Abstract
Background
Individuals with severe mental illnesses (SMIs) are at an increased risk of exhibiting violent behaviors, which may result in significant negative consequences, including damaged relationships, property destruction, and harm to themselves or others. The purpose is to investigate the current status of violent behaviors among individuals with SMIs and identify factors within the demographic information, psychological status, and treatment status of individuals with SMIs that may influence the occurrence of violent behaviors.
Methods
We conducted a cross-sectional survey of 1108 individuals with SMIs. The Logistic regression and Chi-squared Automatic Interaction Detection (CHAID) tree model were employed to analyze the influencing factors of violent behaviors in individuals with SMIs and compare their predictive performance.
Results
49.6% of the participants engaged in violent behaviors in the past 12 months. The study identified that factors influencing violent behavior in individuals with SMIs include medication adherence, self-reported health status, employment, household income, experience of discrimination, disease concealment, access to medical assistance, and comorbidities. Medication adherence was identified as the most critical factor affecting violent behavior in individuals with SMIs. Logistic regression model and CHAID tree model had comparable predictive accuracy with AUC values of 0.734 and 0.730, respectively. No statistically significant difference was observed in the predictive performance of the two models (Z = -0.745, P = 0.456).
Conclusions
Individuals with SMIs are at a higher risk of violent behavior, which is influenced by multiple factors, particularly medication adherence. This adherence may be a key determinant in the occurrence of violent behavior among individuals with SMIs. Healthcare professionals should implement targeted interventions addressing these influencing factors to prevent the manifestation of violent behavior in individuals with SMIs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-025-06714-6.
Keywords: Severe mental illnesses, Violent behaviors, Risk prevention, Medication adherence
Introduction
Individuals with severe mental illnesses (SMIs) face numerous challenges in their daily lives, including violence, stigma, and the burden of treatment [1]. These problems not only reduce the quality of life of patients, but also place a significant burden on society and the economy [2]. According to statistics, mental illnesses caused nearly 5 trillion USD in economic losses in 2019, accounting for 16% of the global disease burden [3]. Individuals with SMIs have a life expectancy that is 10–20 years shorter than that of the general population [4], and often experience prolonged illness duration, frequent relapses, and significant disability [5, 6]. In China, SMIs include six diagnoses: schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, psychotic disorder due to epilepsy, and mental retardation-associated mental disorder [7]. As of the end of 2020, there were an estimated 6.43 million registered cases of SMIs in China, with a reported prevalence of 0.46% [8]. The global prevalence rates of schizophrenia and bipolar disorder are approximately 0.3% and 0.5%, respectively [9]. Although the reported prevalence of SMIs in China is relatively lower, the overall burden of mental illness remains significant and is currently estimated to be about one-sixth of the total global burden of disease [10].
Individuals with SMIs frequently exhibit impaired behavioral control during disease onset, leading to impulsive, injurious, suicidal, and other harmful behaviors that pose serious threats to public safety [11, 12]. The relationship between SMIs and violent behaviors has received extensive attention from researchers for decades. Several international studies have consistently demonstrated that individuals with SMIs have a higher incidence of violent behaviors and are also more likely to be victims of violence than the general population [13, 14]. The complexity of this phenomenon requires early and accurate identification of factors that influence violent behaviors in individuals with SMIs to ensure patient and public safety [15]. Existing research emphasizes the heterogeneity of risk factors for violent behaviors across diagnoses and contexts, with established risk factors including homelessness, childhood adversity, substance abuse, and lack of social support and other factors [11, 16]. However, many questions remain to be answered about how to effectively identify and manage violent behaviors in this population. In addition, the evidence on the factors influencing violent behaviors in individuals with SMIs needs to be further supplemented and validated.
In this context, identifying the factors closely associated with the risk assessment and intervention strategies for violent behaviors is critical importance. Demographic variables, such as gender, age, and socioeconomic status, have been shown to significantly influence violent behaviors, with females, younger individuals, and those from economically disadvantaged backgrounds being at higher risk [17–19]. More recent research has highlighted the influence of psychological factors, such as stigma and self-stigmatization, on violent behaviors [20, 21], suggesting that addressing these psychological factors can effectively reduce the risk of violent behaviors [22]. Furthermore, their cognition and behavior are significantly affected by the illness itself [23], while treatment-related factors, including medication adherence, type of illness, and access to mental health services, play a substantial role in shaping violent behaviors [24]. Therefore, focusing on these variables provides a more comprehensive understanding of the complex mechanisms underlying violent behavior in individuals with SMIs and offers practical guidance for clinicians and policymakers in developing early risk identification and tailored intervention strategies.
The purpose of this study is to achieve a more comprehensive understanding of how risk factors interact and predict violent behaviors in individuals with SMIs. This cross-sectional study aims to identify significant predictors of violent behaviors in individuals with SMIs using both Logistic regression and CHAID decision tree analysis. The goal is to develop a comprehensive model incorporating key risk factors across demography, psychological, and treatment domains. By offering targeted insights for early risk identification and the development of tailored intervention strategies, the study ultimately seeks to improve treatment outcomes for patients and contribute to public health advancement.
Materials and methods
Study design and participants
A cross-sectional study was conducted from January to July 2022, recruiting individuals with SMIs from 23 community health centers in Nanjing, China. These community health service centers provide individuals with SMIs (Mainly includes the six major categories of the Chinese Norms for the Chinese Management and Treatment of Severe Mental Illnesses (2018 Edition): schizophrenia, schizoaffective disorder, paranoid psychosis, bipolar disorder, epilepsy-related mental disorder, and intellectual disability with mental disorder) with filing management and community rehabilitation services [25]. Participants were randomly selected using a random number table method with 50 individuals per center (n = 1,150). After excluding incomplete data (n = 42), a final sample of 1,108 individuals with SMIs was analyzed.
We included participants with 1) diagnosed by attending psychiatrists according to the Chinese Classification and Diagnostic Criteria for Mental Disorders, 3rd Edition (CCMD-3); 2) total illness duration ≥ 3 years; 3) aged ≥ 18 years; 4) stable condition, positive and negative symptom scale (PANSS) total score ≤ 60. The CCMD-3 is widely used in China and demonstrates a high degree of consistency with the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD) in its diagnostic categories [26]. Additionally, it incorporates cultural and social factors specific to the Chinese context, addressing how these influences shape the presentation of mental disorders [27]. This cultural sensitivity makes CCMD-3 particularly well-suited for clinical practice and community management among Chinese patients [25].
We excluded participants with 1) severe cardiovascular, cerebrovascular, hepatic, renal, or other physical diseases; 2) history of drug dependence or addiction; 3) currently in the acute phase of mental illness, with a PANSS total score > 60; 4)non-cooperation or withdrawal from the study; 5) data incomplete. The decision to exclude a history of substance use was based on scientific considerations of study design and objectives. The focus of this study was to explore potential risk factors for violent behaviors among individuals with SMIs in terms of demographic information, psychological status, and treatment status. It has been shown that a history of substance use is strongly associated with violent behaviors [28], but the inclusion of such patients may result in drug-related factors overshadowing the role of other risk factors, affecting the independence of the study results. In addition, the strict regulation psychotropic medications in China reduces the prevalence of substance-related disorders in individuals with SMIs [29]. Finally, many patients may choose to conceal their a history of substance use due to social stigma or legal consequences, which may lead to biased data and further affect the reliability of the study [30]. Therefore, after comprehensive consideration, we excluded this population from the study.
The study was approved by the Ethics Committee of Nanjing Medical University (approval number 2023–047). Written informed consent was obtained from a legally authorised representative for anonymised patient information to be published in this article.
