Abstract
Background
The aim of this investigation was to evaluate if the hard and soft tissue dentoalveolar process of the mandible follows the tooth movements after lower premolar extractions and anterior retraction in Class III camouflage treatment.
Methods
This retrospective study included 25 patients in retention (f/m 12,13) who had previously been treated with lower premolar extractions for Class III camouflage with a completely customized lingual appliance (Wits at T0 -6.7, ± 2.5 mm). The periodontal and dental health of the lower 6 anterior teeth was evaluated (T1) by a thermal sensitivity test, probing and visual inspection after a mean retention period of 3.1 years (± 2.5, min/max 1.0/9.6 years). A novel non-invasive method was used to measure the thickness of the hard and soft tissue dentoalveolar process on the labial and lingual side of the teeth before treatment (T0) and in retention (T1) at 3 different levels using superimposed intraoral scans. A paired t-test with α = 5% was used to evaluate differences between the endpoints.
Results
At T1, all 25 patients (mean age 26.8 ± 9.7 years, min/max 16.3/49.5 years) presented uncompromised periodontal and dental situations in the lower anterior segment. The presented digital method for evaluating dimensional changes of the dentoalveolar process had excellent reliability (ICC) with a method error of 0.01 mm. The mean total labio-lingual dimension of the hard and soft tissue dentoalveolar process (min/max 7.89/10.02 mm at T0) was identical at T0 and T1 (mean change of 0.00 ± 0.33 mm, min/max -0.98/0.8 mm). At all levels, the teeth moved only 0.12 mm to the lingual side within the dentoalveolar process and therefore, they moved with the dentoalveolar process and not through it.
Conclusion
In non-surgical camouflage treatment with lower premolar extractions in moderate to severe Class III malocclusions, the dentoalveolar process can follow the movement of the mandibular incisors and canines during controlled retraction without any adverse effects.
Keywords: Lingual orthodontics, Completely customized lingual appliance, Class III camouflage, Dentoalveolar process remodelling, Digital 3-D superimposition
Introduction
Dentoalveolar compensation of skeletal discrepancies is one of the most frequently applied orthodontic treatment concepts [1–9]. The indications of this treatment approach and the extent to which it makes sense clinically have been discussed controversially to this day [10, 11]. Consensus has been achieved as to the assessment of how well various orthodontic appliances can perform, with fixed appliances being preferred over removable appliances in terms of controlling the precise, 3-dimensional movement of the teeth [12, 13]. Along with the choice of the orthodontic appliance, the orthodontist’s level of qualification has a decisive influence [14]. Orthodontic mechanotherapy is a complex task in which, as in any medical/dental procedure, the quality of how a challenging treatment plan is executed in the patient’s mouth reflects the level of training as well as the skill of the orthodontic practitioner to a great extent. In line with this, the discussion of the possibilities associated with the dentoalveolar compensation of skeletal discrepancies, controversial to this day, is shaped by addressing these prerequisites (kind of appliance inserted/therapist’s qualification). An orientation for selecting the best treatment plan offered by Proffit and White are the so-called envelopes of possible corrections which define the limits of dentoalveolar compensation in still growing and in adult patients [15]. More recent developments in orthodontic mechanotherapy, such as skeletal anchorage as well as Herbst treatment in adult patients, would even suggest a potentially larger envelope than described by Proffit and White [2, 4, 6–8]. However, the modern shift from multibracket appliances to removable aligners may restrict the range of indications substantially, which immediately raises the subsequent question of the ethical/moral background of this treatment approach, like in other medical disciplines [16, 17]. There is certainly general consensus in medicine/dentistry that no patient should undergo surgery because 1) the orthodontist favours this or that type of approach and dentoalveolar compensation is not possible with the preferred appliance or 2) the orthodontist’s limited mechanotherapeutic training and skill requires assistance by a maxillofacial surgeon. Therefore, a clear definition of what is clinically feasible in relation to the relevant skeletal discrepancy in the sagittal, transverse, and vertical planes is essential. In this regard, completely customized lingual appliances (CCLA) have been demonstrated to achieve clinical performance in cases with skeletal discrepancies by numerous studies [2–5, 7–9, 18–23]. In these discrepancies, tooth movements considered unusual to the present state of our knowledge have been achieved in practice with precision, reliability and efficiency according to the treatment plan.
In a previous study on the inclination control of the lower front teeth in a Class III camouflage treatment with extraction in the mandible, a significant and controlled movement of all front teeth to the lingual side was observed, with a shift of up to more than 7 mm in the area of the centre of resistance [7]. With such a large correction, the question arises as to whether the dentoalveolar process, including its hard and soft tissues, follows the tooth movement or whether the tooth, instead of involving the alveolar process, moves through it. The aim of the present study was therefore to evaluate the condition of the anterior mandibular dentoalveolar process in the identical patient collective after a retention period of at least one year.
