S3).
Fig. 8.
Predictive Analysis of refraction disorders Burden to 2050. (A) The predicted case number and ASR of prevalence to 2050; (B) The predicted case number and ASR of DALYs to 2050. Abbreviations: ASR, age-standardized rate; DALYs, disability-adjusted life-years
Discussion
This study presents updated data on the global, regional, and national prevalence and DALYs associated with refraction disorders from 1990 to 2021. It includes a comprehensive analysis through trend evaluation, decomposition, inequality assessment, and predictive modeling. Despite variations in prevalence and DALYs across countries, the global burden has generally declined over this period, with females being more affected than males. Decomposition analysis highlights population growth and aging as primary contributors to the burden. Inequality analysis shows that low-SDI countries have shouldered a disproportionate share of the burden, although these disparities have diminished over time. The ASR for both prevalence and DALYs are projected to experience a slight annual decline from 2022 to 2050.
Focusing on the prevention of refraction disorders has significantly reduced their health burden [6]. In 2021, refraction disorders accounted for 159.8 million prevalent cases and 6.6 million DALYs globally, with the highest burden observed in low-middle SDI regions and the lowest in high-SDI regions. Notably, the low-middle SDI region experienced the most significant decline in both ASPRs and age-standardized DALYs. Tang et al. reported that in 2017, lower middle-income countries bore the highest burden of refraction disorders and saw the greatest decline in age-standardized DALY rates, whereas high-income countries had the lowest age-standardized DALY rates [11]. Their study classified countries by World Bank income levels, while our study used SDI classifications, but the findings were consistent. Li et al. also found that the low-middle SDI region had higher ASRs of both DALY and prevalence in 2019, potentially due to better access to eye care services in developed countries [6]. Surprisingly, although high-SDI regions had the lowest burden overall, only these regions exhibited a slight increase in ASPR from 1990 to 2021. This suggests that high-SDI areas should not become complacent and should actively implement policies to prevent refractive errors and curb the rising ASPR.
At the national level, disparities in the burden and trends of refraction disorders suggest the need for adaptable health policies tailored to specific country conditions. In 2021, Oman recorded the highest ASR for prevalence and DALYs of refraction disorders. Recent improvements in health and living standards in Oman have led to a reduction in environment-related and infectious diseases. The country is now undergoing an epidemiological transition characterized by a baby boom, youth bulge, and increasing longevity, with chronic non-communicable diseases becoming unexpectedly common [30]. Khandekar et al. observed that myopia rates among Omani schoolchildren increased with grade, with younger students more frequently affected. Female students had a significantly higher risk of myopia compared to males [31]. Vankudre et al. found that most participants at the University of Oman had inappropriate vision correction with spectacles and had not undergone prior ocular examinations. Few wore spectacles, and those who did often had inappropriate prescriptions. Reasons for not wearing spectacles included ordering new ones or losing/breaking existing pairs [32]. As the burden of refraction disorders continues to rise in Oman, it is crucial to develop preventive strategies, improve management approaches, and implement more evidence-based treatments.
To better understand the relationship between age and refraction disorders, the population was divided into 5-year age groups to account for the impact of aging. Females were found to be more vulnerable to health burdens and vision loss due to refraction disorders than males, with gender inequality influenced by age and socioeconomic levels [6]. Li et al. also noted that global DALY numbers and crude DALY rates of refraction disorders were significantly higher in females than in males of the same age [6]. Pan et al. examined gender disparities in the global burden of refractive disorders in children under 15 by year, age, and national development status, finding that girls had a higher burden than boys of the same age, with disparities increasing with age [23]. Our study similarly found that females consistently exhibited higher prevalence and DALY numbers and rates compared to males from 1990 to 2021, with this trend persisting across all age groups in 2021. The higher burden of refractive disorders in females may be attributed to physiological, social, educational, cultural, and economic differences between the sexes [23].