A standardized protocol was adopted to explain the purpose of the survey and the requirements for completing the data to participants, emphasizing data accuracy. Due to the sensitivity of the topic, all questionnaires were distributed and collected on-site by the researchers. Data collection was supplemented with medical records and file documentation to verify inclusion/exclusion criteria. These records were maintained by community mental health centers and included detailed psychiatric diagnostic, disease duration, comorbidities, and medication use. In addition, information was gathered through questionnaires and interviews with participants and their primary caregivers, which was cross-verified by the researchers to ensure accuracy and reliability. Data quality control procedures included pre-survey training for all research staff, multiple data entry, and strict accuracy checks.
Instruments
Positive and Negative Symptom Scale (PANSS)
The PANSS is used to assess the severity of psychiatric symptoms in individuals with SMIs. The scale is a clinician-administered tool to assess positive (such as hallucinations and delusions) and negative (such as affective withdrawal and emotional retardation) symptoms of psychiatric disorders and general psychopathology (such as, anxiety and depression) [31]. The scale consists of 30 items divided into three subscales: positive symptoms (7 items), negative symptoms (7 items), and general psychopathology (16 items). Each item is rated on a 7-point Likert scale ranging from 1 (absent) to 7 (extremely severe), with higher scores indicating more severe symptoms This scale is now widely validated in clinical practice and has high reliability in the population with SMIs [32].
In this study, participants’ symptom status was assessed by professional psychiatrists using the PANSS. Patients with a total score of ≤ 60 were included to ensure that the study population was in a relatively stable mental state, thereby minimizing the potential interference of acute symptoms on the research outcomes. Furthermore, this inclusion criterion enhanced the feasibility of patient participation and improved the reliability of the collected data.
Predictor variables
The questionnaire assessed potential influencing factors of violent behaviors in individuals with SMIs. Key domains, informed by literature review and expert consultation [33–36].
Demographic information: age (categorized according to WHO standards as 18–45 years [young], 46–59 years [middle-aged], and ≥ 60 years [elderly]), gender (male or female), education (elementary or below, middle school, high school, college or higher), marital status (no spouse or present spouse), employment (unemployed or employed), annual household income (< 30,000, 30,000–60000, > 60,000 RMB), poverty or subsistence allowances (yes or no), family history of mental illness (yes or no), and diagnosis of mental illness (schizophrenia or other severe mental illnesses).
Psychological status: The concealment of illness was assessed by asking participants, “Do you often hide your mental illness from others?” with responses categorized as “yes” or “no.” Family acceptance was evaluated by asking, “Does your family reject you because of your illness?” with responses also categorized as “yes” or “no.” Experiences of discrimination were determined by asking participants, “Have you ever been discriminated against or avoided by others because of your illness?” Responses were similarly categorized as “yes” or “no.” To ensure data accuracy, responses were further confirmed with the patients’ primary caregivers.
Treatment status: home-to-hospital time (≤ 30, 31–60, > 60 min), presence of comorbidities (yes or no), disease duration (< 10, 10–20, 21–30, > 30 years), access to medical assistance (yes or no), self-reported health status (good, average, poor), and medication adherence (regularly use, intermittently use, rarely use, not use).
All information was initially collected through patient interviews and self-reports, which were subsequently verified by their primary caregivers. To further ensure the accuracy and reliability of the data, key details such as psychiatric diagnoses, family history, comorbidities, and disease progression were cross-referenced with the patients’ medical records.
Outcome variable
Risk assessment employed the 6-level system defined in the Chinese Norms for the Management and Treatment of Severe Mental Illnesses (2018 version). The system is a widely used expert judgment tool in China to guide clinical management, and is now widely used in the risk assessment of individuals with SMIs [37]. The levels are defined as follows: Level 0: no behaviors meet criteria for levels 1–5; Level 1: verbal threats, shouting without property damage; Level 2: Property damage confined to the home, able to be stopped through persuasion; Level 3: Unprovoked property damage, unable to be stopped through persuasion; Level 4: Persistent property damage or harm directed at oneself or others, regardless of context, unable to be stopped through persuasion; Level 5: Violence against a person with a dangerous weapon, arson, or similar, regardless of context. The World Health Organization (WHO) defines violent behaviors as the intentional use of force or weapons to threaten or harm oneself, others, groups, or society, resulting in or potentially leading to injury, developmental disorders, psychological harm, death, or deprivation of rights. This definition emphasizes that violent behaviors is not limited to physical abuse but also includes threats, coercion, deprivation of rights, and neglect [38]. Based on this framework, verbal threats and shouting are also considered forms of violent behaviors in our study, as they can cause significant psychological harm and emotional distress [39], which align with the broader understanding of violent behaviors outlined by the WHO. For analysis, “violent behaviors” included any patient classified as L1-L5, while those at L0 were categorized as “no violent behaviors” [40]. For our study, violent behaviors were assessed by psychiatrists through interviews with patients about whether they had exhibited any of the above behaviors in the past 12 months [41]. To ensure accuracy, the primary caregivers of the patients were also interviewed to confirm the information.
Statistical analysis
Data were analyzed using IBM SPSS 27.0. Analysis followed three stages. Firstly, Enumeration data were presented as frequencies and percentages. Measurement data were described as mean ± standard deviation, and univariate analysis used the χ2 test (α = 0.05) to identify variables associated with violent behaviors. Statistically significant variables from the univariate analysis were included in a binary Logistic regression model (α = 0.05) to identify independent risk factors for violent behaviors.
In the second phase, a Chi-squared Automatic Interaction Detection (CHAID) decision tree model was employed to reexplore interactions between risk factors and identify subgroups at varying risk levels. The CHAID algorithm is a method for decision tree analysis. It divides data into smaller subgroups based on homogeneity and uses “if–then” logic to predict binary outcomes [42]. This method visualizes the relationship between the target variable (dependent variable) and related variables in a tree-like structure [43], making it an effective approach for data analysis and identifying significant correlated factors. Additionally, the CHAID algorithm determines the optimal combination of categorical or continuous variables based on data homogeneity. Over-fitting was prevented by pruning the tree with a maximum depth of 3, minimum parent/child node sizes of 100/50, and a stopping rule of α = 0.05.
In the third stage, Receiver operating characteristics (ROC) curves were constructed for both models. Area under the ROC curve (AUC), sensitivity, and specificity were used to compare model performance. AUC values were interpreted according to the criteria. The closer the AUC value is to 1, the better the performance of the model. The AUC value > 0.5 indicates that the model has some level of discriminatory ability. However, only when the AUC value > 0.7 is the model’s discriminatory ability considered acceptable, indicating that the model has more than a 70% probability of correctly distinguishing between positive and negative samples [44].
Results
Violent behaviors in individuals with SMIs
A total of 1,108 participants were included in the study. Among them, 39.6% were aged between 46 and 59 years. The majority of participants were female (60.5%), employed (84.6%), and present spouse (64.2%). Nearly half of the participants had an education level of elementary school or below (50.6%). Schizophrenia was the predominant diagnosis, accounting for 60.3% of the sample. Additionally, 550 participants (49.6%) reported engaged in violent behaviors in the past 12 months. Univariate analysis identified significant differences (p < 0.05) in violent behaviors prevalence based on several factors, including employment, family history, poverty or subsistence allowance status, access to assistance, household income, home-to-hospital time, self-reported health status, experiences of discrimination, and medication adherence. Detailed results are presented in Table 1.
Table 1.
