Abstract
Antimicrobial peptides (AMPs) are essential components of the innate immune response. They have direct killing ability as well as immunomodulatory functions. Here, we describe techniques to identify specific AMPs involved in the protection against microbial keratitis, a vision threatening infection of the cornea of the eye which is the most serious complication of contact lens wear. Specifically we detail the use of siRNA technology to temporarily knockdown AMP expression at the murine ocular surface in vivo and then describe ex vivo assays to determine the level of bacteria, relative number of neutrophils, and levels of cytokines, chemokines, and AMPs in infected corneas.
Keywords: Antimicrobial peptide, Inflammation, Keratitis, Neutrophil, Pseudomonas
1. Introduction
Antimicrobial peptides (AMPs) are small, generally cationic peptides that can kill a range of microorganisms. These molecules are also known to modulate mammalian cell behavior and can, for example, influence the immune response and wound healing [1, 2]. Several groups of AMPs have been identified in mammals including humans, with the primary ones being defensins and cathelicidins [3, 4]. It is important to understand how AMPs function in vivo and to gain a deeper insight in to their potential as novel pharmaceutical agents to treat and prevent infection as well as modulate processes such as wound healing.
Here we describe techniques that can be utilized to study the role of endogenously expressed AMPs and efficacy of exogenously applied AMPs in a murine model of microbial keratitis. The latter refers to infection of the cornea of the eye, the transparent covering of the pupil and iris, and it may lead to blindness or even enucleation if not treated quickly or if unresponsive to treatment. Microbial keratitis is the most serious complication of contact lens wear but may also occur after trauma to the eye [5–8]. Common agents include the Gram-negative bacterium Pseudomonas aeruginosa, the fungus Fusarium solani, and protozoa Acanthamoeba spp. [2, 7]. Here we use bacterial keratitis induced by P. aeruginosa as the model as this pathogen is the most common cause of contact lens-related microbial keratitis in Western countries [2, 5, 7]. The first assay is in vivo knockdown of AMP expression by topical application of siRNA to the ocular surface. This approach allows for the specific knockdown of one or more AMPs so that the role of endogenously produced AMPs in modulating the severity of corneal infection can be assessed directly. The development of knockout technology to eliminate genetic expression has led to many important discoveries regarding the participation of specific molecules in various biological processes. There have been a small number of AMP knockout mice created, and these have provided valuable information in regard to the involvement of AMPs including defensins mBD-1 [9–11] and mBD-3 [12, 13] and the cathelicidin CRAMP [13–18] in the recovery/protection from various infections and of β-defensins in sperm maturation [19]. However, genetic knockouts are not available for all of the AMPs one may have an interest in studying. Transient knockdown by siRNA interference is an alternative way to impair local expression of specific AMPs and hence study their role in specific infections such as keratitis. The siRNA is first administered 24 h before initiation of the infection, and then additional doses (at half the starting concentration) are administered over several days to ensure that AMP expression remains knocked down during the course of the experiment. This approach, which is described in this chapter, has been used successfully to study the involvement of defensins in experimental microbial keratitis induced by P. aeruginosa and F. solani [13, 20, 21].
The subsequent assays are viable bacterial counts and myeloperoxidase assays to determine how many pathogens and neutrophils are present in the cornea at a given time during infection. These assays provide insight regarding the underlying pathology of the response, for example, for testing the efficacy of a topically applied AMP, a reduction in the number of viable bacteria suggests that the AMP is directly killing the infecting pathogen. Quantitation of cytokines and chemokines is also informative in regard to the pathological changes, for example, high levels of infiltrating neutrophils and corneal damage may be correlated to excessive corneal levels of neutrophil-specific chemokines. Also described are methods to determine the level of AMP (mRNA and protein) at the ocular surface. This can, for example, reveal which AMPs are differentially modulated by pathogen exposure hence indirectly implicating them in protection against particular pathogens.
2. Materials
All solutions should be prepared using ultrapure water and analytical grade reagents. Reagents to be used in vivo should be kept sterile by preparation in a Class II biological safety cabinet and if necessary filtered using a 0.2 μm filter unit prior to storage or use. Use of animals requires prior approval by the relevant institutional/local regulatory body. All waste should be disposed of appropriately and experiments conducted at biosafety level 2 with relevant personal protective equipment provided to all laboratory personnel.
2.1. AMP Knockdown Using siRNA
AMP-specific and scrambled control siRNA.
6- to 8-week-old C57BL/6 mice.
Ketamine.
Xylazine.
Hamilton syringe (10 μL, 26 gauge) for subconjunctival injection.
Surgical stereomicroscope.
P. aeruginosa (ATCC 19660) suspended at 2 × 108 colony-forming units (cfu)/mL in phosphate buffer: 8.2 mM Na2HPO4, 1.8 mM KH2PO4, pH 7.4.
