Abstract
In order to characterize the cellular response to and identify potential diagnostic markers for the early detection of Ebola virus, an in vitro culture system involving nonhuman primate alveolar macrophages was developed. Ebola virus replication in the alveolar macrophages was characterized by plaque assay, immunohistochemical analysis, and in situ hybridization. Fluorogenic 5′ -nuclease assays specific for nonhuman primate proinflammatory cytokines and chemokines were designed and used to evaluate mRNA transcription in macrophages infected with Ebola virus. Transient increases in cytokine and chemokine mRNA levels were observed immediately following exposure to Ebola virus. At 2 h postexposure, levels of cytokine and chemokine mRNAs were markedly reduced. Although Ebola virus infection of alveolar macrophages failed to induce a sustained increase in proinflammatory cytokine and chemokine mRNA transcription (potentially reducing the use of these markers as diagnostic tools), the fluorogenic 5′-nuclease assays developed may have prognostic value for individuals infected with Ebola virus. Recently published data have indicated that persons who remain asymptomatic after exposure to Ebola virus are capable of mounting an early proinflammatory cytokine response and that those who become clinically ill are not. If implemented immediately after exposure, these assays could be used to predict which individuals will be more likely to remain asymptomatic as opposed to those who will be more likely to develop clinical signs and eventually succumb to the virus.
Ebola virus is one of two members of the family Filoviridae. Members of this family are responsible for sporadic epidemics of hemorrhagic fever in human and nonhuman primates, with mortality rates ranging from 22 to 88% (21, 25). The disease course associated with Ebola hemorrhagic fever is acute and progresses rapidly. The incubation period after exposure to Ebola virus can range from 2 to 10 days. Patients often present with flu-like symptoms, such as fever, myalgia, headache, diarrhea, and vomiting. Clinical signs may progress rapidly and include severe nausea, pharyngitis, diarrhea, hematemesis, and melena. The primary routes of transmission are improper needle hygiene, direct contact with infected tissue or fluid samples, and close contact with infected patients (3, 4, 6, 18). Other modes of filovirus transmission, including oral, conjunctival, and aerosol routes, have been identified through experimental infection of laboratory animals (15, 16, 18).
To study the host response to and identify potential diagnostic markers for Ebola virus infections, an in vitro culture system involving nonhuman primate alveolar macrophages was developed and characterized. Macrophages are known to be primary targets for Ebola virus replication, and there is both experimental and epidemiological evidence suggesting that aerosol spread of this virus can occur (2, 8, 15, 18). Aerosol spread has been validated experimentally with nonhuman primates exposed to Ebola virus (Zaire subtype) and Marburg virus (2, 18). In addition, there is evidence suggesting that aerosol spread of the virus occurred among monkeys housed in distant cages in a quarantine facility during the Ebola virus (Reston subtype) outbreak (15). During this same outbreak, several of the animal caretakers in contact with infected monkeys were found seropositive for Ebola virus antibodies by an indirect immunofluorescent-antibody assay (5). Three out of four of the animal caretakers who seroconverted had no known history of parenteral or trauma-induced exposure to Ebola virus; therefore, the possibility of aerosol transmission in these cases has been suggested (18).
Normal host defenses in the lungs include both innate (nonspecific) and acquired (specific) immune responses. Alveolar macrophages are the major immune effector cells resident in the airways and thus are key players in both arms of the immune response (24). They constitute the first line of phagocytic defense against infectious agents (innate response) and orchestrate the acquired (specific) response by the ordered expression and secretion of cytokines and chemokines (27). During a viral infection, they participate in the innate response by producing alpha/beta interferons (IFN-α/β) and the acquired response through antigen presentation, lymphocyte activation (through the secretion of soluble mediators), and IFN-α/β-induced major histocompatibility complex (MHC) class I gene expression (32).
Based on previously published studies, we hypothesized that infection of alveolar macrophages with Ebola virus would alter the expression of proinflammatory cytokines, chemokines, and IFN-α/β (1, 10, 29). Ebola virus infection of monocytes/macrophages can induce tumor necrosis factor alpha (TNF-α) production and, when compared to patients who recovered from Ebola virus infection, those with fatal outcomes had markedly elevated levels of gamma interferon (IFN-γ), IFN-α, interleukin 10 (IL-10), IL-2, and TNF-α(29). In addition, a more recent study showed that the VP35 protein of Ebola virus altered IFN-α/β production (1).
The purpose of these studies was to determine the effects of Ebola virus (Zaire subtype) on alveolar macrophage cytokine and chemokine and IFN-α/β production. In this report, we describe the development and evaluation of a one-step fluorogenic reverse transcription (RT)-PCR assay for evaluating RNA transcription of nonhuman primate cytokine and chemokine genes and discuss the potential of these markers for detecting filovirus infections. We report on the replication of Ebola virus in nonhuman primate alveolar macrophages and on the effects of viral infection on the expression of cytokine and chemokine and IFN-α/β mRNAs. We specifically focused on TNF-α, IL-1β, IL-8, IL-6, macrophage inflammatory protein 1α (MIP-1α), and IFN-β.
MATERIALS AND METHODS
Virus preparation.
Ebola virus (Zaire subtype, 1995 strain) was propagated in Vero E6 cells. Upon visualization of 60 to 70% cytopathic effects, supernatants were harvested, clarified by centrifugation, and stored at −70°C. Viral titers were determined by performing plaque assays on Vero E6 cells as described previously (22). Briefly, viral stock was diluted serially in minimal essential medium with Earle salts and nonessential amino acids, adsorbed to confluent Vero E6 cells in 12-well dishes, incubated for 1 h at 37°C, and covered with an agarose overlay. A 1:5,000 dilution of neutral red in buffered saline solution was added 7 days later, and plaques were counted the next day.
Isolation of alveolar macrophages.
Cynomolgus monkey lungs were obtained from Biowhittaker (Walkersville, Md.). Four research-naive cynomolgus monkeys were euthanatized, and the lungs were surgically removed. Approximately 60 ml of sterile, pyrogen-free phosphate-buffered saline (PBS) containing 0.5 mM EDTA was injected into the lung through the trachea. The trachea was then clamped, and the entire lung was immersed in cold PBS-EDTA solution. The container with the lung was placed on ice during transport to our laboratory.
Alveolar macrophages were harvested by flushing the lung with sterile PBS-EDTA. Cells were pelleted by centrifugation at 240 × g for 5 min. Pelleted cells were washed once in sterile PBS-EDTA, centrifuged at 240 × g for 5 min, and suspended in macrophage-serum-free medium (M-SFM; Gibco-BRL, Gaithersburg, Md.). Cells were counted, and viability was determined by trypan blue exclusion. Viability exceeded 95% in all four experiments. After being counted, the cells were seeded in six-well plates (for flow cytometry and cytokine determinations) at a density range of 2.5× 106 to 4.0 × 106 cells/well (depending on cell yield per lung) and allowed to adhere for 1.5 h at 37°C in 5% CO2. At the end of the 1.5 h, nonadherent cells were removed by washing twice with M-SFM, and an additional 3 ml of M-SFM was added to the remaining cells. Isolated alveolar macrophages were >99% pure, as determined by Wright-Giemsa staining. For cytospin preparations, cells were seeded in 48-well plates at a density of 2.5 × 105 cells/well. Individual alveolar macrophage cultures derived from each of the four cynomolgus monkey lungs are henceforth referred to as cultures from experiments 1 to 4.
Macrophage culture and infection conditions.