A univariate analysis of the influencing factors of violent behaviors in individuals with SMIs
| Variables | Total (n = 1080) | Risk behavior | X2 | P-value | |
|---|---|---|---|---|---|
| No (n = 558) | Yes (n = 550) | ||||
| Gender | 1.112a | 0.292 | |||
| Male | 438(39.5%) | 212 (48.4%) | 226 (51.6%) | ||
| Female | 670(60.5%) | 346 (51.6%) | 324 (48.4%) | ||
| Age | 0.564a | 0.754 | |||
| 18 ~ 45 | 383(34.6%) | 187 (48.8%) | 196 (51.2%) | ||
| 46 ~ 59 | 409(36.9%) | 210 (51.3%) | 199 (48.7%) | ||
| ≥ 60 | 316(28.5%) | 161 (50.9%) | 155 (49.1%) | ||
| Education | 3.863a | 0.277 | |||
| Elementary or below | 561(50.6%) | 272 (48.5%) | 289 (51.5%) | ||
| Middle school | 348(31.4%) | 190 (54.6%) | 158 (45.4%) | ||
| High school | 144(13.0%) | 68 (47.2%) | 76 (52.8%) | ||
| Collage or higher | 55(5.0%) | 28 (50.9%) | 27 (49.1%) | ||
| Marital status | 0.755a | 0.385 | |||
| No spouse | 397(35.8%) | 193 (48.6%) | 204 (51.4%) | ||
| Present spouse | 711(64.2%) | 365 (51.3%) | 346 (48.7%) | ||
| Employment | 13.532a | P < 0.001 | |||
| Unemployed | 171(15.4%) | 64 (37.4%) | 107 (62.6%) | ||
| Employed | 937(84.6%) | 494 (52.7%) | 443 (47.3%) | ||
| Family history | 6.050a | 0.014 | |||
| Yes | 125(11.3%) | 50 (40%) | 75 (60%) | ||
| No | 983(88.7%) | 508 (51.7%) | 475 (48.3%) | ||
| Poverty or subsistence allowances | 5.571a | 0.018 | |||
| Yes | 309(27.9%) | 138 (44.7%) | 171 (55.3%) | ||
| No | 799(72.1%) | 420 (52.6%) | 379 (47.4%) | ||
| Access to medical assistance | 13.142a | P < 0.001 | |||
| Yes | 335(30.2%) | 141 (42.1%) | 194 (57.9%) | ||
| No | 773(69.8%) | 417 (53.9%) | 356 (46.1%) | ||
| Household income (CNYa) | 9.401a | 0.009 | |||
| 0 ~ 30,000 | 682(61.6%) | 331 (48.5%) | 351 (51.5%) | ||
| 30,001 ~ 60,000 | 276(24.9%) | 134 (48.6%) | 142 (51.4%) | ||
| > 60,000 | 150(13.5%) | 93 (62.0%) | 57 (38.0%) | ||
| Diagnosis | 1.336a | 0.248 | |||
| Schizophrenia | 668(60.3%) | 327 (49.0%) | 341 (51.0%) | ||
| Other severe mental illnesses | 440(39.7%) | 231 (52.5%) | 209 (47.5%) | ||
| Disease duration(year) | 1.677a | 0.642 | |||
| 0 ~ 10 | 499(45.0%) | 241 (48.3%) | 258 (51.7%) | ||
| 11 ~ 20 | 285(25.7%) | 150 (52.6%) | 135 (47.4%) | ||
| 21 ~ 30 | 198(17.9%) | 101 (51.0%) | 97 (49.0%) | ||
| > 30 | 126(11.4%) | 66 (52.4%) | 60 (47.6%) | ||
| Home-to-hospital time (min) | 6.497a | 0.039 | |||
| 0 ~ 30 | 990(89.4%) | 488 (49.3%) | 502 (50.7%) | ||
| 31 ~ 60 | 84(7.6%) | 52 (61.9%) | 32 (38.1%) | ||
| > 60 | 29(2.6%) | 18 (62.1%) | 11 (37.9%) | ||
| Missing Data | 5(0.5%) | - | - | ||
| Disease concealment | 1.502a | 0.22 | |||
| Yes | 677(61.1%) | 331 (48.9%) | 346 (51.1%) | ||
| No | 431(38.9%) | 227 (52.7%) | 204 (47.3%) | ||
| Family acceptance | 0.176a | 0.675 | |||
| Yes | 834(75.3%) | 417 (50.0%) | 417 (50.0%) | ||
| No | 274(24.7%) | 141 (51.5%) | 133 (48.5%) | ||
| Experience of discrimination | 22.937a | P < 0.001 | |||
| Yes | 305(27.5%) | 118 (38.7%) | 187 (61.3%) | ||
| No | 803(72.5%) | 440 (54.8%) | 363 (45.2%) | ||
| Self-reported health status | 66.597a | P < 0.001 | |||
| Good | 515(46.5%) | 326 (63.3%) | 189 (36.7%) | ||
| Fair | 528(47.7%) | 201 (38.1%) | 327 (61.9%) | ||
| Poor | 65(5.9%) | 31 (47.7%) | 34 (52.3%) | ||
| Medication adherence | 108.513a | P < 0.001 | |||
| Regularly | 646(58.3%) | 397 (61.5%) | 249 (38.5%) | ||
| Intermittently | 334(30.1%) | 104 (31.1%) | 230 (68.9%) | ||
| Rarely | 68(6.1%) | 16 (23.5%) | 52 (76.5%) | ||
| Not | 60(5..4%) | 41 (76.5%) | 19 (31.7%) | ||
| Comorbidities | 0.462a | 0.497 | |||
| Yes | 364(32.9%) | 178 (48.9%) | 186 (51.1%) | ||
| No | 744(67.1%) | 380 (51.1%) | 364 (48.9%) | ||
aCNY (Chinese Yuan) represents Chinese currency
Predictors of violent behaviors in individuals with SMIs using logistic regression
The Logistic regression analysis identified five key factors associated with violent behaviors in individuals with SMIs: medication adherence, self-reported health status, employment, household income, and experience of discrimination.
Employed patients had a lower prevalence of violent behaviors compared to unemployed patients (OR = 0.519, p < 0.001). Patients with annual household income exceeding ¥60,000 had a lower risk of violent behaviors compared to those earning less than ¥30,000 (OR = 0.637, p < 0.05). Patients reporting good health status had a lower risk of violent behaviors compared to those with general health (OR = 2.481, p < 0.001). Patients who reported experiencing discrimination were more likely to engage in violent behaviors (OR = 1.87, p < 0.001). Patients with intermittent (OR = 2.872, p < 0.001) or rare (OR = 4.038, p < 0.001) medication adherence were more likely to exhibit violent behaviors. For detailed results, refer to Tables 2 and supplementary Table 4.
Table 2.