2.2. Corneal Homogenate Preparation
Surgical equipment for corneal harvesting: 2 pairs of small scissors, 1 pair of large blunt forceps, 2 pairs of small forceps—blunt and sharp, iris scissors.
Sterile plastic dishes.
Premade sterile 10× phosphate-buffered saline (PBS)—pH 7.4, diluted 1:10 in sterile water.
Kinematica AG homogenizer.
Ultrasonic dismembrator.
2.3. Viable Bacterial Counts
Pseudomonas isolation agar: glycerol is added to isolate P. aeruginosa based on pigment formation. Dissolve 45 g of Pseudomonas isolation agar powder in 1 L of purified water, add 20 mL of sterile glycerol, then place the mixture on a stirring hot plate, boil for 1 min to dissolve the powder completely, autoclave the mixture at 121 °C for 15 min to sterilize to make the plates pour 25–30 mL of the cooled mixture into sterile 100 mm dishes, and allow to dry in a Class II Biosafety cabinet.
Premade sterile 10× PBS—pH 7.4, diluted 1:10 in sterile water.
Shaker incubator.
Alpha Imager Documentation System.
2.4. Myeloperoxidase Assay and ELISAs
Myeloperoxidase (MPO).
Phosphate buffer: 50 mM KH2PO4 at pH 6.
O-dianisidine dihydrochloride (O-d-d).
Premade sterile 10× PBS—pH 7.4, diluted 1:10 in sterile water.
Hexadecyltrimethylammonium bromide: prepare a 0.5 % (w/v) solution by dissolving 0.5 g/100 mL in 50 mM KH2PO4, pH 6.
Table-top Eppendorf centrifuge.
30 % Hydrogen peroxide solution.
Corning 96 well plates.
FLUOstar Omega spectrophotometer plate reader.
Liquid nitrogen.
BCA protein assay kit.
ELISA kits for cytokines/chemokines of interest.
2.5. Real-Time PCR for AMP Expression
Aerosol-resistant (ART) barrier filter tips.
ToTALLY RNA total RNA isolation kit.
Cell lysis buffer—denaturation solution from the ToTALLY RNA kit.
DNase I.
NanoDrop 2000 spectrophotometer.
SuperScript III First-Strand Synthesis System.
SYBR green quantitative PCR Master Mix kits.
AMP-specific forward and reverse primers.
Table-top Eppendorf centrifuge.
Sterile 96 well polypropylene PCR plates.
PCR tubes.
DNase-/RNase-free, pyrogen safe PCR plate caps.
Real-time thermal cycler Mx3005p.
2.6. Immunostaining for Corneal AMP Protein Expression
General: Coplin jars for washing; large petri dishes, paper towels, and wooden coffee stirrers to create moist chambers; Pap pen.
Tissue-Tek optimal cutting temperature compound.
Superfrost/Plus Microscope Slides.
Leica CM 1950 Cryostat.
Sterile, cold (4 °C) premade Dulbecco’s PBS.
Acetone.
Blocking solution: 5 % (w/v) bovine serum albumin + 10 % normal serum from relevant species + 0.1–0.3 % (v/v) Triton X-100 diluted in PBS. Store at 4 °C.
Control serum/IgG: Immunopure Normal goat serum, rabbit serum, goat control IgG.
Primary AMP antibodies: goat anti-CRAMP, rabbit anti-mBD3, rabbit anti-mBD4.
Secondary antibodies: Donkey anti-goat-Alexa Fluor 546, goat anti-rabbit-Alexa Fluor 546.
Vectashield® prolong gold mounting medium.
Cover slips—#1, 22 × 60 mm.
DeltaVision Core inverted microscope.
3. Methods
3.1. In Vivo AMP Knockdown by siRNA
AMP-specific siRNA or scrambled control siRNA prepared as follows: specific or scrambled siRNA is diluted in sterile water to make a stock concentration of 10 μM. The stock is then diluted to 8 or 4 μM concentrations, aliquoted, and stored at −20 °C until use. Aliquots should not be subject to freeze-thaw cycles. Any excess should be disposed of and fresh aliquots used for each administration. The product is thawed on ice ready for use.
24 h prior to ocular infection, 6–8-week-old C57BL/6 mice are anesthetized by intraperitoneal injection of a mix of ketamine (100 mg/kg of body weight) and xylazine (10 mg/kg) with the level of anesthesia being checked by lack of response to a toe pinch.
The anesthetized animal is positioned under a surgical stereomicroscope, and 5 μL of 8 μM AMP-specific siRNA or scrambled control siRNA is injected subconjunctivally into the superior-temporal quadrant of the designated eye (usually the right eye is used as the experimental eye) using a 26 g Hamilton syringe. Flush the syringe ten times with sterile water (the diluent for the siRNA) between animals to prevent cross contamination.
