Plain Language Summary
We describe the treatment of a patient recovering after reconstruction surgery for brachial plexus injury (BPI), which causes damage to the nerves of the arm. We used 3D motion capture to create a 3D “map” of the patient’s reachable workspace—that is, how far the patient could reach within his own environment as a measure of how well his arm functioned—and tracked changes over a 2-year period. We also describe the patient’s self-reported outcomes and compare them to the workspace measurement.
Keywords: brachial plexus injury, rehabilitation, nerve repair, patient-reported outcomes
Introduction
Adult traumatic brachial plexus injuries (BPIs) often result in reduced functional use of the upper extremity. For patients who do not recover neurologic function spontaneously, brachial plexus reconstruction can facilitate recovery of upper extremity function [12,14]. The physiologic limitations of nerve regeneration lead to an extended timeline to see improvement in function, which can be frustrating to patients while they await recovery [1,3,8]. Current methods to assess recovery are typically centered on clinician grading of manual muscle testing [5,7], which is limited in accuracy and reliability and does not reflect function. Patient-reported outcome measures (PROMs) are increasingly used in evaluation of patients with BPI, but it would be ideal to have a complementary outcome measure that is objective, reliable, and reflective of function.
Three-dimensional (3D) motion capture has been developed over the past several years for applications spanning physical therapy [6,13,15], digital goniometry [6,13,15], and even non-medical purposes in films. 3D motion capture methods use reflective markers placed at several points on the body and a multi-camera system to track motion in real-time.
Along with quantifying movement, motion capture during functional tasks can calculate a “reachable workspace” for patients. This idea was explored in other musculoskeletal disorders such as Duchenne’s uscular dystrophy [2] and amyotrophic lateral sclerosis [9] using a Kinect sensor. Richardson et al [10] utilized this technique to describe how much of their surrounding environment children with BPI can reach, termed as a workspace.
We report on an adult patient with BPI with whom 3D motion capture technology was used to track humerothoracic motion during 4 functional tasks and thereby determine an upper limb reachable workspace. We also assessed how those objective measures related to PROMs longitudinally at multiple time points after BPI reconstruction.
Case Report
This report was prepared using the CARE checklist. Following approval from our institutional review board and obtaining informed consent, one pilot patient with unilateral traumatic BPI, a 44-year-old man, completed the study protocol 5 times at 6-month intervals: 0 months, 6 months, 12 months, 18 months, and 24 months. The patient (Table 1) had an upper trunk injury and was treated with distal nerve transfers (to restore shoulder abduction and elbow flexion) 14 months prior to his first workspace assessment. This initial assessment was taken at the beginning of the patient’s meaningful recovery, which was then tracked over a 2-year course.
Table 1.
Patient information for research participant.
| BPI-01 Demographics | Sex: M, Age: 44 | Type of BPI: C5-6 postganglionic injury caused by laceration proximal to upper trunk-division trifurcation, treated with distal nerve transfers (double Oberlin and triceps to axillary) to restore shoulder abduction and elbow flexion. Initial measurement is 14 months postoperative. | ||||
|---|---|---|---|---|---|---|
| Race: White, Non-Hispanic | ||||||
| BPI-01 Metrics | Time | 0 | 6 | 12 | 18 | 24 |
| Calculated Workspaces (Anterior, Injured side—Fraction of Healthy) | Superior | 0.17 | 0.28 | 0.45 | 0.60 | 0.71 |
| Inferior | 0.73 | 0.78 | 0.78 | 0.79 | 0.77 | |
| 3D Motion Capture Data Maximum Range of Motion (Degrees) | Shoulder forward flexion | 75.93 | 87.9 | 98.12 | 121.44 | 138.17 |
| Shoulder abduction | 31.4 | 45.34 | 49.18 | 73.88 | 79.33 | |
| Shoulder external rotation | 8.9 | 7.6 | 7.65 | 7.7 | 4.5 | |
| Elbow flexion | 94.22 | 109.84 | 96.91 | 96.36 | 63.72 | |
| Patient-Reported Outcome Measures (Scale Varies Depending on specific PRO) | PROMIS depression | 41.7 | 38.9 | 38.9 | 41.7 | 34.2 |
| PROMIS pain interference | 53.9 | 52.6 | 50.5 | 46.5 | 52.2 | |
| PROMIS anxiety | 44 | 42.9 | 52.1 | 43.3 | 46.6 | |
| Impact of BPI post injury | 37.25 | 14.8 | 25.1 | 24.8 | 27.2 | |
| SF-36 Sum | 583 | 720 | 625.5 | 499.5 | 680.5 | |
| DASH | 31.6 | 38.6 | 45.8 | 30.8 | 11.7 | |
| Surgeon-Graded MRC (1-5 Scale) | Shoulder abduction | 2 | 2 | 2 | 3 | 3 |
| Shoulder external rotation | 2 | - | 2 | 3 | 3 | |
| Elbow flexion | 4 | - | 4 | 5 | 5 | |
Thirty-seven retro-reflective skin markers were placed according to the established Vicon Upper Limb Kinematics Model [4]. With these markers on, the participant followed a protocol of several tasks including shoulder flexion, abduction, external rotation, and elbow flexion on both the injured and healthy arms [4]. A minimum of 3 trials per task were recorded for each arm. A 10-camera motion capture system (Vantage 5, Vicon Inc.) recorded the patient’s motions at 100 Hz. Data collection took 20 minutes (marker placement taking 10 minutes and the tasks taking 10 minutes).