Examining the effects of age, period, and birth cohort on refraction disorders enhances our understanding of the disease’s epidemiology. By 2050, over 700 million people are projected to experience moderate and severe vision impairment (MSVI) or blindness, primarily due to the growing and aging global population [33]. Refraction disorders are the leading cause of MSVI and the second leading cause of blindness after cataracts. The relative risk of prevalence increases with age, peaking in the 75–79 years age group, indicating the need for focused eye care in this demographic. Regarding birth cohort effects, a declining trend in relative risks for prevalence and DALYs was observed with each successive cohort, suggesting that earlier-born individuals have a higher risk of refraction disorders than later-born individuals. This may be linked to improvements in living conditions, education, and health services over time. In terms of period effects, the relative risks for prevalence and DALYs have slightly increased, likely due to the rising use of electronic devices like smartphones and tablets, especially among children and adolescents, which has heightened near-eye activity and possibly exacerbated refractive errors [34]. Additionally, modern lifestyles have reduced outdoor time, which has been shown to protect against myopia [35]. The decomposition analysis indicated that the overall reduction in the burden of refractive disorders is primarily attributable to population growth. This finding suggests that current strategies for preventing refractive disorders are effective, as the prevalence has not increased in proportion to the growing population.
The cross-country inequality analysis revealed that a disproportionate burden of refraction disorders is concentrated in low SDI countries, aligning with previous studies indicating that nations with lower sociodemographic development bear a greater share of this burden [6, 11]. The average number of eye doctors per million population increases with a country’s income, and people in developed countries have easier access to eye care services [36]. Major barriers to correcting refraction disorders in lower-income countries include the availability and affordability of eye care services, such as a shortage of ophthalmologists and the cost of spectacles or refractive surgery [37]. Additional factors include parental unawareness of vision problems, attitudes towards the necessity of spectacles, high costs, and concerns that wearing spectacles may worsen refractive errors [38]. Efforts such as providing free spectacles and vision screening have been implemented to improve eye care services, especially in low and middle SDI countries [39–43].
This study has several limitations. Firstly, the GBD database primarily aggregates data from national and regional reports and publications rather than direct country reports, resulting in considerable variability in data collection methods across different countries. This variability may lead to significant heterogeneity in the findings. Secondly, the accuracy of refraction disorder diagnoses and the level of medical expertise differ among the 204 countries and regions included in the study. In some low- and middle-income countries, the lack of reliable epidemiological data and the underreporting of refraction disorder cases could result in an underestimation of the true disease burden. Lastly, although GBD collaborators employ data cleaning, correction, and advanced statistical modeling techniques to address these limitations, the findings still rely heavily on assumptions and modeling, which may introduce some uncertainty into the estimates.
In conclusion, the global burden of refraction disorders decreased steadily from 1990 to 2021, and was expected to decline by 2050. The burden on females was greater compared to males. Population growth was the main driver behind the global changes in ASR of prevalence and DALYs. Countries with low SDI have borne a disproportionately high burden, and SDI-related inequalities have lessen over time. However, although high-SDI regions had the lowest burden overall, only these regions exhibited a slight increase in ASPR from 1990 to 2021. This suggests that high-SDI areas should not become complacent and should actively implement policies to prevent refractive errors and curb the rising ASPR.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our heartfelt gratitude to the contributors of the Global Burden of Diseases, Injuries, and Risk Factors Study 2021 for their invaluable efforts. We also sincerely thank the Institute for Health Metrics and Evaluation (IHME) for providing access to the GBD data used in this research.
Abbreviations
- URE
Uncorrected refractive error
- VI
Vision impairment
- GBD
Global Burden of Disease
- UI
Uncertainty interval
- DALY
Disability-adjusted life year
- YLD
Years lived with disability
- SDI
Sociodemographic index
- APC
Annual percent change
- CI
Confidence interval
- AAPC
Average annual percent change
- ASPR
Age-standardized prevalence rate
- EAPC
Estimated annual percentage change
- MSVI
Moderate and severe vision impairment
- RR
Relative risk
- ASR
Age-standardized rate
- BAPC
Bayesian age-period-cohort
- INLA
Integrated nested Laplace approximation
Author contributions
OY contributed to conceptualization, data curation, formal analysis, investigation, methodology, software, resources, validation, visualization and writing–review & editing. DM contributed to funding acquisition, project administration, supervision, writing–original draft and writing–review & editing.
