Abstract
The 16-kDa cytosolic antigen of M. tuberculosis was purified to homogeneity by molecular sieving chromatography, and the diagnostic potential of the antigen was evaluated in various categories of patients by enzyme-linked immunosorbent assay (ELISA). The immunoglobulin G (IgG), IgA, and IgM antibody levels to 16-kDa antigen were estimated in the two polar groups, namely, smear- and culture-positive pulmonary tuberculosis (S+C+) patients and healthy subjects (HS). Sensitivities of 62, 52 and 11% with specificities of 100, 97, and 95% were obtained for the three isotypes, respectively. The total number of positives by a combination of the three isotypes was analyzed in the polar groups, and the sensitivity improved to 83% with a specificity of 93%. Even when a combination of IgG and IgA alone was considered, the sensitivity was 82% with a specificity of 97%. Polyethylene glycol precipitation of the circulating immune complex (CIC) in sera was carried out. The CIC-bound antibodies to 16-kDa antigen were assessed by ELISA in the S+C+, S−C+, and S−C− categories of patients. Measuring the IgG-IgA-IgM combination positivities of the CIC-bound antibodies gave sensitivities of 97.5, 100, and 45.3%, respectively. The specificity of the assay with these combinations was maintained at 95.4%.
Tuberculosis is a major health problem throughout the world, resulting in about 3 million deaths annually (17). This contagious disease, though preventable, has had an increased incidence in recent years, mainly due to its association with human immunodeficiency virus disease (30) and also due to the occurrence of multidrug resistance (36). In spite of the availability of an adequate treatment regimen, attempts to restrict and eradicate the disease have failed.
The alarming increase in morbidity and mortality due to tuberculosis indicates the need to strengthen control measures. Control of the disease depends largely on early detection and treatment of active cases. There is promise in serodiagnostic tests like enzyme-linked immunosorbent assay (ELISA) because of their ease of performance and cost-effectiveness. Serodiagnosis was attempted in earlier days, using crude and semipurified antigens, and was found to give different ranges of sensitivity and specificity (10, 14). The results underline the importance of identifying species-specific antigens and using them for diagnosis.
Daniel and Anderson (12) were the first to report on the species-specific antigen 5 of Mycobacterium tuberculosis, which was later proved to be the same as the 38-kDa antigen. As antigen 5, it has shown high specificity in all studies conducted in different parts of the world (88 to 98%), while the sensitivity varied from 49 to 89% (2, 3, 13, 15, 23). Other than this and a limited number of other antigens, species specificity (at least M. tuberculosis complex specificity) is quite rare among the M. tuberculosis antigens.
In a preliminary study of immunoblots with patients' sera, we observed the specific recognition of a 16- or 17-kDa band by pooled tuberculous sera, which encouraged us to attempt the isolation of this protein. In the present study, the 16-kDa antigen has been purified from the cytosol fraction of M. tuberculosis H37Rv and evaluated for its diagnostic potential in the sera of various categories of tuberculosis patients by ELISA. Anti-16-kDa antibodies bound to the circulating immune complex (CIC) in the same groups of patients were also measured.
MATERIALS AND METHODS
Study population.
This study has complied with the relevant governmental guidelines and was approved by our institutional Scientific Advisory Committee and Ethical Committee. Informed consent was obtained from the study population before blood was drawn.
Sera were obtained from the various categories of patients and healthy individuals, as described below. A total of 555 sera were used in the study, 345 of which were obtained from pulmonary tuberculosis patients, which could be subdivided into the following groups. (i) Smear- and culture-positive cases, pretreatment (S+C+) (n = 175). Smear and culture examination were done according to standard procedures (1). Two spot and one overnight sputum specimens were collected from each patient, and direct smears stained for acid-fast bacilli were observed under a fluorescent microscope. The sputa were also decontaminated, concentrated, and inoculated on Lowenstein-Jenson medium and incubated for up to 8 weeks at 37°C to check positivity and negativity. (ii) Smear-negative, culture-positive cases, pretreatment (S−C+) (n = 41). (iii) Smear- and culture-negative, clinically and radiologically diagnosed cases (S−C− [X-ray]) (n = 50). The X rays were read by two independent readers (and by one more reader in case of disagreement between the two) and classified as possible or probable tuberculosis. This group formed part of a sample survey for prevalence of the disease in the community (16). (iv) Smear- and culture-negative cases, treated and remaining quiescent for at least 5 years (S−C− [treated]) (n = 79).