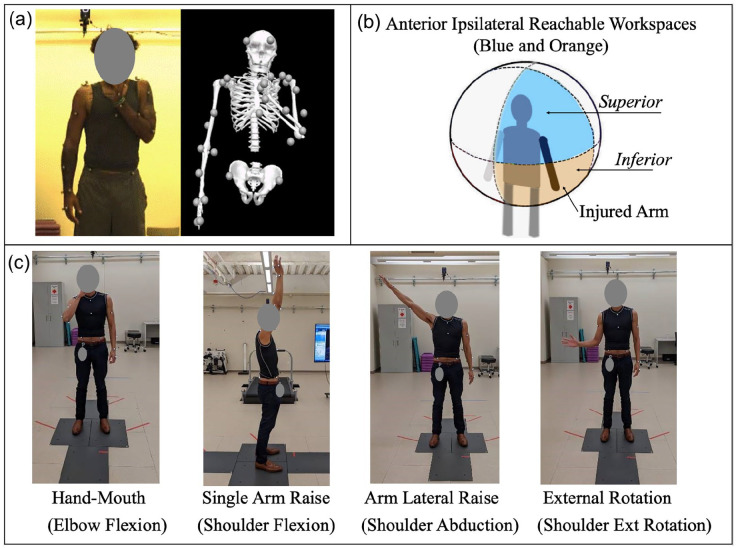
Skin marker trajectories were labeled in Vicon Nexus software and imported to Visual3D software for calculation of joint angles. In Visual3D, a 9-segment model was created including the hands, forearms, upper arms, trunk, pelvis, and head (Fig. 1a). Marker trajectories were filtered with a fourth order low-pass Butterworth filter at 6Hz and then used to drive the motion of the model segments. Segment coordinate systems were established and the following angles were calculated via inverse kinematics: maximum shoulder abduction (measured as the upper arm relative to the trunk in the coronal plane), maximum shoulder flexion (upper arm relative to trunk in sagittal plane), maximum shoulder external rotation (measured by upper arm rotation relative to the trunk in transverse plane), and elbow flexion (measured by forearm segment relative to upper arm in sagittal plane). Joint angles from the 3 trials on each arm were averaged to represent the motion of that patient and arm.
Fig. 1.
(a) Example of in-software motion tracking. (b) Representation of Superior and Inferior Anterior Injured Arm Workspace. (c) 4 movements measured to calculate workspace.
A theoretical reachable workspace was created as a sphere-like space centered at the pelvis of the subject and extending bilaterally to the furthest distance superior, anterior, and lateral that a subject could reach with their healthy arm during the shoulder flexion and abduction tasks (Fig. 1c). The workspace was further divided into superior and inferior halves at the level of the subject’s waist, defined by markers placed on the anterior superior iliac spines of the pelvis (Fig. 1b) [4] in accordance with established definitions. For each subject, the size of the reachable workspace was calculated as a weighted average of the 4 functional tasks (see equation below). A subject’s workspace on the injured arm was calculated as the percent of reachable workspace they were able to access. For example, if a patient was able to flex and abduct their shoulder above their waist to the same maximum degrees in both their injured and their healthy arms, they were said to have 100% superior workspace. Likewise for the inferior workspace, this calculation was an average of the 4 following motions: below-the-waist shoulder abduction, below-the-waist shoulder flexion, elbow flexion, and shoulder external rotation. Raw data of injured arm range of motion (ROM) is included by Hingtgen et al [4].