Binary logistic regression analysis of influencing factors for violent behaviors in individuals with SMIs
| Variables | Category | β | S.E | Wald | P-value | OR (95%CI) |
|---|---|---|---|---|---|---|
| Constant | −0.454 | 0.215 | 4.461 | 0.035 | 0.635 | |
| Employment | Employed | −0.656 | 0.188 | 12.225 | p < 0.001 | 0.519 (0.359, 0.749) |
| Family history | Yes | 0.362 | 0.212 | 2.916 | 0.088 | 1.437 (0.948, 2.177) |
| Poverty or subsistence allowances | Yes | −0.071 | 0.176 | 0.164 | 0.686 | 0.931 (0.659, 1.315) |
| Access to medical assistance | Yes | 0.307 | 0.165 | 3.447 | 0.063 | 1.359 (0.983, 1.878) |
| Experience of discrimination | Yes | 0.626 | 0.158 | 15.763 | p < 0.001 | 1.870 (1.373, 2.547) |
| Household income (CNYa) | 0 ~ 30,000 | 4.822 | 0.090 | |||
| 30,001 ~ 60,000 | −0.035 | 0.160 | 0.048 | 0.827 | 0.966 (0.706, 1.322) | |
| > 60,000 | −0.451 | 0.208 | 4.687 | 0.030 | 0.637 (0.424, 0.958) | |
| Home-to-hospital time (min) | 0 ~ 30 | 4.150 | 0.126 | |||
| 31 ~ 60 | −0.523 | 0.271 | 3.740 | 0.053 | 0.592 (0.349, 1.007) | |
| > 60 | −0.348 | 0.423 | 0.674 | 0.412 | 0.706 (0.308, 1.619) | |
| Self-reported health status | Good | 42.753 | p < 0.001 | |||
| Fair | 0.909 | 0.139 | 42.709 | p < 0.001 | 2.481 (1.889, 3.258) | |
| Poor | 0.416 | 0.288 | 2.092 | 0.148 | 1.517 (0.863, 2.666) | |
| Medication adherence | Regularly | 70.147 | p < 0.001 | |||
| Intermittently | 1.055 | 0.155 | 46.358 | p < 0.001 | 2.872 (2.120, 3.892) | |
| Rarely | 1.396 | 0.310 | 20.224 | p < 0.001 | 4.038 (2.198, 7.419) | |
| Not | −0.602 | 0.312 | 3.721 | 0.054 | 0.548 (0.297, 1.010) |
Abbreviations: OR odds ratio, CI confidence interval
aCNY (Chinese Yuan) represents Chinese currency
Decision tree analysis of violent behaviors in individuals with SMIs
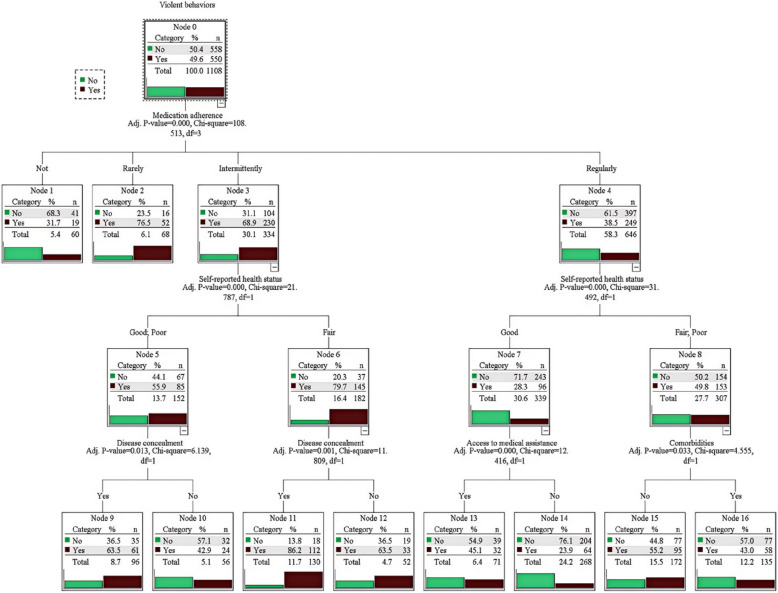
The CHAID decision tree model contains a total of 4 layers, 17 nodes, and 10 terminal nodes (Fig. 1). The model predicts violent behaviors by sequentially splitting the population into subgroups based on the most significant predictors at each level. Each split is determined by statistical significance (p < 0.05), and terminal nodes represent the final subgroups with distinct probabilities of violent behaviors. The model analysis identified five key factors associated with violent behaviors in individuals with SMIs: medication adherence, self-reported health status, disease concealment, access to medical assistance, and comorbidities. The root node of the decision tree was medication adherence, indicating it has the strongest association with violent behaviors in individuals with SMIs. Patients were divided into three groups based on their medication adherence: regular, intermittent, and rare. Those with rare medication adherence exhibited the highest risk of violent behaviors (76.5%) and were classified as a high-risk group without further stratification.
Fig. 1.
CHAID algorithm classification decision tree analysis of influencing factors violent behaviors in individuals with SMIs
Health status further stratified both intermittent and regular medication groups. Good health consistently reduced risk across subgroups. In the intermittent medication group, regardless of health status, disease concealment further stratified this group, with patients concealing their condition being at higher risk of violent behaviors.
Among patients with good health taking medication regularly, the risk of violent behaviors was further influenced by access to medical assistance, with those having access showing a higher risk. In contrast, among patients with fair or poor health, comorbidities played a key role, as the absence of comorbidities was associated with a higher risk of violent behaviors.
Model performance comparison
Both Logistic regression and CHAID decision tree models achieved moderate predictive efficacy (0.7 ~ 0.9) for violent behaviors in individuals with SMIs, as demonstrated by ROC curve analysis (Fig. 2). Area under the curve (AUC) values were similar for both models: Logistic regression: AUC = 0.737 (95% CI 0.708–0.766), sensitivity = 64%, specificity = 70.4%; CHAID decision tree: AUC = 0.730 (95% CI 0.701–0.759), sensitivity = 58%, specificity = 63.3%. No statistically significant difference in AUC was observed between models (Z = −0.712, p = 0.456). This suggests comparable performance in predicting violent behaviors. Although the predictive performance of the Logistic regression and CHAID decision tree models was comparable, they produce different results. The Logistic regression model provided a comprehensive evaluation of risk factors, identifying independent predictors with overarching significance. In contrast, the CHAID decision tree model introduced a hierarchical structure that emphasized interactions between predictors and stratified patients into subgroups with varying levels of risk. This approach visually represented complex interactions, making it particularly valuable for clinical decision-making. These findings demonstrate that the two models offer unique and complementary insights into the risk assessment of violent behaviors from different perspectives, underscoring the importance of employing multiple analytical approaches to gain a more comprehensive understanding of violent behaviors in individuals with SMIs. Detailed results are presented in Table 3.
Fig. 2.
Comparison of ROC curves for Logistic regression models and CHAID decision tree models
Table 3.
Comparison of predictive performance of Logistic regression model and CHAID decision tree model
| MODEL | AUC | S.E | 95%CI | Youden Index | Sensitivity (%) | Specificity(%) | Differentials | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC | S.E | 95%CI | Z | P-value | |||||||
| Logistic regression | 0.737 | 0.015 | 0.708 ~ 0.766*** | 0.344 | 64 | 70.4 | 0.456 | 0.171 | (−0.027,0.012) | −0.745 | 0.456 |
| CHAID decision tree | 0.730 | 0.015 | 0.701 ~ 0.759*** | 0.367 | 58 | 63.3 |
Abbreviations: OR odds ratio, CI confidence interval
*P < 0.05
**P < 0.01
***P < 0.001
Discussion
Current situation of violent behaviors in individuals with SMIs
This study found a 49.6% prevalence of violent behaviors in individuals with SMIs, similar to L Wang, et al. [45] finding of 42.4%. However, our results were significantly higher than other national studies [46, 47]. This discrepancy may be attributed to differences in the criteria used to assess violent behaviors. This study strictly followed the WHO definition of violence, adopting a broader classification of “violent behaviors” [38]. Furthermore, individuals with SMIs in this study were drawn from multiple community settings, and this diverse social context may have allowed for the identification of a wider range of risk behaviors [48].
Influencing factors of violent behaviors in individuals with SMIs
Violent behaviors in individuals with SMIs pose a significant threat to public safety, not only due to their potential risks but also because of the complex social and psychological factors underlying these behaviors. We examine the occurrence and influencing factors of violent behaviors in individuals with SMIs within the community, considering their demographic information, psychological status, and treatment status.
Unemployment was significantly associated with higher violent behaviors in SMIs, consistent with previous findings of Qiao et al. [49]. This may be due to reduced social interaction, poor social adaptation, and financial struggles impacting treatment adherence. In addition to this, the financial struggles associated with unemployment can add stress and make it more difficult for individuals to manage long-term behaviors and decisions [50]. Chronic stress and limited resources may exacerbate mental health symptoms and reduce patients’ ability to engage in rehabilitation programs, making them vulnerable to violent behaviors [51]. At the same time, violent behaviors itself may be a major cause of unemployment among individuals with SMIs. Addressing this issue requires enhanced rehabilitation services to improve employability and government support for vocational training [52].