A total of 210 sera were obtained from controls, as follows. (i) Patients with nontuberculous lung diseases (non-TB) (n = 60). This category includes conditions that present with X-ray shadows, such as asthma, allergy, etc.; lung carcinoma; other infectious conditions likely to have cross-reactive antigens, such as nocardiasis; and patients with lung pathology in whom mycobacteria other than M. tuberculosis have been isolated. (ii) Healthy subjects from the laboratory and voluntary donors from a blood bank (HS) (n = 150).
The sera were aliquoted and stored at −70°C till the time of use.
Purification of 16-kDa antigen.
M. tuberculosis H37Rv sonicate and cytosol antigens were prepared as described earlier (32).
The cytosol fraction of the sonicate antigen of M. tuberculosis H37Rv was passed through gel filtration chromatography using Ultrogel ACA34 matrix (Pharmacia, Uppsala, Sweden). Initially, 150 mg of the cytosol fraction was loaded on the gel filtration column (75 by 5 cm) along with bromophenol blue and blue dextran to serve as indicators for the mobility of samples. The elution was carried out with 20 mM Tris-HCl buffer along with 1 mM EDTA, 1 mM dithiothreitol, and 0.5 M NaCl at pH 8.2. The cytosol antigens separated by Ultrogel ACA34 were collected as 1-ml fractions at a rate of 0.75 ml per min. A total of 350 fractions were collected.
The quantification of the proteins was done with a bicinchoninic acid protein assay kit (Pierce, Rockford, Ill.).
Analytical SDS-PAGE.
The cytosol and fractions were analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) by the method of Laemmli (21), using a 12.5% resolving gel. After electrophoresis, the gels were stained with 0.2% Coomassie brilliant blue stain.
ELISA.
ELISA was carried out to estimate the immunoglobulin G (IgG), IgA, and IgM antibody levels against the 16-kDa antigen of M. tuberculosis H37Rv as described previously (34). The coating concentration of antigen was 0.2 μg/ml. The sera were tested at 1/3,200.
CIC precipitation.
The method of CIC precipitation with polyethylene glycol (PEG) has been described elsewhere (29). Reconstituted PEG precipitates (1/100 dilution) were tested for the presence of anti-16-kDa antibodies of the classes IgG, IgA, and IgM by ELISA.
In experiment 1, four categories of sera, namely, S+C+ (n = 20), S−C+(n = 26), S−C− (n = 37), and HS (n = 39) were randomly selected and subjected to CIC precipitation with 3.5% PEG. The CIC-bound 16-kDa antibodies were measured, and the number of positives in each category was calculated as before (greater than the mean plus 2 standard deviations [SD] of HS).
The experiment was repeated (experiment 2) with another set of sera (S+C+ [n = 20]. S−C+ [n = 26], S−C− [n = 27], and HS [n = 48]) to test reproducibility.
The results of experiments 1 and 2 were merged and analyzed.
RESULTS
Purification of 16-kDa antigen.
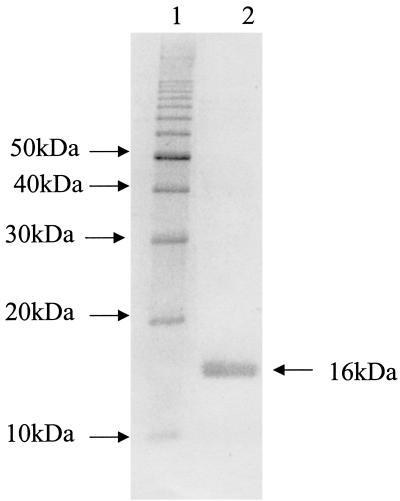
The cytosol antigens were separated on a gel filtration column. Every fifth fraction collected was analyzed by SDS-12.5% PAGE after being stained with Coomassie brilliant blue stain. The SDS-PAGE analysis of the purified protein is shown in Fig. 1.