Material and methods
This investigation is a follow-up evaluation of the study by Thiem et al. who surveyed 25 adolescent or adult patients presenting a Class III molar relationship on one or both sides [7]. All patients received camouflage treatment with uni- or bilateral lower premolar extraction and were consecutively debonded between 2015 and 2024, after fixed-appliance orthodontic treatment with a CCLA (WIN, DW Lingual Systems, Bad Essen, Germany) in one orthodontic specialist practice (Bad Essen, Germany). Between 2015 and 2024 twelve different orthodontists or postgraduate students have been working in this specialist practice. All cases were supervised by D.W.. The approval for this retrospective cohort study was received from the Ethics Committee of the Hannover Medical School, Hannover, Germany (3151–2016). For Class III camouflage, the lower incisors were retracted “en masse” with precise inclination control (Fig. 1). The mean Wits value before camouflage treatment (T0) was −6.7 mm (± 2.5, min/max −10.8/−2.1) and the lingual displacement of the centre of resistance of the lower incisors was 3.7 mm on average (± 1.3, min/max 1.4/7.1 mm) [7].
Fig. 1.

Adult patient with Class III malocclusion (same patient as Fig. 6 b). Camouflage treatment with lower premolar extractions and lower incisor inclination control
After a minimum retention phase of at least 1 year (mean: 3.1 years, SD ± 2.5, min/max 1.0/9.2 years), all 25 patients (f/m 12/13) were called in for a clinical re-evaluation (T1) of the achieved treatment result with particular attention to the periodontal situation in the lower anterior segment. To get an impression of the tooth movement achieved during camouflage, superimpositions of the mandible before and directly after treatment were traced by an orthodontist with comprehensive expertise in this field (P.R.). The profile x-rays before and after treatment were checked and corrected for enlargement differences and traced with Adobe Illustrator 9.0 (Adobe Inc. San José, USA) [24]. The tracings were superimposed on the stable anatomical structures in the mandible according to Björk [25], Björk and Skieller [26] and Springate [27]. All 25 patients showed up and the actual clinical situation could be re-evaluated: 1) A thermal tooth sensitivity test with a refrigerant spray was performed on the lower incisors and canines. 2) On the same teeth, the probing depth was measured on the lingual side with a periodontal probe (PCP11, Aesculap AG, Tuttlingen, Germany) at the deepest point of the gingival margin. 3) To document potential lingual recessions in this segment, high-resolution, digital, intraoral photographs (Camera D200, with Nikkor 105 mm, Nikon, Tokyo, Japan) were taken with the help of an intraoral mirror (Filtrop AG, Balzers, Liechtenstein). Similar to the methodology of Renkema et al., a lingual recession was scored if the lingual root surface was clearly exposed [28]. 4) An intraoral scan of the mandible with the Trios 3 (3shape, Copenhagen, Denmark) was performed with particular attention to the anterior dentoalveolar process.
Hard and soft tissue dentoalveolar process evaluation
This scan was compared to the initial Trios 3 scan before treatment (T0) with the help of the software GOM 2021 (2021 Hotfix 8, Rev. 152,091, GOM Braunschweig, Germany). As measurements of the thickness of the alveolar process or its bone morphology may lead to wrong results when rotated teeth are measured before and after derotation, teeth rotated by 6° or more at T0 were excluded (Figs. 2 and 3). A customized best-fit algorithm was used to standardize and facilitate the matching process of every single anterior tooth (lower canine to canine) and define and cut a reproducible plane in the labio-lingual tooth axis (Beyer 3D Scan und Messtechnik GmbH, Ahaus, Germany). Any change in thickness of the alveolar process between the two timepoints was recorded as the difference (T1-T0) of the distance between its outer soft tissue borders/margins on the labial and lingual sides at the relevant tooth measured at both T0 and T1 on three different levels, 1, 2 and 3 mm apical from the gingival margin as found at T1 (Figs. 4 and 5). Also, the overall dimension of the alveolar process on these three different levels was recorded in millimetres at both timepoints.
Fig. 2.
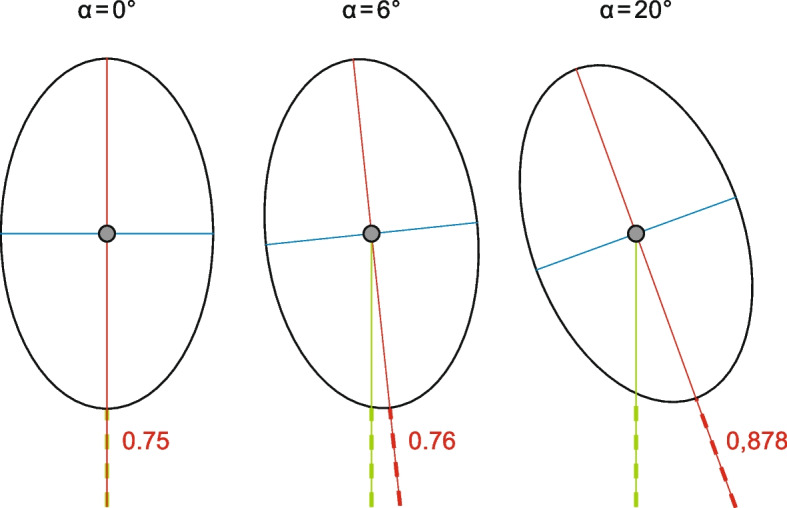
The measurement of dentoalveolar process dimensions on the labial or on the lingual side of the root leads to wrong results if teeth are rotated. With α < 6° of rotation the error amounted to under 0.01 mm, which seemed acceptable for this study (left and middle image). With more severe rotations, the results would be misleading (right image)
Fig. 3.
Customized GOM software for rotation measurements. Individual markers on the incisor edges of the malocclusion model from canine to canine (a, b). Transfer of the individual markers to the final model after debonding (c, d). Measurement of the angle of rotation correction during treatment after matching (e, f)
Fig. 4.

