Rabies is an acute infection of the central nervous system (CNS) and caused by rabies virus or related members of the genus Lyssavirus, family Rhabdoviridae.1 The virus is usually transmitted through a dog bite and produces one of the most important viral encephalitides worldwide, with at least 40 000 deaths reported annually.2 However, it is rare in the United Kingdom, where just 12 cases have been reported since 19773: 11 were imported from overseas, and one occurred in a bat handler infected in Scotland with European bat lyssavirus type 2a.4 Most UK patients presented with furious rabies, which is characterised by hydrophobia and spasms. We report a case of paralytic rabies in a tourist after a two week holiday in Goa, India.
Case report
A woman in her late 30s was admitted to her local general hospital under the orthopaedic surgeons, with lower back pain radiating to the left leg. The pain had started four days earlier, was severe and shooting in nature, and was getting worse. She had been seen twice in casualty in the preceding days, and by the time of admission she was unable to walk. She also had a headache and had vomited once. Three and a half months before admission, during a two week holiday to Goa, India, she had been bitten by a dog; she was walking in the street when a puppy on a lead nipped her on the left leg. There was a slight graze, which she wiped with a tissue, but she did not seek further medical help. Her family reported that she was not aware of the risk of rabies and had not received any pre-exposure or post-exposure vaccination. She had also had intermittent diarrhoea for the past four months, which preceded her trip to India, but gastroscopy and flexible sigmoidoscopy on return from India were normal. On examination she had a temperature of 38.5°C. The left leg, which was extremely painful and required morphine, was areflexic and weak, with sensory loss in L4-S1 dermatomes. She had leucocytosis. A computed tomography scan of the spine looking for a prolapsed disc was normal. Over the next few days she developed a sore throat and had difficulty swallowing, a swollen left eyelid, a goose pimple rash on her skin, and marked bilateral loss of hearing. On day 8 the patient was referred to the medical team, which noted that she was now lethargic and had flaccid weakness in both legs and arms. A provisional diagnosis of Guillain-Barré syndrome was made, and she was treated with intravenous immunoglobulin. A lumbar puncture found clear cerebrospinal fluid with a white cell count of 11 cells/μl (9 lymphocytes, 2 polymorphonuclear cells), a red cell count of 4 cells/μl, protein 2.16 g/l, and a glucose concentration of 3.1 mmol/l, with a plasma glucose measurement of 5.9 mmol/l. By day 11 the patient was deteriorating with increased drowsiness; she was intubated and ventilated. On day 13 she had absent oculocephalic reflexes, and unreactive pupils, and a diagnosis of Bickerstaff's encephalitis was considered. A computed tomography scan of the brain was normal.
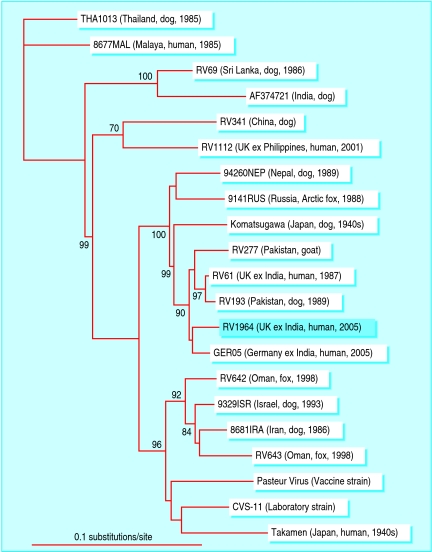
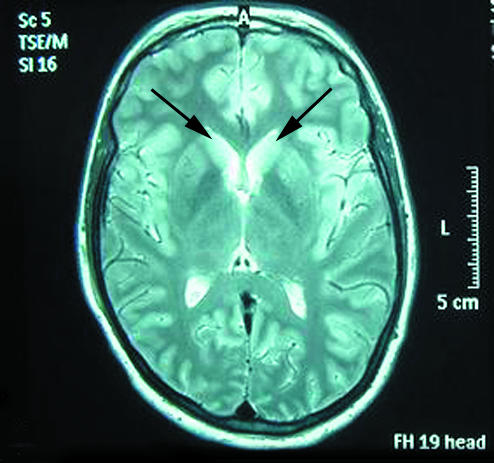
On the 15th day of admission, the infectious diseases unit and specialist neurology centre were contacted for advice. On account of the history of ascending paralysis after a dog bite in India, immediate investigation for rabies (including saliva and serum testing and a skin biopsy from the nape of the neck) was advised, and the patient was transferred for further care. A magnetic resonance imaging scan of the head showed high signal intensity on T2 weighted images bilaterally, in the hippocampal gyri, and the head of the caudate nucleus (fig 1), changes seen previously in rabies5; an electroencephalogram showed encephalopathic changes with periodic complexes. Within five hours of receipt of the specimens, saliva and skin tested with