Abstract
Background:
War and forced migration expose refugees to trauma and ongoing stress, often contributing to long-term psychological consequences. Typically, trauma exposure is assessed cumulatively; yet trauma type may better predict psychological outcomes. This study examined the differential impact of cumulative trauma and trauma subtypes (victimization, death threat, accidental/injury) on post-migration trajectories of posttraumatic stress and anxiety in refugees.
Methods:
77 Syrian (88.3%) and Iraqi (9.1%) adult refugees self-reported prior trauma exposure and psychological symptoms at time of arrival in the United States and two years post. Linear mixed-effects modeling (LMM) was performed to assess for associations between trauma variables and symptom trajectories. Models using cumulative trauma as a predictor were compared to models including the three trauma subtype variables as predictors, using pseudo-R2 values to compare variance explained between the two methods of trauma measurement.
Results:
LMM indicated that prior exposure to victimization predicted progressively worsening PTSD symptoms over time post-migration (b=.97, SE=.45, t=2.14, p=0.036). Cumulative trauma also predicted increasing PTSD symptoms (b=.124, SE=.06, t=2.09, p=0.041), but explained less variance than victimization (9% vs. 18.1%). Direct effects of cumulative trauma (p=0.009) and victimization (p=.002) on anxiety severity emerged; however, anxiety symptoms did not change over time depending on prior trauma exposure. Accidents/injuries and death threats did not predict PTSD or anxiety.
Conclusions:
These findings can be leveraged towards focused identification of those at highest risk for progressive illness post-migration, thus providing empirical guidance for allocation of interventions and resources for refugees.
Keywords: refugees, trauma, PTSD, anxiety, longitudinal
Introduction
The psychological consequences of war and forced migration contribute to a high prevalence of trauma-related disorders in people resettling as refugees (Bustamante et al., 2017; Lindert et al., 2009)—with symptoms typically remaining elevated, yet stable, or improving over time (Galatzer-Levy et al., 2018; Schock et al., 2016). Often, traumatic experiences prior to migration are conceptualized broadly as “war trauma,” and thought to drive high prevalence rates of mental health disorders; still, recent findings have indicated that psychological symptoms may be better predicted using a more fine-grained approach to assessing and classifying pre-migration trauma (Arnetz et al., 2014; Hinchey et al., 2022). Past exposure to specific trauma subtypes—or empirically classified categories of traumatic events such as victimization traumas (e.g., physical or sexual assault) or death threat traumas (e.g., exposure to a toxic substance or combat zone)—has been shown to differentially impact psychological outcomes for both resettled refugees (Arnetz et al., 2014; Haldane & Nickerson, 2016; Hinchey et al., 2022) and other populations (Contractor et al., 2020; Wamser-Nanney et al., 2018). Accordingly, understanding the impact of trauma subtypes on trajectories of mental health symptoms for refugees post-migration is crucial for prevention, early intervention, and drawing stronger conclusions regarding causation.
Differing patterns of psychological symptom progression following trauma have emerged across diverse populations. Most commonly, these include variations upon the following trajectories: resilience (i.e., few to no symptoms following trauma-exposure), recovery (i.e., clinically relevant symptoms decreasing over time), chronic (i.e., stable, high levels of symptoms over time), and delayed-onset (i.e., subclinical symptoms worsening over time to severe; (Armenta et al., 2019; Galatzer-Levy et al., 2018). Distinct symptom trajectories have been documented in relation to post-traumatic stress disorder (PTSD) in particular (Armenta et al., 2019; Galatzer-Levy et al., 2013), though similar patterns have also been observed in depression and anxiety symptoms (Armenta et al., 2019; Bachem et al., 2021; Hinchey et al., 2023).
Importantly, this indicates that an assessment at only one time-point in a refugee’s trajectory post-arrival may lack validity: early resilient and delayed-onset trajectories, for instance, would read the same (i.e., neither would meet diagnostic thresholds). Thus, a greater understanding of the predictors and risk-factors associated with discrete symptom trajectories may provide more clinically useful insight than single time-point screenings focused on binary diagnostic categorization. The ability to accurately predict an individual’s probable symptom trajectory early in resettlement would allow for a more targeted allocation of resources and support aimed towards preventing worsening outcomes. For instance, in a study of comorbid PTSD and major depressive disorder (MDD) in military service members and veterans, psychosocial correlates such as older age and lower perceived social support and were reliably predictive of chronic symptom trajectories, as compared to recovery trajectories (Armenta et al., 2019).
Certain types of trauma may also be associated with differing patterns of symptom severity over time. While cumulative trauma has been associated with consistently higher PTSD scores over time in refugees (Kaltenbach et al., 2018), little is known regarding the role of specific trauma subtypes in predicting symptom trajectories. Further, while differing symptom trajectories have been observed in refugee groups (Lamkaddem et al., 2014), the correlates of these trajectories are not well-understood. Immigration policy (Steel et al., 2011) and post-migration stressors (Kaltenbach et al., 2018) have been associated with more severe patterns of symptoms, but potential associations between trauma subtypes prior to forced migration and longitudinal symptom trajectories have not been thoroughly explored. A recent review found that “refugee/war trauma” was associated with chronic and resilient psychological symptom trajectories as compared to “military” and “civilian” traumas (Galatzer-Levy et al., 2018), providing robust support for the trajectory approach; nevertheless, “refugee/war trauma” represents a relatively non-specific classification of traumatic events. Though a broad classification is often necessary in the context of a review, findings from non-refugee populations indicate that specific types of trauma, such as assault-based traumas (Armenta et al., 2019; Sumner et al., 2021) or accidental traumas (Galatzer-Levy et al., 2018) have been differentially associated with psychological symptom trajectories.
Considering these findings, additional research is indicated—particularly for under-researched minority populations such as refugees. Substantial differences in the characteristics and correlates of symptom trajectories have emerged in prior studies (Galatzer-Levy et al., 2018; Sumner et al., 2021; Utzon-Frank et al., 2014), indicating that future investigations of these patterns may benefit from population-specific research. Indeed, prior studies of refugee mental health provide evidence that the experience of forced migration may result in unique networks of trauma-related risk-factors and outcomes, as compared to these dynamics in other populations (Javanbakht & Grasser, 2022). Historically, most trajectory research has not focused on refugees, and these groups may also face assumptions by researchers and clinicians that arrival in a presumably “safe” country will automatically engender better outcomes. Further, forced migration and resettlement itself is a unique, potentially highly stressful experience; gaining insight into trauma-related correlates of post-migration symptom trajectories may allow for early identification of newly-arriving refugees at risk for significant symptoms.
Though specific types of trauma have been explored in refugee groups, many of the trauma subtypes utilized in past investigations have been classified using factor analysis, an approach not statistically compatible with the taxonomy of traumatic events (for details regarding this incompatibility, see Contractor et al. (2020)). The recommended statistical approach for identifying categories of trauma—network analysis—has more recently been used to identify relevant subtypes of trauma within the Life Events Checklist of the DSM-5 (LEC-5), as well as link them to differing PTSD, depression, and emotion regulation outcomes (Contractor et al., 2020). These empirically classified subtypes include: victimization traumas (e.g., physical or sexual assault), death threat traumas (e.g., being threatened with a weapon, exposure to toxic substances), and accidental/injury traumas (e.g., transportation accident, non-assaultive injury). The aim of the current study was to examine the potentially differential impact of these empirically supported LEC-5 trauma subtypes on trajectories of PTSD and anxiety symptom severity post-migration. Based on prior findings, we hypothesized that cumulative trauma scores and specific trauma subtypes would be differentially associated with symptom trajectories over the study period (i.e., time of arrival in the U.S. to two years post). Specifically, we predicted that exposure to victimization trauma would predict worsening symptom trajectories over time.