Method for measuring the change of hard and soft tissue dentoalveolar process thickness on the labial and the lingual side and its total labio-lingual dimension at 3 different levels. Definition of areas for matching (red) after isolating each single tooth together with its periodontal process (a, b). The incisor edge should not be used for the matching process because it is frequently abraded, particularly in Class III patients. Matched central incisor at T0 and T1 (c, d). Customized software-assisted sagittal cut of the incisor and its surrounding hard and soft tissue dentoalveolar process (e)
Fig. 5.

Measurements of the changes in the labial and lingual dentoalveolar process thickness after superimposition (T0 grey/T1 colored) 1, 2, and 3 mm apical from the gingival margin at T1 (a). Measurements of the total labio-lingual dimension of the dentoalveolar process at T0 (grey) on the same levels (b)
Statistical analysis
Intrarater reliability was evaluated using intraclass correlation coefficients (ICC). For this purpose, 10% of the sample was randomly selected and remeasured after at least 2 weeks by the main investigator (R.L.). ICC estimates and their 95% confidence intervals were calculated based on a single-measurement, absolute-agreement, 2-way mixed effects model. Interpretation of the correlation coefficients followed the cut-off limits of Koo and Li 2016 [29]. The error of measurement was determined using Dahlberg’s formula [30]. All data were summarized descriptively for each endpoint using mean, ± standard deviation (SD), min, max. The difference between T0 and T1 at the different levels and for the different kinds of teeth were analysed using a paired t-test. A p-value p < 0.05 was considered as statistically significant.
Results
The baseline characteristics are summarized in Table 1. The amount of anterior tooth movements in each patient during Class III camouflage treatment with lingual appliances and the corresponding clinical lingual view of the lower front teeth in retention (T1) is shown in Fig. 6. Overall, a clinically uncompromised periodontal and dental situation was evident at T1: All (n = 150) lower anterior teeth responded positively to the thermal tooth sensitivity testing. The mean probing depth on the lingual side of the lower incisors and canines was 1.27 mm (± 0.45, min/max 1/2 mm). Four patients showed 6 recessions in total on the lingual side, all less than 1 mm, which became visible after the removal of calculus around the fixed retainer. All fixed retainers were intact at T1.
Table 1.
Baseline Characteristics
| Number of included patients | 25 |
| Male/Female | 13/12 |
| Evaluated teeth | 150 |
| Age at T1 (years) Mean, ± SD, Min/Max | 26.8, ± 9.7, 16.3/49.5 |
| Time in retention at T1 (years) Mean, ± SD, Min/Max | 3.1, ± 2.5, 1.0/9.6 |
| Wits Male at T0 (mm) Mean, ± SD, Min/Max | −7.1, ± 2.5, −10.7/−2.1 |
| Wits Female at T0 (mm) Mean, ± SD, Min/Max | −6.3, ± 2.5, −10.8/−3.4 |
| Lower 1 Cr displacement (mm) Mean, ± SD, Min/Max | 3.7, ± 1.3, 1.4/7.1 |
Fig. 6.
Structural superimpositions of the mandible of the 25 included patients before and after Class III camouflage treatment with lower premolar extractions and the corresponding clinical situation at recall (T1)
Alveolar process remodelling
Measurements of the tooth rotation achieved during active treatment led to the exclusion of 82 teeth as they were rotated by 6° or more at T0 compared to their position at T1 (Figs. 2 and 3). The thickness of the dentoalveolar process, including hard and overlaying soft tissue, of 26 central incisors, 21 lateral incisors and 21 canines could be evaluated in the end. Intrarater reliability was excellent for changes in alveolar process thickness on the labial and on the lingual side of the matched teeth (ICC 0.998, 95% CI 0.996–0.999) and for labio-lingual total alveolar process dimension (ICC 0.990, 95% CI 0.970–0.996). According to Dahlberg’s formula, a measurement error of 0.01 mm and 0.06 mm must be assumed, accordingly, for this study (Table 2). The descriptive statistics for all included teeth and the results of the corresponding t-tests are shown in Tables 3, 4 and 5. Looking at all included teeth, there was no change of mean total dentoalveolar process dimension at all 3 levels together (mean: 0.00 mm, ± 0.33 mm, min/max −0.98/0.8 mm, CI95% −0.08, 0.08, Table 3). Overall, there was a mean augmentation of the thickness on the labial side of 0.12 mm (± 0.25 mm, min/max −0.71/0.82 mm) and a mean reduction of the thickness on the lingual side of −0.11 mm (± 0.24 mm, min/max −0.7/0.46 mm, Table 3). Furthermore, in none of the 3 different tooth groups a significant change in alveolar process thickness was found when evaluating the three different levels together (Table 4). Looking at the different levels of the different tooth groups, a statistically significant, but clinically irrelevant mean change of 0.19 mm for the first level of the canines (± 0.36, min/max −0.61/1.05 mm) and −0.13 mm for the second level of the lateral incisors (± 0.28, min/max −0.9/0.18 mm) was found (Table 4). Looking at the different levels separately, no statistically significant dimension change could be seen. The mean total labio-lingual dimension changes on the different levels were all less than 2% compared to their dimension at T0 (Table 4). Although the mean total thickness of the alveolar process did not change, the position of the central and lateral incisors within the process appeared to be a bit more (−0.15/−0.17 mm) towards the lingual side (Table 5).