Higher annual household income (> 60,000 RMB) was associated with a lower risk of violent behaviors, consistent with previous studies [53, 54]. Financial stability may enable access to better healthcare and sustained rehabilitation, fostering a more stable environment for recovery. Conversely, low-income families may face barriers to effective disease control, including limited access to medication and rehabilitation services, which can increase the risk of violent behaviors [55]. Expanding community initiatives and free treatment programs for low-income individuals with SMIs is critical to addressing these disparities.
Recipients of medical assistance exhibited a higher risk of violent behaviors, which contrasts with findings by Q Li, et al. [56]. This could be due to individuals with SMIs who receives medical assistance may have more severe symptoms or fall into a diagnostic category with a higher inherent risk of violent behaviors, such as psychotic disorder or mood disorder. Additionally, these patients in need of medical assistance may themselves be unstably housed, receive more sporadic and inadequate treatment, and may have poorer treatment adherence [57]. Addressing these issues requires prioritizing psychological needs, including emotional support, stress management, and reducing stigma to promote social inclusion [58, 59]. These needs stem from patients’ lived experiences, such as feelings of exclusion and helplessness, rather than being imposed by care systems. Prompt management of dysphoria, continuity of care, and a supportive environment are critical to preventing violent behavior in individuals with SMIs [60].
Both models identified good health as a protective factor against violent behaviors in individuals with SMIs, aligning with previous research [61]. This suggests that physical and mental health rehabilitation strengthens resilience and reduces adverse risks [62]. Families and rehabilitation organizations can play a crucial role by emphasizing holistic training for improved well-being.
Discrimination significantly increased violent behaviors in individuals with SMIs, consistent with previous research [63]. This suggests that experiences of inferiority, helplessness, and exclusion contribute to aggressive and hostile behaviors. However, such violent behaviors may lead to further avoidance and alienation by others, exacerbating the discrimination faced by individuals with SMIs. Therefore, providing mental health support, social support, and combating stigma are crucial in reducing these risks [64].
Medication adherence is a critical factor influencing violent behaviors in individuals with SMIs. While the initial analysis suggested lower violent behaviors risk in non-medicated patients, excluding those not needing medication due to stabilization revealed a negative correlation between medication adherence and violent behaviors. This aligns with previous research [65], highlighting the importance of long-term medication for controlling symptoms and reducing risks of violent behaviors in individuals with SMIs [66]. Therefore, individuals with SMIs should be on regular long-term medication to promote their own mental recovery. While long-term medication is a critical foundation for stabilizing symptoms and preventing relapse in individuals with SMIs, it is not sufficient to achieve full recovery on its own [67]. In the short term, therapies such as cognitive-behavioral therapy and community-based rehabilitation are essential to address underlying psychological and social factors and reduce violent behaviors [68]. Factors like low economic status, mental disability, social issues, and lack of support can hinder medication adherence [69]. To improve medication adherence and outcomes, targeted interventions such as enhanced health education, expanded mental health services, improved access to affordable medication, and stronger social support networks are necessary to empower patients and promote recovery [70].
Concealing their disease emerged as a risk factor for violent behaviors in the decision tree analysis. This aligns with research highlighting the detrimental impact of stigma on mental rehabilitation [71]. Stigma-related factors, such as reduced social acceptance and feelings of shame, can hinder recovery and increase the likelihood of violent behaviors in individuals with SMIs. However, this risk is not universal. For some patients, concealing their disease may act as a psychological coping mechanism to protect themselves from anticipated stigma or social rejection [72]. For example, patients may conceal their condition to avoid being labeled as “dangerous”. In such instances, hiding their condition is less about contributing to violent behavior and more about mitigating fears of discrimination and social exclusion. Therefore, multi-pronged efforts are crucial: reducing societal discrimination against individuals with mental illnesses, fostering a supportive environment within families and communities, and addressing the personal shame experienced by these patients [73].
Interestingly, the CHAID decision tree identified the absence of comorbidities as a risk factor for violent behaviors in individuals with SMIs, contrary to previous findings of higher risk in co-morbid patients [74]. One possible explanation for this discrepancy is that patients with comorbidities are often more closely monitored by healthcare providers, which may result in better adherence to treatment plans and more structured daily routines. The increased frequency of medical visits and interactions with healthcare professionals provides these patients with additional opportunities for mental health evaluations, counseling, and reinforcement of positive health behaviors [75]. These factors may collectively help reduce the risk of violent behaviors. However, this interpretation requires caution and further empirical investigation, as there is currently no direct evidence to support these claims. Regardless of the underlying factors, implementing effective and engaging rehabilitation plans for all individuals with SMIs remains crucial.
This study highlights the complex interactions between factors contributing to violent behaviors in individuals with SMIs. For example, the CHAID decision tree revealed how disease concealment and access to medical assistance interact with medication adherence and health status to influence outcomes, insights that were not evident from the logistic regression model. These findings emphasize the need for a holistic approach to risk assessment that considers the interplay of demographic, psychological, and treatment-related factors. An overarching narrative that integrates these factors can guide more effective interventions tailored to the diverse needs of individuals with SMIs.
This study employed Logistic regression and CHAID decision tree analyses to comprehensively assess risk factors for violent behaviors in individuals with SMIs. To the best of our knowledge, few researchers have utilized machine learning in conjunction with traditional regression models to investigate the factors that influence violent behaviors in individuals with SMIs. While both models demonstrated comparable predictive accuracy, they offered complementary insights into the underlying risk factors. The Logistic regression identified independent predictors and quantified their individual contributions to violent behaviors, providing a global perspective on risk. On the other hand, the CHAID decision tree highlighted interactions between predictors and stratified patients into subgroups with varying risk levels, offering a more granular understanding of subgrouP-specific risks. These differences highlight the complexity and multidimensional nature of risk factors for violent behavior, with each model offering a unique perspective on their characteristics. By combining the strengths of both models, this study provides a more comprehensive understanding of the multifaceted nature of risk factors, enabling clinicians to develop personalized interventions and targeted risk management strategies.
Limitations
This study has several limitations that should be considered when interpreting its findings. First, the data were primarily self-reported by patients, which may lead to underreporting of violent behaviors and introduce potential bias. Second, the study subjects were mainly from Jiangning District, Nanjing. This region is more economically developed, has a higher level of urbanization, and has better constructed community rehabilitation services for individuals with SMIs, which is very different from less developed or rural areas. These regional characteristics may affect the prevalence and nature of violent behaviors among individuals with SMIs, thus limiting the generalizability of the findings to other populations and settings. Future studies should include participants from more diverse regions to improve external validity. Third, this study excluded patients with a history of drug dependence or addiction and did not consider the role of caregivers. As drug dependence is strongly linked to violent behaviors in individuals with SMIs [76], and caregivers play a critical role in shaping patients’ behaviors [77], these exclusions limit the generalizability of the findings and overlook important influencing factors. Future studies should include these populations to provide a more comprehensive understanding of violent behaviors. Fourth, this study excluded patients who were in the acute phase of illness, defined as having a PANSS total score > 60. While this exclusion criterion was necessary to ensure the stability of the study population and the reliability of the data, it also resulted in a selective study population that may not fully represent individuals with SMIs who are in more severe or unstable conditions. Future studies should include patients in the acute phase to better understand the full spectrum of violent behaviors in individuals with SMIs. Fifth, this study only assessed whether patients engaged in violent behaviors within the past 12 months, without quantifying their frequency or severity. This limits a deeper understanding of the characteristics of violent behaviors and how they differ across populations. For example, episodic minor violent behaviors may have completely different impact mechanisms and intervention needs than frequent and severe violent behaviors. Future research should collect more comprehensive data on the frequency, intensity, and situational factors of violent behaviors to better explore the potential influences of violent behaviors and its variation across populations. In addition, this study did not use a quantitative psychometric tool to assess patients’ psychological state, which limits quantitative analysis of measurement error. Future studies should introduce validated psychometric tools to improve the reliability and generalizability of results. Finally, the cross-sectional design precludes investigation of causal relationships between identified factors and violent behaviors. Longitudinal studies are needed to draw stronger causal inferences and examine the temporal dynamics of these relationships.