Methods
Participants and Procedures
The current study population is comprised of a convenience sample of adults from Syria and Iraq, resettling as refugees in southeast Michigan between 2016–2017. All participants had experienced forced migration due to war and were part of an ongoing longitudinal study of refugee mental health (Javanbakht et al., 2019). This larger study represents a collaboration led by an academic institution and a non-profit social service agency conducting physical health screenings for newly arrived refugees. Initial screenings were held during the first month after arrival in the U.S., during which participants were offered the opportunity to join a voluntary, paid research study, introduced to the researchers by their physician, and provided with informed consent documents (n=156). Follow-up screenings included in this analysis occurred two years post-initial screenings (n=77; 79 lost to attrition) for all participants. For a detailed report of participants and procedures, see prior works (Javanbakht et al., 2019, 2020). All study procedures were carried out in accordance with the latest version of the Declaration of Helsinki and approved by the Institutional Review Board at Wayne State University—IRB #012416B3F.
Measures
All measures were administered in both Arabic and English by bilingual clinicians and research assistants. Questionnaires were translated by a native speaker from English to Arabic, back-translated by a different Arabic speaker to ensure accuracy, and approved by external review. A demographic questionnaire was used to obtain participant characteristics such as age, sex, and country of origin. Exposure to trauma was queried using the LEC-5, which prompts respondents to report level of exposure to 16 potentially traumatic events and is valid and reliable across cultures (Lima et al., 2016; Rzeszutek et al., 2018). Participants respond “yes” or “no” to whether they a) directly experienced an event, b) witnessed it, c) learned about it, or d) experienced it as part of their job. To avoid confounding interpretation of results with non-specific definitions of trauma (e.g., the context of learning about or witnessing an event may differ broadly between respondents), only directly exposure to an event was investigated (Gray et al., 2004). “Yes” responses to items related to directly experiencing an event were summed to calculate a cumulative trauma score, as well as continuous scores within each trauma subtype category (Contractor et al., 2020; see Table 1 for items in each subtype). PTSD-related symptoms were measured using the PTSD Checklist based on the DSM-IV (PCL-C) at time of arrival and DSM-5 (PCL-5; Weathers et al., 2013) two years post-resettlement. Symptom severity scores were generated by summing all items on each measure. The PCL-C and PCL-5 are valid across multiple cultures and trauma experiences (Bovin et al., 2016), and reliability in the current sample was excellent (α = .90 and α = .94, respectively). The 25-item Hopkins Symptom Checklist (HSCL-25) was used to measure severity of anxiety-related symptomatology and was administered at both time points. The first 10 items relate to anxiety symptoms, with higher mean scores indicating greater symptom severity (Hesbacher et al., 1980). The HSCL-25 is valid for refugee populations (Lavik et al., 1999), and demonstrated excellent reliability for the anxiety (Time 1: α = .86; Time 2: α = .87) subscale in this sample.
Table 1.
Participant characteristics and descriptive statistics
| Range | M | SD | |
|---|---|---|---|
|
| |||
| Age | 17–65 | 36.1 | 11.14 |
| Female, % | 53.2 | ||
| Country of origin, % | |||
| Syria | 88.3 | ||
| Iraq | 9.1 | ||
| Other | 2.6 | ||
| Ethnicity, % | |||
| Arab | 92.2 | ||
| Kurdish | 3.9 | ||
| Chaldean/Asyrian | 3.9 | ||
| Accident/Injury | 0–4 | .42 | .83 |
| Victimization | 0–1 | .08 | .27 |
| Death threat | 0–4 | .86 | 1.30 |
| Cumulative trauma | 0–8 | 1.43 | 2.02 |
| Anxiety Sxs, T1 | 1–3.6 | 1.9 | .73 |
| Anxiety Sxs, T2 | 1–3.5 | 1.67 | .58 |
| PTSD Sxsa, T1 | 0–75 | 24.77 | 18.42 |
| PTSD Sxsa, T2 | 0–73 | 23.46 | 18.1 |
Note. Ranges refer to the range of the sample, not the possible range of scores on measures (n=77). LEC-5 was used to assess trauma variables, with items included in each subtype category as follows: 1) accident/injury (items 1–4 and 12), 2) victimization (items 6, 8, and 9), and 3) death threat (items 5, 7, 10, 11, and 13–16). Abbreviations: Symptoms (Sxs); Time 1 (T1), Time 2 (T2).
. Descriptive statistics for PTSD symptoms converted PCL-4 data to PCL-5 scores based on protocol described in Moshier et al. (2019).
Statistical Analyses
Analyses were conducted in SPSS version 29.0. Descriptive statistics were examined to assess data distributions and adherence to model assumptions. Screening for data normality yielded no significant skew or kurtosis. Univariate outliers were identified using median absolute deviation (MAD) and corrected using winsorization (n = 4). Pairwise plots were generated to assess linearity, homoskedasticity, and normality of residuals, for which no assumptions were violated. Pairwise correlations were reviewed and revealed no issues of multicollinearity (r < .9 for all) nor any confounding variables. No significant differences emerged between the group that dropped out of the study and those that remained enrolled, apart from the drop-out group containing more Iraqi participants. To allow for longitudinal analysis, scale scores on the PCL-C and PCL-5 were standardized using Z-scores. Percentages of missing data were low-to-moderate (<5% for most variables; 16.9% for Time 1 anxiety; 6.5% for Time 2 anxiety) and MCAR (Little’s x2 = 69.64).
To probe potentially differential effects of cumulative trauma and trauma subtype exposure on symptom trajectories, linear mixed-effects modeling (LMM) was performed. LMM is an appropriate statistical technique for data that violate the assumption of independence, accounts for inter-individual variation of baseline symptoms, and handles missing data well, using maximum likelihood estimation (McNeish & Matta, 2018). As the analyses included only two time points, fixed slopes were used, while intercepts were allowed to vary. Data was time-structured; therefore, time was operationalized as the interval between Time 1 and Time 2. Four models were developed to examine symptom trajectories of PTSD (Model 1) and anxiety (Model 2) as outcome variables: Models 1A, 1B, 2A, and 2B. For each outcome investigated, A models test cumulative trauma score as a predictor, while B models include the three trauma subtype variables as predictors. All models were adjusted for age and sex, due to their previously documented influence (McGinty et al., 2021). Models were built using a nested approach, beginning with a null model and using Likelihood Ratio Tests (LRT) to conduct pairwise comparisons (see Tables A.1, A.2, and A.3 in Appendix). Marginal and conditional pseudo-R2 values as described by Nakagawa and Schielzeth, (2013) were used to assess variance explained in final models. In each model, time, age at Time 1, sex, and trauma variables were entered as fixed effects. To test for differences in slopes depending on trauma variable, interaction vectors were included reflecting the following format:
Time X Trauma Variable
Based on the results of LRT (see Tables A1 and A2), the resulting final LMM equations predicting PTSD and anxiety were as follows:
Results
Descriptive Statistics
Table 1 summarizes sample characteristics. The mean participant age at Time 1 was 36.1 years (SD=11.14; range = 17.7 to 65.4) and approximately half were female (53.3%; n=41). Most participants were from Syria (88.3%; n=68), with fewer reporting Iraq (9.1%; n=7) or “Other” (2.6%; n=2) for their country of origin. The average number of cumulative trauma exposures endorsed was 1.43 (SD=2.02), with 37.7% (n=29), 24.7% (n=19), and 7.8% (n=6) of participants reporting at least one death threat trauma, accident/injury trauma, and/or victimization trauma, respectively. In the current sample, the victimization trauma subtype represented physical assault only, as no sexual assault was reported. The average severity of symptoms related to PTSD (Time 1: M=24.77, SD=24.77; Time 2: M=23.46, SD=18.1) and anxiety (Time 1: M=1.9, SD=.73; Time 2: M=1.67, SD=.58) was low-to-moderate.