hemi-nested reverse transcriptase polymerase chain reaction (RT-PCR) and real time PCR were positive for rabies virus (figure A on bmj.com).3,6 A 400 base pair region of the nucleoprotein gene was sequenced7 and a phylogenetic tree constructed, which confirmed that the virus amplified was a rabies virus imported from India, rather than indigenous infection with European bat lyssavirus, or a laboratory contaminant (fig 2). Once the PCR diagnosis was confirmed, ionotropic support was withdrawn at the family's request, and the patient died on the 18th day of admission. She had never had hydrophobia, aerophobia (fear of air), hypersalivation, or spasms. With the family's permission, brain tissue was obtained after death by needle biopsies through the foramen magnum and supraorbital routes; this confirmed the diagnosis of rabies by both fluorescent antibody testing4 and by PCR. In addition, rising antirabies antibody titres were found in the serum, as measured by the fluorescent virus neutralisation assay (figure A on bmj.com).4
Fig 1.
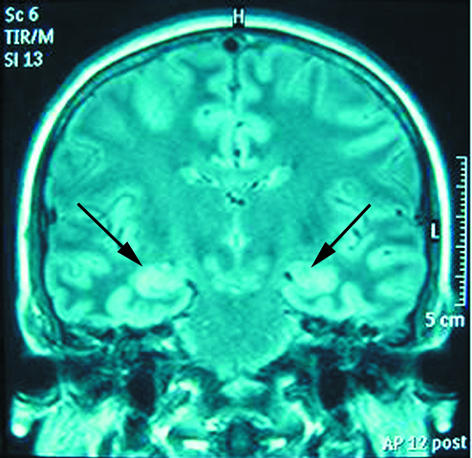
T2 weighted magnetic resonance imaging showing high signal (arrows) bilaterally in the hippocampal gyri (left image, T2 fluid attenuated inversion recovery—FLAIR), and the head of the caudate nucleus (right image, T2 turbo spin echo), which have been seen before in rabies
Fig 2.
Phylogenetic tree depicting the relation between the rabies virus sequence amplified from our patient (RV1964—boxed) and other viruses originating in Asia. The horizontal branch lengths represent the extent of difference between the strains (expressed as nucleotide substitutions per nucleotide site), and the closer viruses are on the tree, the more closely they are related
Discussion
This case serves as an important reminder of the risk of rabies for any traveller to a country where rabies is endemic, even tourists on a short visit to a holiday resort, and provides several useful lessons. Most importantly, travellers need to know whether they are visiting a country where rabies is endemic, and that any dog bite in such a country must be taken seriously by the recipient and any medical staff dealing with the patient subsequently.8 Although rabies is more likely after the bite of a stray or rabid dog, our case shows that even an apparently innocuous bite from a pet must be considered carefully, especially if it was unprovoked: such an animal may be in the early stages of rabies. The wound should be cleaned carefully and, depending on the circumstances, post-exposure vaccination and immunoglobulin given; detailed recommendations are available on the website of the Department of Health.9 Pre-exposure vaccination, which is recommended in some circumstances, simplifies the post-exposure vaccination regime and reduces the risk of developing rabies. If no post-exposure vaccination is given, the risk of developing rabies after the bite of a rabid dog is about 50%, depending on the location and severity of the bite.10
Most patients present with furious rabies, which is characterised by hydrophobia or aerophobia, or both, and associated with phobic or inspiratory spasms. However, up to one third of patients may present with the paralytic or “dumb” form of the disease.10 This is often harder to diagnose clinically, and has been confused with Guillain-Barré syndrome before, particularly the acute motor axonal form of this syndrome.11 However, headache and fever at presentation, asymmetry of limb weakness, bladder involvement, and cells in the cerebrospinal fluid are clues that flaccid paralysis could be due to a virus infection of the anterior horn cells in the spinal cord, rather than immunologically mediated Guillain-Barré syndrome.12 Severe pain in the bitten limb, which is common in rabies, itching, and goose pimples may be additional clues of rabies infection.