Conclusions
This study identified a concerningly high prevalence of violent behaviors in individuals with SMIs. Combined analysis of Logistic regression and CHAID decision tree models revealed several key factors associated with increased risk of violent behaviors in individuals with SMIs, including unemployment, low income, dependence on medical assistance, poor health status, medication non-adherence, disease concealment, experiences of discrimination, and absence of comorbidities (potentially indicating reduced healthcare engagement). Among the many influencing factors, medication adherence may be the most critical factor contributing to violent behavior in individuals with SMIs. These findings provide valuable insights for developing targeted interventions to reduce violent behaviors in individuals with SMIs. Potential strategies include implementing cognitive and behavioral therapy alongside medication management, enhancing community-based follow-up and rehabilitation programs, expanding access to free treatment, increasing medical assistance frequency and amounts, and offering comprehensive, multifaceted support to patients. By addressing these crucial factors through integrated interventions and effective policy measures, we can work towards reducing the incidence of violent behaviors and improving the well-being of individuals with SMIs.
Relevance for clinical practice
This study underscores the multifaceted factors contributing to violent behaviors in individuals with SMIs and offers actionable recommendations for clinical practice. The findings highlight the pivotal roles of medication adherence, demographic factors, and psychological factors, such as stigma and discrimination, in influencing violent behaviors. To address these issues, clinicians and healthcare systems should prioritize enhancing medication adherence through targeted health education, regular follow-ups, and ensuring access to affordable medications. Concurrently, socioeconomic challenges should be mitigated through vocational training and financial assistance programs. Efforts to reduce stigma and promote social inclusion, such as psychoeducation and community-based rehabilitation programs, are equally critical. For high-risk groups, including those concealing their illness or relying on medical assistance, personalized interventions focusing on emotional support, stress management, and continuity of care are essential.
Supplementary Information
Acknowledgements
The authors gratefully acknowledge the assistance of the staff in the Center for Disease Control and Prevention of Jiangning District in Nanjing in conducting the survey.
Clinical trial number
Not applicable.
Financial support
This research was supported by the National Natural Science Foundation of China (Grant No.72374109); the Open Research Fund Program of Changzhou Institute for Advanced Study of Public Health, Nanjing Medical University (CPHS202301); the 2022 China Medical Board Open Competition Program (CMB-OC2, 22-475); and the Project of “Nursing Science” Funded by the 4th Priority Discipline Development Program of Jiangsu Higher Education Institutions (Jiangsu Education Department[2023] No.11). The funders had no role in the design and conduct of the study, data collection, analysis, and interpretation; writing of the manuscript; or the decision to submit the article for publication.
Authors’ contributions
YW and HF participated in the conception and design of the study; YW analyzed and interpreted the data and wrote the manuscript; JJD participated in the formal analysis and visualization; JF and JWZ contributed to the interpretation of the results; SZW and XZ took part in the investigation and data curation; HF and LW coordinated and supervised data collection; HF critically reviewed and revised the manuscript and obtained funding. All authors have read and approved the final manuscript.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in adherence to the local and international ethical principles including those in the Declaration of Helsinki. The study was approved by the Ethics Committee of Nanjing Medical University (approval number 2023–047). Written informed consent was obtained from a legally authorised representative for anonymised patient information to be published in this article.
Consent for publication
Before their involvement in the study, all participants provided informed consent.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
5/3/2025
Reference 74 was incorrect in the original publication. The article has been updated to rectify the error.
References
- 1.DeVylder JE. Preventing schizophrenia and severe mental illness: a grand challenge for social work. Res Soc Work Pract. 2016;26(4):449–59. 10.1177/1049731515622687. [Google Scholar]
- 2.Baughman KR, Bonfine N, Dugan SE, Adams R, Gallagher M, Olds RS, Piatt E, Ritter C. Disease burden among individuals with severe mental illness in a community setting. Community Ment Health J. 2016;52:424–32. 10.1007/s10597-015-9973-2. [DOI] [PubMed] [Google Scholar]
- 3.Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54:10. 10.1016/j.eclinm.2022.101675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–60. 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gronholm PC, Chowdhary N, Barbui C, Das-Munshi J, Kolappa K, Thornicroft G, Semrau M, Dua T. Prevention and management of physical health conditions in adults with severe mental disorders: WHO recommendations. Int J Ment Heal Syst. 2021;15(1):22. 10.1186/s13033-021-00444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fiorillo A, Luciano M, Pompili M, Sartorius N. Editorial: reducing the mortality gap in people with severe mental disorders: the role of lifestyle psychosocial interventions. Front Psychiatry. 2019;10:3. 10.3389/fpsyt.2019.00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Health and Health Commission of the People's Republic of China. Chinese norms for the management and treatment of serious mental illnesses (2018 Edition). Chinese Practical Journal of Rural Doctor. 2018;25(7):11-22. 10.3969/j.issn.1672-7185.2018.07.002.