Before infection, alveolar macrophages were incubated at 37°C in 5% CO2 for approximately 2 h. Medium was removed, and alveolar macrophages were infected at a multiplicity of infection (MOI) of 1.0 in a total volume of 0.2 ml. Ebola virus was allowed to adsorb for 1 h at 37°C in 5% CO2. Unadsorbed virus was removed by washing once with prewarmed (37°C) M-SFM. Three milliliters of virus-free M-SFM was added back to each well, and this time was defined as time zero (T0) postexposure. Mock-infected wells were treated exactly the same as Ebola virus-infected wells, except that 0.2 ml of virus-free M-SFM was added to each well during infection. Lipopolysaccharide (LPS) (20 μg/ml) from Escherichia coli O55:B5 (Sigma Chemical Co., St. Louis, Mo.) was added to cultures as a positive control for cytokine induction. Culture supernatants were collected at 0, 6, 12, and 24 h postexposure and stored in aliquots at −70°C. The remaining cells were used for RNA preparation.
Cytospin preparations.
Cytospin preparations were made with a cytocentrifuge (Shandon, Pittsburgh, Pa.). At the time of initial cell preparation, an aliquot of 2.5 × 105 cells was harvested and centrifuged at 400 × g for 3 min. Cytospin preparations were allowed to air dry for 15 min and were fixed in 10% neutral buffered formalin (NBF) for 10 min. At the end of fixation, slides were washed in nuclease-free water (Quality Biologicals, Gaithersburg, Md.), stained with Wright-Geisma stain, and visualized by light microscopy.
Cytospin preparations were made in a biological safety level 4 (BSL-4) containment suite at 6, 12, and 24 h postexposure. Approximately 2.5 × 105 cells were harvested by gentle scraping of the wells. Cells were centrifuged at 400 × g for 3 min. Slides were air dried for 15 min and were fixed in 10% NBF for 24 h. At the end of fixation, slides were removed from the BSL-4 containment suite according to appropriate safety protocols, washed in nuclease-free water, and stored at 4°C until Wright staining was performed or until used in immunohistochemical (IHC) and in situ hybridization (ISH) assays.
IHC assays.
IHC assays were performed on formalin-fixed cytospin preparations and positive control tissue sections with an ENVISION kit (Dako Corp., Carpinteria, Calif.). A cocktail of two mouse monoclonal antibodies (anti-Ebola virus GP and anti-Ebola virus VP40) was used as the primary antibody (16). Positive control tissue sections were deparaffinized, rehydrated, and pretreated with proteinase K solution (Dako) for 6 min at room temperature before being immunostained. Cytospin preparations of alveolar macrophages were washed in PBS and pretreated with proteinase K solution for 6 min at room temperature before being immunostained. Before adding the primary antibody, we blocked endogenous peroxidase activity by adding peroxidase (0.03% hydrogen peroxide) for 25 min. The primary antibody was diluted 1:5,000 in antibody diluent. After applying the primary antibody to tissue sections, we completed the remainder of the protocol using a streptavidin-peroxidase conjugate, followed by development with diaminobenzidine containing hydrogen peroxide. All steps were completed according to the manufacturer’s instructions. Tissues from a monkey experimentally infected with Ebola virus in a previous study were included as positive controls. For negative controls, duplicate cytospin preparations and tissue sections were incubated with normal mouse serum prepared as described for the primary antiserum. After immunostaining was done, all sections were counterstained with hematoxylin, and coverslips were applied.
ISH assays.
Replicate 5-μm tissue sections to be used as positive controls were floated on RNase-free water (Quality Biologicals), collected on glass slides (Superfrost/Plus; Fisher Scientific, Pittsburgh, Pa.), and air dried. The sections were deparaffinized and rehydrated through graded alcohols to RNase-free water. Tissue sections and alveolar macrophage cytospin preparations were treated with 2× standard saline citrate (SSC) (1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate) for 10 min at 70°C and then placed in Tris-buffered saline (TBS; 50 mM Tris HCl, 0.15 M NaCl, 2 mM MgCl2 [pH 7.6]). TBS was removed, and sections were placed in a humidified chamber and digested for 30 min at 37°C with 20 μg of nuclease-free proteinase K (Boehringer Mannheim Biochemicals, Indianapolis, Ind.)/ml in TBS. Slides were washed in RNase-free water and allowed to air dry before we added hybridization solution.
The probe used for hybridization was comprised of two plasmids, one with the pCRII backbone (Invitrogen, San Diego, Calif.) containing a 2.03-kb Ebola virus glycoprotein cDNA insert and one with the pCRII backbone containing a 2.4-kb Ebola virus nucleoprotein cDNA insert. Plasmid DNA was purified using a plasmid midi kit (Qiagen, Valencia, Calif.) according to the manufacturer’s instructions. The probe was labeled with digoxigenin-11-dUTP by nick translation according to the manufacturer’s instructions (Boehringer). The probe was denatured at 95°C for 5 min and placed in an ethanol ice bath. Fifty microliters of hybridization solution [45% (vol/vol) deionized formamide (Ambion Inc., Austin, Tex.), 4× SSC, 4 mg of bovine serum albumin (BSA)/ml, 5μg of poly(A), 25 ng of digoxigenin-labeled probe, nuclease-free H2O to 50 μl] was applied to precleaned (RNase Zap; Ambion) coverslips, which were placed on the tissue sections, and the sections were incubated in a humidified chamber for 16 h at 37°C.
Coverslips were floated off the slides with 1× SSC. Sections were washed in 1× SSC and incubated for 15 min at room temperature in TBS containing 0.1% BSA and 0.1% Triton X-100. Sections were then covered with 500 μl of alkaline phosphatase-conjugated antidigoxigenin antibody (Fab fragment; 1:600 in TBS-0.1% BSA; Boehringer) and incubated for 60 min at 37°C. Sections were washed twice in TBS-0.1% BSA, rinsed in RNase-free water, and placed in chromogen buffer (100 mM Tris-HCl, 100 mM NaCl, 50 mM MgCl2 [pH 9.5]). Bound antibody was visualized by incubating slides in a 1:1 molar ratio of nitroblue tetrazolium chloride and 5-bromo-4-chloro-3-indolyl phosphate containing levamisole (Gibco-BRL) for 1 h at 37°C. Slides were rinsed in water and counterstained with nuclear fast red (Vector Laboratories). A positive signal was identified by blue-purple cytoplasmic staining. Controls included uninfected tissues.
Cytokine and chemokine assays (ELISAs).
Cytokine and chemokine levels were determined by enzyme-linked immunosorbent assays (ELISAs). TNF-α (monkey), IL-1β (human), and IL-8 (human) ELISA kits were purchased from BioSource International (Camarillo, Calif.). IL-6 (human) and MIP-1α (human) kits were purchased from Pierce Endogen (Rockford, Ill.) and R&D Systems (Minneapolis, Minn.), respectively. ELISAs were performed according to the manufacturer’s protocols in a BSL-4 containment suite.
RNA extraction.
Total RNA was extracted from alveolar macrophages using Trizol (Gibco-BRL). Cells were lysed by adding Trizol (Gibco-BRL) to individual wells of a six-well plate. After allowing sufficient time for cell lysis to occur, the Trizol mixture was removed from the wells and stored at −70°C. Total RNA was extracted according to the manufacturer’s instructions. Briefly, after the addition of chloroform, the mixture was centrifuged, and the aqueous phase containing the RNA was harvested. The RNA was precipitated by adding isopropanol, and the pellet was washed in 75% ethanol. Total RNA was resuspended in 200 μl of RNase-free water (Ambion) and treated for 30 min at 37°C with RNase-free DNase I (Ambion). The DNase I was subsequently inactivated by incubating samples for 15 min at 95°C. RNA was quantitated by spectrometry, and A260/A280 ratios were determined.
Cytokine and chemokine primer and probe design.