Table 2.
Intrarater correlation coefficient and method error
| Measurement | Description | ICC (95%CI) | Method error |
|---|---|---|---|
| Change in dentoalveolar process thickness on labial and lingual side on 3 different levels | Distance between the superposed labial and lingual borders of the hard and soft tissue alveolar process at T0 and T1 |
0.998 (0.996–0.999) |
0.01 mm |
|
labio-lingual dentoalveolar process dimension on 3 different levels |
Thickness of the total hard and soft tissue alveolar process perpendicular to the incisor edge |
0.990 (0.970–0.996) |
0.06 mm |
ICC < 0.5: poor reliability; 0.5 ≤ ICC < 0.75: moderate reliability; 0.75 ≤ ICC < 0.9: good reliability; ICC ≥ 0.9: excellent reliability
Table 3.
Change of the thickness of the hard and soft tissue dentoalveolar process on labial and lingual side of the teeth and difference in total dimension in different levels in millimeters. Paired t-Test over all teeth (Post – Pre treatment) H0: difference = 0
| All teeth | N | Mean | SD | 95% Confidence Intervall | Min | Max | p-value |
|---|---|---|---|---|---|---|---|
| Labial level 1 | 68 | 0.09 | 0.24 | (0.03, 0.15) | −0.9 | 0.8 | 0.0045 |
| Labial level 2 | 68 | 0.12 | 0.26 | (0.06, 0.18) | −0.72 | 0.86 | 0.0002 |
| Labial level 3 | 68 | 0.14 | 0.31 | (0.06, 0.21) | −0.71 | 0.8 | 0.0004 |
| Lingual level 1 | 68 | −0.07 | 0.26 | (−0.13, 0) | −0.55 | 0.66 | 0.0383 |
| Lingual level 2 | 68 | −0.11 | 0.26 | (−0.18, −0.05) | −0.76 | 0.49 | 0.0004 |
| Lingual level 3 | 68 | −0.16 | 0.3 | (−0.23, −0.09) | −0.85 | 0.55 | < 0.0001 |
| All labial levels | 204 | 0.12 | 0.25 | (0.06, 0.18) | −0.71 | 0.82 | 0.0003 |
| All lingual levels | 204 | −0.11 | 0.24 | (−0.17, −0.05) | −0.7 | 0.46 | 0.0003 |
| Total dimension difference level 1 | 68 | 0.02 | 0.36 | (−0.07, 0.11) | −1.14 | 1.05 | 0.6275 |
| Total dimension difference level 2 | 68 | 0.01 | 0.32 | (−0.07, 0.08) | −0.9 | 0.94 | 0.8474 |
| Total dimension difference level 3 | 68 | −0.02 | 0.38 | (−0.11, 0.07) | −0.89 | 0.91 | 0.6792 |
| Total dimension difference all levels | 204 | 0 | 0.33 | (−0.08, 0.08) | −0.98 | 0.8 | 0.9343 |
Table 4.
Hard and soft tissue dentoalveolar process total dimension on different levels by tooth group in millimeters and change in total dimension. Paired t-Test of the change in total dimension (Post – Pre treatment) H0: difference = 0
| Tooth-type | N (teeth) | Labio-lingual dimension at T0 in mm | Treatment effect in mm (%) | SD | 95% Confidence Intervall | Min | Max | p-value |
|---|---|---|---|---|---|---|---|---|
| Central incisor level 1 | 26 | 7.89 | −0.02 (−0.25) | 0.34 | (−0.16, 0.11) | −0.85 | 0.73 | 0.7317 |
| Central incisor level 2 | 26 | 8.31 | 0.03 (−0.36) | 0.36 | (−0.11, 0.18) | −0.88 | 0.94 | 0.6654 |
| Central incisor level 3 | 26 | 8.42 | 0 (0) | 0.45 | (−0.18, 0.18) | −0.87 | 0.91 | 0.9863 |
| Central incisor all | 78 | 8.20 | 0 (0) | 0.36 | (−0.14, 0.15) | −0.87 | 0.8 | 0.9771 |
| Lateral incisor level 1 | 21 | 8.29 | −0.09 (−1.09) | 0.35 | (−0.25, 0.06) | −1.14 | 0.46 | 0.2339 |
| Lateral incisor level 2 | 21 | 8.62 | −0.13 (−1.51) | 0.28 | (−0.25, 0) | −0.9 | 0.18 | 0.0459 |
| Lateral incisor level 3 | 21 | 8.69 | −0.07 (−0.81) | 0.36 | (−0.23, 0.09) | −0.89 | 0.51 | 0.374 |
| Lateral incisor all | 63 | 8.53 | −0.1 (−1.17) | 0.3 | (−0.23, 0.04) | −0.98 | 0.22 | 0.1535 |
|
Canine level 1 |
21 | 9.79 | 0.19 (1.94) | 0.36 | (0.03, 0.36) | −0.61 | 1.05 | 0.0254 |
|
Canine Level 2 |
21 | 9.98 | 0.11 (1.10) | 0.27 | (−0.01, 0.24) | −0.31 | 0.59 | 0.067 |
|
Canine level 3 |
21 | 10.02 | 0.01 (0.10) | 0.31 | (−0.13, 0.15) | −0.43 | 0.67 | 0.8786 |
|
Canine all |
63 | 9.93 | 0.11 (1.11) | 0.29 | (−0.03, 0.24) | −0.38 | 0.65 | 0.1126 |
Table 5.