- 8.Zhang W, Ma N, Wang X, Wu X, Zhao M, Chen R, Guan L, Ma H, Yu X, Lu L. Management and services for psychosis in the People’s Republic of China in 2020. Chin J Psychiatry. 2022;55(2):122–8. [Google Scholar]
- 9.Freeman M. The World Mental Health Report: transforming mental health for all. World Psychiatry. 2022;21(3):391–2. 10.1002/wps.21018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fu J, Zhu JW, Wang SZ, Xia Z, Ran Z, Nan Z, Fan H. A comparative study on rehabilitation service models of severe mental disorders at home and abroad. Med Philos. 2023;44(07):60–3. [Google Scholar]
- 11.Whiting D, Lichtenstein P, Fazel S. Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry. 2021;8(2):150–61. 10.1016/S2215-0366(20)30262-5. [DOI] [PubMed] [Google Scholar]
- 12.Melo APS, Dippenaar IN, Johnson SC, Weaver ND, de Assis AF, Malta DC, Ribeiro ALP, Júnior AAG, Wool EE, Naghavi M, Cherchiglia ML. All-cause and cause-specific mortality among people with severe mental illness in Brazil’s public health system, 2000–15: a retrospective study. Lancet Psychiatry. 2022;9(10):771–81. 10.1016/s2215-0366(22)00237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamperman AM, Henrichs J, Bogaerts S, Lesaffre E, Wierdsma AI, Ghauharali RRR, Swildens W, Nijssen Y, van der Gaag M, Theunissen JR, Delespaul PA, van Weeghel J, van Busschbach JT, Kroon H, Teplin LA, van de Mheen D, Mulder CL. Criminal victimisation in people with severe mental illness: a multi-site prevalence and incidence survey in the Netherlands. PLoS ONE. 2014;9(3):13. 10.1371/journal.pone.0091029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fazel S, Wolf A, Palm C, Lichtenstein P. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry. 2014;1(1):44–54. 10.1016/s2215-0366(14)70223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeng Y-z, Cheng Y-x. Recognition and control dangerous behavior of severe mental patients in Beijing. Soft Sci Health. 2020;34(7):46–50. 10.3969/j.issn.1003-2800.2020.07.010. [Google Scholar]
- 16.Rund BR. A review of factors associated with severe violence in schizophrenia. Nord J Psychiatry. 2018;72(8):561–71. 10.1080/08039488.2018.1497199. [DOI] [PubMed] [Google Scholar]
- 17.Harford TC, Chen CM, Kerridge BT, Grant BF. Self-and other-directed forms of violence and their relationship with lifetime DSM-5 psychiatric disorders: results from the National Epidemiologic Survey on Alcohol Related Conditions− III (NESARC− III). Psychiatry Res. 2018;262:384–92. 10.1016/j.psychres.2017.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai H, Mei Z, An A, Wu J. Epidemiology of physical and mental comorbidity in Canada and implications for health-related quality of life, suicidal ideation, and healthcare utilization: a nationwide cross-sectional study. J Affect Disord. 2020;263:209–15. 10.1016/j.jad.2019.11.146. [DOI] [PubMed] [Google Scholar]
- 19.Talevi D, Collazzoni A, Rossi A, Stratta P, Mazza M, Pacitti F, Costa M, Crescini C, Rossi R. Cues for different diagnostic patterns of interpersonal violence in a psychiatric sample: an observational study. BMC Psychiatry. 2020;20:1–9. 10.1186/s12888-020-02594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Labrum T, Simonsson P, Solomon PL. Stigma contributes to the risk of violence by persons with mental illness. J Psychosoc Rehabil Ment Health. 2018;5:209–12. [Google Scholar]
- 21.Fusar-Poli P, Sunkel C, Larrauri CA, Keri P, McGorry PD, Thornicroft G, Patel V. Violence and schizophrenia: the role of social determinants of health and the need for early intervention. World Psychiatry. 2023;22(2):230–1. 10.1002/wps.21074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McIntosh LG, Janes S, O’Rourke S, Thomson LD. Effectiveness of psychological and psychosocial interventions for forensic mental health inpatients: a meta-analysis. Aggress Violent Beh. 2021;58: 101551. [Google Scholar]
- 23.Fu J, Zhu J, Dong J, Wang Y, Wang S, Zhang X, Wen L, Fan H. Recovery from severe mental illnesses: the influence of personal and psychosocial factors in community settings. Int J Ment Health Nurs. 2024. 10.1111/inm.13440. [DOI] [PubMed] [Google Scholar]
- 24.Kane JM, Correll CU. Optimizing treatment choices to improve adherence and outcomes in schizophrenia. J Clin Psychiatry. 2019;80(5):10. 10.4088/jcp.In18031ah1c. [DOI] [PubMed] [Google Scholar]
- 25.Chen YF. Chinese classification of mental disorders (CCMD-3): towards integration in international classification. Psychopathology. 2002;35(2–3):171–5. 10.1159/000065140. [DOI] [PubMed] [Google Scholar]
- 26.Yunfei D, Zeping X. Comparison of the Chinese classification and diagnostic criteria for mental disorders, 3rd edition, with the international classification of diseases, 10th edition. J Clin Psychiatry. 2013;23(6th):426–7. [Google Scholar]
- 27.Dai YF, Yu X, Xiao ZP, Xu YF, Zhao M, Correia JM, Maj M, Reed GM. Comparison of Chinese and international psychiatrists’ views on classification of mental disorders. Asia Pac Psychiatry. 2014;6(3):267–73. 10.1111/appy.12146. [DOI] [PubMed] [Google Scholar]
- 28.Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8): e1000120. 10.1371/journal.pmed.1000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao M. Supply reduction policy against new psychoactive substances in China: policy framework and implementation. Int J Law Crime Justice. 2020;60: 100374. [Google Scholar]
- 30.Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, Wagner HR, Rosenheck RA, Stroup TS, McEvoy JP, Lieberman JA. A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63(5):490–9. 10.1001/archpsyc.63.5.490. [DOI] [PubMed] [Google Scholar]
- 31.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76. 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 32.Kumari S, Malik M, Florival C, Manalai P, Sonje S: An Assessment of Five (PANSS, SAPS, SANS, NSA-16, CGI-SCH) commonly used Symptoms Rating Scales in Schizophrenia and Comparison to Newer Scales (CAINS, BNSS). J Addict Res Ther 2017, 8(3). 10.4172/2155-6105.1000324. [DOI] [PMC free article] [PubMed]
- 33.Ose SO, Lilleeng S, Pettersen I, Ruud T, van Weeghel J. Risk of violence among patients in psychiatric treatment: results from a national census. Nord J Psychiatry. 2017;71(8):551–60. 10.1080/08039488.2017.1352024. [DOI] [PubMed] [Google Scholar]
- 34.Ribeiro WS, Bauer A, Andrade MCR, York-Smith M, Pan PM, Pingani L, Knapp M, Coutinho ESF, Evans-Lacko S. Income inequality and mental illness-related morbidity and resilience: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4(7):554–62. 10.1016/S2215-0366(17)30159-1. [DOI] [PubMed] [Google Scholar]
- 35.Iozzino L, Ferrari C, Large M, Nielssen O, De Girolamo G. Prevalence and risk factors of violence by psychiatric acute inpatients: a systematic review and meta-analysis. PLoS ONE. 2015;10(6): e0128536. 10.1371/journal.pone.0128536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sumner SA, Mercy JA, Dahlberg LL, Hillis SD, Klevens J, Houry D. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478–88. 10.1001/jama.2015.8371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y, Yan LL, Ronsmans C, Wen H, Xu J, Wang D, Yang M. Excess mortality among patients with severe mental disorders and effects of community-based mental healthcare: a community-based prospective study in Sichuan, China. BJPsych Open. 2021;7(3): e84. 10.1192/bjo.2021.46. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 38.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. The lancet. 2002;360(9339):1083–8. [DOI] [PubMed] [Google Scholar]
- 39.Wang Q-W, Hou C-L, Wang S-B, Huang Z-H, Huang Y-H, Zhang J-J, Jia F-J. Frequency and correlates of violence against patients with schizophrenia living in rural China. BMC Psychiatry. 2020;20:1–8. 10.1186/s12888-020-02696-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang ZH, Wang F, Chen ZL, Xiao YN, Wang QW, Wang SB, He XY, Migliorini C, Harvey C, Hou CL. Risk factors for violent behaviors in patients with schizophrenia: 2-year follow-up study in primary mental health care in China. Front Psychiatry. 2022;13: 947987. 10.3389/fpsyt.2022.947987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yao Wenshan, ed. National norms for basic public health services, 3rd edition. 2017.
- 42.Choi HY, Kim EY, Kim J. Prognostic factors in diabetes: comparison of Chi-square automatic interaction detector (CHAID) decision tree technology and logistic regression. Medicine (Baltimore). 2022;101(42):6. 10.1097/md.0000000000031343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pradhan B. A comparative study on the predictive ability of the decision tree, support vector machine and neuro-fuzzy models in landslide susceptibility mapping using GIS. Comput Geosci. 2013;51:350–65. 10.1016/j.cageo.2012.08.023. [Google Scholar]
- 44.Narkhede S. Understanding auc-roc curve. Towards Data Sci. 2018;26(1):220–7. [Google Scholar]
- 45.Wang L, Xu JL, Zou HO, Zhang HY, Qu YH. Violence against primary caregivers of people with severe mental illness and their knowledge and attitudes towards violence: A cross-sectional study in China. Arch Psychiatr Nurs. 2019;33(6):167–76. 10.1016/j.apnu.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 46.Qiu J, Liao C, Zhu L, Huang P, Chen H. Relationship between personality and coping styles among assaultive psychiatric patients. J Nurs Sci. 2014;29(13):62–5. [Google Scholar]
- 47.Chang WC, Chan SSI, Hui CLM, Chan SKW, Lee EHM, Chen EYH. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: a 3-year follow-up study. Aust N Z J Psych. 2015;49(10):914–22. 10.1177/0004867415603130. [DOI] [PubMed] [Google Scholar]
- 48.Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, Rosenberg SD, Meador KG. The social–environmental context of violent behavior in persons treated for severe mental illness. Am J Public Health. 2002;92(9):1523–31. 10.2105/ajph.92.9.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qiao XW, Di ZX. Analysis of factors of troubles caused by serious psychiatric patients in Lanzhou. Foreign Med Sci(Section of Medgeography). 2016;37(04):316–9. [Google Scholar]
- 50.Wilson H, Finch D: Unemployment and mental health. The Health Foundation 2021. https://www.health.org.uk/sites/default/files/2021-04/2021%20-%20Unemployment%20and%20mental%20health.pdf.