FIG. 1.
Purified 16-kDa protein on SDS-PAGE. Lane 1, molecular mass marker; lane 2, purified 16-kDa protein.
Characterization of 16-kDa antigen.
The protein purified by gel filtration chromatography was subjected to reverse-phase high-performance liquid chromatography (HPLC) in order to ascertain the homogeneity of the protein. Ten micrograms of protein was loaded on a C18 column. The run was carried out with an isocratic flow of 30% acetonitrile with a 0.2-ml/min flow rate. The protein was eluted at retention times (RT) of 9 and 13 min. The individual fractions obtained at the two time points were analyzed on SDS-PAGE. The peak obtained at an RT of 9 min showed a protein in the 16-kDa region, while the peak at 13 min was found to contain a band in the 16-kDa region as well as a band in the 32-kDa region (data not shown).
The circular dichroism (CD) spectrum for the purified protein was analyzed and showed a maximum peak at 214 nm with a molar ellipticity of −65,779.9° cm2 · dmol−1, characteristic of β-sheet structure (data not shown).
The identity of the purified 16-kDa antigen was established by an immunoblot with monoclonal antibodies (MAbs) IT-1 and IT-4 from the World Health Organization bank and a polyclonal antibody against H37Rv as a positive control. A positive reaction with the established MAbs suggests identity of this protein with the already reported 16-kDa antigen (data not shown).
Serum antibody levels. (i) Polar groups.
The serum antibodies in the two polar groups, namely, the S+C+ and the HS groups, were measured. The mean optical densities (ODs) for IgG, IgA, and IgM obtained for the S+C+ group were 0.338, 0.367, and 0.453, respectively. In the case of the HS group, the mean ODs were observed to be 0.187, 0.162, and 0.373, respectively, which were significantly less (p = 0.0001) than those of the tuberculous patients.
Using a cutoff of greater than the mean plus 2 SD of HS, the sensitivities of the assay in S+C+ cases were 62.28, 52, and 10.85% for the three isotypes IgG, IgA, and IgM, respectively. The number and percentage of positives in the two polar groups are given in Table 1. The maximum number of positives was seen with IgG antibody. However, when individual results were scrutinized, it was observed that some sera negative for IgG were positive for IgA and/or IgM. By combining the results for IgG and IgA, the sensitivity of the assay was increased to 82.28%, while the specificity remained at 96.6%. When the results for IgM were also combined, the sensitivity was 82.85% and the specificity decreased to 93.3%.
TABLE 1.
ELISA positivity in polar groupsa
| Isotype | S+C+ (n = 175)
|
HS (n = 150)
|
||
|---|---|---|---|---|
| No. positive | % Sensitivity | No. positive | % Specificity | |
| IgG | 109 | 62 | 0 | 100 |
| IgA | 91 | 52 | 4 | 97 |
| IgM | 19 | 11 | 7 | 95 |
| IgG + IgA | 144 | 82 | 4 | 97 |
| IgG + IgA + IgM | 145 | 83 | 10 | 93 |
Positivity is defined as greater than the mean plus 2 SD of HS OD.
(ii) Other groups.
In the S−C+ cases, positivities of 39% with both IgG and IgA and 9.75% with IgM were obtained. In the S−C− (X-ray-positive) cases, the antigen identified 58% as positive for IgG, 38% positive for IgA, and none positive for IgM.
For the S−C− (treated) cases, positivities of 20.25% (IgG), 25.31% (IgA), and 1.26% (IgM) were obtained. Among the non-TB lung disease cases, the percentages positive for 16-kDa antigen were 40, 10, and 1.66% for the three isotypes. The percentages positive in all these categories are shown in Table 2.
TABLE 2.
ELISA positivity in other categories
| CATEGORY | IgG
|
IgA
|
IgM
|
|||
|---|---|---|---|---|---|---|
| No. positive | % positive | No. positive | % positive | No. positive | % positive | |
| S−C− (X ray) (n = 50) | 29 | 58 | 19 | 38 | 0 | 0 |
| S−C+ (n = 41) | 16 | 39 | 16 | 39 | 4 | 10 |
| S−C− (treated) (n = 79) | 16 | 20 | 20 | 25 | 1 | 1 |
| Non-TB lung diseases (n = 60) | 24 | 40 | 6 | 10 | 1 | 2 |
With a combination of IgG, IgA, and IgM isotypes, the sensitivity increased to 74% in S−C− (X-ray) cases, increased to 63.4% in S−C+ cases, and remained similar (43%) in non-TB lung disease cases.