Change of the thickness of the hard and soft tissue dentoalveolar process on labial and lingual side in 3 different levels by tooth group and paired t-test for the difference (Post – Pre treatment) H0: difference = 0
| Tooth-Type | Variable | N | Mean | SD | 95% Confidence Intervall | Min | Max | p-value |
|---|---|---|---|---|---|---|---|---|
| Central Incisor | Labial level 1 | 26 | 0.11 | 0.25 | (0.01, 0.21) | −0.7 | 0.8 | 0.0301 |
| Labial level 2 | 26 | 0.16 | 0.28 | (0.05, 0.27) | −0.72 | 0.86 | 0.008 | |
| Labial level 3 | 26 | 0.18 | 0.34 | (0.04, 0.32) | −0.71 | 0.8 | 0.0124 | |
| Lingual level 1 | 26 | −0.13 | 0.19 | (−0.21, −0.06) | −0.5 | 0.23 | 0.0016 | |
| Lingual level 2 | 26 | −0.13 | 0.2 | (−0.21, −0.05) | −0.51 | 0.25 | 0.0033 | |
| Lingual level 3 | 26 | −0.18 | 0.27 | (−0.29, −0.07) | −0.85 | 0.33 | 0.0021 | |
| Labial all levels | 78 | 0.15 | 0.28 | (0.04, 0.26) | −0.71 | 0.82 | 0.0103 | |
| Lingual all levels | 78 | −0.15 | 0.19 | (−0.22, −0.07) | −0.5 | 0.23 | 0.0004 | |
| Lateral Incisor | Labial level 1 | 21 | 0.02 | 0.27 | (−0.1, 0.14) | −0.9 | 0.38 | 0.7724 |
| Labial level 2 | 21 | 0.08 | 0.27 | (−0.05, 0.2) | −0.53 | 0.53 | 0.2139 | |
| Labial level 3 | 21 | 0.13 | 0.33 | (−0.02, 0.29) | −0.46 | 0.53 | 0.0763 | |
| Lingual level 1 | 21 | −0.11 | 0.27 | (−0.23, 0.01) | −0.55 | 0.35 | 0.0786 | |
| Lingual level 2 | 21 | −0.21 | 0.32 | (−0.35, −0.06) | −0.76 | 0.49 | 0.0084 | |
| Lingual level 3 | 21 | −0.21 | 0.39 | (−0.38, −0.03) | −0.8 | 0.55 | 0.0261 | |
| Labial all levels | 63 | 0.08 | 0.27 | (−0.05, 0.2) | −0.62 | 0.46 | 0.2158 | |
| Lingual all levels | 63 | −0.17 | 0.31 | (−0.31, −0.03) | −0.7 | 0.46 | 0.0184 | |
| Canine | Labial level 1 | 21 | 0.13 | 0.21 | (0.03, 0.22) | −0.17 | 0.6 | 0.0121 |
| Labial level 2 | 21 | 0.12 | 0.21 | (0.03, 0.22) | −0.29 | 0.55 | 0.0129 | |
| Labial level 3 | 21 | 0.09 | 0.23 | (−0.01, 0.19) | −0.34 | 0.6 | 0.0846 | |
| Lingual level 1 | 21 | 0.06 | 0.27 | (−0.06, 0.19) | −0.48 | 0.66 | 0.285 | |
| Lingual level 2 | 21 | −0.01 | 0.21 | (−0.1, 0.09) | −0.33 | 0.43 | 0.8621 | |
| Lingual level 3 | 21 | −0.08 | 0.21 | (−0.17, 0.01) | −0.51 | 0.28 | 0.092 | |
| Labial all levels | 63 | 0.11 | 0.19 | (0.03, 0.2) | −0.27 | 0.55 | 0.0142 | |
| Lingual all levels | 63 | −0.01 | 0.21 | (−0.1, 0.09) | −0.35 | 0.4 | 0.8671 |
After Class III camouflage treatment with lower premolar extractions and precise inclination control of the lower anterior teeth during dentoalveolar compensation, the hard and soft tissue dentoalveolar process had followed the bodily lingual movement of the teeth, even in severe cases, after a mean retention period of 3.1 years. Although the teeth moved towards lingual perpendicular to the alveolar process up to > 7 mm, the tooth movement expressed involved the surrounding hard and soft tissues (Fig. 7).
Fig. 7.
