Kawasaki disease (KD) is an acute febrile disease with systemic vasculitis in children (2). Although its etiology remains unknown, KD is believed to be caused by an infectious agent. In the acute phase of KD, we recently demonstrated that lipopolysaccharide (LPS) was bound to the surfaces of circulating neutrophils via CD14 receptor (4) and that the soluble CD14 (sCD14) levels in the plasma increased markedly (5). LPS binding protein (LBP) binds to LPS, and the LPS-LBP complexes bind to CD14-positive cells such as macrophages and neutrophils (6). Alternatively, LBP transfers LPS to sCD14, and the LPS-sCD14 complexes can thus stimulate CD14-negative cells (6). LBP and sCD14 thus work together in an LPS transport system. On the other hand, LBP is an acute-phase response protein synthesized by hepatocytes, in the same manner as C reactive protein (CRP), and the elevated levels of LBP in plasma have not only been reported in gram-negative sepsis (GNS) but also in other infections (1) and systemic inflammatory response syndrome (3).
In the present study, we evaluated the plasma LBP, sCD14, interleukin 6 (IL-6), and tumor necrosis factor alpha (TNF-α) in patients with KD, patients with GNS, and healthy controls (HC), using the following enzyme-linked immunosorbent assays: for LBP, HyCult Biotechnology, Uden, Netherlands; for sCD14, IBL, Hamburg, Germany; and for IL-6 and TNF-α, R&S Systems, Minneapolis, Minn. The GNS group (n = 10; ages 2 months to 3 years) consisted of six children infected with Haemophilus influenzae and four children with Escherichia coli, as determined by blood cultures. In the KD group (n = 20; ages 6 months to 5 years), no bacterial species were identified in the blood culture. No patients with GNS and KD had such shock symptoms as hypotension or disseminated intravascular coagulation (DIC). The HC group consisted of 10 healthy children (ages 7 months to 4 years). There were no significant differences in the leukocyte counts and CRP levels between the GNS and KD groups: 18,920 ± 4,492 versus 15,982 ± 6,572/μl and 12.8 ± 5.4 versus 11.1 ± 4.9 mg/dl, respectively.
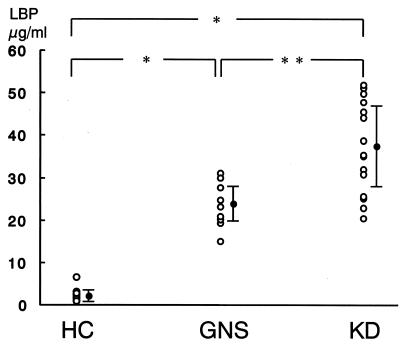
Figure 1 shows that the GNS patients and KD patients had significantly higher (P < 0.001) levels of LBP than HC and, furthermore, that the KD patients had significantly higher (P < 0.01) LBP levels than the GNS patients. There was no significant difference in the LBP levels between the patients with H. influenzae and those with E. coli. The increased levels of LBP observed in the acute phases of KD and GNS decreased to the levels observed in HC, during the convalescent phase when the CRP levels were <0.3 mg/dl. The LBP values correlated with the sCD14 levels (r = 0.52; P < 0.01) but not with the peripheral leukocyte counts, CRP levels, or the IL-6 and TNF-α levels.
FIG. 1.
Plasma LBP concentrations in HC (n = 10), patients with GNS (n = 10), and patients with KD (n = 20). The blood samples were obtained at the same time in both the GNS and the KD groups: 3.9 ± 2.3 versus 4.4 ± 2.1 days after the onset of fever, respectively. Mean values were as follows: HC, 2.7 ± 1.6 μg/ml; GNS, 23.5 ± 5.1 μg/ml; KD, 37.3 ± 10.9 μg/ml. *, P < 0.001; **, P < 0.01 (Mann-Whitney U test).
In summary, the plasma LBP levels increased markedly in the acute phase of KD. The mean LBP level was significantly higher in KD than in GNS, although there were no significant differences in the CRP level between the KD and GNS groups. Our results therefore suggest that the acute-phase response to LPS may be involved in the pathogenesis of KD and also support the possibility that KD might have an infectious and postinfectious etiology. The elevation in the plasma LBP level may also be a clinical marker for KD. On the other hand, we cannot rule out the possibility that the LPB levels may be merely a potential marker for disease activity. Therefore, further studies are needed to determine the clinical significance of the plasma LBP value in severely ill children with sepsis and DIC and in patients with noninfectious inflammatory diseases such as systemic lupus erythematosus and leukemia.
REFERENCES
- 1.Gallay, P., C. Barras, P. S. Tobias, T. Calandra, M. P. Glauser, and D. Heumann. 1994. Lipopolysaccharide (LPS)-binding protein in human serum determines the tumor necrosis factor response of monocytes to LPS. J. Infect. Dis. 170:1319–1322. [DOI] [PubMed] [Google Scholar]
- 2.Kawasaki, T. 1967. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Clinical observation of 50 cases. Jpn. J. Allergy 16:178–222. [PubMed] [Google Scholar]
- 3.Myc, A., J. Buck, J. Gonin, B. Reynolds, U. Hammerling, and D. Emanuel. 1997. The level of lipopolysaccharide-binding protein is significantly increased in plasma in patients with the systemic inflammatory response syndrome. Clin. Diagn. Lab. Immunol. 4:113–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeshita, S., K. Nakatani, H. Kawase, S. Seki, M. Yamamoto, I. Sekine, and S. Yoshioka. 1999. The role of bacterial lipopolysaccharide-bound neutrophils in the pathogenesis of Kawasaki disease. J. Infect. Dis. 179:508–512. [DOI] [PubMed] [Google Scholar]
- 5.Takeshita, S., K. Nakatani, H. Tsujimoto, Y. Kawamura, H. Kawase, and I. Sekine. 2000. Increased levels of circulating soluble CD14 in Kawasaki disease. Clin. Exp. Immunol. 119:376–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright, S. D. 1995. CD14 and innate recognition of bacteria. J. Immunol. 155:6–8. [PubMed] [Google Scholar]