Abstract
Cryptococcosis is an opportunistic mycosis caused by Cryptococcus, mainly affecting the immunocompromised. We report a case of pulmonary cryptococcosis within a 31-year-old immunocompetent patient admitted for painful chest swelling evolving for 4 months prior to admission. The chest X-Ray showed a rounded pulmonary opacity. The chest ultrasound revealed a pulmonary abscess diffusing under the skin. Direct examination using the Indian ink and the May-Grunwald Giemsa staining revealed encapsulated yeasts in the pus. The Culture of the pus on the Sabouraud medium with chloramphenicol confirmed the presence of Cryptococcus neoformans. Cryptococcal antigen was positive. This case reminds us that cryptococcosis should be considered even without immunosuppression.
Keywords: Cryptococcosis, Lung, Cryptococcus neoformans, Immunocompetent, Cote d’Ivoire
1. Introduction
Cryptococcosis is an opportunistic mycotic infection caused by encapsulated yeasts of the genus Cryptococcus [1] which are, Cryptococcus neoformans and Cryptococcus gattii [2]. This mycosis often affects immunocompromised patients, particularly those with human immunodeficiency virus (HIV) [3,4], and frequently manifests as neuromeningeal cryptococcosis [2]. However, pulmonary cases in immunocompetent patients are increasingly reported, albeit rarely [5].
These cases pose a diagnostic challenge as the clinical and radiological manifestations may mimic other pathologies, such as tuberculosis, pulmonary neoplasia, pneumonia, abscesses and other pulmonary mycoses [6]. Nevertheless, pulmonary nodules are the most common radiological features of pulmonary cryptococcosis [6,7]. The aim of this report was to describe a rare and fatal case of pulmonary cryptococcosis within an apparently immunocompetent patient.
2. Case
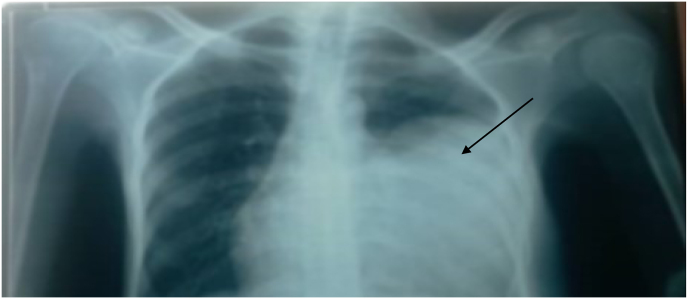
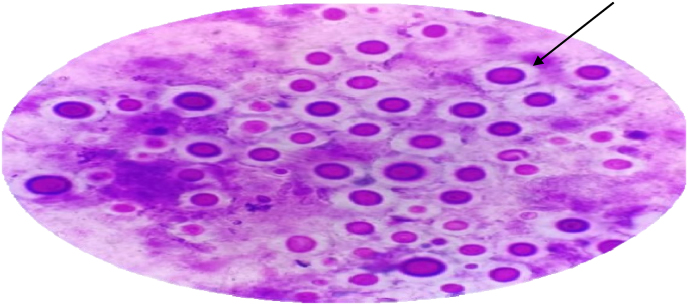
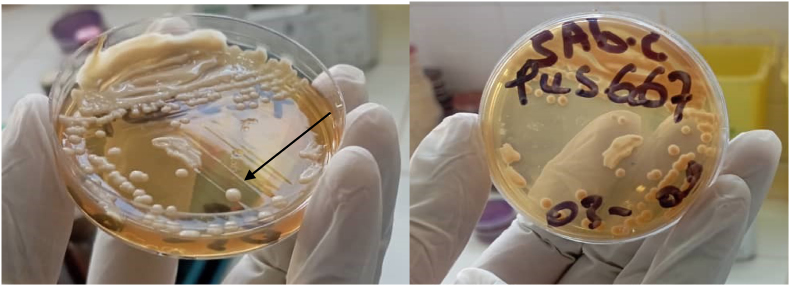
A male patient, aged 31, with a polyester technician profession with no medical background, corticosteroid use or immunosuppressive therapy, was referred to the thoracic surgery department on September 30, 2024, which was defined as day zero (day 0) for the management of a left thoracic swelling (Fig. 1) associated with left thoracic pain of moderate intensity evolving for four months (- day 120). , In addition to the swelling and chest pain, he reportedly showed progressive weight loss, asthenia, and anorexia. He used self-medication of paracetamol and unspecified traditional therapy. At the day 0 [at the admission], the clinical features were characterized by a large, painful, fluctuating, and warm thoracic mass associated with an altered general condition. His respiratory rate was normal at 19 cycles per minute with 98 % saturation, and his heart rate at 92 beats per minute. The chest X-ray (Fig. 2A) revealed a large, well-limited, homogeneous, rounded opacity of watery tone occupying the lower 2/3 of the left pulmonary hemichamber. It rose the suspicion of a lung cancer. The chest ultrasound examination of the swelling highlighted an abscessed lung with subcutaneous diffusion. The chest CT confirmed these observations, revealing a voluminous intrapulmonary mass with infiltration of adjacent tissues (Fig. 2B). The patient HIV negative along with leukocytes at 2098/mm3, platelets at 637,000/mm3, hemoglobin at 4.4 g/dl, and blood glucose at 0.9g/l. At day +1 Ultrasound-guided fine needle aspiration of the abscessed mass yielded a light-brown and squinty fluid. At this stage, given the suspicion of a bacterial or parasitic abscess, the patient benefited from antibiotic treatment (ceftriaxone 2g daily parenterally) combined with metronidazole 500mg three times per day. Etiological investigation of the puncture fluid in the parasitology-mycology laboratory revealed encapsulated yeasts characteristic of Cryptococcus on direct examination under an optical microscope, using Indian ink. MGG staining of the pus revealed yeasts surrounded by a clear halo (Fig. 3). The culture on Sabouraud medium enriched in chloramphenicol was positive after 2 days (Fig. 4), and thus, confirming the presence of the Cryptococcus neoformans. The cryptococcal antigen test performed on pus using the latex agglutination technique with the pastorex™ crypto plus test was also positive. The diagnosis of pulmonary cryptococcosis was made at day +3, but unfortunately the patient had already left hospital after a three-day stay against medical advice, before the diagnosis was made, due to lack of financial means. He died three days after the discharge.