One included patient had a CBCT scan in retention because of a surgical indication. The matching of the central incisor (left image), lateral incisor (middle image), and canine (right image) in the CBCT scan and the intraoral scan highlight the size and the position of the roots within the alveolar process
Discussion
This is the first study that evaluates the periodontal and dental health of the lower anterior teeth that have been in retention for at least 12 months after Class III camouflage treatment with lower premolar extractions. Previously, Thiem et al. showed a dentoalveolar compensation in these cases, introducing unusual, but favourable tooth movements [7]. In particular, the authors could show superior control of the incisor inclination during retraction due to the 3-dimensional torque control of the appliance used. In some cases, the lower incisors were bodily retracted for more than 7 mm as demonstrated on the lateral cephalograms before and after lingual orthodontic treatment (Fig. 6b). On the lateral cephalograms taken directly after debonding, it was difficult to define if the alveolar process, including its hard and soft tissues, had followed the tooth movements or the incisor roots in the end had passed beyond the limits of the envelope of possible corrections described by Proffit and White [15]. Looking only at the hard tissues, several studies based on CBCT analysis reported that after the retraction of maxillary and mandibular incisors, the alveolar process did not follow entirely [31–33]. In a systematic review, Guo et al. reported a reduction of bone thickness of 0.57 mm on the lingual side of mandibular incisors in the finishing stage of treatment after anterior retraction in protrusive cases measured 3 mm apical of the cemento-enamel junction [31]. In contrast, Kobylyanskyy et al. did not find any reduction of the lingual bone thickness after the alignment phase in which the anterior teeth were reclined [34]. Recently, several authors found significant remodelling and increasing alveolar bone thickness after orthodontic retraction on the lingual side of the anterior teeth in the retention phase [35–39]. Similar findings have been reported for retracted maxillary incisors after up to 9 years in retention [35, 37–40]. This leads to the hypothesis that the envelope of possible corrections in adult Class III patients with orthodontic tooth movement only is possibly larger than what Proffit and White had in mind [15]. The results of our study support these findings, even for more severe Class III corrections with exceptional root control and, therefore, substantial root movement of lower anterior teeth to the lingual side.
Tooth related 3-dimensional superimposition of the alveolar process
A novel method of digital 3-dimensional superimposition of the dentoalveolar process comprising its hard and soft tissues is introduced in this study. Digital models have been used to evaluate dimensional changes on the labial and lingual side of the teeth and its total dimension in three different levels. Earlier studies on this aspect have been based almost exclusively on data acquisition with CBCT scans [31–33]. Upon closer examination of these studies, the section on limitations in these studies often highlights the recurring issue of an undeniably coarse voxel resolution, which makes an accurate assessment of structures smaller than 0.5 mm impossible. Particularly in the region of the mandibular anterior teeth, the labial and lingual bony coverage of the roots is often physiologically thinner than 0.5 mm [41, 42]. Moreover, in all European countries, CBCT imaging is not considered part of standard orthodontic diagnostics due to its high radiation exposure deemed disproportionate to its clinical benefit [43]. Therefore, in addition to the simplicity of clinical application in nearly every orthodontic practice, the evaluation using intraoral scans is also advantageous from the perspective of medical ethics. Not only the teeth, but also the dentoalveolar process should be captured as comprehensively as possible, which, in the present study, was achieved through data collection before treatment (T0) and in retention (T1) on all three levels. Since intraoral scanning, which is required as a basis for the 3D superimposition presented here, can be exceedingly challenging when aiming to capture not only the teeth, but also the upper portion of the alveolar process, a perfectly digitized plaster model taken from an alginate or even a silicone impression could alternatively be used for the described evaluation.
Evaluation of the thickness of the dentoalveolar process dimensions around rotated teeth
In this study the thickness of the alveolar process was evaluated exclusively on teeth which were not visibly rotated (< 6°) at the onset of orthodontic treatment. As displayed in Fig. 2, the changes in thickness of the alveolar process should not be measured on rotated teeth, as the initial thickness, which is always the baseline, may be overestimated, just as in almost all studies on CBCT scans [31–40].
Strengths and limitations
The present study is a continuation of the investigations by Thiem et al. on Class III camouflage treatment. A patient group treated with a comparable treatment concept does not exist. Therefore, this study allows, for the first time, an assessment of the periodontal and dental situation after an average retention period of more than three years following the completion of active camouflage therapy with premolar extractions exclusively in the mandible. The results provide initial indications of a potentially necessary update of the definition of the envelopes of possible corrections according to Proffit and White [15].
The measurement of changes in the thickness of the alveolar process without any radiation exposure, due to the limitations of intraoral scanning, allows an assessment of its upper portion only. However, the measurement 3 mm apical from the gingival margin results in good comparability with studies based on CBCT imaging. As the measurements reflect the dimensions of the entire dentoalveolar process, including hard and soft tissues, an evaluation of dimensional changes of hard and soft tissues separately is not possible with this method. Thanks to a purpose-developed, major customization of the GOM software, the intrarater reliability (ICC) as well as the error of measurement (Dahlberg) showed excellent values.
A minimum retention period of one year after debonding is not extensive; however, no clinical differences in periodontal or dental health were observed even after more than nine years of retention.
Conclusions
In non-surgical camouflage treatment with lower premolar extractions in moderate to severe Class III malocclusions, the dentoalveolar process can follow the movement of the mandibular incisors and canines during controlled retraction without any adverse effects.
Discussing a redefinition of some of Proffit and White’s definitions of the envelope of possible corrections by orthodontic tooth movements only could make sense.
The novel method of measuring dimensional changes of the periodontal process relative to the teeth is reproducible, precise, and non-invasive.
Authors’ contributions
D.W. initiated the investigation and wrote the main manuscript. D.W., J.Q.S. and Y.J. defined the conception of the method. D.W. and R.L. treated the patients and prepared the documents for the measurements. P.R. made all the superimpositions. R.L. made the measurements. J.Q.S. (lead) and Y.J. provided the statistical evaluation. All authors reviewed the manuscript.
Funding
No Funding was received.
Data availability
The data underlying this study can be shared upon reasonable request to the corresponding author.