Primers and probes specific for macaque TNF-α, IL-1β, IL-8, IL-6, and MIP-1α genes were designed by evaluation of both published sequences (GenBank) and an unpublished sequence (the cDNA sequence for MIP-1α was kindly provided by Francois Villinger, Emory University, Atlanta, Ga.) using Primer Express Software (Applied Biosystems, Foster City, Calif.) (Table 1). The primers and probes were designed to meet the guidelines recommended by Applied Biosystems. The primers were designed with melting temperatures (Tm) of 58 to 60°C. The probes were designed to have a Tm of at least 7 to 10°C higher than the primer Tm. The presence of a guanine at the 5′ end of the probes was avoided, and the amplicons were designed to be less than 200 bp long. Primer and probe dimers, hairpins, stem-loop structures, and false priming sites were minimized. Primers specific for IFN-β were designed by evaluation of published sequences (GenBank) using Primer Express Software as described above (Table 1).
TABLE 1.
Sequences of PCR primers and sequence-specific probes for macaque cytokines
| Cytokine | Primer or probe | Sequence | Corresponding cDNA sequence | Product length (bp) |
|---|---|---|---|---|
| IL-1βa | Forward primer | 5′TCACTGCACTGCACACTCCG3′ | 361-380 | 101 |
| Reverse primer | 5′TGCTCCAGATCCTGTCCCTG3′ | 442-461 | ||
| Probe | 5′-FAM-AAGCTTGGTGATGTCTGGTCCATATGAACTGAAAG-TAMRA-3′ | 396-430 | ||
| IL-8a | Forward primer | 5′AGAGTGGACCACACTGTGCC3′ | 217-236 | 138 |
| Reverse primer | 5′ATGGATTTTGATTCTCAGCCC3′ | 334-354 | ||
| Probe | 5′-FAM-TGGGTGCAGAGGGTTGTGGAGAA-TAMRA-3′ | 300-322 | ||
| IL-6a | Forward primer | 5′CACACAGCCAGCCACTGACC3′ | 125-144 | 137 |
| Reverse primer | 5′TTCTGCCAGTGCCTCTTTGC3′ | 242-261 | ||
| Probe | 5′-FAM-CACATTCGGTACATCCTCGACGGCATCT-TAMRA-3′ | 166-191 | ||
| TNF-αa | Forward primer | 5′CAGCCTCTTCTCCTTCCTGC3′ | 127-146 | 143 |
| Reverse primer | 5′AAGATGATCTGACTGCCTGAGC3′ | 248-269 | ||
| Probe | 5′-FAM-CCACGCTCTTCTGTCTGCTGCACTTT-TAMRA-3′ | 162-187 | ||
| MIP-1αb | Forward primer | 5′ACTACTTGGAGACGAGCAGCC3′ | 86-106 | 114 |
| Reverse primer | 5′CGCTGACATATTTCTGGACCC3′ | 179-199 | ||
| Probe | 5′-FAM-CTCCAAGCCCGGTGTCATCTTCCTAA-TAMRA-3′ | 111-136 | ||
| IL-10a | Forward primer | 5′CTTGCTGGAGGACTTTAAGGG3′ | 214-234 | 116 |
| Reverse primer | 5′GCTCCTTGATGTCTGGGTCG3′ | 310-329 | ||
| IFN-βa | Forward primer | 5′CAACATGACCAACAAGTGTCTCC3′ | 24-46 | 122 |
| Reverse primer | 5′TTGTAGGAATCCAAGCAAGTTGTAGC3′ | 120-145 |
Fluorogenic 5′-nuclease assays.
RT-PCR was performed with an ABI PRISM 7700 sequence detection system and an Applied Biosystems TaqMan EZ RT-PCR kit according to the manufacturer’s instructions. Thermocycling conditions for newly designed cytokine and chemokine primer sets were identical and were as follows: 55°C for 45 min; 94°C for 1 min, and 40 cycles at 94°C for 15 s and 60°C for 30 s. Final concentrations used in the 50-μl reaction mixture were as follows: 0.5 μM each primer, 0.2 mM probe, 5 U or rTth enzyme, 300 μM each deoxynucleotide triphosphate, 1× TaqMan EZ RT-PCR buffer containing the passive reference dye ROX, and 2.5 mM manganese acetate. To account for variations in the amount of input RNA, RNA encoded by an endogenous housekeeping gene, that for glyceraldehyde-3-phosphate dehydrogenase (GAPDH), was amplified and quantified, and all results were normalized to this value. All assays were performed in triplicate, and averages from the three threshold cycle (CT) values were used for quantitating cytokine and chemokine mRNA levels. Twenty-five nanograms of total RNA was used in all RT-PCRs.
Quantitation of cytokine and chemokine RNA transcription.
Three methods exist to quantitate target mRNA levels in a sample using fluorogenic 5′-nuclease assays. They are the relative and absolute standard curve methods and the comparative CT method (user bulletin no. 2, ABI PRISM 7700 sequence detection system, revision A, 11 December 1997, p. 3–15). To determine the most rapid and accurate method for quantifying cytokine and chemokine mRNA levels in this study, two of the methods, the relative standard curve method and the comparative CT method, were evaluated using RNA samples isolated from alveolar macrophage cultures from experiment 1.
For the relative standard curve method, each sample was quantitated by using linear regression analysis from a standard curve. The standard curve was established over a range of RNA concentrations (75, 25, 10, 1, and 0.1 ng) from a designated calibrator sample (total RNA from 12-h LPS-stimulated alveolar macrophages). RNA from 12-h LPS-stimulated macrophages was chosen as the calibrator sample because previous experiments had indicated that cytokine and chemokine target RNAs were expressed at high levels at this time. The CT value (y axis) was then plotted against the log of the mass of total RNA (x axis). RNA transcription levels of cytokine and chemokine genes were determined by division of the concentration of the cytokine or chemokine RNA of interest (interpolated from the standard curve for that cytokine or chemokine RNA) by the concentration of the endogenous reference RNA (GAPDH; interpolated from the GAPDH standard curve).
To use the comparative CT method to quantitate RNA transcription, a validation experiment was performed in order to demonstrate that the amplification efficiencies of the target cytokine and chemokine RNA and the endogenous reference RNA (GAPDH) primer sets were approximately equal. The amplification efficiencies were determined using data generated from an examination of the relative standard curve method. For the comparative CT method to be valid, the absolute value of the slope of log input amount versus CT should be less than 0.1. The slope was calculated by plotting the ΔCT value (y axis) (where ΔCT is the average of the cytokine CT value minus the average of the GAPDH CT value) against the log nanograms of total RNA (x axis) using linear regression analysis. If the slope is <0.1, then the formula 2−ΔΔCT can be used to determine the relative quantities of target RNA present; the −ΔΔCT value is defined as the ΔCT of the sample of interest minus the ΔCT of the calibrator sample. In this instance, the Δ CT of the sample is defined as the average of the cytokine CT value minus the average of the GAPDH CT value for the same time point (averages were derived from experiments performed in triplicate). The calibrator sample in this instance was the ΔCT of the T0 mock-infected RNA sample. Target mRNA transcription in samples from experiments 2, 3, and 4 was determined by the comparative CT method. All samples were normalized to the calibrator T0 mock-infectedΔΔ CT value, which was assigned as 1. Ranges given for samples were determined by evaluating the expression 2−ΔΔ CT with ΔΔCT ±s, where s is the standard deviation of theΔΔCT value. The standard deviation ofΔΔCT is defined as the square root of the sum of the standard deviations of the average CT values for the cytokine or chemokine and GAPDH individually squared.
IFN-β RT-PCR assay.