Funding
The study of this paper is supported by Self-financed Science and Technology Innovation Projects of Foshan City (2220001005468). The sponsor or funding organization had no role in the design or conduct of this research.
Data availability
The data resources from the GBD study 2021 can be accessed online through the Global Health Data Exchange (GHDx) query tool at https://ghdx.healthdata.org/gbd-results-tool.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harb EN, Wildsoet CF. Origins of refractive errors: environmental and genetic factors. Annual Rev Vis Sci. 2019;5:47–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naidoo KS, Leasher J, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, Limburg H, Pesudovs K, Price H, White RA, et al. Global vision impairment and blindness due to uncorrected refractive error, 1990–2010. Optom Vis Sci. 2016;93(3):227–34. [DOI] [PubMed] [Google Scholar]
- 3.Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol. 2012;60(5):432–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varma R, Vajaranant TS, Burkemper B, Wu S, Torres M, Hsu C, Choudhury F, McKean-Cowdin R. Visual impairment and blindness in adults in the united States: demographic and geographic variations from 2015 to 2050. JAMA Ophthalmol. 2016;134(7):802–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zebardast N, Friedman DS, Vitale S. The prevalence and demographic associations of presenting Near-Vision impairment among adults living in the united States. Am J Ophthalmol. 2017;174:134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li HY, Liu YM, Dong L, Zhang RH, Zhou WD, Wu HT, Li YF, Wang YX, Wei WB. Global, regional, and National prevalence, disability adjusted life years, and time trends for refraction disorders, 1990–2019: findings from the global burden of disease study 2019. BMC Public Health. 2021;21(1):1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith TS, Frick KD, Holden BA, Fricke TR, Naidoo KS. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ. 2009;87(6):431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, Matsui KO, Wu PC, Sankaridurg P, Chia A et al. Myopia. Nat Rev Dis Primers 2020, 6(1):99. [DOI] [PubMed]
- 9.Kandel H, Khadka J, Goggin M, Pesudovs K. Patient-reported outcomes for assessment of quality of life in refractive error: A systematic review. Optom Vis Sci. 2017;94(12):1102–19. [DOI] [PubMed] [Google Scholar]
- 10.Bourne RRA, Cicinelli MV, Sedighi T, Tapply IH, McCormick I, Jonas JB, Congdon NG, Ramke J, Naidoo KS, Fricke TR, et al. Effective refractive error coverage in adults aged 50 years and older: estimates from population-based surveys in 61 countries. Lancet Glob Health. 2022;10(12):e1754–63. [DOI] [PubMed] [Google Scholar]
- 11.Tang X, Lou L, Xu Y, Jin K, Cao J, Shao J, Gao Z, Yao K. Socioeconomic inequality in the global burden of refraction disorders: results from the global burden of diseases study 2017. Acta Ophthalmol. 2020;98(7):e864–9. [DOI] [PubMed] [Google Scholar]
- 12.Jeganathan VSE, Robin AL, Woodward MA. Refractive error in underserved adults: causes and potential solutions. Curr Opin Ophthalmol. 2017;28(4):299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tafida A, Kyari F, Abdull MM, Sivasubramaniam S, Murthy GVS, Kana I, Gilbert CE. Nigeria National survey of B, visual impairment study G: poverty and blindness in Nigeria: results from the National survey of blindness and visual impairment. Ophthalmic Epidemiol. 2015;22(5):333–41. [DOI] [PubMed] [Google Scholar]
- 14.He Y, Jiang W, Wang W. Global burden of osteoarthritis in adults aged 30 to 44 years, 1990 to 2019: results from the global burden of disease study 2019. BMC Musculoskelet Disord. 2024;25(1):303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li XY, Kong XM, Yang CH, Cheng ZF, Lv JJ, Guo H, Liu XH. Global, regional, and national burden of ischemic stroke, 1990–2021: an analysis of data from the global burden of disease study 2021. EClinicalMedicine 2024, 75:102758. [DOI] [PMC free article] [PubMed]