- 51.Silva M, Resurrección DM, Antunes A, Frasquilho D, Cardoso G. Impact of economic crises on mental health care: a systematic review. Epidemiol Psychiatric Sci. 2020;29: e7. 10.1017/S2045796018000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weng R-z. Analysis of influencing factors and preventive measures of trouble-making and accident-causing behaviors of schizophrenic patients. Shanghai Nurs. 2023;23(07):50–3. [Google Scholar]
- 53.Hu X, Chen T, Liang Z, Zhang Y, Zhao J. Analysis of the employment status and influencing factors of community patients with severe mental disorders in Jiading District. J Psychiatry. 2020;33(01):54–7. [Google Scholar]
- 54.Liu YY, Liu X, Wen H, Wang D, Yang XM, Tang WW, Li YX, Zhang T, Yang M. Risk behavior in patients with severe mental disorders: a prospective study of 121,830 patients managed in rural households of western China. BMC Psychiatry. 2018;18:13. 10.1186/s12888-018-1709-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sonnweber M, Lau S, Kirchebner J. Violent and non-violent offending in patients with schizophrenia: exploring influences and differences via machine learning. Compr Psychiat. 2021;107:6. 10.1016/j.comppsych.2021.152238. [DOI] [PubMed] [Google Scholar]
- 56.Li Q, Song J, Zhang W, Liu Y, Liu G. Free Medication for Severe Mental Illness in Rural Communities Management. Chinese J Health Psychol. 2014;22(10):1494–6. 10.13342/j.cnki.cjhp.2014.10.022. [Google Scholar]
- 57.Goff DC. The pharmacologic treatment of schizophrenia—2021. JAMA. 2021;325(2):175–6. 10.1001/jama.2020.19048. [DOI] [PubMed] [Google Scholar]
- 58.Zúñiga A, Navarro JB, Lago P, Olivas F, Muray E, Crespo M. Evaluation of needs among patients with severe mental illness. A community study. Actas Españolas de Psiquiatría. 2013;41(2):115–21. [PubMed] [Google Scholar]
- 59.Kudva KG, El Hayek S, Gupta AK, Kurokawa S, Bangshan L, Armas-Villavicencio MVC, Oishi K, Mishra S, Tiensuntisook S, Sartorius N. Stigma in mental illness: perspective from eight Asian nations. Asia Pac Psychiatry. 2020;12(2): e12380. 10.1111/appy.12380. [DOI] [PubMed] [Google Scholar]
- 60.Gaine G, Dubue J, Purdon S, Abba-Aji A. The relation between psychological need satisfaction in acute psychiatric hospital and recovery among emerging adults: a self-determination theory approach. Psychiatr Rehabil J. 2021;44(2):186–96. 10.1037/prj0000459. [DOI] [PubMed] [Google Scholar]
- 61.Bo S, Abu-Akel A, Kongerslev M, Haahr UH, Simonsen E. Risk factors for violence among patients with schizophrenia. Clin Psychol Rev. 2011;31(5):711–26. 10.1016/j.cpr.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 62.Yang C, Hou X, Ma X, Wu D. Frailty among inpatients with Schizophrenia: Status, influencing factors, and their correlation with quality of life. Front Psychiatry. 2023;13:1067260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry : Off J World Psychiatric Assoc (WPA). 2002;1(1):16–20. [PMC free article] [PubMed] [Google Scholar]
- 64.Karni-Vizer N, Salzer MS. Verbal violence experiences of adults with serious mental illnesses. Psychiatr Rehabil J. 2016;39(4):299. 10.1037/prj0000214. [DOI] [PubMed] [Google Scholar]
- 65.Varghese A, Khakha DC, Chadda RK. Pattern and type of aggressive behavior in patients with severe mental illness as perceived by the caregivers and the coping strategies used by them in a Tertiary Care Hospital. Arch Psychiatr Nurs. 2016;30(1):62–9. 10.1016/j.apnu.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 66.Wu H, Zhang W, Xu L. Factors Related with Schizophrenia Relapse and Management. Chinese Journal of Rehabilitation Theory and Practice. 2014;20(4):378–81. [Google Scholar]
- 67.National Institute for Health and Care Excellence: Guidelines. In: Psychosis and schizophrenia in adults: prevention and management. edn. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2019.; 2014. 10.1016/S2215-0366(18)30511-X.
- 68.Haddock G, Lewis S. Psychological interventions in early psychosis. Schizophr Bull. 2005;31(3):697–704. 10.1093/schbul/sbi029. [DOI] [PubMed] [Google Scholar]
- 69.Mao C, Nie L, Wang Y, Zhang Y, Shen W, Guo C. Survey analysis of influential factors of medication compliance and adverse drug reactions of home-based patients with severe mental disorders in Jinshan district of Shanghai. Chin Pharm. 2022;33(19):2373–7. 10.6039/j.issn.1001-0408.2022.19.14. [Google Scholar]
- 70.Killaspy H, Harvey C, Brasier C, Brophy L, Ennals P, Fletcher J, Hamilton B. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry. 2022;21(1):96–123. 10.1002/wps.20940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Penas P, Uriarte JJ, Gorbeña S, Slade M, Moreno-Calvete MC, Iraurgi I. Discrepancy between experience and importance of recovery components in the symptomatic and recovery perceptions of people with severe mental disorders. BMC Psychiatry. 2021;21(1):11. 10.1186/s12888-021-03287-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van der Sanden RL, Bos AE, Stutterheim SE, Pryor JB, Kok G. Experiences of stigma by association among family members of people with mental illness. Rehabil Psychol. 2013;58(1):73–80. 10.1037/a0031752. [DOI] [PubMed] [Google Scholar]
- 73.Zhou X, Li J. Meta-analysis of risk factors for high-risk behaviors in patients with severe mental disorders in Chinese communities. Chinese Journal of Prevention and Control of Chronic Non-Communicable Diseases. 2020;28(7):545–8. [Google Scholar]
- 74.Boles SM, Johnson PB. Violence among comorbid and noncomorbid severely mentally ill adults: a pilot study. Substance Abuse 2001;22(3):167-73. [DOI] [PubMed]
- 75.Westert GP, Satariano WA, Schellevis FG, Van Den Bos GA. Patterns of comorbidity and the use of health services in the Dutch population. The European Journal of Public Health. 2001;11(4):365–72. [DOI] [PubMed] [Google Scholar]
- 76.Holland KM, Jones C, Vivolo-Kantor AM, Idaikkadar N, Zwald M, Hoots B, Yard E, D’Inverno A, Swedo E, Chen MS. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiat. 2021;78(4):372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wildman EK, MacManus D, Harvey J, Kuipers E, Onwumere J. Prevalence of violence by people living with severe mental illness against their relatives and its associated impacts: a systematic review. Acta Psychiatr Scand. 2023;147(2):155–74. 10.1111/acps.13516. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.