CIC-bound antibody to 16-kDa antigen.
The results of experiments 1 and 2 were merged and are summarized in Table 3.
TABLE 3.
Antibody levels in CIC
| Isotype | No. (%) positive
|
|||
|---|---|---|---|---|
| S+C+ (n = 40) | S−C+ (n = 52) | S−C− (n = 64) | HS (n = 87) | |
| IgG | 35 (87.5) | 42 (80.7) | 21 (32.8) | 1 (1.0) |
| IgA | 39 (97.5) | 52 (100) | 13 (20.3) | 2 (2.2) |
| IgM | 28 (70) | 22 (42.3) | 10 (15.6) | 1 (1.0) |
| IgG + IgA | 39 (97.5) | 52 (100) | 25 (39) | 3 (3.4) |
| IgG + IgA + IgM | 39 (97.5) | 52 (100) | 29 (45.3) | 4 (4.5) |
Among the S+C+ cases, 35 of 40 were positive for CIC IgG. In the S−C+ group, 42 of 52 were positive, and in the S−C− group, 21 of 64 were positive. Positivity for IgA antibodies, as well as IgM antibodies, was also seen, as shown in Table 3. One out of 87 HS CICs was positive for IgG (99% specificity). HS CICs were also positive for IgA (two) and IgM (one). As seen in Table 3, 97.5, 100, and 45% positivities were achieved for the S+C+, S−C+, and S−C− groups for detection of all three of the CIC-bound immunoglobulins. After combination of the results, the specificity of the test was 95.4% (83 of 87).
Out of the 60 sera from patients with non-TB lung diseases, 13 which were false positive for anti-16-kDa serum IgG and 7 which were negative were tested for CIC IgG. All serum positives but one proved to be negative for CIC-bound antibodies (results not shown).
DISCUSSION
Research for identification of a suitable antigen for serodiagnosis of tuberculosis has come a long way, and yet there is lot more to be explored. In this study, a cytosol protein of 16-kDa molecular mass was isolated from the virulent strain M. tuberculosis H37Rv and evaluated for its diagnostic value.
The 16-kDa protein belongs to the alpha crystallin superfamily of small heat shock proteins and has been variously referred to as sHsp16, Hsp.16.3, Acr, and MPT63. It is similar to the major membrane protein (22) and Nox16 (18) referred to previously.
The antigen described in this study, isolated from the cytosol fraction, has been assigned a mass of 16 kDa based on its movement in SDS-PAGE. Further evidence for confirmation of the identity of this protein with Hsp. 16.3, reported earlier, comes from the study of the circular dichroism of this native protein. Our purified protein has been assigned a predominantly β-sheet structure with a peak in the 210- to 215-nm region, which is in agreement with the report of Berengian et al. (4). Further, a positive reaction of this protein with MAbs IT-1 and IT-4 from the World Health Organization bank suggests the similarity of this 16-kDa protein to the reported 16-kDa Hsp antigen.
The antigen seems to exist in two different molecular forms, as two peaks at different RT were obtained from the purified antigen preparation when it was analyzed by HPLC. However, when the two peaks were separately analyzed by SDS-PAGE, both peaks contained only the 16-kDa protein, which shows that the protein exists in different oligomeric forms. Hsp.16.3 has been found to occur as oligomers consisting of a trimer of trimers (a nine-subunit complex) (11, 37).
The species specificity of this antigen has been extensively studied by various investigators. The mpt63 gene is found only in species of the M. tuberculosis complex, as shown by DNA hybridization studies (24). Antibodies against MPT63 do not cross-react with common environmental mycobacteria (24). Species-specific B-cell epitopes on this antigen have been demonstrated (19), and it has also been shown that its TB68 MAb-reacting epitope, as well as the T-cell clones, are specific for the M. tuberculosis complex (27). In a preliminary study of immunoblots with patients' sera, we have observed the specific recognition of a 16- or 17-kDa band by pooled tuberculous sera (n = 65) and not by pooled normal sera (n = 65), which also suggests the specificity of 16 kDa.