Trauma exposure and PTSD symptom trajectories
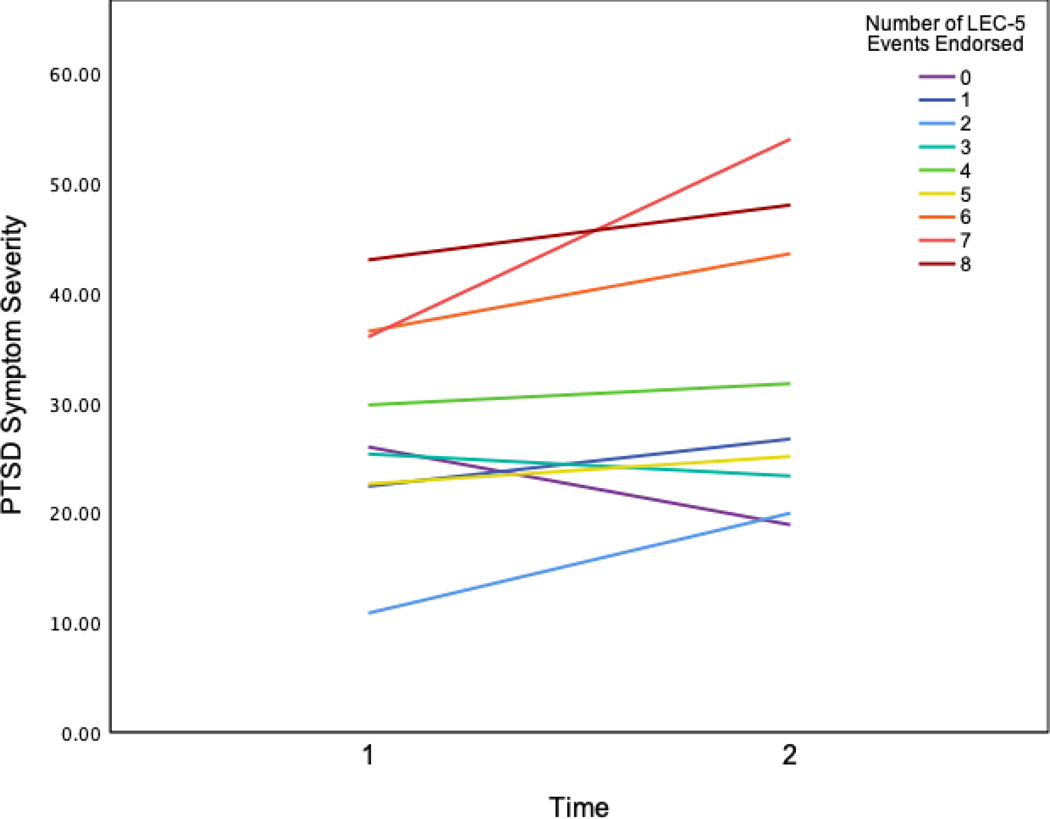
To determine whether cumulative trauma impacted changes in PTSD symptoms over time, a random-intercepts fixed-slopes LMM analysis was conducted using PTSD symptoms as the dependent variable and controlling for age and sex (Model 1A). The model revealed a significant interaction effect of time X cumulative trauma, where higher cumulative trauma scores predicted increasing PTSD symptom severity over time (b=.124, SE=.06, t=2.09, p=0.041, LLCI=.01, ULCI=.24; Table 2; Fig. 1). The marginal R2 value indicated that 9.0% of the variance was explained by fixed effects, with 43.1% of the variance explained by both fixed and random effects (conditional R2). The second LMM analysis with PTSD as the outcome variable tested for effects of the trauma subtype variables over time (Model 1B). Here, victimization was associated with a significant increase in PTSD-related symptoms over time (b=.97, SE=.45, t=2.14, p=0.036, LLCI=.07, ULCI=1.88; Table 2; Fig. 2). Death threat (p=0.082) and accident/injury-related traumas (p=0.371) were not associated with changes to PTSD symptoms. Marginal R2 indicated that 18.1% of the variance in PTSD symptoms was accounted for by fixed effects in Model 1B, with fixed and random effects explaining 47.2% of the variance.
Table 2.
Results of final linear mixed-effects models predicting PTSD symptom severity
| Est/Beta | SE | 95% CI | t | p | |
|---|---|---|---|---|---|
|
| |||||
| Cumulative Trauma Model | |||||
| Intercept | −.28 | 0.35 | −.95 − .42 | −.80 | .425 |
| Time | −.15 | 0.15 | −.45 − .14 | −1.03 | .309 |
| Female | .36 | 0.18 | −.004 − .73 | 1.97 | .052 |
| Age (Time 1) | 0.00 | 0.01 | −.02 − .02 | −.01 | .994 |
| Cumulative Trauma | .05 | 0.06 | −.06 − .16 | .84 | .400 |
| Time X Cumulative Trauma | .124 | 0.06 | .01 − .24 | 2.09 | .041* |
|
| |||||
| Trauma Subtypes Model | |||||
| Intercept | −.60 | .35 | −1.30 − .10 | −1.70 | .092 |
| Time | −.15 | .14 | −.43 − .14 | −1.04 | .300 |
| Female | .53 | .18 | .17 − .90 | 2.92 | .005* |
| Age (Time 1) | .01 | .01 | −.01 − .02 | .78 | .437 |
| Victimization | .66 | .42 | −.17 – 1.49 | 1.57 | .118 |
| Death Threat | −.07 | .10 | −.26 − .12 | −.72 | .476 |
| Accident/Injury | .15 | .14 | −.13 − .43 | 1.06 | .291 |
| Time X Victimization | .97 | .45 | .07 – 1.88 | 2.14 | .036* |
| Time X Death Threat | .18 | .10 | −.02 − .39 | 1.76 | .082 |
| Time X Accident/Injury | −.14 | .16 | −.46 − .18 | −.90 | .371 |
|
Random Effects | |||||
| Cumulative Trauma Model | Variance | SE | |||
| Residual | .535 | .09 | |||
| Intercept (Participant) | .321 | .11 | |||
|
| |||||
| Trauma Subtypes Model | |||||
| Residual | .497 | .08 | |||
| Intercept (Participant) | .274 | .10 | |||
|
Model fit | |||||
| Cumulative Trauma Model | |||||
|
| |||||
| Pseudo-R2 | Marginal | Conditional | |||
|
| |||||
| 0.090 | 0.431 | ||||
|
| |||||
| Trauma Subtypes Model | |||||
|
| |||||
| Pseudo-R2 | Marginal | Conditional | |||
|
| |||||
| 0.181 | 0.472 | ||||
Note. Abbreviations: Random effects (RE); Fixed effects (FE). Pseudo-R2 values were calculated using SPSS version 29.0 via methods described in Nakagawa & Schielzeth (2013).
p < .05
Figure 1.