RT-PCR assays were performed with an Applied Biosystems EZ rTth RNA PCR kit as instructed by the manufacturer. Thermocycling conditions for the IFN-β primer set were as follows: 55°C for 45 min, 94°C for 1 min, and 40 cycles at 94°C for 15 s and 60°C for 30 s. Final concentrations used in the 50-μl reaction mixture were as follows: 0.5 μM each primer, 5 U of rTth enzyme, 300 μM each deoxynucleotide triphosphate, 1× EZ buffer, and 2.5 mM manganese acetate. One hundred nanograms of total RNA was used in IFN-β RT-PCR assays. All assays were performed with a PTC 100 thermocycler (Applied Biosystems).
Direct analysis and detection of PCR-amplifed products on agarose gels.
Five-microliter aliquots of the RT-PCR products were analyzed by electrophoresis on 4% agarose gels (NuSieve; FMC BioProducts, Rockland, Maine) in Tris-borate buffer containing 1 μg of ethidium bromide/ml. The DNA bands were visualized with an Alpha-Inotech imaging system.
Sequencing of PCR-amplified products.
To verify the identities of PCR products, amplicons from RT-PCRs were sequenced by using dye-labeled terminators and cycle sequencing (Taq Prism kit; ABI, Foster City, Calif.). Products from sequencing reactions were analyzed on an ABI 377 sequencer. The sequences were then identified using the National Center for Biotechnology Information basic local alignment search tool (BLAST) (www.ncbi.nlm.nih.gov/BLAST/).
Flow cytometry.
To characterize the cell surface expression of MHC class I and class II molecules, alveolar macrophages were analyzed by fluorescence-activated cell sorting. Cells were collected by gently scraping the wells at 0, 2, 12, and 24 h postexposure. Cold RPMI 1640 (4°C) containing 0.5% BSA was added to each well. Single-cell suspensions were obtained by vigorous mixing with a vortexer. Cells were pelleted by centrifugation at 240 × g for 5 min, medium was removed, and 20 μl of each fluorescein isothiocyanate (FITC)-conjugated antibody (anti-HLA-A, B, and C [Pharmingen, San Diego, Calif.] and anti-HLA-DR [Pharmingen]) was added to individual tubes. Antibody staining was performed at 4°C for 45 min. At the end of the 45 min, RPMI 1640 containing BSA was added to each tube, and cells were again pelleted by centrifugation at 240 × g for 5 min. Medium was aspirated, and the cell pellet was fixed in 10% NBF (4% paraformaldehyde) at 4°C for 72 h before reading was done by flow cytometry with a FACSsort instrument operating with CELLQuest software (Becton Dickinson). Dead cells and debris were excluded from the analyses. Each histogram plot was generated from at least 104 events.
Statistical Analysis.
Data obtained from ELISAs and fluorogenic 5′-nuclease assays were evaluated for significant differences by the Kruskal-Wallis analysis of variance. For each time point examined, data from alveolar macrophages isolated from individual monkeys were normalized by transformation to the logarithmic scale, analyzed, and ranked. Ranked samples were then analyzed, and significant differences were determined by comparison to data for mock-infected cells at each time point. A significant difference was determined when the P value was <0.05.
RESULTS
Ebola virus replication in alveolar macrophages.
To evaluate the ability of Ebola virus to infect and replicate in an in vitro culture of alveolar macrophages, freshly isolated cells from cynomolgus monkeys were infected with Ebola virus (Zaire) at an MOI of 1.0. Viral infection was characterized by plaque assays, IHC analysis, ISH, and light microscopy. Culture medium was removed at 0, 6, 12, and 24 h postexposure and was titrated by plaque assays on Vero E6 cells. As shown in Fig. 1C, Ebola virus (Zaire) productively infected the alveolar macrophages, showing a 10-fold increase in titer in macrophages from experiments 1 and 2 and a 100-fold increase in titer in macrophages from experiments 3 and 4 over a 24-h period. Under light microscopy, Ebola virus caused visible cytopathic effects in cell cultures during the 24-h period. By 12 h postexposure, cells in Ebola virus-infected wells began to detach from the culture plates, and by 24 h, 50 to 60% of the cells were detached and floating in the culture medium. At 12 h postexposure, alterations in cellular morṕhology which are indicative of irreversible cell injury were observed in Ebola virus-infected alveolar macrophages. Alterations such as membrane blebbing were present throughout the cultures. At 24 h postexposure, numerous plasma membranes were disrupted (blebbing was prominent), there was prominent karyorrhexis, and cells were vacuolated. Large amounts of cellular debris were present in Ebola virus-infected cultures, and cytolysis was evident. In contrast, alveolar macrophages in mock-infected and LPS-treated wells remained firmly attached to the bottoms of wells during the 24-h incubation period. Under light microscopy, mock-infected cells appeared normal. Cells stimulated with LPS appeared to increase in size and take on the characteristics of activated macrophages.
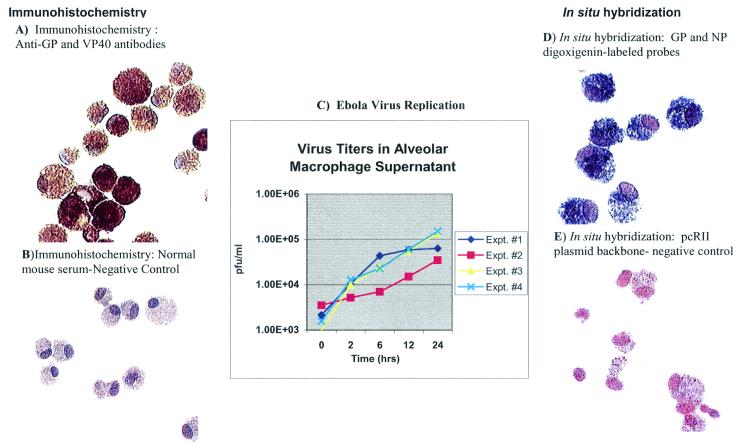
FIG. 1.
To characterize alveolar macrophage infection, IHC (A and B) and ISH (D and E) analyses were performed on alveolar macrophages. IHC analysis was performed with a cocktail of primary antibodies consisiting of anti-Ebola virus glycoprotein (GP) and anti-Ebola virus VP40 antibodies. The probe used for ISH analysis consisted of two plasmids, one with the pCRII backbone containing a 2.03-kb Ebola virus glycoprotein (GP) insert and one with the pCRII backbone containing a 2.4-kb Ebola virus nucleoprotein (NP) insert. At 12 h after exposure, abundant amounts of viral protein (A) and RNA (D) were observed in Ebola virus-infected cells. Mock-infected cells stained negative for viral protein (B) and RNA (E). Viral replication, as determined by plaque assays, showed a 10- to 100-fold increase in titer during the 24 h after exposure.
IHC analysis and ISH were used to further characterize Ebola virus infection in alveolar macrophage cultures. Compared to the results seen at T0, at T6 there was a notable increase in the amounts of Ebola virus RNA and protein in the cytoplasm of infected cells. Throughout the course of infection (Fig. 1), the numbers of cells staining positive in IHC analysis and ISH increased steadily. By 24 h postexposure, the cytoplasm of 80 to 90% of infected cells stained intensely for viral protein and RNA.
Additionally, fluorogenic 5′-nuclease assays were performed to further confirm the presence or absence of viral RNA in infected alveolar macrophage cultures. Positive CT values and the visualization of a 143-bp band by agarose gel electrophoresis indicated the presence of viral RNA. RT-PCR detected viral RNA throughout the course of infection in Ebola virus-infected cells but not in LPS- and mock-infected cells.
Flow cytometry.