Patients with suspected rabies should be investigated by collecting saliva, cerebrospinal fluid, serum, and a punch biopsy from the skin at the nape of the neck, which includes hair follicles containing peripheral nerve endings. A fluorescent antibody test to detect rabies virus antigen in a skin biopsy is one of the best tests13; in addition, our report confirms earlier observations3 that polymerase chain reaction of the saliva is also a useful rapid diagnostic test. Because initial results may be negative, investigations should be repeated on a daily basis.14 In some patients, all tests before death will be negative, and the diagnosis is made only after death by examining brain material. This can be obtained at autopsy, or by biopsy with a Vim-Silverman needle or other long biopsy needle, such as that used for aspirating bone marrow.13 Without such investigation, the diagnosis may not be made. It is not known how many patients diagnosed with fatal Guillain-Barré syndrome in the past actually had paralytic rabies11; however, every year many cases of encephalitis are diagnosed clinically for which the causative organism is not determined.15
Rapid diagnosis of rabies is important for appropriate infection control and public health measures to be instituted, and rabies is a notifiable disease.9 Although no well documented cases of transmission between humans have been reported (except through organ transplantation16), barrier nursing is used, vaccination offered to relatives and exposed staff, and reassurance given to other staff members; in addition, specimens sent to non-specialist laboratories may need to be tracked down. Until recently, once clinical features developed, rabies was considered almost universally fatal. The only documented survivors had received some vaccination before or after exposure17 but not complete, prompt post-exposure vaccination, which makes them essentially failures of the vaccination regime.10 However, in 2004 a teenager in the US state of Wisconsin, who developed rabies after a bat bite, was successfully treated with a combination of ketamine, midazolam, ribavirin, and amantadine.18 Her treatment was instituted on the fifth day of disease, when she was semi-obtunded, with cranial nerve signs and ataxia. We considered such treatment for our patient but thought that the disease was too advanced. Although rabies is rare in the UK, we are likely to continue to see sporadic cases. The potential for treatment in rabies provides an additional impetus to try to make the diagnosis as soon as possible.
Supplementary Material
Acknowledgments
We thank the patient's family for permission to publish this case; we are also grateful to our many clinical, nursing, technical, public health, infection control and administrative colleagues at the Walton Centre for Neurology and Neurosurgery, the Pennine Acute Hospitals NHS Trust, the North Manchester General Hospital, Liverpool School of Tropical Medicine, the Veterinary Laboratories Agency (Weybridge), the Health Protection Agency, and the Department of Health, and the Department for Food, Environment and Rural Affairs (DEFRA), who were involved in this case.
 Editorial by Pounder
Editorial by Pounder
A history of a dog bite from a rabies endemic country should always be taken seriously
 Further details about
figure 2, Genbank accession numbers for the strains of virus, and a supplementary figure, showing hemi-nested reverse transcriptase-polymerase chain reaction on diagnostic samples and serological results, are on bmj.com
Further details about
figure 2, Genbank accession numbers for the strains of virus, and a supplementary figure, showing hemi-nested reverse transcriptase-polymerase chain reaction on diagnostic samples and serological results, are on bmj.com
Contributors: All authors had the idea; TS and ARF wrote the paper with contributions from all authors. TS is the guarantor.
Funding: None.
Competing interests: None declared.
Ethical approval: Not needed.
References
- 1.Rupprecht CE, Hanlon CA, Hemachudha T. Rabies re-examined. Lancet Infect Dis 2002;2: 327-43. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. World Health Organization rabies fact sheet. Geneva: WHO, 2001. www.who.int/mediacentre/factsheets/fs099/en/ (accessed 22 Jul 2005).
