Abstract
Aims
Edentulism's impact on overall well-being is widely recognized, but there is limited information on regional and sex disparities in its global burden. This study aims to fill this gap by providing an updated picture of edentulism's burden by region and sex and predicting its global trend for the next 2 decades.
Methods
This study analyzed and reported Global Burden of Disease (GBD) data on the prevalence, incidence, and disability adjusted life years (DALYs) of edentulism, with a breakdown by sex and sociodemographic index (SDI). Epidemiological trends from 1990 to 2021 were characterized using Joinpoint regression analysis. An Autoregressive Integrated Moving Average (ARIMA) model was used to forecast edentulism prevalence trends from 2022 to 2040.
Results
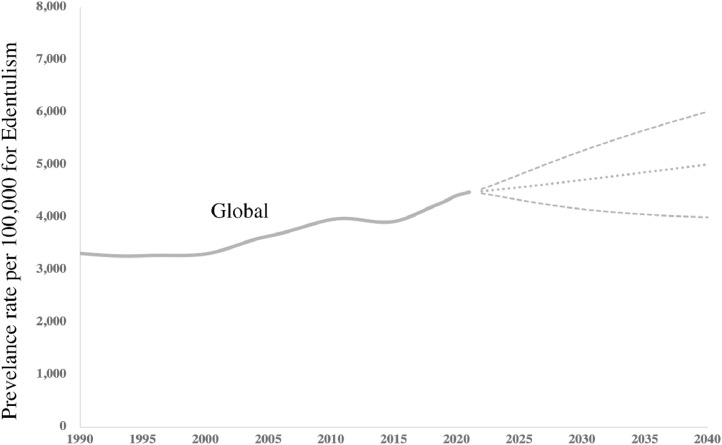
A double increase was found in the number of people with edentulism during the last 30 years. A decrease in the incidence rate of edentulism was found in younger age groups, and a shift in the peak age of prevalence from 70-74 in 1990 to 75-79 in 2021. Females had a higher prevalence rate of edentulism than males globally, with a disproportionate burden in regions of high SDI countries. The global prevalence rate is projected to increase to 5,004 individuals per 100,000 in 2040.
Conclusion
These results indicate that edentulism continues to be a significant global public health concern, particularly as its prevalence is expected to rise with the aging population.
Clinical Relevance
Public and clinical preventative measures against edentulism is imperative for the welling being of the population, especially in female group.
Key words: Tooth loss, Edentulism, Sex disparity, Regional disparity
Introduction
The world is facing a demographic shift towards an increasingly older population due to declining birth rates and increasing life expectancy. According to WHO report in 2022, population aged above 60 years old will account for one sixth of the whole population. Developed countries are the first to experience the trend of population aging, and then this aging trend spreads from developed countries to developing countries. It is estimated the majority (around two-thirds) of the global population aged 60 and above will reside in countries with low- and middle-income levels in 2050, which will cause substantial demand for health care in these countries.1
Edentulism, or complete tooth loss, is defined as loss of all permanent teeth.2 As an irreversible condition, edentulism is usually regarded as the ultimate outcome of oral disease.3 Two microbial diseases including dental caries and periodontal disease were regarded as dominating contributors for edentulism, with additional factors such as genetic factors and traumatic factors also playing a role in this condition.4 As one particular form of disability, edentulism not only significantly impairs the individual's ability to chew food effectively, but it also exerts a notable influence on their overall food intake, thereby affecting their nutritional status.5,6 The repercussions extend beyond the physical realm and into the social domain, potentially leading to speech impairment and social isolation.7,8 This, in turn, can contribute to the emergence of psychological complications such as depression and anxiety9,10 Additionally, it is important to note that edentulism may have an underlying connection with various chronic disease including cardiovascular disease,11 dementia and stroke.12,13 As a result, the actual burden of edentulism is underestimated. Edentulism is largely preventable which can be managed by prevention in caries and periodontal disease.4 Unfortunately, it is often ignored by the public as being regarded as unavoidable as people ages and thus do not be assigned significant importance.
Gender disparity exists in disease epidemiology, pathophysiology, and disease progression.14 Apart from biological factors, traditional gender role shapes the social behaviors including daily routine, food intake and physical activity. As a result, certain diseases are more likely to happen on women, with ischemic heart disease being a typical example.15 Meanwhile, women are more susceptible to the adverse effects of risk factors for heart disease, such as high blood pressure and diabetes.16 Similarly, in a comprehensive review conducted by Sangalli et al. in 2023, it was found that there are notable sex differences in the prevalence and manifestation of oral diseases.17 Men, being less likely to seek medication for oral problems may face an increased risk of poorer oral hygiene which may lead to periodontal disease.18 Additionally, life habits such as drinking and smoking predispose both men and women to developing oral cancers, but men may have a higher risk compared to women due to hormonal differences.18
The GBD dataset continually incorporates new diseases and definitions over time, providing a reliable statistical tool for analyzing the epidemiological trend of oral health.19 A meta-analysis conducted in 2010 showed a decline in both prevalence and incidence of edentulism.20 However, GBD data showed an increase in prevalence and DALYs due to edentulism in the global level in 2015.21 In a recent paper, researchers found that economic status has an impact on the burden of dental caries, severe periodontitis, and edentulism.22
Despite worldwide efforts have been made to lower the burden caused by severe tooth loss and the prevalence of edentulism being examined in several studies, there is lack of detailed and updated evaluation regarding edentulism disparity among different sociodemographic index (SDI) regions and sex, and future prediction of global edentulism is lacking.