24 h later the mouse eye is inoculated with bacteria to create the infection. The animal is again anesthetized and placed under the surgical stereomicroscope. Three parallel 1 mm scratches are made using a 27½ gauge needle on the central cornea of the experimental eye to create a central corneal wound. Five microliter (1 × 106 cfu in phosphate buffer) of P. aeruginosa (ATCC 19660) is then applied onto the wounded cornea using a Gilson pipette.
Five microliter of 4 μM AMP or scrambled control siRNA is applied topically 12 h postinfection and every 12 h thereafter for the days following infective agent challenge (see Note 1).
3.2. Ex Vivo Assays
Laboratory animals are infected with the pathogen of choice in the cornea of one eye. The precise details vary with pathogen and animal species, but as a general rule it is necessary to disrupt the corneal surface in some way (e.g., by superficial scratches on the corneal surface as described above (see Subheading 3.1, step 4)) in order to get the infection to take hold. At specific time points during the experiment, animals are euthanized as per the institutional approved method; corneas are then harvested under a dissecting microscope for analysis using the following procedures. Here we use infection with P. aeruginosa in mice as the model, but the procedures are readily applicable to other pathogens such as fungi and other species such as rat.
3.2.1. Preparation of Corneal Homogenates
Corneal homogenates are prepared as described below and then used to determine viable bacterial counts, MPO activity, and the levels of cytokines and chemokines (or other analytes of interest). The assays for viable counts and MPO should be performed on the same day as the homogenate is prepared. The remaining volume of homogenate can be stored frozen for determination of cytokines/chemokines at a later date.
Harvest corneas from three to five control or P. aeruginosa-19660-infected euthanized mice under a dissecting microscope.
Pool the corneas in 200 μL of sterile PBS/cornea in an Eppendorf tube and place on ice (see Note 2).
Homogenize the pooled corneas using a Kinematica AG homogenizer for 30 s at a setting of 5, pulsing it ten times by moving the tube up and down. The process is repeated two times keeping the tube of tissue on ice in between. To avoid cross contamination between samples, rinse the probe at least three times with sterile PBS between each sample. For preparation and maintenance of the probe, see Note 3.
Place the tube containing the sample in a small beaker filled with ice, and then sonicate at a setting of 3–4 and a rate of ten strokes for 10 s. Repeat this for a total of three times. To avoid cross contamination between samples, rinse the probe at least three times with sterile PBS between each sample. Preparation and maintenance of the probe are as for the homogenizer (see Note 3).
3.2.2. Viable Bacterial Counts
Using 100 μL of the homogenate prepared above, make a series of tenfold dilutions by mixing 10 μL of homogenate and 90 μL of sterile PBS. Making and plating 6–8 dilutions should ensure that at least one of the dilutions can be easily counted.
Plate 10 μL of each dilution in duplicate on to Pseudomonas isolation agar plates using bacterial spreaders. For fungal plating, see Note 4.
Incubate the plates for 16–18 h at 37 °C.
Take images of the plates with an Alpha Imager Documentation System, and then count the number of colonies by direct counting. The upper limit of detection for accurate counting is 200 cfu/plate.
3.2.3. Myeloperoxidase (MPO) Assay Protocol
Quantitation of MPO activity is used as an indicator of neutrophil (PMN) recruitment to the site of infection.
Add 10 μL of 0.5 % hexadecyltrimethylammonium bromide to 90 μL corneal homogenate (prepared as in Subheading 3.2.1) in an Eppendorf tube.
Sonicate the samples prepared in step 1: place the tube in a small beaker of ice, and sonicate at levels 3–4 of the ultrasonic dismembrator, two times for 5 s for a total of 10 s.
Freeze each sample in liquid nitrogen and then thaw. Repeat this for a total of three times (see Note 5).
Centrifuge the samples at 13,000 × g at 4 °C for 20 min in a table-top Eppendorf centrifuge.
Make up the MPO standards using 50 mM phosphate buffer, pH 6. Begin by preparing 0.1 U of MPO, and then make 9 twofold serial dilutions. Make sufficient volume of each standard to allow each to be run in duplicate or triplicate 10 μL volumes on the plate.
Add 10 μL of each standard to duplicate wells of a flat-bottomed 96 well plate and 10 μL of each sample (in triplicate).
Make up the ODD mixture by dissolving 0.00334 g O-dianisidine dihydrochloride (final concentration 0.0167 % w/v) in 20 mL of the 50 mM phosphate buffer, then add 1.33 μL of 30 % hydrogen peroxide (final hydrogen peroxide is 0.002 % v/v), and protect the tube from light by covering with aluminum foil.
Initiate the reaction by adding 90 μL of the ODD mixture (step 8) to each well.
Place the plate in the plate reader and read every 15 min for 120 min at 450 nm, and plot in comparison to the standard curve generated on the same plate.
Results are expressed as relative units of MPO activity per cornea. 1 MPO unit is proportional to 2 × 105 infiltrating neutrophils [22, 23].