Declarations
Ethics approval and consent to participate
The approval for this retrospective cohort study was received from the Ethics Committee of the Hannover Medical School, Hannover, Germany (3151–2016).
Consent for publication
All patients signed a written consent form.
Competing interests
D. Wiechmann is the inventor of the WIN system. All other authors have no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ruf S, Pancherz H. Orthognathic surgery and dentofacial orthopedics in adult Class II Division 1 treatment: mandibular sagittal split osteotomy versus Herbst appliance. Am J Orthod Dentofacial Orthop. 2004;126(2):140–52. [DOI] [PubMed] [Google Scholar]
- 2.Mujagic M, Pandis N, Fleming PS, Katsaros C. The Herbst appliance combined with a completely customized lingual appliance: A retrospective cohort study of clinical outcomes using the American Board of Orthodontics Objective Grading System. Int Orthod. 2020;18(4):732–8. [DOI] [PubMed] [Google Scholar]
- 3.Janssens Y, Foley PF, Beyling F, Stamm T, Schwestka-Polly R, Schmid JQ. Quality of occlusal outcome in adult Class II patients treated with completely customized lingual appliances and Class II elastics compared to adult Class I patients. Eur J Orthod. 2024;46(5). [DOI] [PMC free article] [PubMed]
- 4.Beyling F, Klang E, Niehoff E, Schwestka-Polly R, Helms HJ, Wiechmann D. Class II correction by maxillary en masse distalization using a completely customized lingual appliance and a novel mini-screw anchorage concept - preliminary results. Head Face Med. 2021;17(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lossdörfer S, Schwestka-Polly R, Wiechmann D. Control of lower incisor inclination with a completely customized lingual appliance for dentoalveolar compensation of class III malocclusion J Orofac Orthop. 2013;74(5):381–96. [DOI] [PubMed] [Google Scholar]
- 6.Zimmer B, Gaida S, Dathe H. Compensation of skeletal Class III malocclusion by isolated extraction of mandibular teeth: Part 2: Skeletal, dentoalveolar and soft tissue parameters in comparison with nonextraction Class III therapies. J Orofac Orthop. 2016;77(2):119–28. [DOI] [PubMed] [Google Scholar]
- 7.Thiem LC, Rank P, Schmid JQ, Janssens Y, Bettenhäuser-Hartung L, Wiechmann D. Favourable dentoalveolar changes after lower premolar extractions for Class III camouflage with completely customized lingual appliances. Head Face Med. 2024;20(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmid JQ, Gerberding E, Hohoff A, Kleinheinz J, Stamm T, Middelberg C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults-The Amount of Posterior Crossbite Correction. J Pers Med. 2022;12(11):1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmid JQ, Gerberding E, Hohoff A, Kleinheinz J, Stamm T, Middelberg C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults-Tipping or Translation in Posterior Crossbite Correction? J Pers Med. 2023;13(5):807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jędrzejewski M, Smektała T, Sporniak-Tutak K, Olszewski R. Preoperative, intraoperative, and postoperative complications in orthognathic surgery: a systematic review. Clin Oral Investig. 2015;19(5):969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thiem DGE, Schneider D, Hammel M, Saka B, Frerich B, Al-Nawas B, et al. Complications or rather side effects? Quantification of patient satisfaction and complications after orthognathic surgery-a retrospective, cross-sectional long-term analysis. Clin Oral Investig. 2021;25(5):3315–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robertson L, Kaur H, Fagundes NCF, Romanyk D, Major P, Flores MC. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod Craniofac Res. 2020;23(2):133–42. [DOI] [PubMed] [Google Scholar]
- 13.Haouili N, Kravitz ND, Vaid NR, Ferguson DJ, Makki L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2020;158(3):420–5. [DOI] [PubMed] [Google Scholar]
- 14.Huggare J, Derringer KA, Eliades T, Filleul MP, Kiliaridis S, Kuijpers-Jagtman A, Martina R, Pirttiniemi P, Ruf S, et al. The Erasmus programme for postgraduate education in orthodontics in Europe: an update of the guidelines. Eur J Orthod. 2014;36(3):340–9. [DOI] [PubMed] [Google Scholar]
- 15.Proffit WR, White RP Jr. Who needs surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990;5(2):81–9. [PubMed] [Google Scholar]
- 16.Stanley TH. Fentanyl. J Pain Symptom Manage. 2005;29(5 Suppl):67–71. [DOI] [PubMed] [Google Scholar]
- 17.Kuczyńska K, Grzonkowski P, Kacprzak Ł, Zawilska JB. Abuse of fentanyl: An emerging problem to face. Forensic Sci Int. 2018;289:207–14. [DOI] [PubMed] [Google Scholar]
- 18.Wiechmann D. Novel concept for posterior crossbite correction : Preliminary results. J Orofac Orthop. 2023. [DOI] [PMC free article] [PubMed]
- 19.Graf I, Bock NC, Bartzela T, Röper V, Schumann U, Reck K, Christ H, Höfer K, Fritz U, Wiechmann D, Jost-Brinkmann PG, Wolf M, Ruf S, et al. Quality of orthodontic care-A multicenter cohort study in Germany : Part 1: Evaluation of effectiveness of orthodontic treatments and predictive factors. J Orofac Orthop. 2022;83(5):291–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.AlQatami FM, Alouini O, Knösel M, Helms HJ, Schwestka-Polly R. Objective treatment outcome assessment of a completely customized lingual appliance: A retrospective study. Int Orthod. 2021;19(3):445–52. [DOI] [PubMed] [Google Scholar]