Visual representation of PTSD symptoms over time at each number of total traumatic events endorsed on the LEC-5. Higher cumulative trauma scores on the LEC-5 were significantly associated with increasing PTSD symptom severity over time. Time 1 refers to time of arrival in the U.S., with Time 2 referring to two years post-arrival. Y-axis represents PTSD symptoms using PCL-5 scores. PCL-C scores at Time 1 were converted to PCL-5 scores using protocol from Moshier et al. (2019).
Figure 2.
Exposure to victimization on the LEC-5 was significantly associated with increasing PTSD symptom severity over time, as compared to those not reporting victimization. Time 1 refers to time of arrival in the U.S., with Time 2 referring to two years post-arrival. Y-axis represents PTSD symptoms using PCL-5 scores. PCL-C scores at Time 1 were converted to PCL-5 scores using protocol from Moshier et al. (2019). A cut-off score of 35 on the PCL-5 is recommended for a probable PTSD diagnosis (Mat et al., 2020).
Trauma exposure and anxiety symptom trajectories
The potential effects of trauma-related variables on anxiety symptom trajectories were also examined using LMM. The cumulative trauma model (Model 2A) revealed significant positive direct effects of cumulative trauma on anxiety (b=.11, SE=.04, t=2.66, p=0.009, LLCI=.03, ULCI=.19; see Table A.4 in Appendix), but no significant interaction effect of time X cumulative trauma (p=.262), suggesting that differences in anxiety symptoms based on cumulative trauma exposure remained consistent over time. Model 2B, the trauma subtypes LMM analysis with anxiety as the dependent variable, was subsequently tested. A significant direct effect of victimization trauma was observed (b=.89, SE=.29, t=3.12, p=.002, LLCI=.33, ULCI=1.46), though no time X trauma subtype interactions were observed. Overall, none of the trauma variables in either model was found to significantly impact trajectories of anxiety symptoms (see Table A.4 in Appendix).
Discussion
The present study assessed differential effects of cumulative trauma and various trauma subtypes on trajectories of post-migration PTSD and anxiety symptoms in Syrian and Iraqi refugees. Regarding PTSD-related symptoms, both hypotheses were supported. Specifically, higher cumulative trauma scores and exposure to victimization were associated with worsening PTSD symptoms over the two-year period, while accident/injury trauma and death threat trauma did not predict changes in PTSD-related symptoms. Results from the anxiety models, however, were contrary to hypotheses. While a positive direct effect of cumulative trauma and victimization trauma on anxiety symptom severity emerged, anxiety symptoms did not significantly change over time depending on trauma exposure. As such, these findings indicate that trauma subtype assessment may be salient in predicting longitudinal PTSD outcomes in this population, while evidence for its use in predicting anxiety trajectories was lacking.
Findings regarding the use of trauma subtype models to predict PTSD are predominately in line with prior observations. Namely, while both cumulative trauma scores and victimization trauma exposure predicted worsening PTSD symptom trajectories, the trauma subtype model explained twice the variance (18.1%) in PTSD compared to the cumulative model (9.0%). Though pseudo-R2 values for LMM must be interpreted with some caution (i.e., variance explained by the trauma subtypes model cannot be attributed only to the victimization X time effect—it reflects total variance explained by all fixed effects in the model), this statistic may indicate that trauma subtypes models possess greater explanatory power overall than cumulative trauma models. Comparable findings emerged in a cross-sectional study conducted with this cohort (Hinchey et al., 2022); the current results expand our understanding of the utility of trauma subtypes in predicting not only PTSD symptoms at one time-point, but their potential to progressively worsen post-migration based on type of prior trauma exposure. Several studies in refugee and non-refugee populations have also supported the predictive utility of trauma subtypes as compared to cumulative trauma, both cross-sectionally (Arnetz et al., 2014; Wamser-Nanney et al., 2018) and longitudinally (Armenta et al., 2019; Galatzer-Levy et al., 2018). One study, however, was contrary to these findings: results indicated that differing PTSD trajectories observed across studies were due to differences in source population, rather than type of trauma exposure (Fink et al., 2017). This group observed similar trajectories of PTSD emerging across members of the U.S. Reserve and National Guard regardless of trauma type—operationalized as either “civilian trauma exposure” (i.e., non-deployed members) or “military trauma exposure” (i.e., deployed members). Still, this discrepancy may be explained by several methodological differences. For one, civilian and military trauma are broad classifications, the taxonomy of which are not based on network or cluster analyses evidencing that these categories represent clinically relevant trauma types. Specific trauma exposures (e.g., physical assault) may have also occurred within both categories, thereby confounding results and confronting similar lack of specificity issues as refugee experiences that are defined broadly as “war trauma.” As such, the bulk of evidence to date suggests that classifying traumatic burden by migration status or cumulative trauma exposures is likely not sensitive enough; consideration of individual trauma types may improve ability to predict risk of PTSD development, as well as possible worsening.
The specific implications of these findings for early detection of long-term PTSD risk in newly arriving refugees are noteworthy. Interestingly, as illustrated in Figure 2, participants exposed to prior victimization reported subclinical levels of PTSD (Mat et al., 2020) at time of arrival in the U.S.; two years later, average PTSD symptoms in this group well-exceeded the diagnostic threshold (i.e., PCL-5 ≥ 35). This pattern emphasizes that single time-point screenings may lack validity towards predicting PTSD risk—a concern that has been documented in other studies of refugee health as well (Kaltenbach et al., 2018; Lamkaddem et al., 2014). Notably, a small sample reported victimization in this study (n = 6); results should therefore be interpreted with caution prior to replication in a larger sample. Still, the finding is corroborated by much of the extant literature.
The observed pattern of symptoms associated with victimization is most comparable with delayed onset trajectories of PTSD documented in prior literature. This trajectory typically begins with subclinical symptoms, as presently observed, which worsen over time (Utzon-Frank et al., 2014). Prior works have provided some indication that delayed PTSD trajectories may be more common in refugee populations than average: a recent meta-analysis found that delayed onset is relatively rare among those with PTSD (8.9% prevalence; Galatzer-Levy et al., 2018), while another review reported that approximately 20% of refugees with PTSD experience delayed onset (Utzon-Frank et al., 2014). Additionally, Lamkadden et al. (2014) found evidence that delayed onset PTSD is a significant contributor to the high overall prevalence of the disorder in refugees. Possibly, this is a result of the unique stressors of migration and resettlement; perhaps symptoms are inhibited due to the more pressing need to meet the demands of resettlement and are only fully expressed later. It is also possible that victimization trauma more reliably primes one’s physiology for stronger responses to later stressors (e.g., forced migration and resettlement; Sheridan & McLaughlin, 2014), thus increasing susceptibility to post-migration stress that then provokes PTSD symptoms. In other words, environmental stressors (e.g., ongoing socioeconomic stress, stress of adjustment to new environment) may exacerbate symptoms and those exposed to victimization may be more vulnerable to these environmental effects. This is in line with Galatzer-Levy and colleagues’ (2018) conclusion that delayed onset PTSD likely occurs only under specific circumstances and in the presence of additional post-event stressors. While their meta-analysis did not investigate the impact of specific types of trauma, in combination with the current findings it is possible that victimization trauma constitutes one such circumstance—which, for refugees, is often followed by additional stressors. Indeed, prior investigations of PTSD trajectories in refugees have indicated that stressful life events post-migration may cause similar increases in PTSD symptoms to having experienced another traumatic event (Schock et al., 2016). Taken together, it is plausible that some refugees (e.g., those who have experienced victimization) are more vulnerable to later stressors than others.