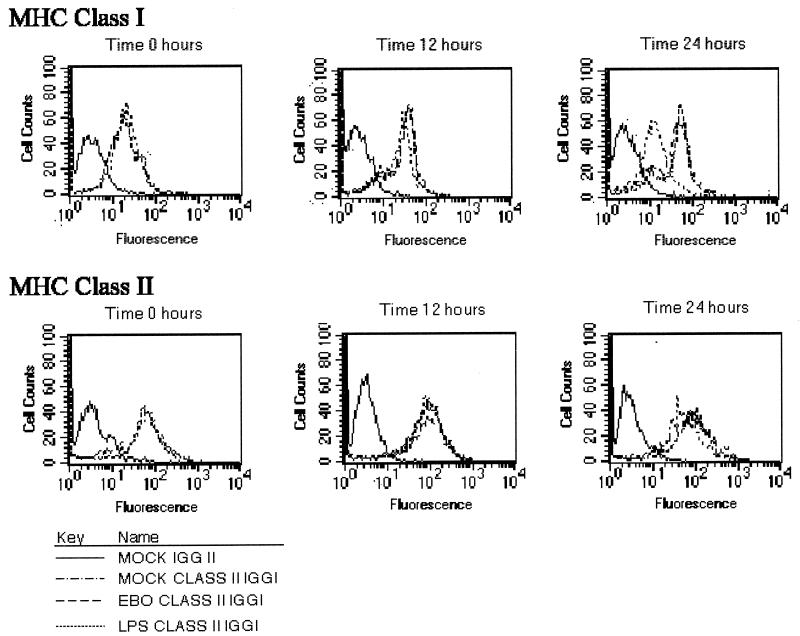
Flow cytometry was performed to characterize the alveolar macrophage population and determine the state of cellular activation after infection with Ebola virus (Zaire). Alveolar macrophages were analyzed for MHC class I and MHC class II expression after exposure to medium (mock-infected controls), Ebola virus (MOI, 1.0), and LPS (20 μg/ml). Figure 2 shows MHC class I and II expression on alveolar macrophages from a single cynomolgus monkey in a representative experiment. Ebola virus infection did not induce the expression of HLA-A, HLA-B, HLA-C, or HLA-DR in alveolar macrophages compared to the results seen for mock-infected controls at the same time points. At 24 h postexposure, MHC class I cell surface expression was decreased in Ebola virus-infected cells compared to mock-infected controls (Fig. 2).
FIG. 2.
HLA-A, B, C, and HLA-DR expression by alveolar macrophages. Alveolar macrophages from cynomolgus monkeys exposed to medium (mock-infected control), Ebola virus (EBO) (MOI, 1.0), or LPS were harvested at 0, 12, and 24 h postinfection. Cells were left untreated or were treated with monoclonal antibodies to HLA-DR (MHC class II) or to HLA-A, B, and C (MHC class I), washed, fixed in 4% paraformaldehyde, and analyzed by fluorescence-activated cell sorting. A total of 104 cells per condition were analyzed. Relative fluorescence intensity for HLA-DR and for HLA-A, HLA-B, and HLA-C proteins is displayed on the horizontal axis. These data are from a representative experiment with cells from one of the four cynomolgus monkeys.
Alveolar macrophage supernatant cytokine and chemokine levels.
Cytokines and chemokines play important roles in both innate and acquired immune responses to viral pathogens. Secretion of these soluble mediators by alveolar macrophages is key in establishing an effective antiviral pulmonary response. The accumulation of TNF-α, IL-1β, IL-8, IL-6, and MIP-1α in aliquots of supernatants from alveolar macrophages exposed to medium (mock-infected controls), Ebola virus (MOI, 1.0), and LPS (20 μg/ml) was examined. The results are shown in Table 2. Alveolar macrophages incubated in medium alone failed to produce significant levels of TNF-α, IL-1β, IL-8, IL-6, and MIP-1α during 24 h of incubation. In contrast, at 6, 12, and 24 h poststimulation with LPS, there were significant increases in cytokine and chemokine production compared to the results seen for mock-infected controls (P < 0.05). IL-1β reached maximum levels of production at 12 h after LPS stimulation. IL-6, IL-8, TNF-α, and MIP-1α protein levels rose steadily during the 24-h period after LPS stimulation (Table 2). At 24 h postexposure, alveolar macrophages infected with Ebola virus showed significantly increased levels of IL-1β and TNF-α (P < 0.05); however, IL-6, IL-8, and MIP-1α protein levels in Ebola virus-infected cultures were similar to those in mock-infected controls at all time points examined (Table 2).
TABLE 2.
Effects of Ebola virus infection and LPS stimulation on cytokine and chemokine protein production in nonhuman primate alveolar macrophages
| Time | Treatment | Mean ± SEM concn (pg/ml) ofa:
|
||||
|---|---|---|---|---|---|---|
| IL-1β | IL-6 | IL-8 | MIP-1α | TNF-α | ||
| T0 | Mock infected | 0 | 0 | 1.71 ± 1.71 | 0 | 1.11 ± 1.11 |
| Infected | 0 | 8.19 ± 8.19 | 24.20 ± 24.20 | 0 | 0 | |
| T6 | LPS | 94.06 ± 29.38b | 55.51 ± 23.51b | 8,598.61 ± 1,025.66b | 1,940.59 ± 476.56b | 3,070.28 ± 870.74b |
| Mock infected | 0 | 0 | 440.01 ± 155.20 | 30.28 ± 26.88 | 0 | |
| Infected | 0 | 1.73 ± 1.42 | 842.92 ± 306.37 | 112.66 ± 57.69 | 1.44 ± 1.44 | |
| T12 | LPS | 216.69 ± 139.31b | 665.59 ± 314.41b | 26,098.57 ± 3,218.03b | 18,600.80 ± 5,287.57b | 5,625.12 ± 1,633.96b |
| Mock infected | 0 | 0.04 ± 0.04 | 912.31 ± 394.92 | 209.04 ± 122.67 | 29.01 ± 24.95 | |
| Infected | 0 | 0 | 1,079.49 ± 368.21 | 141.92 ± 113.45 | 1.44 ± 1.44 | |
| T24 | LPS | 212.95 ± 117.15b | 1,240.08 ± 666.67b | 37,840.58 ± 2,704.53b | 36,735.02 ± 4,850.02b | 5,966.06 ± 1,532.75b |
| Mock infected | 0 | 23.73 ± 23.73 | 676.83 ± 287.05 | 158.45 ± 127.00 | 0.00 | |
| Infected | 16.02 ± 7.60b | 7.24 ± 7.24 | 2,762.62 ± 1,076.25 | 218.65 ± 143.03 | 102.51 ± 56.35b | |
Data are for alveolar macrophages from four different cynomolgus monkeys in four separate experiments.
Value was significantly different (P < 0.05) from value for mock-infected cells at the same time point.
Comparison of relative standard curve method versus comparative CT method for quantitation of cytokine and chemokine mRNA levels.
To determine the most rapid and accurate method for quantitating cytokine and chemokine mRNA levels, total RNA isolated from alveolar macrophages from experiment 1 was tested by using two methods: the relative standard curve method and the comparative CT method. The relative standard curve method was performed as described in Materials and Methods.
To use the comparative CT method, the amplification efficiencies of each cytokine and chemokine primer set and the reference set (GAPDH) were analyzed (user bulletin no. 2, ABI PRISM 7700 sequence detection system). The amplification efficiency of each primer set was evaluated by establishing standard curves with the calibrator sample (12-h LPS-stimulated alveolar macrophage RNA) and then plotting the ΔCT value (y axis) against the log nanograms of total RNA (x axis). The slope of the line was calculated using linear regression analysis. When the amplification efficiencies of the cytokine and chemokine primer sets were compared to those of the GAPDH reference set, only two sets (IL-8 and MIP-1α) had amplification efficiencies similar to those of the reference set (GAPDH) (slope was <0.1). Analysis of all other primer sets indicated that the amplification efficiencies were not equal (slopes were not <0.1). However, data collected by both methods of quantitation yielded results which were essentially indistinguishable. Data calculated by the relative standard curve method most often fell within the range of data calculated by the comparative CT method. Thus, we chose the comparative CT method to analyze samples from all alveolar macrophage experiments.