3.2.4. Enzyme-Linked Immunosorbent Assays for Cytokines, Chemokines, and Other Analytes
Corneal homogenates prepared as described above (see Subheading 3.2.1, steps 1–4) are centrifuged at 4000 × g at 4 °C for 20 min. Collect the supernatant and store frozen at −80 °C until ready to perform ELISAs (see Note 6).
Determine the total protein concentration in each sample by a standard protein assay kit such as the BCA kit.
Levels of analytes of interest such as cytokines and chemokines IL-1β, IL-6, TNF-α, MIP-2, and KC are quantitated in the corneal homogenate supernatants by specific ELISA kits. The typical sample size used is 100 μL of the supernatant and triplicate samples are plated. The assay is performed as per the kit manufacturer’s instructions and data expressed as amount/mg total protein. For some analytes the supernatant may need to be diluted in order for the reading to fall within the appropriate range (above 20 % but less than 80 %) on the standard curve. This needs to be determined empirically for each analyte of interest.
3.2.5. Relative Quantitative Real-Time PCR for AMP Expression
Harvest and pool 6–8 corneas from control or infected mice in RNA lysis buffer (200 μL/cornea) on ice (see Note 7).
-
Extract total RNA from each sample using ToTALLY RNA total cellular RNA kit as per the manufacturer’s instructions.
All samples should be treated with DNase I (RNase-Free DNase Set kit) to avoid any genomic DNA contamination as follows.
Mix 10 μL DNase I with 70 μL Buffer RDD from the kit by gently flicking the Eppendorf tube. Pulse briefly in a microtube mini-centrifuge to collect all residual liquid from the sides of the tube. DO NOT VORTEX. Make sufficient volume for all samples to be tested.
Add 80 μL of the diluted DNase I to each RNA sample, and mix by flicking the tube gently. Place in a rack and leave at room temperature for 30 min.
Proceed with the RNA phenol-chloroform extraction as per the instructions of the ToTALLY RNA kit.
Quantitate the amount of RNA in 2 μL of the DNase I-treated sample using a NanoDrop spectrophotometer (see Note 8)
For each sample 1 μg of total RNA is reverse transcribed to make 20 μL of cDNA reaction volume using the SuperScript III First-Strand Synthesis System, which contains Moloney murine leukemia virus reverse transcriptase (RT). Each reaction tube will contain a final volume of 20 μL composed of 10 μL 2× kit buffer; 3 μL oligo dT, 1 μL RT/Block, 6 μL RNA + RNase-free water (i.e., 1 μg sample RNA + appropriate volume of RNase-free water for a final sample volume of 6 μL). Samples containing RNase-free water instead of RT serve as negative controls. The incubation conditions for the RT step are 25 °C for 5 min, 42 °C for 45 min, and 95 °C for 5 min.
At the end of the RT reaction, dilute the 20 μL of reaction mix 1:1 with 20 μL sterile RNase-free water.
Prepare the samples for relative quantitative real-time PCR amplification performed using SYBR green PCR Master Mix kits. Gene-specific optimized primers to quantitate the mRNA expression of various murine AMPs and a relevant housekeeping gene (in this case we use RNA polymerase II, RPII) are presented in Table 1 (see Note 9). All steps and thawing of reagents are performed on ice, and the PCR plate is kept in a cold block, while the samples are being added. The preparation steps are as follows:
Dilute 1 μL ROX reference dye in 499 μL RNase-free water.
Thaw primers on ice and dilute in sterile RNase-free water, and mix to give a final concentration of 10 μM Forward (F) and 10 μM Reverse (R) in an Eppendorf tube. The premixed primers can be stored in small aliquots at −20 °C for up to 2 months.
Prepare the PCR reaction mix: 12.5 μL SYBR Green 2× Master Mix + 0.375 μL of the diluted reference dye + 0.5 μL of premixed gene-specific F and R primer mix + 9.625 μL RNase-free water giving a total final volume of 23 μL per reaction. These are the volumes for a single reaction—the actual volume should be scaled up based on the number of samples to be analyzed/gene of interest and accounting for performing each reaction in triplicate.
Pipette 23 μL of the reaction mix in to the wells of a PCR plate.
Add 2 μL of each cDNA to be teted in to the relevant wells to give a final PCR reaction volume of 25 μL.
Seal the PCR plate tightly and spin the plate briefly (30 s, 200 × g, room temperature) in a centrifuge equipped with a 96 well plate rotor to bring all of the contents to the bottom of the wells.
Place the plate in the real-time thermal cycler and run under the following conditions: 10 min denaturation at 95 °C followed by 40 cycles of amplification as follows—denaturation, 95 °C for 30 s; annealing, 56 °C for 1 min; and extension, 72 °C for 30 s.
Perform initial data analysis using the Stratagene Mx3005p software. Disassociation melt curve analysis should be included to ensure reaction specificity (see Note 10).