Hence, there is a need to reassess the global burden and disparities in edentulism and predict the future epidemiological pattern of edentulism using available high-quality data. This study aims to investigate the difference in global and regional burden of edentulism in both sexes and provide forecast trend based on current data. This study is driven by the following questions:
-
1)
How have the patterns of edentulism burden evolved from 1990 to 2021?
-
2)
To what extend did sex difference exist in the epidemiology of edentulism revealed by incidence, prevalence and disability adjusted life years (DALYs) from the global level?
-
3)
What is the future forecast of edentulism epidemiology in the following 2 decades?
Material and methods
Data source
The epidemiological data regarding oral disorders came from Global Burden of Disease study (GBD) study (2021 update) managed by the Institute of Health Metrics and Evaluation (IHME). As a longitudinal study, GBD data on the global and regional trends in edentulism for all age groups from 1990 to 2021 were gathered in 204 countries and regions around the world. Detailed methods for GBD study were recorded.23 Edentulism is defined as having no teeth in the oral cavity by WHO.2 The dataset provides estimates for health loss due to risk factors, injuries and illness by measuring prevalence, incidence, and DALYs. DALY is generally defined as the sum of Years Lived with Disability (YLD) and Years of Life Lost (YLL) which can reflect the true suffering caused by certain medical conditions compared to prevalence and incidence.24 YLLs (Years of Life Lost) are typically minimal and often not considered in most research focusing on dental conditions. In edentulism, as YLL is too minimal so that it is not considered in GBD study, therefore, DALY is equivalent to YLD in the current study. The disability resulting from edentulism is measured using disability weights, which quantify the impact of specific health conditions on an individual's overall health. These weights are utilized to calculate the years lived with disability (YLD) attributed to edentulism within a particular population.25 Unadjusted age estimates were used to measure the difference in population and represent the actual burden of each region based on their health systems. The SDI is a metric used to assess the social and economic development of a particular region, with implications for health outcomes.26 It is determined by calculating the average values of various factors, including fertility rate among those under 25 years old, mean education levels, mean education for individuals aged 15 and above, and lag distributed income per capita. The index ranges from 0 to 1, with higher values indicating better development. The data displayed in this study is disaggregated by sex and SDI index.26 This study was reported following the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) principles proposed by WHO.27
Statistical analysis
R package (version 4.2.2,) and GraphPad Prism (version 8.0.2, GraphPad Software Inc, USA) was applied in the data display and visualizations. Joinpoint software (version 5.2.0, National Cancer Institute) was used to portray the temporal trends in the age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR) and age-standardized DALY rate of edentulism. The ARIMA model in SPSS Time Series Modeler (IBM, Armonk NY, USA) was applied to estimate the trend of prevalence of edentulism from 2022 to 2040.
Results
Global burden of edentulism
An estimated 0.35 billion (95%UI: 0.30-0.42 billion) people were affected by edentulism, accounting for 4.44% of the whole population. Compared with 1990, the number of people who were affected by edentulism nearly doubled from 1990 to 2021 (0.18 billion vs 0.35 billion). From 1990 to 2021, an upward trend in the prevalence of edentulism was observed. Globally, the prevalence (4,473.26 per 100,000), incidence (336.16 per 100,000), and DALY (121.54 per 100,000) rates in 2021 were higher than the 1990 rates, which were 3309.80 per 100,000 for prevalence, 256.95 per 100,000 for incidence, and 90.41 per 100,000 for DALY (Table 1). Similar trend was also found in periodontal disease with high SDI countries bear a heavier burden (Supplemental Table 1).
Table 1.
Disease burden of edentulism, 1990-2021.