Effective serodiagnosis using 16-kDa antigen has been reported by previous investigators, though only a limited number of studies have been done with this antigen (22, 35). Other groups of workers have evaluated a 14-kDa antigen (which was later renamed Hsp16) and its epitopes (6, 20).
In all of the studies reported so far, only IgG has been measured, and the sensitivities ranged from 70 to 75%. In our study, a sensitivity of 62% was obtained in S+C+ cases by measuring IgG response alone, whereas when the IgA and IgM isotype response were combined, the sensitivity increased to 83%. Our sensitivity results show an improvement over those reported earlier, and the specificity (93%) is also comparable to those reported with other preparations of 16-kDa antigen.
In smear-negative cases, the sensitivity reported with this antigen was less. In the study conducted by Bothamley et al. (6), 46 and 11% sensitivities were obtained with 16-kDa whole antigen and the TB68 epitope, respectively. In another study, the 16-kDa antigen identified 54% of cases (20). In our study, using this antigen in the diagnosis of S−C+ patients, there was 39% positivity for the IgG and IgA isotypes and 10% positivity for the IgM isotype. By combining IgG, IgA, and IgM isotypes, the sensitivity was increased to 63.4%. A similarly high sensitivity of 74% was obtained for S−C− (X-ray) cases. Here again, an improvement in test outcome by combining three isotypes is demonstrated compared to IgG alone.
However, following a similar approach, the false positivity was very high (43%) in non-TB lung diseases. Cutoff limits of the mean plus 3 SD were used, and the results were recalculated. This did not eliminate the nonspecificity in this group, as 19 of 60 cases (31.7%) were still positive
Since the antigen is species specific, the false positivity may be attributed to nonspecific hyperglobulinemia, common in bronchial diseases (7), or other causes. Irrespective of the reason, this is a complicating factor in diagnosis and is likely to compromise the specificity of the assay when applied in clinical situations. Therefore, the value of the 16-kDa antigen for diagnosis based on serum antibodies is limited.
A large number of studies have reported the presence of CIC in tuberculous patients (8, 9, 25). Many of these studies measured the mycobacterial antigens (5, 25, 31) only after breaking the complex and concentrating them. Demonstration of antimycobacterial antibodies in CIC has posed fewer problems (5, 25, 31).
In one of our previous studies (29), we demonstrated that PEG-precipitable CICs are present in smear-positive, as well as smear-negative, patients' sera. In fact, the quantity of CIC (as judged by the OD at 280 nm) was significantly higher in smear-negative cases. Anti-mycobacterial-antibody measurement in CICs was more discriminatory between the groups than serum antibody measurement.
In the present study, we have measured CIC-bound antibodies of the classes IgG, IgA, and IgM against the 16-kDa antigen. While the majority of the CIC was IgG positive, IgA and IgM could also be measured. It was observed that many tuberculous sera, which were negative for free antibody, were positive for complexed antibody. Detection of anti-16-kDa antibodies in CIC greatly improved the outcome of the test, showing 97.5% sensitivity in the S+C+ group. Among S−C+ cases, too, 52 of 52 were positive for CIC antibodies, and among S−C− radiologically diagnosed cases, 45% were positive for CIC antibodies. Thus, these results reconfirm our previous observation of 100% sensitivity in culture-proven cases (29).
Out of the 60 sera from non-TB lung disease patients, 13 which were false positive for anti-16-kDa serum IgG and 7 which were negative were tested for CIC IgG. All serum positives but one proved to be negative for CIC-bound antibodies. Thus, the interfering serum component contributing to nonspecific high OD was removed. This is not a chance phenomenon, since we have also reported similar results for a 38-kDa antigen in the same study population (34).