The unique experience of forced migration and resettlement may also explain a contrasting observation in non-refugee populations—for whom interpersonal traumas have been associated with immediately symptomatic or chronic PTSD trajectories, as opposed to delayed onset (Forbes et al., 2011; Sumner et al., 2021). Functional demands during the stress of migration may delay what would otherwise present as consistently high levels of PTSD symptoms following assault. The higher prevalence of delayed onset in veterans and first responders also supports this explanation, as these groups must also continue to function and cope with immediate demands following trauma (though in these populations, underreporting of early symptoms may also play a role; Utzon-Frank et al., 2014).
The specific significance of victimization, as compared to accident/injury- or death threat-related events—is also in line with an extensive body of literature implicating interpersonal traumas (typically defined as physical or sexual assault, and thus analogous to victimization trauma) as particularly impactful (Chen et al., 2010; Preston et al., 2021). Evidence that interpersonal trauma is reliably associated with intrapsychic factors such as high event centrality (i.e., the extent to which an event impacts one’s identity and worldview), a strong predictor of trauma-related symptoms, may partially explain this consistent impact of victimization across populations and experiences (Berntsen & Rubin, 2006; Reiland & Clark, 2017). Victimization traumas also require a more reliable proximity to and greater severity of threat, as they involve direct infliction by a perpetrator, often too closely involved both physically and psychologically. Thus, perceived and actual threat are more reliably close, severe, and potentially harmful. For instance, while exposure to war can be highly variable—from distant exposure to an explosion, to serious bodily injury—torture invariably involves direct physical and psychological threat. Moreover, actual or perceived loss of control over events and one’s safety is a central aspect of trauma and its consequences, and is, by definition, compromised in victimization traumas (Ehlers & Clark, 2000). While many studies have supported the significance of victimization/interpersonal trauma in predicting more severe psychopathological outcomes over time (Forbes et al., 2011; Preston et al., 2021; Steenkamp et al., 2012), the finding that prior victimization predicts actual worsening of post-migration PTSD symptomatology over time in a refugee population is novel. One study in unaccompanied refugee minors corroborated delayed onset PTSD as a clinically relevant outcome for refugee youth; however, types of trauma correlated with this trajectory were not examined (Smid et al., 2011). Still, as only a small sample reported victimization in this analysis (n=6), future studies are needed to assess the generalizability of victimization as a marker of eventual PTSD risk—despite an initial presentation of subclinical symptoms.
Taken together, the existing findings have broad significance for the taxonomy of trauma and of PTSD: a presence/absence approach to PTSD and single time-point assessment is likely flawed regardless of population. The current body of evidence corroborates claims that reliance on diagnostic categories alone may lack validity when defining and assessing PTSD in research (Galatzer-Levy et al., 2018). Greater focus on longitudinal studies and heterogeneity of PTSD—for instance, by considering type of trauma exposure—may aid in identifying functional phenotypes of PTSD, accurately predicting risk, and investigating whether specific treatments are more effective for certain subclassifications of PTSD, thereby preventing development or exacerbation of disease.
The current findings are also relevant in guiding treatment and prevention. Despite being in a presumably safer location post-migration, exposure to certain types of trauma and cumulative traumas resulted in a worsening of PTSD symptoms for this group. Particularly given the growing discrepancy between mental health need and available services, the ability to accurately identify those at risk of progressive illness is crucial in focusing prevention and early intervention efforts. Practitioners’ ability to allocate resources and services towards those with the greatest need may contribute to lessening the gap in mental health care. Additionally, as refugees may remain transitory even after migration, providing focused screenings and available treatment upon arrival and prior to worsening of symptoms may allow for intervention before post-migratory factors necessitate patients’ relocation. Early identification of likely PTSD trajectory may also guide specific treatments: there is evidence that some interventions (e.g., CBT) are effective for certain PTSD trajectories and not others (Galatzer-Levy & Bryant, 2013). Future research is necessary to improve our understanding of the predictive correlates of various PTSD trajectories, as well as the related efficacy of certain interventions.
This study found evidence for correlates of heterogeneous PTSD outcomes following the experience of forced migration. The discussed approaches to screening and intervention would be further strengthened by biological data that could elucidate whether biomarkers of PTSD symptomatology are parallel to these findings. For instance, differing biomarker profiles may present in those exposed to victimization compared to those not exposed. Further neuroimaging and biological research in refugees and other trauma exposed populations is needed and would aid in the identification of relevant, treatment-guiding phenotypes of PTSD (Javanbakht & Grasser, 2022).
Our findings must be interpreted considering several limitations. As discussed, the sample size for victimization was small (7.8%). Though this is in line with the average 8–10% of trauma-exposed individuals who typically develop PTSD (Benjet et al., 2016)—and the particular impact of victimization/interpersonal trauma as compared to other trauma types has been extensively documented in prior literature (Chen et al., 2010; Forbes et al., 2011)—the current findings must be considered preliminary; further research is necessary to confirm these relations. As the current sample was primarily from Syria, it is also possible that results may not be generalizable to refugees from other countries of origin. Additionally, post-migration challenges faced by refugees often necessitate non-probability sampling, limit participant availability for multiple time-point data collection, and contribute to attrition (Hinchey et al., 2023). Generalizability is therefore also limited by potential bias introduced by study attrition or self-selection of refugees into the host country. Future studies with internally displaced populations or refugees prior to arrival in host countries would assist in addressing this bias. Further, data from only two time points across a two-year interval is limited in its ability to describe symptom change over time; conclusions should be considered preliminary and investigated further using multiple time points with shorter intervals. Additionally, the overall symptom levels in our sample were low-to-moderate; however, as the study was not focused on only those meeting diagnostic thresholds, the findings may have broader relevance for refugee groups in general, regardless of diagnostic status. This continuous approach to operationalizing symptoms is also better powered for a small sample size and in line with RDoC recommendations for researching neurobehavioral functioning and disease development. Additionally, as discussed, symptoms that are subclinical at one time point may not remain so. Another limitation involves the self-report nature of data collection. Inaccurate recall and under-reporting—especially of trauma-related variables—may introduce additional measurement error when relying on self-reports. Future studies should utilize multiple classes of variables, including biological data, to extend this work.
Conclusion
The current findings emphasize the need for assessment that considers type of trauma exposure in refugee populations, rather than assuming equivalence of experiences due to migration status. Experiencing victimization specifically emerged as a possible risk factor for progressively worsening post-migration PTSD—a pattern which also highlighted the importance of trajectory-based research when defining and investigating trauma and trauma-related disorders. Future research can expand upon these findings by moving past detection of risk and investigating treatment efficacy for various trauma exposures and PTSD trajectories in refugees. As the need for trauma-informed care is only growing, the ability to accurately identify those at highest risk—perhaps prior to development of symptoms meeting diagnostic thresholds for PTSD—is crucial to meeting mental health care needs.
Clinical Impact Statement:
These findings provide valuable preliminary insights into early indicators of risk for posttraumatic stress disorder (PTSD) in an underrepresented population in scientific research—people of Middle Eastern descent resettling as refugees. Compared to other types of trauma, exposure to victimization (i.e., assault-related) events predicted worsening PTSD symptoms during the first two years of resettlement. Cumulative trauma exposure also predicted worsening PTSD, though not as efficiently as victimization history. These findings can be leveraged to improve early identification of those at high risk for progressive illness, perhaps via trauma screenings upon arrival in a host country.