To determine the relative fold change in AMP expression in infected versus control mice, the data for the amplified gene products should be normalized to the housekeeper RPII and calibrated to uninfected samples and relative fold expression calculated using the 2ΔΔct method [24].
Table 1.
The table shows the sequences of primers used to determine β-defensin, cathelicidin (CRAMP), and RNA polymerase II (RPII, housekeeping gene) expression in normal and infected murine corneas [13]
| Primer | Forward/reverse | Sequence (5′–3′) |
|---|---|---|
|
| ||
| mBD1 | Forward | CTGGGAGTTTCACATCCTCTC |
| Reverse | CTCCATGTTGAAGGCATTTGT | |
|
| ||
| mBD2 | Forward | CTACCAGCCATGAGGACTCTC |
| Reverse | GTACTTGCAACAGGGGTTCTT | |
|
| ||
| mBD3 | Forward | GGATCCATTACCTTCTGTTTGC |
| Reverse | ATTTGAGGAAAGGAACTCCAC | |
|
| ||
| mBD4 | Forward | GCTTCAGTCATGAGGATCCAT |
| Reverse | CTTGCTGGTTCTTCGTCTTTT | |
|
| ||
| mBD5 | Forward | CCTTCTCTTTGCATTTCTCCT |
| Reverse | TTTCTCTTGCAGCAGTTGAGA | |
|
| ||
| mBD6 | Forward | TACCTGCTCTTTGCCTTTATCC |
| Reverse | TTCTGGCACTTATTCACATTGC | |
|
| ||
| mBD14 | Forward | TCTTGTTCTTGGTGCCTGCT |
| Reverse | CGACCGCTATTAGAACATCGAC | |
|
| ||
| CRAMP | Forward | GCCGCTGATTCTTTTGACAT |
| Reverse | GCCAAGGCAGGCCTACTACT | |
|
| ||
| RPII | Forward | CTACACCACCTACAGCCTCCAG |
| Reverse | TTCAGATGAGGTCCATGAGGAT | |
3.2.6. Immunostaining for Corneal AMP Protein Expression
The antibodies and methodology described here are to stain for the presence of murine defensins or cathelicidin (CRAMP), but the method can be optimized and used to determine the expression of other molecules of interest.
Euthanize the mouse, then harvest the whole globe, and rinse with sterile cold Dulbecco’s PBS and embed in orientation (superior, inferior, nasal, temporal) pre-marked small cryomolds containing Tissue-Tek optimal cutting temperature compound, and rapidly freeze by submerging in liquid nitrogen. Store at −80 °C until ready to use.
Cut 10 μm thick sections on a cryostat and mount (4–6 sections/slide) on Superfrost slides. If need be store slides at −80 °C until ready to perform the staining.
Preparation for staining: Prepare 1–2 L of PBS and store in fridge. Decant some acetone in to a small glass vial and chill in the fridge overnight. Prepare the blocking solution as described in Subheading 2.7—10 mL is sufficient for five slides (see Note 11).
If using stored frozen sections, thaw the sections for 60 min at room temperature before use.
Fix sections in ice-cold acetone for 3 min. Simply add sufficient acetone to cover each section. At the end of the 3 min, tip off the acetone, catching the liquid in a paper towel.
Rinse the sections in PBS three times, dry off carefully around sections with a Kimwipe, and then use a Pap pen to draw around each section so forming a “well” into which the antibodies can be added.
Place the slides in to a moist chamber (see Note 12) and add 100–200 μL (enough to cover the section completely) of blocking solution and incubate for 2 h at room temperature.
-
During the blocking step, prepare the appropriate dilutions of the desired primary antibodies in blocking solution. For polyclonal antibodies, use a nonspecific IgG from the same species as the primary antibody was raised in as the nonspecific binding control. For monoclonal antibodies, use the relevant non-specific isotype control from the same species as the primary antibody (see Note 13). The amount of primary antibody and IgG/isotype control should be the same. For our purposes [13], we use the following dilutions of primary and control antibodies:
Goat anti-CRAMP (0.2 μg/μL) diluted 1:50; goat IgG (0.4 μg/μL) diluted 1:100.
Rabbit anti-mBD-3 (0.2 μg/μL) diluted 1:50; rabbit IgG (1 μg/μL) diluted 1:250.
Rabbit anti-mBD-4 (0.2 μg/μL) diluted 1:50; rabbit IgG (1 μg/μL) diluted 1:250.
At the end of the blocking step, remove the blocking reagent by tipping the slide and catching the fluid in a paper towel. Then add 50–100 μL (sufficient to cover the section) of diluted primary antibody. Incubate overnight at 4 °C.
At the end of the incubation in primary antibody, wash the sections three times in PBS for 5 min each time.
Repeat the blocking step by adding 100–200 μL blocking solution, and incubate for 30 min at room temperature.