IL-1β, IL-8, IL-6, MIP-1α, and TNF-α mRNA transcription in Ebola virus-infected alveolar macrophages.
The mRNA transcription of IL-1β, IL-8, IL-6, MIP-1α, and TNF-α in alveolar macrophages exposed to medium alone, Ebola virus, and LPS was monitored at 0, 6, 12, and 24 h postexposure. mRNA transcription in each of the cultures was expressed as the percent increase over the values for the T0 mock-infected samples. The data shown in Table 3 represent the mean and the standard error of the mean for all four experiments. Statistical analysis was performed by using the Kruskal-Wallis analysis of variance by ranks. Observations were considered statistically significant when the P value was <0.05. Cytokine and chemokine mRNA expression in mock-infected cells did not significantly increase at any time during the experiment compared to the values for the T0 mock-infected cells. Cells stimulated with LPS produced significantly greater amounts of all cytokines and chemokines examined with the fluorogenic 5′-nuclease assays at 6, 12, and 24 h poststimulation. Alveolar macrophages infected with Ebola virus produced significantly greater amounts of IL-1β, IL-6, MIP-1α, and IL-8 mRNAs at T0 (1 h postexposure) than did cells treated with medium alone. However, at T6, the levels of cytokine and chemokine mRNA transcription in Ebola virus-infected cells were similar to those in mock-infected cells. At T24, when we observed a large proportion of cell death in infected cultures, levels of all cytokine and chemokine mRNAs were statistically higher than those in mock-infected cultures (Table 3).
TABLE 3.
Effects of Ebola virus infection and LPS stimulation on cytokine and chemokine RNA production in nonhuman primate alveolar macrophages
| Time | Treatment | Mean ± SEM % increase in template RNA fora:
|
||||
|---|---|---|---|---|---|---|
| IL-1β | IL-6 | IL-8 | MIP-1α | TNF-α | ||
| T0 | Mock infected | 1 | 1 | 1 | 1 | 1 |
| Infected | 1.9 ± 0.47b | 54.16 ± 34.93b | 1.87 ± 0.22b | 3.91 ± 0.59b | 1.19 ± 0.41 | |
| T6 | LPS | 52.35 ± 6.00b | 19,533.49 ± 6,432.60b | 24.81 ± 5.50b | 98.30 ± 17.24b | 60.10 ± 23.94b |
| Mock infected | 0.47 ± 0.05 | 0.71 ± 0.15 | 0.20 ± 0.03 | 3.52 ± 2.70 | 1.11 ± 0.86 | |
| Infected | 0.83 ± 0.31 | 00.63 ± 0.11 | 0.41 ± 0.05b | 3.43 ± 1.37 | 0.28 ± 0.07 | |
| T12 | LPS | 41.82 ± 6.23b | 24,999.04 ± 8,976.29b | 25.71 ± 6.50b | 144.23 ± 58.92b | 162.31 ± 127.46b |
| Mock infected | 1.53 ± 1.20 | 245.14 ± 229.05 | 0.35 ± 0.27 | 9.02 ± 7.37 | 5.51 ± 5.15 | |
| Infected | 0.44 ± 0.19 | 1.04 ± 0.39 | 0.51 ± 0.08 | 3.80 ± 1.14 | 3.32 ± 2.63 | |
| T24 | LPS | 18.57 ± 5.10b | 14,218.51 ± 9,022.08b | 12.69 ± 4.30b | 67.60 ± 28.6b | 58.87 ± 53.02b |
| Mock infected | 0.04 ± 0.02 | 2.53 ± 1.15 | 0.01 ± 0.00 | 0.60 ± 0.14 | 0.05 ± 0.05 | |
| Infected | 6.44 ± 4.19b | 5,864.48 ± 5,858.41b | 5.49 ± 2.96b | 25.38 ± 17.58b | 67.54 ± 63.64b | |
Data are for treated cells relative to T0 mock-infected cells over time in four separate experiments with alveolar macrophages from four separate cynomolgus monkeys.
Value was significantly different (P < 0.05) from value for mock-infected cells at the same time point.
IFN-β expression in Ebola virus-infected alveolar macrophages.
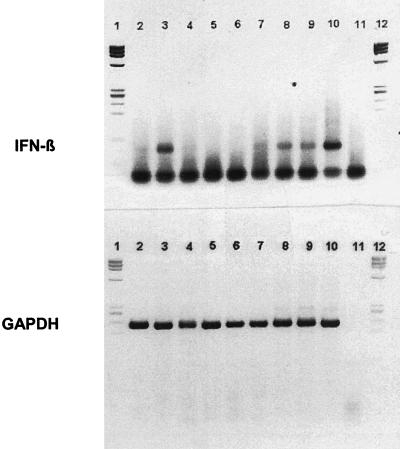
One of the most important and early components of the host defense against viral infections is the production of IFN-α/β. IFN-α/β are synthesized in response to viral infections or the presence of double-stranded RNA (dsRNA) species (14, 17). In an attempt to determine whether Ebola virus induced IFN-α/β production, the mRNA expression of IFN-β was monitored at 0, 2, and 6 h postexposure in alveolar macrophages exposed to medium alone (mock-infected controls), Ebola virus, and LPS. In two of the four experiments, at T0 IFN-β was expressed at higher levels in Ebola virus-infected cells than in mock-infected cells (Fig. 3). However, by 2 h after exposure to Ebola virus, there was a significant reduction in the amount of IFN-β mRNA present in alveolar macrophages (Fig. 3). The IFN-β response was absent in macrophages from the other two cultures. At 6 h postexposure, equal amounts of IFN-β were observed in both mock-infected and Ebola virus-infected cells. IFN-β production was not detected in cells stimulated with LPS at 6 h postexposure (Fig. 3).
FIG. 3.
IFN-β expression by alveolar macrophages, as analyzed by RT-PCR. One hour after exposure to Ebola virus (lane 3), cells expressed IFN-β mRNA at significantly increased levels over mock-infected cells. However, by 2 h postexposure, the expression of IFN-β was markedly reduced (lane 6) (observed in two of four monkeys). In the other two monkeys, Ebola virus infection failed to stimulate any IFN-β production (data not shown). GAPDH was used as an internal control. Lane 1 and 12, molecular weight markers; lane 2, T0 mock-infected cells; lane 3, T0 Ebola virus-infected cells; lane 4, T2 LPS-stimulated cells; lane 5, T2 mock-infected cells; lane 6, T2 Ebola virus-infected cells; lane 7, T6 LPS-stimulated cells; lane 8, T6 mock-infected cells; lane 9, T6 Ebola virus-infected cells; lane 10, LPS-stimulated peripheral blood mononuclear cells (positive control); lane 11, no-template control (NTC).
DISCUSSION
In this study, we developed and characterized an in vitro model of alveolar macrophages in which the host response to filovirus infection can be studied. This is the first documented evidence of Ebola virus infection and replication in alveolar macrophages in an in vitro system.
Data from this study indicate clearly that nonhuman primate alveolar macrophages are susceptible to Ebola virus infection in vitro and are capable of replicating the virus to a high titer within 24 h. These data are particularly significant, as alveolar macrophages are the first line of phagocytic defense against inhaled pathogens and are known to be important in orchestrating the host immune response (i.e., cytokine production and regulation of MHC molecule expression) to infectious agents that reach the alveoli (32). In this system, Ebola virus replication appeared to proceed efficiently. Within 24 h of initial infection, viral replication led to irreversible cell injury and severe cytolysis.