| 1990 |
2021 |
|||||
|---|---|---|---|---|---|---|
| Prevalence rate | Incidence rate | DALY rate | Prevalence rate | Incidence rate | DALY rate | |
| Both sex | ||||||
| Global | 3,309.80 [2,637.93, 4,011.21] | 256.95 [209.73, 310.24] | 90.41 [57.90, 126.48] | 4,473.26 [3,809.13, 5,273.72] | 336.16 [286.56, 394.96] | 121.54 [78.60, 170.70] |
| High SDI | 5,849.51 [4,682.33, 7,186.53] | 411.43 [334.60, 497.63] | 159.01 [101.33, 224.65] | 7,755.30 [6,345.65, 9,336.30] | 508.32 [420.89, 610.22] | 209.34 [137.18, 294.07] |
| High-middle SDI | 4,408.58 [3,528.44, 5,354.15] | 341.57 [277.46, 415.99] | 120.40 [76.90, 169.68] | 6,401.88 [5,407.07, 7,566.06] | 487.06 [408.10, 579.94] | 173.82 [114.21, 244.40] |
| Middle | 2,680.31 [2,122.48, 3,240.85] | 227.37 [184.82, 274.18] | 73.57 [47.34, 102.43] | 4,762.26 [4,106.66, 5,562.98] | 379.06 [325.03, 443.03] | 129.73 [84.24, 182.60] |
| Low-middle SDI | 2,079.07 [1,648.24, 2,566.03] | 167.44 [136.04, 203.36] | 56.79 [36.31, 80.01] | 2,670.08 [2,277.35, 3,123.26] | 211.77 [183.20, 244.23] | 72.66 [46.51, 101.04] |
| Low SDI | 1,518.19 [1,183.65, 1,853.72] | 114.22 [92.79, 137.38] | 41.64 [25.60, 58.65] | 1,465.93 [1,200.48, 1,736.56] | 110.76 [94.55, 128.20] | 40.36 [25.02, 56.84] |
| Male | ||||||
| Global | 2,708.55 [2,137.96, 3,301.37] | 224.46 [181.95, 274.13] | 74.47 [47.61, 104.30] | 3,735.89 [3,152.17, 4,458.31] | 297.65 [251.55, 352.94] | 102.27 [65.82, 144.54] |
| High SDI | 4,676.54 [3,689.10, 5,789.50] | 362.76 [292.60, 444.89] | 127.86 [81.60, 180.63] | 6,657.57 [5,379.82, 8,081.59] | 463.35 [378.91, 560.57] | 180.89 [116.51, 254.70] |
| High-middle SDI | 3,381.04 [2,678.06, 4,128.25] | 282.30 [228.01, 347.02] | 93.02 [59.31, 130.39] | 5,054.60 [4,228.49, 6,054.02] | 417.17 [346.35, 502.23] | 138.35 [90.06, 197.47] |
| Middle SDI | 2,208.03 [1,738.05, 2,683.69] | 198.24 [158.98, 242.34] | 60.99 [38.99, 85.44] | 3,893.31 [3,316.57, 4,601.71] | 330.48 [280.52, 388.87] | 106.80 [69.16, 151.03] |
| Low-middle SDI | 1,930.17 [1,525.60, 2,393.08] | 158.31 [128.24, 193.23] | 53.05 [33.90, 75.05] | 2,350.11 [1,992.28, 2,776.18] | 192.60 [165.79, 222.66] | 64.49 [41.12, 90.08] |
| Low SDI | 1,468.08 [1,147.24, 1,794.83] | 110.83 [90.35, 133.46] | 40.57 [24.98, 56.99] | 1,384.96 [1,137.35, 1,645.38] | 105.08 [89.59, 122.12] | 38.49 [23.68, 54.47] |
| Female | ||||||
| Global | 3,919.65 [3,134.64, 4,727.50] | 289.91 [237.74, 347.67] | 106.57 [68.30, 149.40] | 5,215.77 [4,463.23, 6,106.29] | 374.93 [321.32, 437.05] | 140.94 [91.56, 197.18] |
| High SDI | 6,988.98 [5,610.15, 8,538.33] | 458.70 [376.62, 549.69] | 189.26 [122.14, 267.68] | 8,847.71 [7,303.78, 10,619.62] | 553.08 [460.46, 658.28] | 237.66 [157.53, 333.89] |
| High-middle SDI | 5,426.45 [4,359.19, 6,576.72] | 400.28 [328.04, 483.49] | 147.52 [94.53, 207.94] | 7,751.41 [6,555.45, 9,071.44] | 557.08 [469.94, 659.62] | 209.34 [137.56, 291.41] |
| Middle | 3,170.02 [2,525.82, 3,828.19] | 257.57 [210.87, 307.91] | 86.61 [55.80, 120.40] | 5,643.96 [4,884.48, 6,560.72] | 428.36 [369.34, 494.42] | 153.00 [99.55, 214.64] |
| Low-middle SDI | 2,233.47 [1,775.15, 2,744.26] | 176.92 [144.09, 214.24] | 60.66 [38.80, 85.32] | 2,993.51 [2,574.36, 3,497.65] | 231.15 [200.55, 265.76] | 80.92 [52.12, 111.87] |
| Low SDI | 1,568.97 [1,225.07, 1,917.14] | 117.65 [95.14, 141.56] | 42.73 [26.12, 60.33] | 1,547.03 [1,263.21, 1,835.31] | 116.45 [99.12, 134.49] | 42.24 [26.21, 59.53] |
DALY, disability adjusted life years; SDI, sociodemographic index.