During the second blocking step, prepare 1:400 dilution of the relevant secondary antibodies in blocking reagent. Secondary antibodies for our purposes were goat anti-rabbit alexa-546 for mBD3 and mBD4 and donkey anti-goat Alexa-5 46 for CRAMP.
At the end of the second blocking step, remove the blocking reagent by tipping the slide and catching the fluid in a paper towel. Add 50–100 μL of diluted secondary antibody, and incubate the sections for 60 min at room temperature in the dark (cover with aluminum foil or place in a closed cupboard).
Sections are then washed three times in ice-cold PBS for 5 min each time. Remove the wash solution by tipping the slide and catching the fluid in a paper towel.
The labeled slides are then dried by using a Kimwipe to dab off any excess fluid and cover slips mounted with Vectashield® prolong gold mounting medium (see Note 14).
The slides are left at room temperature overnight in the dark to better bond the mounting medium and then can be stored at 4 °C (in the dark) until visualized by fluorescence microscopy.
4. Notes
The efficacy and specificity of siRNA silencing should be tested by performing quantitative real-time PCR and/or immunostaining for the AMP of interest. RT-PCR results showed a 60–74 % decrease in the expression of AMPs compared to untreated or scrambled siRNA control 3 days postinfection [13, 21]. How long the AMP expression remains knocked down after terminating siRNA treatment has not been reported. Wu et al. [21] report a significant effect 5 days postinfection following knockdown of mBD-4 despite siRNA application being terminated 3 days postinfection. This suggests that AMPs remain knocked down for some time.
While pooling of multiple corneas is preferable to maximize the amount of material for analysis, if tissue is limited, repeatable data have been obtained by using as few as 1–2 corneas in 100 μL of PBS for MPO and viable pathogen count analyses ([25], unpublished data from our lab).
Immediately before the first sample, clean the probe of the homogenizer by rinsing in sterile water twice. Dry off with a Kimwipe and then wash twice again with sterile PBS. Between samples rinse with sterile PBS at least three times. After the last sample rinse with PBS, then sterile water, and finally 70 % ethanol and allow the probe to air-dry.
For viable count of fungal pathogens: Plate samples of the serial dilutions on Sabouraud Dextrose agar plates in duplicate. Incubate the plates for 48–72 h at 30 °C and then image and count the number of culturable units.
To freeze hold the tube containing the sample with a pair of tongs and dip the end in to the liquid nitrogen for 10–20 s. To thaw remove the tube from the liquid nitrogen, place on the lab bench and allow to thaw at room temperature for about 1 min. Liquid nitrogen should be handled with care. Always use thick gloves and eye protection and work with the smallest amount possible. Always use a suitable container such as an ethylene-vinyl acetate laboratory ice bucket or Styrofoam container. Any excess should be clearly labeled and left to evaporate in a fume hood.
If multiple ELISAs are to be performed, then it is optimal to store multiple small volume aliquots to avoid the risks associated with freeze/thawing of larger volume samples. In order to ensure sufficient material for meaningful analysis of multiple analytes, the number of corneas harvested and pooled can be increased to 8–10/1 mL PBS. If material is limited, then measuring analytes by a cytometric bead assay (such as the Luminex platform) can enable the detection of multiple analytes in a much smaller volume of supernatant.
While harvesting corneas of C57BL/6 mice for analysis, special care must be taken to avoid contamination with pigmented tissue as melanin is known to interfere with polymerase activity hence RT-PCR reactions [26].
The purity of the RNA is assessed using the ratio of absorbance at 260 and 280 nm as read by the NanoDrop spectrophotometer. A ratio of approximately 2 is desirable. A ratio of less than 2 indicates the presence of contaminants such as protein and phenol in which case re-extraction of the RNA may be required.
Although the primers and methodology reported here were optimized to test mouse defensins and cathelicidin (CRAMP), this method can be optimized and used to determine the expression of other molecules of interest.
Sometimes it is desirable (e.g., to check transcript size) to visualize the PCR products by agarose gel electrophoresis. If this is the case, then the dissociation melt curve analysis step should be omitted and the products generated at the end of the last cycle of PCR amplification loaded directly on to a 1.5 % agarose gel and stained with ethidium bromide for analysis.
The blocking reagent should contain 10 % normal serum. The serum should be from a different species to that in which the primary antibody was raised, e.g., if the primary antibody is a rabbit polyclonal, then do NOT use normal rabbit serum in the blocking reagent.
To make a moist chamber (Fig. 1), take a large plastic or glass petri dish and line it with paper towel. Dampen the paper towel with water or PBS. Break off the ends from four wooden coffee stirrers if necessary so that they fit in the petri dish and bind them together in pairs with tape. Then place the wood sticks in the petri dish like train tracks. Balance the slides carefully on the wooden sticks, add the antibodies, and then cover with the lid and incubate for the specified amount of time.