We employed workspace equations based on the following input and output variables:
Input Variables
SAi = shoulder abduction of injured arm (maximum degrees)
SAh = shoulder abduction of healthy arm (maximum degrees)
SFi = shoulder flexion of injured arm (maximum degrees)
SFh = shoulder flexion of healthy arm (maximum degrees)
SEi = shoulder external rotation of injured arm (maximum degrees)
SEh = shoulder external rotation of healthy arm (maximum degrees)
EFi = elbow flexion of injured arm (maximum degrees)
EFh = elbow flexion of healthy arm (maximum degrees)
P = angle of shoulder flexion at which the hand is above the pelvis (degrees)
Xa, Xf = intermediate variables (for calculation only)
Output Variables
SWS = superior workspace (% of healthy arm)
LWS = inferior workspace (% of healthy arm)
Equations
Only for
In addition to the 3D motion capture data, the participant completed the following PROMs at each time point: Disabilities of the Arm, Shoulder, and Hand (DASH), Patient-Reported Outcomes Measurement Information System (PROMIS), Impact of BPI, and Short Form 36 Health Survey (SF-36). Clinical evaluations were noted from charts regarding Medical Research Council (MRC) Scale for Muscle Strength at time points aligning with their ROM measurements.
Statistical Analysis
Two-tailed independent t tests were used to assess mean differences at different time points, with 2 degrees of freedom given that there were 3 trials for each time point. Welch’s correction factor for unequal variance was applied. Correlations with PROMs were calculated using linear regression with the analysis of variance (ANOVA) test to determine correlation coefficient (r and r2) and statistical significance (P value) at a threshold of α = 0.05.
Results
In initially assessing the change in workspace over time, superior workspace was significantly more inhibited than the inferior (Mdiff = 0.56, P < .01). However, over the course of 2 years there was significant improvement (Mdiff = 0.54, P < .01) in the superior workspace compared to no change (Mdiff = 0.04, P > .05, ns) in the inferior workspace. Increases in superior workspace correlated moderately with lower PROMIS Depression scores (r = −0.580, P < .05) and DASH scores (r = −0.585, P < .05). Other PROMs and all inferior workspace correlations were non-significant. Graphs of workspaces over time for the patient are included in Fig. 2a. A representation of how workspace changed in a 3D space is provided in Fig. 2b.
Fig. 2.
(a) Superior and Inferior Workspaces over time, patient BPI 01. Graph annotated (right) to demonstrate significant Superior WS improvement over time. (b) Change of BPI-01 Workspace over time, graphical representation.
Discussion
This case report describes the use of motion capture assessments in measuring recovery of function after BPI reconstruction over time with the workspace model. Longitudinal tracking of workspace can display improvement in function to patients, therapists, and surgeons in an objective and visually simple manner. These visualizations may also be used to guidedtreatment strategies, as the patient and care team can more readily converse about functional deficits that remain and how to accommodate or treat them. For complex patients, this technology may allow for an individualized, composite patient dashboard to track improvement rather than a broad one-size-fits-all approach with only a handful of metrics. From a broader perspective, accumulation of longitudinal workspace data over a multitude of BPI types and treatment strategies will facilitate development of tools that can predict outcomes, which has applicability to preoperative counseling.
Patient-reported outcomes, such as PROMIS, DASH, SF36, and Impact of BPI, will continue to have a role in assessment after BPI [11], as they account for the patient’s subjective perspective of their injury through a number of individual variables. Three-dimensional motion-capture based workspace assessment, being a purely quantitative metric, stands in contrast to these measures but can be complementary to PROMs. Moreover, knowing which PROMs match quantitative metrics and which reflect other factors will help assess what is missing in tracking holistic recovery. In our case, superior workspace improvements aligned moderately with lower PROMIS Depression and a lower DASH score, although these metrics are more variable between adjacent time points. Inferior workspace did not match any of these reported outcomes, as it did not vary over time. Overall, this reveals how patient perception does not always track perfectly with functional recovery, emphasizing the need to measure both. In the instances in which it does associate with quantitative metrics, it matches more closely with upper workspace, reaffirming its relative predictive capability compared to lower workspace.
The limitations for this work revolve around its small scope, considering that it is a pilot study testing the feasibility of this system on a single patient. Given this, this report has limited diagnostic ability for the specific patient participating in it. The trends discussed are rather examples of analyses made possible by applying the workspace model. This furthers reachable workspace as a practical and quantitative way to describe BPI injury severity and lays the foundation for future work to address these associations. The main drawback of this method is the high resource investment required to record motion capture data. Going forward, this gold-standard process may be simplified with 2D systems to quantify each of the constituent motions and apply the same workspace calculation. These simplified systems would use this approach as a foundation and work on improving accessibility. The benefit to this model is that it can establish accurate and function-specific recovery timelines. However, there remains work to be done prior to utilizing this technology more broadly: this study represents the first step in a line of inquiry that will require further testing, both at scale and with a more robust validation against other 3D quantitative measures. This standardized data may help with the validation of new systems, assessing surgical techniques, and tracking complex injuries. Essentially, this model is a rigorous baseline system which can be adapted and simplified to individual clinical needs.
In conclusion, in this report we describe the use of 3D motion capture technology to calculate and track changes in reachable workspace in a patient recovering from brachial plexus reconstruction. Advantages of this system include its high spatial accuracy and its ease of understanding for the patient as it describes a “reachable workspace” rather than just ROM values. Ideally, workspace can be implemented alongside PROMs assessments to provide an accurate, reliable, and comprehensive battery of measures to track recovery of upper limb function after BPI.