Acknowledgments:
The authors would like to thank all the participants who engaged in this research, contributed their data, and shared their stories. The authors would also like to thank Lana Grasser, Tarek Almasaddi, Heba Al-Saghir, Mohammed Alsaud, Michael Kabbash, Suzanne Manji, Luna Nasry, Dalya Saleem, Safa Sankari, Rajaa Shoukfeh, Celine Bazzi, and Samantha Sonderman for their assistance with data collection and data entry. Many thanks as well to Dr. Alireza Amirsadri and Dr. Luay Haddad. Finally, thank you to the organizations and institutions who have provided financial support for this research—including the State of Michigan Lycaki/Young Foundation and the Department of Psychiatry and Behavioral Neuroscience. Dr. Javanbakht’s effort is supported by R01HD099178 (PI: Javanbakht).
Funding
This work was supported by the National Institute of Health (grant number R01HD099178; PI: Arash Javanbakht). The funding sources had no involvement in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Data Availability
Wayne State University requires data use agreements to be drafted and approved prior to any data sharing. If investigators are interested in accessing data, agreements will need to be drafted and approved between institutions and investigators in order to protect these data. Therefore, data cannot be made publicly available at this time, however, data can be made available by request to the authors and institutional approval with an appropriate data use agreement.
Appendix A
Table A.1.
Model comparison and model building process for PTSD
| Sampling Units | N total observations = 149 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N subjects = 77 | ||||||||||
|
| ||||||||||
| Model Specification | Model Name | Nested Model | Fixed Effects | Random Effects | Model fit | LRT Test against nested | ||||
|
| ||||||||||
| AIC | BIC | −2 LL | df | df | X2 | |||||
|
| ||||||||||
| RE only | Null | - | - | intercepts | 407.2 | 416.2 | 401.2 | 3 | - | - |
|
| ||||||||||
| FE main effect | Model 1 | Null | Time | intercepts | 409.1 | 425.2 | 401.1 | 4 | 1 | .1 |
|
| ||||||||||
| FE two-way interactions – cumulative trauma | Model 2 | Model 1 | Time + Age + Gender + Cumulative Trauma + Cumulative Trauma x Time | intercepts | 404.8 | 428.8 | 388.8 | 8 | 8 | 12.3* |
|
| ||||||||||
| FE two-way interactions – trauma subtypes | Model 3 | Model 1 | Time + Age + Gender + Victimization + Death Threat + Accident/Injury + Victimization x Time + Death Threat x Time + Accident/Injury x Time | intercepts | 398.4 | 434.4 | 374.4 | 12 | 8 | 26.7* |
Note. The PTSD variable is operationalized as standardized (Z) scores on the PCL for DSM IV at Time 1 and PCL-5 at Time 2, to allow for comparison across time. Abbreviations: Random effects (RE); Fixed effects (FE); Akaike’s Information Criterion (AIC); Schwarz’s Bayesian Criterion (BIC); −2 Log Likelihood (−2 LL); Likelihood ratio test (LRT)
Table A.2.
Model comparison and model building process for anxiety
| Sampling Units | N total observations = 149 N subjects = 77 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Model Specification | Model Name | Nested Model | Fixed Effects | Random Effects | Model fit | LRT Test against nested | ||||
|
| ||||||||||
| AIC | BIC | −2 LL | df | df | X2 | |||||
|
| ||||||||||
| RE only | Null | - | - | intercepts | 267.2 | 276.0 | 261.2 | 3 | - | - |
|
| ||||||||||
| FE main effect | Model 1 | Null | Time | intercepts | 262.9 | 274.5 | 254.9 | 4 | 1 | 6.3* |
|
| ||||||||||
| FE two-way interactions – cumulative trauma | Model 2 | Model 1 | Time + Age + Gender + Cumulative Trauma + Cumulative Trauma x Time | intercepts | 257.1 | 280.4 | 241.1 | 8 | 4 | 13.8* |
|
| ||||||||||
| FE two-way interactions – trauma subtypes | Model 3 | Model 1 | Time + Age + Gender + Victimization + Death Threat + Accident/Injury + Victimization x Time + Death Threat x Time + Accident/Injury x Time | intercepts | 248.2 | 283.2 | 224.2 | 12 | 8 | 30.7* |
Note. Abbreviations: Random effects (RE); Fixed effects (FE); Akaike’s Information Criterion (AIC); Schwarz’s Bayesian Criterion (BIC); −2 Log Likelihood (−2 LL); Likelihood ratio test (LRT)
Table A.3.
Model comparison and model building process for depression
| Sampling Units | N total observations = 149 N subjects = 77 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Model Specification | Model Name | Nested Model | Fixed Effects | Random Effects | Model fit | LRT Test against nested | ||||
|
| ||||||||||
| AIC | BIC | −2 LL | df | df | X2 | |||||
|
| ||||||||||
| RE only | Null | - | - | intercepts | 262.2 | 270.9 | 256.2 | 3 | - | - |
|
| ||||||||||
| FE main effects | Model 1 | Null | Time | intercepts | 256.9 | 268.5 | 248.9 | 4 | 1 | 7.3* |
|
| ||||||||||
| FE two-way interactions – cumulative trauma | Model 2 | Model 1 | Time + Age + Gender + Cumulative Trauma + Cumulative Trauma x Time | intercepts | 257.8 | 281.1 | 241.8 | 8 | 4 | 7.1 |
|
| ||||||||||
| FE two-way interactions – trauma subtypes | Model 3 | Model 1 | Time + Age + Gender + Victimization + Death Threat + Accident/Injury + Victimization x Time + Death Threat x Time + Accident/Injury x Time | intercepts | 251.5 | 286.4 | 227.5 | 12 | 8 | 21.4* |
Note. Abbreviations: Random effects (RE); Fixed effects (FE); Akaike’s Information Criterion (AIC); Schwarz’s Bayesian Criterion (BIC); −2 Log Likelihood (−2 LL); Likelihood ratio test (LRT)
Table A.4.