The change with age in the edentulism prevalence and incidence is present in Figure 1 and Supplemental Table 3. Overall, the global prevalence rate for edentulism for both sexes have a steady growth when people age. The trend of incidence rate of edentulism in 2021 present an S-shaped trend with age which was quite similar to that in 1990: the incidence rate gradually increased after adulthood and reached its peak between 70-80 years old, and then gradually declined. The difference lies in that the peak value decreased slightly from 1,769.42 per 100,000 in 1990 to 1,707.81 per 100,000 in 2021. Furthermore, the peak incidence of edentulism in 2021 has shifted to a later age period, specifically from 70-74 to 75-79 (as shown in Figure 1). A significant decline in the incidence rate of edentulism has been observed over the past 3 decades among these young seniors, while for those aged above 85, a slight increase in the incidence rate was reported. Since periodontal disease is usually regarded as one main risk factor for tooth loss, we further investigated the prevalence and incidence rate trend of periodontal disease during the last 3 decades. Results have shown that the prevalence of periodontal disease has a gradual increase from adulthood and peak at the age of 50-59 with a descending trend afterwards. In 2021, the incidence of periodontal disease across all age groups fluctuated around the same level as in 1990 which had an increasing trend starting from adulthood and stabilize after middle age (Supplemental Figure 1).
Fig. 1.
Global age distribution on the prevalence, incidence and DALY rate of Edentulism, and DALY rate for periodontitis in 2021. A, Prevalence and incidence rates of edentulism in 2021 B, Incidence rate change of edentulism in 1990 vs 2021. C) DALY rate per 100,000 for edentulism in different age groups D) DALY rate per 100,000 for periodontal disease in different age groups.
Inequality of burden in edentulism
The global burden of edentulism was substantial for countries with different socio-demographic development in the investigated years. Among five SDI regions, the highest prevalence rate of edentulism exists in high-SDI countries for both male and female (6,657.57 [5,379.82, 8,081.59] for men and 8847.71 [7,303.78, 10,619.62] for women per 100,000 individuals). Interestingly, the prevalence showed an uneven distribution that did not match with social economic development (Table 1). Developed regions such as high SDI countries showed higher prevalence (7,755.30 per 100,000), incidence (508.32 per 100,000) and DALY (209.34 per 100,000) rate compared with global level. Low SDI countries had the least prevalence (1,465.93 per 100,000), incidence (110.76 per 100,000) and DALY (41.64 per 100,000) rate compared with other regions in 2021.
More than half of the burden was borne by adult females who account for 58.10% of the whole edentulous population (calculated from Supplemental Table 2). For example, the DALY rate for women was 140.94 per 100,000 individuals in 2021, while it was 102.27 per 100,000 for men (Table 1). In 2021, the burden of edentulism in female was disproportionately higher in regions of high SDI countries, with over 5 times the rate compared to low SDI countries (DALY 237.66 vs 42.24 per 100,000) (Table 1).
As shown in Figure 2 and Supplemental Table 4, women had a generally higher incidence of edentulism than men in around four-fifths of regions worldwide. Notably, certain countries in the Northern Hemisphere, including Cuba, Estonia, Latvia, Russia, and Ukraine, exhibit a larger gap between the incidence of edentulism in females and males. In contrast, the higher incidence of edentulism in men was primarily observed in a smaller proportion of regions, mainly located in the Middle East, including the United Arab Emirates, Bahrain, Iran, Kuwait, Libya, Saudi Arabia, Syria, and Uzbekistan.
Fig. 2.
Global map of the incidence rate of edentulism for both men and women in 2021.
Among all age groups, the burden of edentulism in females, as measured by DALY, was higher than that in males, with a particularly significant gap observed in the 75-84 age group (928.19 [617.10, 1,317.51] vs 789.67 [528.84, 1,153.38]). However, the trend is opposite in periodontal disease, where men generally bear a slightly heavier burden than women which is reflected by DALY (88.12 [35.33, 180.49] vs 86.83 [34.93, 177.07]) (Figure 1).
Joinpoint regression analysis
The age-standardized average annual percent change (AAPC) and annual percent change (APC) using joinpoint regression analysis is displayed in Table 2. A significant decreased AAPC in the incidence rate was observed in both males (−0.24 [−0.35, −0.14]) and females (−0.24 [−0.31, −0.17]) using the standardized age. The prevalence and DALY trend is on a similar trend: gradual decreased AAPC in the ASPR was observed in both males (−0.30 [−0.36, −0.23]) and females (−0.27 [−0.34, −0.21]) from 1990 to 2021; and the AAPC for DALY is (−0.29 [−0.36, −0.23]) for male and (−0.28 [−0.35, −0.21]) for female (Table 2).
Table 2.