Supplemental Material
Supplemental material, sj-docx-1-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: CJD was supported by (1) a grant from the American Foundation for Surgery of the Hand and (2) grant AR079139-01 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration.
Informed Consent: Informed consent was obtained from the patient included in this case study.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
ORCID iD: Christopher J. Dy  https://orcid.org/0000-0003-1422-2483
https://orcid.org/0000-0003-1422-2483
References
- 1. Dy CJ, Brogan DM, Rolf L, James AS. ‘Being a patient the rest of my life’: the influence of patient participation during recovery after brachial plexus injury. J Hand Ther. 2023;36(1):60–65. 10.1016/j.jht.2021.10.002. [DOI] [PubMed] [Google Scholar]
- 2. Han JJ, Kurillo G, Nicorici A, Johnson LB, Abresch RT, Henricson EK, et al. P.16.11 Upper extremity reachable workspace evaluation in FSHD using Kinect. Neuromusc Dis. 2013;23(9–10):825–826. 10.1016/j.nmd.2013.06.648. [DOI] [Google Scholar]
- 3. Hill JR, Lanier ST, Brogan DM, Dy CJ. Management of adult brachial plexus injuries. J Hand Surg Am. 2021;46(9):778–788. 10.1016/j.jhsa.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 4. Hingtgen B, McGuire JR, Wanget M, Harris GF. An upper extremity kinematic model for evaluation of hemiparetic stroke. J Biomech. 2006;39(4):681–688. 10.1016/j.jbiomech.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 5. James MA. Use of the Medical Research Council muscle strength grading system in the upper extremity. J Hand Surg Am. 2007;32(2):154–156. 10.1016/j.jhsa.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 6. Kasten P, Maier M, Wendy P, Rettig O, Raiss P, Wolf S, Loew M. Can shoulder arthroplasty restore the range of motion in activities of daily living? A prospective 3D video motion analysis study. J Shoulder Elbow Surg. 2010;19(2 suppl):59–65. 10.1016/j.jse.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 7. MacAvoy MCG, David P. Critical reappraisal of Medical Research Council muscle testing for elbow flexion. J Hand Surg. 2007;32(2):149–153. 10.1016/j.jhsa.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 8. Mancuso CA, Lee SK, Dy CJ, Landers ZA, Model Z, Wolfe SW. Expectations and limitations due to brachial plexus injury: a qualitative study. Hand (New York, NY). 2015;10(4):741–749. 10.1007/s11552-015-9761-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oskarsson B, Joyce NC, De Bieet E, et al. Upper extremity 3-dimensional reachable workspace assessment in amyotrophic lateral sclerosis by Kinect sensor. Muscle Nerve. 2016;53(2):234–241. 10.1002/mus.24703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Richardson RT, Russo SA, Chafetz RS, et al. Evaluation of upper extremity reachable workspace in children with brachial plexus birth injury. J Hand Surg. 2024;49(2):141–149. 10.1016/j.jhsa.2023.11.013. [DOI] [PubMed] [Google Scholar]
- 11. Russo SA, Tyler Richardson R, Richards JG, et al. Effect of glenohumeral reduction type combined with tendon transfer for brachial plexus injury on objective, functional, and patient-reported outcomes. J Hand Surg. 2021;46(7):624.E1–624-E11. 10.1016/j.jhsa.2020.11.021. [DOI] [PubMed] [Google Scholar]
- 12. Sakellariou VI, Badilas NK, Mazis GA, et al. Brachial plexus injuries in adults: evaluation and diagnostic approach. ISRN Orthop. 2014;2014:726103. 10.1155/2014/726103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tak I, Wiertz WP, Barendrecht M, Langhout R. Validity of a new 3-D motion analysis tool for the assessment of knee, hip and spine joint angles during the single leg squat. Sensors (Basel). 2020;20(16):4539. 10.3390/s20164539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Terzis JK, Papakonstantinou KC. The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg. 2000;106(5):1097–1122. 10.1097/00006534-200010000-00022. [DOI] [PubMed] [Google Scholar]
- 15. Yamaura K, Mifune Y, Inui A, et al. Accuracy and reliability of tridimensional electromagnetic sensor system for elbow ROM measurement. J Orthop Surg Res. 2022;17(1):60. 10.1186/s13018-022-02961-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316251324165 for Creating a Reachable Workspace Model With 3D Motion Capture to Track Adult Brachial Plexus Injury Recovery: A Representative Case Report by Eshan S. Sane, Rannon Huo, David M. Brogan, Michael J. Harris and Christopher J. Dy in HSS Journal®