Results of final linear mixed-effects models predicting anxiety symptom severity
| Fixed Effects | |||||
|---|---|---|---|---|---|
| Est/Beta | SE | 95% CI | t | p | |
|
| |||||
| Cumulative Trauma Model | |||||
| Intercept | 1.33 | 0.24 | .86 – 1.80 | 5.60 | <.001* |
| Time | −.17 | 0.10 | −.37 − .04 | −1.64 | .107 |
| Female | .27 | 0.12 | .03 − .52 | 2.20 | .031* |
| Age (Time 1) | 0.01 | 0.01 | −.004 − .02 | 1.38 | .173 |
| Cumulative Trauma |
.11 | 0.04 | .03 − .19 | 2.66 | .009* |
| Time X Cumulative Trauma | −.05 | 0.04 | −.13 − .04 | −1.13 | .262 |
|
Trauma Subtypes Model | |||||
| Intercept | 1.13 | .23 | .68 – 1.58 | 5.00 | <.001* |
| Time | −.18 | .10 | −.38 − .02 | −1.76 | .083 |
| Female | .42 | .12 | .19 − .65 | 3.59 | <.001* |
| Age (Time 1) | .01 | .01 | .001 − .02 | 2.11 | .039* |
| Victimization | .89 | .29 | .33 − 1.46 | 3.12 | .002* |
| Death Threat | .07 | .07 | −.06 − .20 | 1.12 | .266 |
| Accident/Injury | .03 | .10 | −.17 − .22 | .27 | .785 |
| Time X Victimization | .12 | .33 | −.54 − .77 | .35 | .726 |
| Time X Death Threat | −.01 | .07 | −.16 − .14 | −.16 | .877 |
| Time X Accident/Injury | −.15 | .12 | −.38 − .08 | −1.27 | .209 |
|
Random Effects | |||||
| Cumulative Trauma Model | Variance | SE | |||
| Residual | .230 | .04 | |||
| Intercept (Participant) | .138 | .05 | |||
|
Trauma Subtypes Model | |||||
| Residual | .229 | .04 | |||
| Intercept (Participant) | .087 | .05 | |||
|
Model fit | |||||
| Cumulative Trauma Model | |||||
|
| |||||
| Pseudo-R2 | Marginal | Conditional | |||
|
| |||||
| 0.152 | 0.470 | ||||
|
| |||||
| Trauma Subtypes Model | |||||
|
| |||||
| Pseudo-R2 | Marginal | Conditional | |||
|
| |||||
| 0.280 | 0.477 | ||||
Note. Abbreviations: Random effects (RE); Fixed effects (FE)
Footnotes
Declarations
Consent to Participate
Participants were given the opportunity to join a paid, voluntary research study during health screenings at primary care clinics during their first month of resettlement. Interested parties were introduced to the research group by their physician and provided with informed consent documents. All participants included in this analysis provided informed consent prior to any study procedures.
Competing Interests
The authors have no financial disclosures nor conflicts of interest to report.
Ethics Approval
All study procedures were carried out in accordance with the latest version of the Declaration of Helsinki and approved by the Institutional Review Board at Wayne State University—IRB #012416B3F.
References
- Armenta RF, Walter KH, Geronimo-Hara TR, Porter B, Stander VA, LeardMann CA, Bauer L, Boparai S, Bukowinski A, Carballo C, Carey F, Davies J, Esquivel A, Gumbs G, Jacobson I, Khodr Z, Kolaja C, Lee W, Lynch G, … for the Millennium Cohort Study Team. (2019). Longitudinal trajectories of comorbid PTSD and depression symptoms among U.S. service members and veterans. BMC Psychiatry, 19(1), 396. 10.1186/s12888-019-2375-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnetz BB, Broadbridge CL, Jamil H, Lumley MA, Pole N, Barkho E, Fakhouri M, Talia YR, & Arnetz JE. (2014). Specific Trauma Subtypes Improve the Predictive Validity of the Harvard Trauma Questionnaire in Iraqi Refugees. Journal of Immigrant and Minority Health, 16(6), 1055–1061. 10.1007/s10903-014-9995-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachem R, Zhou X, Levin Y, & Solomon Z. (2021). Trajectories of depression in aging veterans and former prisoners-of-war: The role of social support and hardiness. Journal of Clinical Psychology, 77(10), 2203–2215. 10.1002/jclp.23168 [DOI] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Shahly V, Stein DJ, Petukhova M, Hill E, Alonso J, Atwoli L, Bunting B, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Gureje O, Huang Y, … Koenen KC. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, & Rubin DC. (2006). The centrality of event scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behaviour Research and Therapy, 44(2), 219–231. 10.1016/j.brat.2005.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bustamante LHU, Cerqueira RO, Leclerc E, & Brietzke E. (2017). Stress, trauma, and posttraumatic stress disorder in migrants: A comprehensive review. Brazilian Journal of Psychiatry, 0. 10.1590/1516-4446-2017-2290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, Elamin MB, Seime RJ, Shinozaki G, Prokop LJ, & Zirakzadeh A. (2010). Sexual Abuse and Lifetime Diagnosis of Psychiatric Disorders: Systematic Review and Meta-analysis. Mayo Clinic Proceedings, 85(7), 618–629. 10.4065/mcp.2009.0583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Natesan Batley P, & Elhai JD. (2020). Clusters of trauma types as measured by the Life Events Checklist for DSM–5. International Journal of Stress Management, 27(4), 380–393. 10.1037/str0000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Fink DS, Lowe S, Cohen GH, Sampson LA, Ursano RJ, Gifford RK, Fullerton CS, & Galea S. (2017). Trajectories of posttraumatic stress symptoms after civilian or deployment traumatic event experiences. Psychological Trauma: Theory, Research, Practice, and Policy, 9(2), 138–146. 10.1037/tra0000147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Parslow R, Phelps A, O†Donnell M, Bryant RA, McFarlane A, Silove D, & Creamer M. (2011). Trauma at the Hands of Another: Longitudinal Study of Differences in the Posttraumatic Stress Disorder Symptom Profile Following Interpersonal Compared With Noninterpersonal Trauma. The Journal of Clinical Psychiatry, 72(3), 21208. 10.4088/JCP.10m06640 [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Ankri Y, Freedman S, Israeli-Shalev Y, Roitman P, Gilad M, & Shalev AY. (2013). Early PTSD Symptom Trajectories: Persistence, Recovery, and Response to Treatment: Results from the Jerusalem Trauma Outreach and Prevention Study (J-TOPS). PLoS ONE, 8(8), e70084. 10.1371/journal.pone.0070084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, & Bryant RA. (2013). 636,120 Ways to Have Posttraumatic Stress Disorder. Perspectives on Psychological Science, 8(6), 651–662. 10.1177/1745691613504115 [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA. (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. 10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW. (2004). Psychometric Properties of the Life Events Checklist. Assessment, 11(4), 330–341. 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Haldane J, & Nickerson A. (2016). The impact of interpersonal and noninterpersonal trauma on psychological symptoms in refugees: The moderating role of gender and trauma type. Journal of Traumatic Stress, 29(5), 457–465. 10.1002/jts.22132 [DOI] [PubMed] [Google Scholar]
- Hesbacher PT, Rickels K, Morris RJ, Newman H, & Rosenfeld H. (1980). Psychiatric illness in family practice. The Journal of Clinical Psychiatry, 41(1), 6–10. [PubMed] [Google Scholar]
- Hinchey LME, Grasser LR, Saad B, Gorski K, Pernice F, & Javanbakht A. (2022). The Predictive Utility of Trauma Subtypes in the Assessment of Mental Health Outcomes for Persons Resettled as Refugees. Journal of Immigrant and Minority Health. 10.1007/s10903-022-01407-8 [DOI] [PMC free article] [PubMed]
- Hinchey LME, Khalil D, & Javanbakht A. (2023). Practical approaches to conducting biopsychosocial research with refugee and internally displaced communities. Comprehensive Psychoneuroendocrinology, 16, 100217. 10.1016/j.cpnec.2023.100217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinchey LM-E, Nashef R, Bazzi C, Gorski K, & Javanbakht A. (2023). The longitudinal impact of war exposure on psychopathology in Syrian and Iraqi refugee youth. International Journal of Social Psychiatry. 10.1177/00207640231177829 [DOI] [PubMed]