APC and AAPC of incidence, prevalence, DALY of global edentulism among males and females.
| Sex | Incidence rate |
Prevalence rate |
DALY rate |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | APC [95%CI] | AAPC [95%CI] | Period | APC [95%CI] | AAPC [95%CI] | Period | APC [95%CI] | AAPC [95%CI] | |
| Both | 1990-1994 | −1.13 [−1.53, −0.92] | −0.23 [−0.26, −0.21] | 1990-1993 | −1.37 [−1.77, −1.08] | −0.29 [−0.31, −0.27] | 1990-1993 | −1.34 [−1.73, −1.07] | −0.29 [−0.31, −0.27] |
| 1994-2000 | −0.51 [−0.72, −0.29] | 1993-2000 | −0.83 [−0.91, −0.62] | 1993-2000 | −0.85 [−0.92, −0.64] | ||||
| 2000-2006 | 0.35 [−0.30, 0.46] | 2000-2004 | 0.77 [0.59, 1.00] | 2000-2004 | 0.81 [0.63, 1.02] | ||||
| 2006-2010 | 0.70 [0.52, 0.91] | 2004-2010 | 0.34 [0.14, 0.42] | 2004-2010 | 0.35 [0.19, 0.43] | ||||
| 2010-2015 | −2.34 [−2.46, −2.22] | 2010-2015 | −1.79 [−1.89, −1.68] | 2010-2015 | −1.76 [−1.85, −1.66] | ||||
| 2015-2019 | 1.66 [1.52, 1.89] | 2015-2021 | 0.82 [0.72, 0.91] | 2015-2021 | 0.76 [0.66, 0.84] | ||||
| 2019-2021 | 0.36 [−0.03, 0.85] | ||||||||
| Male | 1990-1994 | −1.30 [−1.53, −1.07] | −0.24 [−0.35, −0.14] | 1990-1994 | −1.41 [−1.65, −1.18] | −0.30 [−0.36, −0.23] | 1990-1994 | −1.39 [−1.63, −1.15] | −0.29 [−0.36, −0.23] |
| 1994-2007 | 0.05 [0.01, 0.09] | 1994-1999 | −0.19 [−0.43, 0.05] | 1994-1999 | −0.22 [−0.47, 0.02] | ||||
| 2007-2010 | 0.71 [−0.03, 1.46] | 1999-2010 | 0.28 [0.22, 0.34] | 1999-2010 | 0.32 [0.26, 0.38] | ||||
| 2010-2015 | −2.50 [−2.72, −2.27] | 2010-2015 | −2.23 [−2.46, −1.99] | 2010-2015 | −2.21 [−2.45, −1.97] | ||||
| 2015-2019 | 1.68 [1.30, 2.05] | 2015−2021 | 0.94 [0.81, 1.07] | 2015-2021 | 0.89 [0.76, 1.02] | ||||
| 2019-2021 | 0.46 [−0.28, 1.20] | ||||||||
| Female | 1990-2000 | −1.02 [−1.08, −0.97] | −0.24 [−0.31, −0.17] | 1990-2000 | −1.19 [−1.24, −1.13] | −0.27 [−0.34, −0.21] | 1990-2000 | −1.20 [−1.26, −1.15] | −0.28 [−0.35, −0.21] |
| 2000-2010 | 0.69 [0.62, 0.75] | 2000-2004 | 1.01 [0.66, 1.36] | 2000-2004 | 1.04 [0.67, 1.41] | ||||
| 2010-2015 | −2.19 [−2.40, −1.97] | 2004-2010 | 0.41 [0.26, 0.57] | 2004-2010 | 0.41 [0.24, 0.58] | ||||
| 2015-2019 | 1.64 [1.28, 2.00] | 2010-2015 | −1.46 [−1.67, −1.24] | 2010-2015 | −1.42 [−1.65, −1.19] | ||||
| 2019-2021 | 0.29 [−0.41, 1.00] | 2015-2021 | 0.72 [0.60, 0.84] | 2015-2021 | 0.65 [0.53, 0.78] | ||||
AAPC, average annual percent change; APC, annual percent change; CI, confidence interval.
Trends in the future
Statistical forecast using ARIMA model based on data 1990 to 2021 is displayed in Figure 3, Supplemental figure 2, and Supplemental Table 5 to 10. The results indicate a consistent increase in the prevalence of edentulism, projected to reach 5,004 per 100,000 globally by 2040. The upper confidence limit for this projection is 6,010, while the lower limit is 3,999. This represents an increase of 11.87% compared to the prevalence in 2021.
Fig. 3.
Trend in the global prevalence of edentulism from 1990 to 2021 and predictions to 2040. Confidence intervals were shown in dotted lines (Ljung Box Q, P = .890).
Discussion
This study aimed to provide a reassessment of the edentulism today as well as generate credible estimates of the prevalence trend associated with edentulism from 2022 to 2040. The findings were able to provide insight into the changes of global prevalence, incidence and DALY rate in edentulism over the last 3 decades. Inequality of edentulism among different regions and sexes was explored. An estimation of the future trend of edentulism worldwide was provided. These finding may have important implication for policymakers, dentists and the public.