The ability of viruses to replicate efficiently and to a high titer inside the target cell largely depends upon their ability to evade the host immune response. One of the most important and early components of the host defense against viral infections is the production of IFN-α/β and other cytokines that inhibit viral replication (TNF-α and IL-1β). IFN-α/β and proinflammatory cytokines are synthesized in response to viral infections or the presence of dsRNA species. dsRNAs are intermediates that are generated during the replication cycle of many viruses (14, 17). For negative-stranded RNA viruses (filoviruses, paramyxoviruses, and orthomyxoviruses), dsRNA intermediates arise during the production of positive-stranded progeny. In response to dsRNA, IFN-α/β signal through a common receptor to induce the transcription of antiviral proteins such as dsRNA-dependent protein kinase R and 2′, 5′-oligoadenylate synthetase (17). These antiviral proteins then act to inhibit viral replication by blocking viral RNA and protein synthesis and inducing apoptosis (19). In addition, dsRNA induces the transcription of many proinflammatory cytokines, such as IL-6, TNF-α, and IL-1β.
Either the virus itself or the dsRNA species produced by the virus during replication induce the transcription of IFN-α/β and proinflammatory cytokines. Many viruses have developed survival mechanisms that enable them to counteract dsRNA-induced cellular responses (2a). Of the viruses that have developed these mechanisms, those of particular relevance to the current study are members of viral families (the family Paramyxoviridae and the family Orthomyxoviridae) that are closely related to the family Filoviridae. Influenza virus A (11), simian virus 5 (31), measles virus (23), and Sendai virus (12) have all developed distinct mechanisms for subverting the dsRNA-induced IFN-α/β response. In addition, recently published data indicate that Ebola virus, like many other negative-stranded RNA viruses, is capable of suppressing the IFN-α/β response. More specifically, VP35, a phosphoprotein encoded by the Ebola virus genome, acts as an IFN-α/β antagonist by blocking dsRNA- and virus-mediated induction of the IFN-β promoter (1). In this study, infection of alveolar macrophages with Ebola virus appeared to completely block or suppress IFN-β mRNA production. Alveolar macrophages infected with Ebola virus either responded with an initial burst of IFN-β RNA production which was later suppressed or failed to produce any IFN-β (Fig. 3). Many important effector molecules (i.e., MHC class I and cytokines) involved in the host antiviral response are dependent on IFN-α/β expression. Therefore, the ability of VP35 to inhibit IFN-α/β production may explain why Ebola virus replicated to a high titer but failed to induce sustained expression of critical mediators (proinflammatory cytokines and chemokines and MHC class I and II expression) involved in the host antiviral response in alveolar macrophages (Tables 2 and 3 and Fig. 2).
The mechanisms responsible for VP35 inhibition of IFN-α/β production have not been fully elucidated. However, like other viral proteins (NS1 of influenza virus A), VP35 may inhibit the dsRNA-induced activation of transcription factors needed for IFN-α/β gene induction. For example, the NS1 protein of influenza virus A blocks IFN-β production by inhibiting the activation of both IFN regulatory factor 3 and nuclear factor κB (NF-κB), two factors known to be important in induction of the IFN-β promoter (26, 30). If, in fact, VP35 blocks the dsRNA-induced expression of IFN-α/β by inhibiting the activation of transcription factors such as NF-κB, this action could account for the lack of sustained proinflammatory cytokine expression observed in this system. Both TNF-α and IL-1β contain elements in their promoters that are responsive to induction by NF-κB, and the expression of both is known to be induced by dsRNA (13, 28). Furthermore, IFN-α/β are important stimulators of MHC class I expression in virus-infected cells. In this study, we did not observe an upregulation of MHC class I expression after viral infection. At 24 h postexposure, when a large proportion of cell death was observed in infected cultures, MHC class I expression was markedly decreased in Ebola virus-infected cells. These data are similar to those of an earlier report in which Ebola virus was shown to suppress dsRNA induction of IFN regulatory factor 1, MHC class I, IL-6, and 2′, 5′-oligoadenylate expression in endothelial cells (14).
The apparent suppression of IFN-β production after infection with Ebola virus is consistent with recently published data showing that the VP35 phosphoprotein of Ebola virus inhibits IFN-β gene induction (1) and that Ebola virus is capable of inhibiting dsRNA induction of genes important in orchestrating an early antiviral state (14). The lack of an early antiviral response in macrophages is significant because these cells are the earliest and most heavily affected targets for Ebola virus replication (7, 9, 16). In addition, the variability observed among primates with respect to their ability to mount an early IFN response to Ebola virus may provide some indication as to why some individuals remain asymptomatic and others succumb to infection after exposure to Ebola virus (20). It is possible that some individuals are capable of subverting the VP35-induced suppression of the IFN-α/β response and therefore are able to control viral replication and mount an effective immune response early in the course of the disease. In fact, asymptomatic individuals exposed to Ebola virus had very low viral titers. These individuals produced an early and sustained inflammatory response with high levels of IL-1β, TNF-α, IL-6, and MIP-1α (20).
The data presented here provide further evidence to support the hypotheses that Ebola virus is capable of suppressing the dsRNA-induced host antiviral response and that the suppression of this response may play a key role in the ability of the virus to replicate and induce profound immunosuppression during the course of the disease. Further characterization of the early immune response to Ebola virus infection may provide insight into the mechanisms by which the virus evades and suppresses the host immune system.
In conclusion, our data demonstrate that in an in vitro system of alveolar macrophages, Ebola virus infection induced a transient, early increase in proinflammatory cytokine and chemokine mRNA expression. The ability or inability to produce a cytokine response immediately following Ebola virus infection may be a critical factor in determining the prognosis of a patient. Recently published data suggest a link between the clinical status of a patient and the inflammatory response. Persons who remain asymptomatic after exposure to Ebola virus are capable of mounting an early, sustained proinflammatory cytokine response, and those who become clinically ill are not (20). Cytokine responses associated with terminal cases of Ebola virus infections (29) occur late in the course of disease (following damage to the gastrointestinal tract, endotoxin release, and endothelial damage) and therefore are not likely to play a key role in determining the prognosis of Ebola virus-infected patients. Therefore, the fluorogenic 5′-nuclease assays developed and evaluated in this study are of questionable use for early diagnostic purposes but, if used immediately following exposure, may prove to be valuable as prognostic indicators for individuals exposed to Ebola virus. If applied immediately after exposure, these assays could be used to predict which individuals will be more likely to remain asymptomatic as opposed to those who will be more likely to develop clinical signs and eventually succumb to the virus.
Acknowledgments
We thank Deanna Bridge, Bill Hurtle, Jeff Brubaker, and Edna Torres for excellent technical assistance. We thank Sina Bavari for time and valuable guidance in the design of experiments carried out in this study. We thank Francois Villinger for providing guidance and materials used in this study. We thank David Shoemaker, George Ludwig, and Paul Gibbs for helpful suggestions and critical input in the preparation of the manuscript.