- 16.Tuo Y, Li Y, Li Y, Ma J, Yang X, Wu S, Jin J, He Z. Global, regional, and national burden of thalassemia, 1990–2021: a systematic analysis for the global burden of disease study 2021. EClinicalMedicine 2024, 72:102619. [DOI] [PMC free article] [PubMed]
- 17.Ferrari AJ, Santomauro DF, Aali A, Abate YH, Abbafati C, Abbastabar H, Abd ElHafeez S, Abdelmasseh M, Abd-Elsalam S, Abdollahi Aet al: Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021:a systematic analysis for the Global Burden of Disease Study 2021. The Lancet 2024, 403(10440):2133–2161. [DOI] [PMC free article] [PubMed]
- 18.Liu W, Yang C, Chen Z, Lei F, Qin JJ, Liu H, Ji YX, Zhang P, Cai J, Liu YM, et al. Global death burden and attributable risk factors of peripheral artery disease by age, sex, SDI regions, and countries from 1990 to 2030: results from the global burden of disease study 2019. Atherosclerosis. 2022;347:17–27. [DOI] [PubMed] [Google Scholar]
- 19.Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prevention: Publication Am Association Cancer Res Cosponsored Am Soc Prev Oncol. 2014;23(11):2296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bell A. Age period cohort analysis: a review of what we should and shouldn’t do. Ann Hum Biol. 2020;47(2):208–17. [DOI] [PubMed] [Google Scholar]
- 21.Rosenberg PS, Anderson WF. Age-period-cohort models in cancer surveillance research: ready for prime time? Cancer epidemiology, biomarkers & prevention: a publication of the American association for cancer research. Cosponsored Am Soc Prev Oncol. 2011;20(7):1263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shan T, Zhu Y, Fan H, Liu Z, Xie J, Li M, Jing S. Global, regional, and National time trends in the burden of epilepsy, 1990–2019: an age-period-cohort analysis for the global burden of disease 2019 study. Front Neurol. 2024;15:1418926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan W, Lou L, Chen F, Tang X. Gender disparities in the global burden of refractive disorders in children: an analysis from the global burden of disease study 2019. J Pediatr Ophthalmol Strabismus. 2024;61(1):51–8. [DOI] [PubMed] [Google Scholar]
- 24.Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, Maddukuri G, Tsai CY, Floyd T, Al-Aly Z. Analysis of the global burden of disease study highlights the global, regional, and National trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94(3):567–81. [DOI] [PubMed] [Google Scholar]
- 25.Ordunez P, Martinez R, Soliz P, Giraldo G, Mujica OJ, Nordet P. Rheumatic heart disease burden, trends, and inequalities in the Americas, 1990–2017: a population-based study. Lancet Global Health. 2019;7(10):e1388–97. [DOI] [PubMed] [Google Scholar]
- 26.Shu Y, Wu Z, Yang X, Song M, Ye Y, Zhang C, Yuan Q, Wang L. The burden of epilepsy in the People’s Republic of China from 1990 to 2019: epidemiological trends and comparison with the global burden of epilepsy. Front Neurol. 2023;14:1303531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cao F, He YS, Wang Y, Zha CK, Lu JM, Tao LM, Jiang ZX, Pan HF. Global burden and cross-country inequalities in autoimmune diseases from 1990 to 2019. Autoimmun Rev. 2023;22(6):103326. [DOI] [PubMed] [Google Scholar]
- 28.Cao F, Xu Z, Li XX, Fu ZY, Han RY, Zhang JL, Wang P, Hou S, Pan HF. Trends and cross-country inequalities in the global burden of osteoarthritis, 1990–2019: A population-based study. Ageing Res Rev. 2024;99:102382. [DOI] [PubMed] [Google Scholar]
- 29.Hu W, Fang L, Zhang H, Ni R, Pan G. Global disease burden of COPD from 1990 to 2019 and prediction of future disease burden trend in China. Public Health. 2022;208:89–97. [DOI] [PubMed] [Google Scholar]