As a global problem, edentulism affects the living quality of life, especially the elderly group. It significantly impacts individuals' quality of life by limiting their ability to chew certain foods and diminishing their eating pleasure.28 Moreover, individuals facing eating difficulties may avoid social engagements, such as dining out with friends, thereby affecting their overall functioning.29
Despite efforts made in the last few decades, the burden of edentulism remains to be a significant challenging worldwide. With the global population growth and the trend of population aging, the prevalence of edentulism has been a steadily increasing globally, with a striking increase in high SDI countries. This trend is mainly related to the global trend of an increased number of people aged above 65 years and extended life span.30 The findings in this study align with Martin's research, which indicated that individuals aged above 60 years carry the 23% of the global burden of disease.31 In regions with high SDI, the high burden of edentulism may be attributed to longer life expectancies, which are the outcome of advancements in dental care and healthcare in general, as well as improved living standards among elderly population. Conversely, underprivileged regions may lack sufficient access to overall healthcare resulting in diminished life expectancies as indicated by measurements such as life disparity and healthy life disparity.32 This can be reflected in a relatively lower burden of edentulism in low SDI countries. Furthermore, improved healthcare access may result in a rise in dental extractions, potentially leading to a temporary upsurge in edentulism which likely observed on High SDI regions. Additionally, variations in dietary shifts between countries in different SDI regions may contribute to increased rates of caries and periodontal disease in less developed nations in recent years.33,34 This stands in contrast to more advanced countries that have already undergone similar dietary transitions.
Although the unadjusted depiction and prediction of edentulism shows a different trend from age-adjusted measures such as incidence, prevalence, and DALY, which indicate a decreasing trend in joinpoint analysis, this finding further confirms the efforts we have achieved and also emphasizes the significance of age in the epidemiology of edentulism. It is speculated that the rapid advancement in global economic development and healthcare policies played a significant role in the turning points in the joinpoint analysis. Understanding the real picture of the epidemiology of edentulism can help us better comprehend the occurrence and progression of this condition and develop appropriate prevention and treatment strategies.
In 2003, WHO put forward a goal for oral health to be achieved by 2020, which aimed to promote oral health and reduce oral disease to minimize its impact on physical and physiological health.35 Since then, global policies have been adopted and successful coordinated efforts have been made towards this goal.36 It is not surprising to witness a significant decrease in the occurrence of edentulism among the younger elderly population, as well as a shift in the peak incidence of edentulism. The slightly increased incidence of edentulism in 2021 among individuals aged above 80 years can be attributed to population growth and a higher percentage of the aged population compared with 1990.37
On a global scale, the incidence rate of edentulism is typically higher in females than in males. We observed disparities in the epidemiological characteristics of edentulism between two sexes, despite the lack of significant differences identified in the joinpoint analysis between males and females. This can partially be explained by the fact that women outlive than men by an average of 4.8 years, and there is a proportionately the distinctively imbalanced ration of female to male above 80 years.37 On the other hand, attitudes and practices towards oral health play a crucial role in determining overall oral health outcomes. It is worth noting that many individuals with edentulism were born in the mid-20th century and had restricted access to oral education and opportunities. When combined with lower incomes due to insufficient job opportunities for women, these factors may potentially have a more adverse impact on women. Other socio-historical factors, including cultural norms and gender roles, have also shaped attitudes towards oral health and contributed to disparities in tooth loss between men and women. Traditional societal expectations and limited access to oral healthcare for women may have led to neglect of oral health needs. Additionally, the gap in edentulism rates can also be influenced by susceptibility to tooth loss instead of life habits. While men are generally less likely to visit dentists regularly and may have a worse oral condition,18 they appear to be less likely to develop edentulism compared with female. Considering the equal distribution in the prevalence of periodontitis in both sexes (Supplemental Figure 1), the underlying reason why women bear more burden in edentulism than men could be attributed to that the decreased bone density and subsequent higher risk for osteoporosis. This makes women more susceptible to tooth loss.38
In terms of inequality of disease, the Commission on Social Determinants of Health (CSDH) framework was established by WHO in 2005 in order to combat inequality in health. They have identified that social determinants of health encompass structural factors that occur within specific socioeconomic and political contexts which shapes social stratification and influences individuals' socioeconomic status. The determinants, which are deeply rooted in political and historical factors, ultimately impact health inequality and well-being by influencing intermediate factors such as the healthcare system. This in turn highlights the importance of policy efforts to address health inequalities.39,40
Our findings indicate that the current measures implemented to prevent edentulism have been effective. However, given the global aging trend, stronger interventions are needed to alleviate the burden caused by edentulism. The disparity among sexes and regions indicate that resources should be allocated in a more targeted and equitable manner with more attention paid to underprivileged areas and groups. Additionally, the preventive measures taken for periodontal diseases appear to be less effective as depicted in the rising incidence of periodontal disease in younger adults and the stable incidence in other age groups. Thus, it is crucial to make appropriate policy adjustments to address this imbalance, improve oral health outcomes, and implement more effective measures for preventing and treating periodontal disease to prevent its progression to edentulism.
Due to the reliability of the data source, the description and prediction of edentulism provides a comprehensive ongoing picture of its epidemiology. However, this study has some limitation worth mentioning. Firstly, it is important to note that the data used in this study is secondary data sourced from the GBD database. While the GBD database provides valuable information, it may have limitations in terms of comprehensively capturing all types of oral diseases and the associated risk factors that contribute to edentulism. Secondly, although the data already covered almost all regions and countries around the world, there are still some countries where the data is lacking, which may introduce bias when depicting the real disparity among countries and regions. Thirdly, when regional trends are segregated by SDI and sex, it may obscure the inequality among countries and therefore may not accurately reflect the situation within an individual country. Additionally, the Global Burden of Disease (GBD) study currently only provides estimates for edentulism, while no data regarding partial tooth loss is provided. Considering disability and burden caused by partial tooth loss. It is important to take into account factors such as the use and necessity of prostheses in future surveys. These considerations are crucial for future studies to have a comprehensive estimation for the burden caused by edentulism.