- Javanbakht A, Amirsadri A, Abu Suhaiban H, Alsaud MI, Alobaidi Z, Rawi Z, & Arfken CL. (2019). Prevalence of Possible Mental Disorders in Syrian Refugees Resettling in the United States Screened at Primary Care. Journal of Immigrant and Minority Health, 21(3), 664–667. 10.1007/s10903-018-0797-3 [DOI] [PubMed] [Google Scholar]
- Javanbakht A, & Grasser LR. (2022). Biological Psychiatry in Displaced Populations: What We Know, and What We Need to Begin to Learn. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, S2451902222001173. 10.1016/j.bpsc.2022.05.001 [DOI] [PMC free article] [PubMed]
- Javanbakht A, Grasser LR, Kim S, Arfken CL, & Nugent N. (2020). Perceived health, adversity, and posttraumatic stress disorder in Syrian and Iraqi refugees. International Journal of Social Psychiatry, 0020764020978274. 10.1177/0020764020978274 [DOI] [PMC free article] [PubMed]
- Kaltenbach E, Schauer M, Hermenau K, Elbert T, & Schalinski I. (2018). Course of Mental Health in Refugees—A One Year Panel Survey. Frontiers in Psychiatry, 9. https://www.frontiersin.org/article/10.3389/fpsyt.2018.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamkaddem M, Stronks K, Devillé WD, Olff M, Gerritsen AA, & Essink-Bot M-L. (2014). Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry, 14(1), 90. 10.1186/1471-244X-14-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavik NJ, Laake P, Hauff E, & Solberg Ø. (1999). The use of self-reports in psychiatric studies of traumatized refugees: Validation and analysis of HSCL-25. Nordic Journal of Psychiatry, 53(1), 17–20. 10.1080/080394899426666 [DOI] [Google Scholar]
- Lima E. de P., Vasconcelos AG, Berger W, Kristensen CH, Nascimento E. do, Figueira I, Mendlowicz MV. (2016). Cross-cultural adaptation of the Posttraumatic Stress Disorder Checklist 5 (PCL-5) and Life Events Checklist 5 (LEC-5) for the Brazilian context. Trends in Psychiatry and Psychotherapy, 38(4), 207–215. 10.1590/2237-6089-2015-0074 [DOI] [PubMed] [Google Scholar]
- Lindert J, Ehrenstein O. S. von, Priebe S, Mielck A, & Brähler E. (2009). Depression and anxiety in labor migrants and refugees – A systematic review and meta-analysis. Social Science & Medicine, 69(2), 246–257. 10.1016/j.socscimed.2009.04.032 [DOI] [PubMed] [Google Scholar]
- Mat SMN, Ismail H, & Mohd YH. (2020). Reliability and validity of a post-traumatic checklist-5 (PCL-5) among fire and rescue officers in Selangor, Malaysia. Journal of Health Research, 35(4), 379–387. 10.1108/JHR-11-2019-0243 [DOI] [Google Scholar]
- McGinty G, Fox R, Ben-Ezra M, Cloitre M, Karatzias T, Shevlin M, & Hyland P. (2021). Sex and age differences in ICD-11 PTSD and complex PTSD: An analysis of four general population samples. European Psychiatry, 64(1), e66. 10.1192/j.eurpsy.2021.2239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish D, & Matta T. (2018). Differentiating between mixed-effects and latent-curve approaches to growth modeling. Behavior Research Methods, 50(4), 1398–1414. 10.3758/s13428-017-0976-5 [DOI] [PubMed] [Google Scholar]
- Moshier SJ, Lee DJ, Bovin MJ, Gauthier G, Zax A, Rosen RC, Keane TM, & Marx BP. (2019). An Empirical Crosswalk for the PTSD Checklist: Translating DSM-IV to DSM-5 Using a Veteran Sample. Journal of Traumatic Stress, 32(5), 799–805. 10.1002/jts.22438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S, & Schielzeth H. (2013). A general and simple method for obtaining R2 from generalized linear mixed-effects models. Methods in Ecology and Evolution, 4(2), 133–142. 10.1111/j.2041-210x.2012.00261.x [DOI] [Google Scholar]
- Preston TJ, Gorday JY, Bedford CE, Mathes BM, & Schmidt NB. (2021). A longitudinal investigation of trauma-specific rumination and PTSD symptoms: The moderating role of interpersonal trauma experience. Journal of Affective Disorders, 292, 142–148. 10.1016/j.jad.2021.05.049 [DOI] [PubMed] [Google Scholar]
- Reiland SA, & Clark CB. (2017). Relationship between event type and mental health outcomes: Event centrality as mediator. Personality and Individual Differences, 114, 155–159. 10.1016/j.paid.2017.04.009 [DOI] [Google Scholar]
- Rzeszutek M, Lis-Turlejska M, Palich H, & Szumiał S. (2018). The Polish adaptation of the Life Events Checklist (LEC-5) for PTSD criteria from DSM-5. Psychiatria Polska, 52(3), 499–510. 10.12740/PP/OnlineFirst/69218 [DOI] [PubMed] [Google Scholar]
- Schock K, Böttche M, Rosner R, Wenk-Ansohn M, & Knaevelsrud C. (2016). Impact of new traumatic or stressful life events on pre-existing PTSD in traumatized refugees: Results of a longitudinal study. European Journal of Psychotraumatology, 7. 10.3402/ejpt.v7.32106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan MA, & McLaughlin KA. (2014). Dimensions of early experience and neural development: Deprivation and threat. Trends in Cognitive Sciences, 18(11), 580–585. 10.1016/j.tics.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smid GE, Lensvelt-Mulders GJLM, Knipscheer JW, Gersons BPR, & Kleber RJ. (2011). Late-Onset PTSD in Unaccompanied Refugee Minors: Exploring the Predictive Utility of Depression and Anxiety Symptoms. Journal of Clinical Child & Adolescent Psychology, 40(5), 742–755. 10.1080/15374416.2011.597083 [DOI] [PubMed] [Google Scholar]
- Steel Z, Momartin S, Silove D, Coello M, Aroche J, & Tay KW. (2011). Two year psychosocial and mental health outcomes for refugees subjected to restrictive or supportive immigration policies. Social Science & Medicine, 72(7), 1149–1156. 10.1016/j.socscimed.2011.02.007 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Dickstein BD, Salters‐Pedneault K, Hofmann SG, & Litz BT. (2012). Trajectories of PTSD symptoms following sexual assault: Is resilience the modal outcome? Journal of Traumatic Stress, 25(4), 469–474. 10.1002/jts.21718 [DOI] [PubMed] [Google Scholar]
- Sumner JA, Rünger D, Robles TF, Lowe SR, Elashoff D, & Shetty V. (2021). Understanding trajectories of underlying dimensions of posttraumatic psychopathology. Journal of Affective Disorders, 284, 75–84. 10.1016/j.jad.2021.01.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utzon-Frank N, Breinegaard N, Bertelsen M, Borritz M, Eller NH, Nordentott M, Olesen K, Rod NH, Rugulies R, & Bonde JP. (2014). Occurrence of delayed-onset post-traumatic stress disorder: A systematic review and meta-analysis of prospective studies. Scandinavian Journal of Work, Environment & Health, 40(3), 215–229. [DOI] [PubMed] [Google Scholar]
- Wamser-Nanney R, Howell KH, Schwartz LE, & Hasselle AJ. (2018). The moderating role of trauma type on the relationship between event centrality of the traumatic experience and mental health outcomes. Psychological Trauma: Theory, Research, Practice, and Policy, 10(5), 499–507. 10.1037/tra0000344 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz B, Keane TM, Palmieri P, Marx B, & Schnurr P. (2013). The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD at www.ptsd.va.gov, 10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Wayne State University requires data use agreements to be drafted and approved prior to any data sharing. If investigators are interested in accessing data, agreements will need to be drafted and approved between institutions and investigators in order to protect these data. Therefore, data cannot be made publicly available at this time, however, data can be made available by request to the authors and institutional approval with an appropriate data use agreement.