If suitable IgG or isotype control antibody is not available, then sections incubated in the absence of any primary antibody can be used as the nonspecific binding control, but this is less than ideal.
If necessary the slides can be placed on a warm heating block for 5–10 min to help excess liquid evaporate.
Fig. 1.
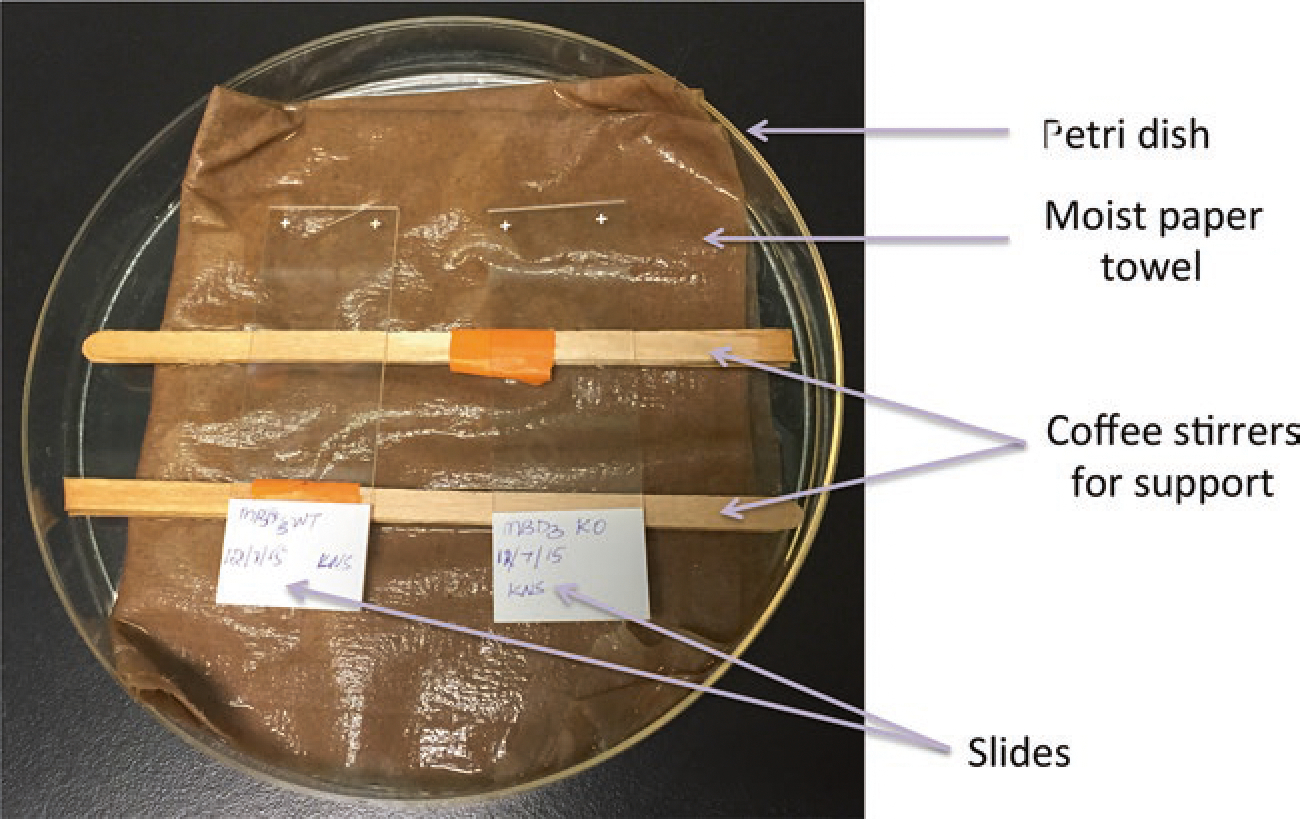
The figure shows the setup of a moist chamber (lid not shown) for immunostaining tissue sections
Acknowledgment
This work was supported by NIH grant EY13175 (AMM) and grants from Sapienza Università di Roma (MLM). Part of the content of this work is the object of US patent application No. 14/506,383.