Conclusion
This study has reassessed the epidemiology of edentulism and estimates its future trends. Over the past 3 decades, the prevenance and DALY of edentulism have continued to rise, affecting the quality of life of aging individuals. The study emphasizes the disproportionately higher burden of edentulism in high SDI countries and among females. Despite some preliminary achievements, a substantial burden regarding edentulism is expected in the next 2 decades. Therefore, prevention strategies, including early treatment of dental caries and periodontitis, should be launched to prevent edentulism, with a greater focus on the female population. This study highlights the urgent need for greater efforts to address the factors contributing to edentulism among the population. Policymakers should take notice of the realization and reduction in health disparities among the world's population.
Competing interests
The authors declare that they no competing interests.
Acknowledgments
Ethic approval
Ethical approval has been waived for the current study since all data used comes from the GBD dataset, which has already been approved by the research ethics board at the University of Washington. All procedures were conducted following the Free-of-Charge Non-Commercial-User Agreement from the IHME website.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Hui Min Chen and Kuo Shen contributed to the original concept, methodology and original draft. Lin Ji contributed to the data collection and formal analysis. Colman McGrath contributed to data interpretation and revision of the manuscript. Hui Chen supervised the whole study process. All authors read and approved the final manuscript. Hui Min Chen and Kuo Shen contributed equally to this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.identj.2024.11.022.
Appendix. Supplementary materials
References
- 1.World Health Organization. Ageing and health. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 25 November, 2024.
- 2.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Cunha-Cruz J, Hujoel PP, Nadanovsky P. Secular trends in socio-economic disparities in edentulism: USA, 1972–2001. J Dent Res. 2007;86(2):131–136. doi: 10.1177/154405910708600205. [DOI] [PubMed] [Google Scholar]
- 4.Cooper LF. The current and future treatment of edentulism. J Prosthodont. 2009;18(2):116–122. doi: 10.1111/j.1532-849X.2009.00441.x. [DOI] [PubMed] [Google Scholar]
- 5.Gaewkhiew P, Sabbah W, Bernabé E. Does tooth loss affect dietary intake and nutritional status? A systematic review of longitudinal studies. J Dent. 2017;67:1–8. doi: 10.1016/j.jdent.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 6.hui Xu K, L Li, lin Jia S, Li Q, xin Hao J, Ma S, et al. Association of tooth loss and diet quality with acceleration of aging: evidence from NHANES. Am J Med. 2023;136(8):773–779.e4. doi: 10.1016/j.amjmed.2023.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Kiuchi S, Cooray U, Aida J, Osaka K, Chan A, Malhotra R, et al. Effect of tooth loss on cognitive function among older adults in Singapore. J Dent Res. 2023;102(8):871–878. doi: 10.1177/00220345231172109. [DOI] [PubMed] [Google Scholar]
- 8.Lee Ka Yi, Chan Charlotte Cheuk Kwan, Yip Ching, Li Joyce Tin Wing, Hau Cheuk Fung, Poon Sarah Suen Yue, et al. Association between tooth loss-related speech and psychosocial impairment with cognitive function: a pilot study in Hong Kong's older population. J of Oral Rehabilitation. 2024;51(8):1475–1485. doi: 10.1111/joor.13718. [DOI] [PubMed] [Google Scholar]
- 9.Özhayat EB. Influence of self-esteem and negative affectivity on oral health-related quality of life in patients with partial tooth loss. Community Dent Oral Epidemiol. 2013;41(5):466–472. doi: 10.1111/cdoe.12032. [DOI] [PubMed] [Google Scholar]
- 10.Schierz O, Baba K, Fueki K. Functional oral health-related quality of life impact: a systematic review in populations with tooth loss. J Oral Rehabil. 2021;48(3):256–270. doi: 10.1111/joor.12984. [DOI] [PubMed] [Google Scholar]
- 11.Dai J, Li A, Liu Y, Chen Y, Tjakkes GHE, Visser A, et al. Denture wearing status, cardiovascular health profiles, and mortality in edentulous patients: a prospective study with a 27-year follow-up. J Dent. 2022;126 doi: 10.1016/j.jdent.2022.104287. [DOI] [PubMed] [Google Scholar]
- 12.Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. 2003;34(1):47–52. doi: 10.1161/01.str.0000052974.79428.0c. [DOI] [PubMed] [Google Scholar]
- 13.Thomson WM, Barak Y. Tooth loss and dementia: a critical examination. J Dent Res. 2021;100(3):226–231. doi: 10.1177/0022034520957233. [DOI] [PubMed] [Google Scholar]
- 14.Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL, et al. Sex and gender: modifiers of health, disease, and medicine. The Lancet. 2020;396(10250):565–582. doi: 10.1016/S0140-6736(20)31561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's & Dementia. 2011;7(3):270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018:k4247. doi: 10.1136/bmj.k4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sangalli L, Souza LC, Letra A, Shaddox L, Ioannidou E. Sex as a biological variable in oral diseases: evidence and future prospects. J Dent Res. 2023;102(13):1395–1416. doi: 10.1177/00220345231197143. [DOI] [PubMed] [Google Scholar]