REFERENCES
- 1.Basler, C. F., X. Wang, E. Muhlberger, V. Volchkov, J. Paragas, H. D. Klenk, A. Garcia-Sastre, and P. Palese. 2000. The Ebola virus VP35 protein functions as a type IIFN antagonist. Proc. Natl. Acad. Sci. USA 97:12289–12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bazhutin, N. B., E. F. Belanov, V. A. Spiridonov, A. V. Voitenko, N. A. Krivenchuk, S. A. Krotov, N. I. Omel′ chenko, A. I. Tereshchenko, and V. V. Khomichev. 1992. The effect of the methods for producing an experimental Marburg virus infection on the characteristics of the course of the disease in green monkeys. Vopr. Virusol. 37:153–156. [PubMed] [Google Scholar]
- 2a.Biron, C. A., and G. C. Sen. 2001. Interferons and other cytolines, p.321–351. In D. M. Knipe and P. M. Howley (ed.), Fields’ Virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 3.Bulletin of the World Health Organization. 1978. Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team. Bull. W. H. O. 56:247–270. [PMC free article] [PubMed] [Google Scholar]
- 4.Bulletin of the World Health Organization. 1978. Ebola haemorrhagic fever in Zaire, 1976. Bull. W. H. O. 56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 1990. Update: filovirus infections among persons with occupational exposure to nonhuman primates. Morb. Mortal. Wkly. Rep. 39:266–267. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 1995. Update: outbreak of Ebola viral hemorrhagic fever— Zaire, 1995. Morb. Mortal. Wkly. Rep. 44:468–469, 475. [PubMed]
- 7.Connolly, B. M., K. E. Steele, K. J. Davis, T. W. Geisbert, W. M. Kell, N. K. Jaax, and P. B. Jahrling. 1999. Pathogenesis of experimental Ebola virus infection in guinea pigs. J. Infect. Dis. 179(Suppl. 1):S203–S217. [DOI] [PubMed] [Google Scholar]
- 8.Dalgard, D. W., R. J. Hardy, S. L. Pearson, G. J. Pucak, R. V. Quander, P. M. Zack, C. J. Peters, and P. B. Jahrling. 1992. Combined simian hemorrhagic fever and Ebola virus infection in cynomolgus monkeys. Lab. Anim. Sci. 42:152–157. [PubMed] [Google Scholar]
- 9.Davis, K. J., A. O. Anderson, T. W. Geisbert, K. E. Steele, J. B. Geisbert, P. Vogel, B. M. Connolly, J. W. Huggins, P. B. Jahrling, and N. K. Jaax. 1997. Pathology of experimental Ebola virus infection in African green monkeys. Involvement of fibroblastic reticular cells. Arch. Pathol. Lab. Med. 121:805–819. [PubMed] [Google Scholar]
- 10.Feldmann, H., H. Bugany, F. Mahner, H. D. Klenk, D. Drenckhahn, and H. J. Schnittler. 1996. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J. Virol. 70:2208–2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia-Sastre, A., A. Egorov, D. Matassov, S. Brandt, D. E. Levy, J. E. Durbin, P. Palese, and T. Muster. 1998. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology 252:324–330. [DOI] [PubMed] [Google Scholar]
- 12.Garcin, D., P. Latorre, and D. Kolakofsky. 1999. Sendai virus C proteins counteract the interferon-mediated induction of an antiviral state. J. Virol. 73:6559–6565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gendelman, H. E., R. M. Friedman, S. Joe, L. M. Baca, J. A. Turpin, G. Dveksler, M. S. Meltzer, and C. Dieffenbach. 1990. A selective defect of interferon alpha production in human immunodeficiency virus-infected monocytes. J. Exp. Med. 172:1433–1442. (Erratum, 173:277, 1991.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harcourt, B. H., A. Sanchez, and M. K. Offermann. 1998. Ebola virus inhibits induction of genes by double-stranded RNA in endothelial cells. Virology 252:179–188. [DOI] [PubMed] [Google Scholar]
- 15.Jaax, N., P. Jahrling, T. Geisbert, J. Geisbert, K. Steele, K. McKee, D. Nagley, E. Johnson, G. Jaax, and C. Peters. 1995. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet 346:1669–1671. [DOI] [PubMed] [Google Scholar]
- 16.Jaax, N. K., K. J. Davis, T. J. Geisbert, P. Vogel, G. P. Jaax, M. Topper, and P. B. Jahrling. 1996. Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch. Pathol. Lab. Med. 120:140–155. [PubMed] [Google Scholar]
- 17.Jacobs, B. L., and J. O. Langland. 1996. When two strands are better than one: the mediators and modulators of the cellular responses to double-stranded RNA. Virology 219:339–349. [DOI] [PubMed] [Google Scholar]
- 18.Johnson, E., N. Jaax, J. White, and P. Jahrling. 1995. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int. J. Exp. Pathol. 76:227–236. [PMC free article] [PubMed] [Google Scholar]
- 19.King, P., and S. Goodbourn. 1998. STAT1 is inactivated by a caspase. J. Biol. Chem. 273:8699–8704. [DOI] [PubMed] [Google Scholar]
- 20.Leroy, E. M., S. Baize, V. E. Volchkov, S. P. Fisher-Hoch, M. C. Georges-Courbot, J. Lansoud-Soukate, M. Capron, P. Debre, J. B. McCormick, and A. J. Georges. 2000. Human asymptomatic Ebola infection and strong inflammatory response. Lancet 355:2210–2215. [DOI] [PubMed] [Google Scholar]
- 21.Martini, G. A., and R. Siegert. 1971. Marburg virus disease, p.1–230. Springer, New York, N.Y.
- 22.Moe, J. B., R. D. Lambert, and H. W. Lupton. 1981. Plaque assay for Ebola virus. J. Clin. Microbiol. 13:791–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naniche, D., A. Yeh, D. Eto, M. Manchester, R. M. Friedman, and M. B. Oldstone. 2000. Evasion of host defenses by measles virus: wild-type measles virus infection interferes with induction of alpha/beta interferon production. J. Virol. 74:7478–7484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Panuska, J. R., R. Merolla, N. A. Rebert, S. P. Hoffmann, P. Tsivitse, N. M. Cirino, R. H. Silverman, and J. A. Rankin. 1995. Respiratory syncytial virus induces interleukin-10 by human alveolar macrophages. Suppression of early cytokine production and implications for incomplete immunity. J. Clin. Investig. 96:2445–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pattyn, S. R. 1978. Ebola virus hemorrhagic fever, p.1–436. Elsevier/North-Holland, Amsterdam, The Netherlands.
- 26.Talon, J., C. M. Horvath, R. Polley, C. F. Basler, T. Muster, P. Palese, and A. Garcia-Sastre. 2000. Activation of interferon regulatory factor 3 is inhibited by the influenza A virus NS1 protein. J. Virol. 74:7989–7996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Unanue, E. R., and J. C. Cerottini. 1989. Antigen presentation. FASEB J. 3:2496–2502. [DOI] [PubMed] [Google Scholar]
- 28.Verdijk, R. M., T. Mutis, B. Esendam, J. Kamp, C. J. Melief, A. Brand, and E. Goulmy. 1999. Polyriboinosinic polyribocytidylic acid (poly(I:C)) induces stable maturation of functionally active human dendritic cells. J. Immunol. 163:57–61. [PubMed] [Google Scholar]
- 29.Villinger, F., P. E. Rollin, S. S. Brar, N. F. Chikkala, J. Winter, J. B. Sundstrom, S. R. Zaki, R. Swanepoel, A. A. Ansari, and C. J. Peters. 1999. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J. Infect. Dis. 179(Suppl. 1):S188–S191. [DOI] [PubMed] [Google Scholar]
- 30.Wang, X., M. Li, H. Zheng, T. Muster, P. Palese, A. A. Beg, and A. Garcia-Sastre. 2000. Influenza A virus NS1 protein prevents activation of NF-κB and induction of alpha/beta interferon. J. Virol. 74:11566–11573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young, D. F., L. Didcock, S. Goodbourn, and R. E. Randall. 2000. Paramyxoviridae use distinct virus-specific mechanisms to circumvent the interferon response. Virology 269:383–390. [DOI] [PubMed] [Google Scholar]
- 32.Zhang, P., W. R. Summer, G. J. Bagby, and S. Nelson. 2000. Innate immunity and pulmonary host defense. Immunol. Rev. 173:39–51. [DOI] [PubMed] [Google Scholar]