- 3.Smith J, McElhinney L, Parsons G, Brink N, Doherty T, Agranoff D, et al. Case report: rapid ante-mortem diagnosis of a human case of rabies imported into the UK from the Philippines. J Med Virol 2003;69: 150-5. [DOI] [PubMed] [Google Scholar]
- 4.Fooks AR, McElhinney LM, Pounder DJ, et al. Case report: isolation of a European bat lyssavirus type 2a from a fatal human case of rabies encephalitis. J Med Virol 2003;71: 281-9. [DOI] [PubMed] [Google Scholar]
- 5.Laothamatas J, Hemachudha T, Mitrabhakdi E, Wannakrairot P, Tulayadaechanont S. MR imaging in human rabies. AJNR Am J Neuroradiol 2003;24: 1102-9. [PMC free article] [PubMed] [Google Scholar]
- 6.Wakeley PR, Johnson N, McElhinney LM, Marston D, Sawyer J, Fooks AR. Development of a real-time, TaqMan reverse transcription-PCR assay for detection and differentiation of lyssavirus genotypes 1, 5, and 6. J Clin Microbiol 2005;43: 2786-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson N, Lipscomb DW, Stott R, Gopal Rao G, Mansfield K, Smith J, et al. Investigation of a human case of rabies in the United Kingdom. J Clin Virol 2002;25: 351-6. [DOI] [PubMed] [Google Scholar]
- 8.Wilde H, Briggs DJ, Meslin FX, Hemachudha T, Sitprija V. Rabies update for travel medicine advisors. Clin Infect Dis 2003;37: 96-100. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health. Rabies—draft updated chapter 27 of immunisation against infectious disease 1996—“The Green Book.” www.dh.gov.uk/assetRoot/04/11/09/70/04110970.pdf (accessed 15 Aug 2005).
- 10.Hemachudha T, Laothamatas J, Rupprecht CE. Human rabies: a disease of complex neuropathogenetic mechanisms and diagnostic challenges. Lancet Neurol 2002;1: 101-9. [DOI] [PubMed] [Google Scholar]
- 11.Sheikh KA, Ramos-Alvarez M, Jackson AC, Li CY, Asbury AK, Griffin JW. Overlap of pathology in paralytic rabies and axonal Guillain-Barre syndrome. Ann Neurol 2005;57: 768-72. [DOI] [PubMed] [Google Scholar]
- 12.Solomon T, Willison H. Infectious causes of acute flaccid paralysis. Curr Opin Infect Dis 2003;16: 375-81. [DOI] [PubMed] [Google Scholar]
- 13.Warrell MJ. Rabies. In: Cook G, Zumlar A, eds. Manson's tropical diseases. 21st ed. London: Saunders, 2003: 807-21.
- 14.Fooks AR, Johnson N, Brookes SM, Parsons G, McElhinney LM. Risk factors associated with travel to rabies endemic countries. J Appl Microbiol 2003;94(suppl): 31S-36S. [DOI] [PubMed] [Google Scholar]
- 15.Davison KL, Crowcroft NS, Ramsay ME, Brown DW, Andrews NJ. Viral encephalitis in England, 1989-1998: what did we miss? Emerg Infect Dis 2003;9: 234-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Srinivasan A, Burton EC, Kuehnert MJ, Rupprecht C, Sutker WL, Ksiazek TG, et al. Transmission of rabies virus from an organ donor to four transplant recipients. N Engl J Med 2005;352: 1103-11. [DOI] [PubMed] [Google Scholar]
- 17.Jackson AC, Warrell MJ, Rupprecht CE, Ertl HC, Dietzschold B, O'Reilly M, et al. Management of rabies in humans. Clin Infect Dis 2003;36: 60-3. [DOI] [PubMed] [Google Scholar]
- 18.Willoughby RE Jr, Tieves KS, Hoffman GM, Ghanayem NS, Amlie-Lefond CM, Schwabe MJ, et al. Survival after treatment of rabies with induction of coma. N Engl J Med 2005;352: 2508-14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.