- 21.Alouini O, Wiechmann D. Completely-customized lingual orthodontics to correct class II malocclusion in adolescents. Orthod Fr. 2018;89(1):3–19. [DOI] [PubMed] [Google Scholar]
- 22.Bock NC, Ruf S, Wiechmann D, Jilek T. Dentoskeletal effects during Herbst-Multibracket appliance treatment: a comparison of lingual and labial approaches. Eur J Orthod. 2016;38(5):470–7. [DOI] [PubMed] [Google Scholar]
- 23.Vu J, Pancherz H, Schwestka-Polly R, Wiechmann D. Correction of Class II, Division 2 malocclusions using a completely customized lingual appliance and the Herbst device. J Orofac Orthop. 2012;73(3):225–35. [DOI] [PubMed] [Google Scholar]
- 24.Rank CP. Guide to superimposition of profile radiographs by "The Structural Method". 2010 (Available from: http://angle-society.com/wp-content/uploads/2020/01/guide.pdf)
- 25.Björk A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55:585–99. [DOI] [PubMed] [Google Scholar]
- 26.Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5: 1–46 [DOI] [PubMed]
- 27.Springate SD. Natural reference structures in the human mandible: a systematic search in children with tantalum implants. Eur J Orthod. 2010;32:354–62. [DOI] [PubMed] [Google Scholar]
- 28.Renkema AM, Fudalej PS, Renkema A, Kiekens R, Katsaros C. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofacial Orthop. 2013;143:206–12. [DOI] [PubMed] [Google Scholar]
- 29.Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dahlberg G. Statistical methods for medical and biological students. London: G. Allen & Unwin ltd.; 1940. p. 122–32. [Google Scholar]
- 31.Guo R, Zhang L, Hu M, Huang Y, Li W. Alveolar bone changes in maxillary and mandibular anterior teeth during orthodontic treatment: A systematic review and meta-analysis. Orthod Craniofac Res. 2021;24(2):165–79. [DOI] [PubMed] [Google Scholar]
- 32.Kalina E, Grzebyta A, Zadurska M. Bone Remodeling during Orthodontic Movement of Lower Incisors-Narrative Review. Int J Environ Res Public Health. 2022;19(22):15002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuc AE, Kotuła J, Nawrocki J, Kulgawczyk M, Kawala B, Lis J, et al. Bone Remodeling of Maxilla after Retraction of Incisors during Orthodontic Treatment with Extraction of Premolars Based on CBCT Study: A Systematic Review. J Clin Med. 2024;13(5):1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kobylyanskyy O, Schwarz L, Rausch MA, Kobylyanska A, Andrukhov O, Rausch-Fan X. Changes in the alveolar bone morphology among different patterns of incisor inclination during the alignment phase in orthodontic treatment without premolar extraction. Orthod Craniofac Res. 2024;27(4):645–55. [DOI] [PubMed] [Google Scholar]
- 35.Li L, Chen Y, Wang J, Luo N, Wu Y, Dai H, et al. Long-term morphometric changes in the anterior alveolar bone in adolescents and adults after space closure: A retrospective study. Orthod Craniofac Res. 2023;26(4):618–31. [DOI] [PubMed] [Google Scholar]
- 36.Wang J, Zhou W, Wu Y, Dai H, Zhou J. Long-term changes in the anterior alveolar bone after orthodontic treatment with premolar extraction: A retrospective study. Orthod Craniofac Res. 2022;25(2):174–82. [DOI] [PubMed] [Google Scholar]
- 37.Wang S, Li L, Liu X, Wang X, Li W, Liu D. Mandibular cortical bone remodeling characteristics in patients with extraction: A cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2024;166(3):215–26. [DOI] [PubMed] [Google Scholar]
- 38.Qin Q, Guo R, Li L, Zhu K, Su X, Zhang L, et al. Alveolar bone remodelling and stability of mandibular incisors in adult patients after orthodontic treatment with premolar extractions: A prospective follow-up study. Orthod Craniofac Res. 2024;27(3):413–20. [DOI] [PubMed] [Google Scholar]
- 39.Kim HJ, Noh HK, Park HS. Recovery bone formation on radiographic palatal bone dehiscences after incisor retraction with microimplants. Angle Orthod. 2024;94(2):168–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bae SM, Kim HJ, Kyung HM. Long-term changes of the anterior palatal alveolar bone after treatment with bialveolar protrusion, evaluated with computed tomography. Am J Orthod Dentofacial Orthop. 2018;153(1):108–17. [DOI] [PubMed] [Google Scholar]
- 41.Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):109–19. [DOI] [PubMed] [Google Scholar]
- 42.Schulze R, Couso-Queiruga E, Katsaros C. Accuracy of cone-beam computed tomography in imaging the components of the periodontal phenotype. Periodontol 2000. 2024. [DOI] [PubMed]
- 43.De Grauwe A, Ayaz I, Shujaat S, Dimitrov S, Gbadegbegnon L, Vande Vannet B, et al. CBCT in orthodontics: a systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur J Orthod. 2019;41(4):381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this study can be shared upon reasonable request to the corresponding author.