Fig. 1.
A clinical feature of cryptococcosis pulmonary: a large swelling in the left hemithorax of a young male.
Fig. 2A.
Radiological aspects: Voluminous and homogeneous opacity occupying the lower 2/3 of the left pulmonary hemichamber, raising the suspicion of a pulmonary tumor or cyst on radiography.
Fig. 2B.
Voluminous left pulmonary hyperdensity on thoracic CT scan.
Fig. 3.
(MGG, 40 X). Yeasts measuring 4–8 μm in diameter surrounded by a clear halo.
Fig. 4.
Culture (Sabouraud medium enriched in chloramphenicol): the growth of yeasts within 48 hours at 37 °C.
3. Discussion
The pulmonary cryptococcosis is an invasive opportunistic mycosis which is common in the immunocompromised patients. Although the patient was not immunosuppressed by HIV, it should be remembered that this type of infection generally occurs in debilitated patients. It is therefore likely that an underlying cause of immunosuppression was present, but that we were unable to identify it due to logistical difficulties, a lack of research resources at our level, and the fact that the patient was discharged against medical advice without wishing to undergo further investigations. In the absence of evidence of this potential cause of immunosuppression, we consider him immunocompetent on the basis of his HIV seronegativity. It is also increasingly reported in immunocompetent patients [8]. In China, a revealed that 60 % of cases of pulmonary cryptococcosis were diagnosed in immunocompetent patients who were HIV negative [9]. In the literature, the most frequent radiographic findings are either single or multiple peripheral nodules [[6], [7], [8]]. The clinical description of pulmonary cryptococcosis in HIV-uninfected individuals is non-specific and rather limited due to the rarity of the disease itself [10]. Chest imaging, however, plays an important role in the diagnosis of this disease [11]. Therefore, this case highlights the diagnostic and management challenges Indeed, prior to the mycological results, the three hypotheses for this mass were a pulmonary abscess, a chest wall cyst and a lung carcinoma. tumor associated with pulmonary cryptococcosis can easily be confused with cancer or pulmonary abscess [7], and environmental risk factors, such as exposure to bird droppings, may explain the occurrence of infection in non-immunocompromised subjects. In Côte d'Ivoire, the Cryptococcus is frequently isolated in urban and rural environments, where humidity and heat favor its proliferation. The diagnostic certitude depends on direct mycological examinations which are essential in our case. As a result, the Indian ink and the Sabouraud medium identified the encapsulated yeasts, particularly Cryptococcus neoformans. A positive latex agglutination test for cryptococcal antigen reinforced the diagnosis. The treatment of isolated pulmonary cryptococcosis without signs of severity is based on fluconazole (200–400 mg per day) for 3–6 months in the immunocompetent patients [12]. The prognosis of this disease is good in immunocompetent patients with a very few recurrences if treated early [12]. It is important to note that the patient's death cannot be ruled out or directly attributed to cryptococcal infection. However, several factors could have been involved: his severe anemia (Hb 4.4 g/dL), for which a blood transfusion could not be administered, could have led to his death, or the large abscessed thoracic mass, which had already spread to surrounding tissues and could not be drained, could have led to septicemia by spreading the infection into the bloodstream, or compressed pulmonary structures, causing obstruction with hypoxia and respiratory failure responsible for death. In any event, cryptococcal lung disease cannot be exclusively blamed for the patient's death, but complications and an undiagnosed underlying cause could be responsible.