References
- 1.Lai Y, Gallo RL (2009) AMPed Up immunity: how antimicrobial peptides have multiple roles in immune defense. Trends Immunol 30:131–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolar SS, McDermott AM (2011) Role of host-defence peptides in eye diseases. Cell Mol Life Sci 68:2201–2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong JH, Ye XJ, Hg TB (2013) Cathelicidins: peptides with antimicrobial, immunomodulatory, anti-inflammatory, angiogenic, anticancer and procancer activities. Curr Protein Pept Sci 14:504–514 [DOI] [PubMed] [Google Scholar]
- 4.Jarczak J, Kosciuczuk EM, Lisowski P, Strazlkowska N, Jozwik A, Horbanczuk J et al. (2013) Defensins: natural components of human innate immunity. Hum Immunol 74:1069–1079 [DOI] [PubMed] [Google Scholar]
- 5.Fleiszig SM, Evans DJ (2010) Pathogenesis of contact-lens associated microbial keratitis. Optom Vis Sci 87:225–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma DP, Sharma S, Wilkins MR (2011) Microbial keratitis after corneal laser surgery. Future Microbiol 6:819–831 [DOI] [PubMed] [Google Scholar]
- 7.Stapleton F, Carnt N (2012) Contact lens-related microbial keratitis: how have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye 26:2185–2193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taneja M, Ashar JN, Mathur A, Nalamada S, Garg P (2013) Microbial keratitis following vegetative matter injury. Int Ophthalmol 33:117–123 [DOI] [PubMed] [Google Scholar]
- 9.Moser C, Weiner DJ, Lysenko E, Bals R, Weiser JN, Wilson JM (2002) beta-Defensin 1 contributes to pulmonary innate immunity in mice. Infect Immun 70:3068–3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morrison G, Kilanowski F, Davidson D, Dorin J (2002) Characterization of the mouse beta defensin 1, Defb1, mutant mouse model. Infect Immun 70:3053–3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tomalka J, Azodi E, Narra HP, Patel K, O’Neill S, Cardwell C et al. (2015) β-Defensin 1 plays a role in acute mucosal defense against Candida albicans. J Immunol 194:1788–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Augustin DK, Heimer SR, Tam C, Li WY, Le Due JM, Evans DJ, Fleiszig SM (2011) Role of defensins in corneal epithelial barrier function against Pseudomonas aeruginosa traversal. Infect Immun 79:595–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolar SS, Baidouri H, Hanlon S, McDermott AM (2013) Protective role of murine β-defensin 3 and 4 and cathelin-related antimicrobial peptide in Fusarium solani keratitis. Infect Immun 81:2669–2677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nizet V, Ohtake T, Lauth X, Trowbridge J, Rudisill J, Dorschner RA et al. (2001) Innate antimicrobial peptide protects the skin from invasive bacterial infection. Nature 414:454–457 [DOI] [PubMed] [Google Scholar]
- 15.Huang LC, Reins RY, Gallo RL, McDermott AM (2007) Cathelicidin-deficient (Cnlp−/−) mice show increased susceptibility to Pseudomonas aeruginosa keratitis. Invest Ophthalmol Vis Sci 48:4498–4508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu FS, Cornicelli MD, Kovach MA, Newstead MW, Zeng X, Kumar A et al. (2010) Flagellin stimulates protective lung mucosal immunity: role of cathelicidin-related antimicrobial peptide. J Immunol 185:1142–1149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kulkarni MM, Barbi J, McMaster WR, Gallo RL, Satoskar AR, McGwire BS (2011) Mammalian antimicrobial peptide influences control of cutaneous Leishmania infection. Cell Microbiol 13:913–923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kovach MA, Ballinger MN, Newstead MW, Zeng X, Bhan U, Yu FS et al. (2012) Cathelicidin-related antimicrobial peptide is required for effective lung mucosal immunity in Gram-negative bacterial pneumonia. J Immunol 189:304–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dorin JR (2015) Novel phenotype of mouse spermatozoa following deletion of nine β-defensin genes. Asian J Androl 17:716–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu M, McClellan SA, Barrett RP, Hazlett LD (2009) Beta-defensin-2 promotes resistance against infection with P. aeruginosa. J Immunol 182:1609–1616 [DOI] [PubMed] [Google Scholar]
- 21.Wu M, McClellan SA, Barrett RP, Zhang Y, Hazlett LD (2009) Beta-defensins 2 and 3 together promote resistance to Pseudomonas aeruginosa keratitis. J Immunol 183:8054–8060 [DOI] [PubMed] [Google Scholar]
- 22.Williams RN, Paterson CA, Eakins KE et al. (1982) Quantification of ocular inflammation: evaluation of polymorphonuclear leucocyte infiltration by measuring myeloperoxidase activity. Curr Eye Res 2:465–470 [DOI] [PubMed] [Google Scholar]
- 23.Cole N, Krockenberger M, Stapleton F, Khan S, Hume E, Husband AJ, Willcox M (2003) Experimental Pseudomonas aeruginosa keratitis in interleukin-10 gene knockout mice. Infect Immun 7:1328–1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(DeltaDelta C(T)) method. Methods 25:402–408 [DOI] [PubMed] [Google Scholar]
- 25.Gao N, Kumar A, Guo H, Wu X, Wheater M, Yu FS (2011) Topical flagellin-mediated innate defense against Candida albicans keratitis. Invest Ophthalmol Vis Sci 52:3074–3082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eckhart L, Bach J, Ban J, Tschachler E (2000) Melanin binds reversibly to thermostable DNA polymerase and inhibits its activity. Biochem Biophys Res Commun 271:726–730 [DOI] [PubMed] [Google Scholar]