- 18.Lipsky MS, Su S, Crespo CJ, Hung M. Men and oral health: a review of sex and gender differences. Am J Mens Health. 2021;15(3) doi: 10.1177/15579883211016361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dye BA. The global burden of oral disease: research and public health significance. J Dent Res. 2017;96(4):361–363. doi: 10.1177/0022034517693567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. 2014;93(7_suppl):20S–28S. doi: 10.1177/0022034514537828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kassebaum NJ, Smith AGC, Bernabé E, Fleming TD, Reynolds AE, Vos T, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96(4):380–387. doi: 10.1177/0022034517693566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.GBD 2017 Oral Disorders Collaborators. Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–373. doi: 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.GBD 2019 Ageing Collaborators Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the global burden of disease 2019 study. BMJ. 2022 doi: 10.1136/bmj-2021-068208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray CJL, Acharya AK. Understanding DALYs. J Health Econ. 1997;16(6):703–730. doi: 10.1016/s0167-6296(97)00004-0. [DOI] [PubMed] [Google Scholar]
- 25.The Global Burden of Disease [GBD] (2021). Disease, injury, and risk factsheets. Available from: https://www.healthdata.org/research-analysis/diseases-injuries/factsheets Accessed 25 November 2024.
- 26.Global Burden of Disease Collaborative Network. Global burden of disease study 2019 (GBD 2019) socio-demographic index (SDI) 1950–2019. [object Object]; 2020 Accessed 17 April 2024. Available from: http://ghdx.healthdata.org/record/ihme-data/gbd-2019-fertility-estimates-1950-2019
- 27.Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 28.Hewlett SA, Yawson AE, Calys–Tagoe BN, Naidoo N, Martey P, Chatterji S, et al. Edentulism and quality of life among older Ghanaian adults. BMC Oral Health. 2015;15(1):48. doi: 10.1186/s12903-015-0034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polzer I, Schwahn C, Völzke H, Mundt T, Biffar R. The association of tooth loss with all-cause and circulatory mortality. Is there a benefit of replaced teeth? A systematic review and meta-analysis. Clin Oral Invest. 2012;16(2):333–351. doi: 10.1007/s00784-011-0625-9. [DOI] [PubMed] [Google Scholar]
- 30.Veron J, Kinsella K, Velkoff VA. An aging world: 2001. Population (French Edition) 2002;57(6):928. [Google Scholar]
- 31.Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O'Donnell M, Sullivan R, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi: 10.1016/S0140-6736(14)61347-7. [DOI] [PubMed] [Google Scholar]
- 32.Zheng Y, Canudas-Romo V. Global health inequality: analyses of life disparity and healthy life disparity. Eur J Public Health. 2024;34(2):225–229. doi: 10.1093/eurpub/ckae010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cui Y, Tian G, Li R, Shi Y, Zhou T, Yan Y. Epidemiological and sociodemographic transitions of severe periodontitis incidence, prevalence, and disability-adjusted life years for 21 world regions and globally from 1990 to 2019: an age-period-cohort analysis. J Periodont. 2023;94(2):193–203. doi: 10.1002/JPER.22-0241. [DOI] [PubMed] [Google Scholar]
- 34.Wen PYF, Chen MX, Zhong YJ, Dong QQ, Wong HM. Global burden and inequality of dental caries, 1990 to 2019. J Dent Res. 2022;101(4):392–399. doi: 10.1177/00220345211056247. [DOI] [PubMed] [Google Scholar]
- 35.Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J. 2003;53(5):285–288. doi: 10.1111/j.1875-595x.2003.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 36.Petersen PE. Global policy for improvement of oral health in the 21st century – implications to oral health research of World Health Assembly 2007, World Health Organization. Comm Dent Oral Epid. 2009;37(1):1–8. doi: 10.1111/j.1600-0528.2008.00448.x. [DOI] [PubMed] [Google Scholar]
- 37.Department of Economic and Social Affairs Population Division. World population ageing, 2019 highlights. New York: United Nations;
- 38.Nguyen TV, Center JR, Eisman JA. Osteoporosis in elderly men and women: effects of dietary calcium, physical activity, and body mass index. J Bone Mineral Res. 2000;15(2):322–331. doi: 10.1359/jbmr.2000.15.2.322. [DOI] [PubMed] [Google Scholar]
- 39.Solar O, Irwin AA. Conceptual framework for action on the social determinants of health. World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 40.Commission on Social Determinants of Health . Final Report of the Commission on Social Determinants of Health. World Health Organization; Geneva, Switzerland: 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.