The pulmonary cryptococcosis is rare in immunocompetent patients. It is probably underdiagnosed due to its non-specific symptoms and the increased frequency of other pulmonary infections. The pulmonary cryptococcosis should be carefully investigated to rule out lung cancer, particularly in endemic regions. The early diagnosis of this disease and its adequate antifungal treatment significantly improve the prognosis of the patient.
CRediT authorship contribution statement
Ahou Sandrine Konan: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Conceptualization. Kalou Dibert Zika: Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Conceptualization. Affoué Sandrine Josette Kouakou: Writing – original draft, Visualization, Validation, Methodology, Conceptualization. Appi Sandrine Kouamé: Data curation, Conceptualization. Malick Senanminfoun Soro: Writing – original draft, Formal analysis, Conceptualization. Koffi Daho Adoubryn: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Methodology, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
We thank the parents who, despite the pain caused by their son's death, had the generosity to agree to the publication of this work.
Handling Editor: Prof Adilia Warris
References
- 1.Brizendine D.K., Baddley W.J., Pappas G.P. Pulmonary cryptococcosis. Semin. Respir. Crit. Care Med. 2011;32(6):727–734. doi: 10.1055/s-0031-1295720. [DOI] [PubMed] [Google Scholar]
- 2.Loua O.O., Alle Akakpo A.E., Ouedraogo D., Cissoko Y., Soumaré M., Konaté I., al Cryptococcose neuroméningée chez une patiente séronégative pour le VIH atteinte de tuberculose pulmonaire au service de Maladies infectieuses et tropicales du CHU du Point G de Bamako, Mali. Médecine Tropicale et Santé Internationale. 2022;2(4):282. doi: 10.48327/mtsi.v2i4.2022.282. 19 octobre 2022): mtsi.v2i4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eholie S.P., N’gbocho L., Bissagnene E., Coulibaly M., Ehui E., Kra O., al « Mycoses profondes au cours du SIDA à Abidjan (Côte d'Ivoire) Bull. Soc. Pathol. Exot. 1997;90(5):307–311. [PubMed] [Google Scholar]
- 4.Chuck S.L., Sande M.A. « Infections with Cryptococcus neoformans in the acquired immunodeficiency syndrome. N. Engl. J. Med. 1989;321:794–799. doi: 10.1056/NEJM198909213211205. https://pubmed.ncbi.nlm.nih.gov/2671735/ [DOI] [PubMed] [Google Scholar]
- 5.Lan C.Q., Weng H., Li H.Y., Chen L., Lin Q.H., Liu J.F., al [Retrospective analysis of 117 cases of pulmonary cryptococcosis] J. Tuberculosis Respirat. Diseases. 2016;39(11):862–865. doi: 10.3760/cma.j.issn.1001-0939.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Sadayuki M., Sakai S., Soeda H., Yabuuchi H., Masuda K., Inoue H., al Pulmonary cryptococcosis in immunocompetent patients: HRCT characteristics. Clin. Imag. 2004;28(3):191–195. doi: 10.1016/S0899-7071(03)00145-1. [DOI] [PubMed] [Google Scholar]
- 7.Ouazzani El, Souhi Achachi HL., Alaziz A.S., El Ftouh M.T., Achir A., El Fassy Fihry M.T. « Aspect pseudotumoral d’une cryptococcose pulmonaire chez un sujet immunocompétent. J. Radiol. 2011;92(3):254–256. doi: 10.1016/j.jradio.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Setianingrum F., Rautemaa-Richardson R., Denning W.D. Pulmonary cryptococcosis: a review of pathobiology and clinical aspects. Med. Mycol. 2019;57(2):133–150. doi: 10.1093/mmy/myy086. [DOI] [PubMed] [Google Scholar]
- 9.Liu K., Ding H., Xu B., You R., Xing Z., Chen J., al Clinical analysis of non-AIDS patients pathologically diagnosed with pulmonary cryptococcosis. J. Thorac. Dis. octobre 2016;8(10):2813–2821. doi: 10.21037/jtd.2016.10.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kazuma K., Sakae H., Atsuko K., Tadasu K., Noriko M., Kunihiko Y. Clinical features and high-resolution CT findings of pulmonary cryptococcosis in non-AIDS patients. Respir. Med. 2006;100(5):807–812. doi: 10.1016/j.rmed.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Kanet K., Zdravko K., Wiwatana T., Warangkana K., Siripen P. Pulmonary cryptococcosis presenting with lung mass: report of 7 cases and review of literature. Clin. Med. Insights Pathol. 4 août 2017;10 doi: 10.1177/1179555717722962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saag M.S., Graybill R.J., Larsen R.A., Pappas P.G., Perfect J.R., Powderly W.G., al Practice guidelines for the management of cryptococcal disease. Infectious diseases society of America. Clin. Infect. Dis.: Offic. Pub. Infect. Diseases Soci. Am. avril 2000;30(4):710–718. doi: 10.1086/313757. [DOI] [PubMed] [Google Scholar]