- 30.Al-Sinawi H, Al-Alawi M, Al-Lawati R, Al-Harrasi A, Al-Shafaee M, Al-Adawi S. Emerging burden of frail young and elderly persons in Oman: for whom the bell tolls? Sultan Qaboos Univ Med J. 2012;12(2):169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khandekar R, Gogri U, Al-Harby S. Changing trends in myopia among schoolchildren in Oman: screening information over 11 years. Oman J Ophthalmol. 2018;11(3):232–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vankudre GS, Noushad B. Barriers and perception towards spectacle wear among a student population of university of Buraimi, Oman. Sultan Qaboos Univ Med J. 2021;21(3):416–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ung L, Jonas JB, Lietman TM, Chodosh J. COVID-19 and the unfinished agenda of VISION 2020. Am J Ophthalmol. 2021;224:30–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hansen MH, Laigaard PP, Olsen EM, Skovgaard AM, Larsen M, Kessel L, Munch IC. Low physical activity and higher use of screen devices are associated with myopia at the age of 16–17 years in the CCC2000 eye study. Acta Ophthalmol. 2020;98(3):315–21. [DOI] [PubMed] [Google Scholar]
- 35.Lee SS, Mackey DA. Prevalence and risk factors of myopia in young adults: review of findings from the raine study. Front Public Health. 2022;10:861044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Resnikoff S, Lansingh VC, Washburn L, Felch W, Gauthier TM, Taylor HR, Eckert K, Parke D, Wiedemann P. Estimated number of ophthalmologists worldwide (International Council of ophthalmology update): will we Meet the needs? Br J Ophthalmol. 2020;104(4):588–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lou L, Yao C, Jin Y, Perez V, Ye J. Global patterns in health burden of uncorrected refractive error. Investig Ophthalmol Vis Sci. 2016;57(14):6271–7. [DOI] [PubMed] [Google Scholar]
- 38.Salomao SR, Cinoto RW, Berezovsky A, Mendieta L, Nakanami CR, Lipener C, Munoz Ede H, Ejzenbaum F, Belfort R Jr., Pokharel GP, et al. Prevalence and causes of visual impairment in low-middle income school children in Sao Paulo, Brazil. Investig Ophthalmol Vis Sci. 2008;49(10):4308–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta V, Saxena R, Vashist P, Bhardwaj A, Pandey RM, Tandon R, Menon V. Spectacle coverage among urban schoolchildren with refractive error provided subsidized spectacles in North India. Optom Vis Sci. 2019;96(4):301–8. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Y, Guan H, Du K, Zhao J, Shi Y, Wang H, Wang D. Effects of vision health education and free eyeglasses on knowledge of vision and usage of spectacles among primary school students: evidence from Gansu and Shaanxi provinces in China. Risk Manage Healthc Policy. 2021;14:1449–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pawar N, Ravindran M, Renagappa R, Ravilla T, Raman R, Uduman MS. Non-compliance for wearing spectacles: prevalence and determinants in school-going children in South India. Indian J Ophthalmol. 2023;71(2):608–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Metsing TI, Jacobs WE, Hansraj R. Vision screening as part of the school health policy in South Africa from the perspective of school health nurses. Afr J Prim Health Care Family Med. 2022;14(1):e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eksteen S, Eikelboom RH, Kuper H, Launer S, Swanepoel W. Prevalence and characteristics of hearing and vision loss in preschool children from low income South African communities: results of a screening program of 10,390 children. BMC Pediatr. 2022;22(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data resources from the GBD study 2021 can be accessed online through the Global Health Data Exchange (GHDx) query tool at https://ghdx.healthdata.org/gbd-results-tool.