The absence of antibody response to any particular antigen is generally interpreted as being due to immunosuppression or the absence of recognition due to host genetic factors. As early as 1980 (9), an inverse relationship between serum C1q binding and serum anti-Mycobacterium bovis BCG antibody was observed, suggesting that some antibodies may be bound to the complexes. Here, we have demonstrated that the absence of anti-16-kDa antibody in the free form could be due to its sequestration in the bound form.
Earlier studies by other authors have reported the detection of CIC antibodies against glycolipid antigens (phosphatidyl inositomannoside and diacyl trehalose), as well as protein antigens (antigen 5) (26, 28, 33). The diagnostic value of anti-16-kDa CIC antibodies has not been reported so far. Our study has demonstrated a high sensitivity of detection of S+ cases, as well as S− cases, where diagnosis is most needed. The CIC antibody-based diagnosis, owing to its high sensitivity and specificity, can be useful for (i) individual patient-based diagnosis; (ii) detection of cases under Tuberculosis Control Program conditions, compared to sputum smears; and (iii) detection of cases while screening populations, compared to X rays.
The method involves overnight incubation, centrifugation, etc. Therefore, it cannot be viewed as a rapid test to be performed under field conditions. However, a large number of samples can be brought to a central laboratory and processed together. As for the time involved in incubation, the test is comparable to the sputum smear, since at least three sputum collections from the same patient (two spot and one overnight) are to be tested under Tuberculosis Control Program conditions. Even then, false negativity can be seen in the smear test, which is overcome by CIC ELISA. (In the present study, sputum smears diagnosed 175 out of 216 [81%] culture-positive cases, while CIC ELISA identified 91 of 92 (98.9%) culture-positive cases.) Although three isotypes have to be measured, they can be combined in a single test, since anti-human IgG-IgA-IgM conjugates are commercially available. This test will be especially useful in cases where sputum positivity is rare, such as childhood tuberculosis, extrapulmonary tuberculosis, and minimal disease.
Acknowledgments
Financial support provided by the Indo-U.S. Vaccine Action Programme, through the Department of Biotechnology, Government of India, is gratefully acknowledged.
K. R. Uma Devi is the recipient of a Junior Research Fellowship from the Department of Biotechnology, Government of India. B. Ramalingam is the recipient of a Senior Research Fellowship from the Council of Scientific and Industrial Research, New Delhi, India.
We are thankful to K. N. Sulochana, Department of Biochemistry, Vision Research Foundation, Chennai, India, and R. Jayakumar, Department of Bio-Organic Chemistry, Central Leather Research Institute, Chennai, India, for providing the facilities for HPLC and CD, respectively.
REFERENCES
- 1.Allen, B., and F. J. Baker. 1968. Treatment of specimens, p. 9-16. In F. J. Baker (ed.), Mycobacteria—isolation, identification and sensitivity testing. Butterworths & Co Ltd., London, United Kingdom.
- 2.Balestrino, E. A, T. M. Daniel, M. D. S. De Latini, O. A. Latini, Y. Ma, and B. Scocozza. 1984. Serodiagnosis of pulmonary tuberculosis in Argentina by enzyme linked immunosorbent assay (ELISA) of IgG antibody to Mycobacterium tuberculosis antigen 5 and tuberculin purified protein derivative. Bull. W. H. O. 62:755-761. [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin, R. G., and T. M. Daniel. 1982. Serodiagnosis of tuberculosis using the enzyme-linked immunosorbent assay (ELISA) of antibody to Mycobacterium tuberculosis antigen 5. Am. Rev. Respir. Dis. 126:1013-1016. [DOI] [PubMed] [Google Scholar]
- 4.Berengian, A. R., M. Parfenova, and H. S. Mchaourab. 1999. Site-directed spin labeling study of subunit interactions in the α-crystallin domain of small heat-shock proteins—comparison of the oligomer symmetry in α-crystallin, HSP 27 and HSP 16.3. J. Biol. Chem. 274:6305-6314. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharya, A., S. N. Ranadive, M. Kale, and S. Bhattacharya. 1986. Antibody-based enzyme linked immunsorbent assay for determination of immune complexes in clinical tuberculosis. Am. Rev. Respir. Dis. 134:205-209. [DOI] [PubMed] [Google Scholar]
- 6.Bothamley, G. H., J. S. Beck, R. C. Potts, J. M. Grange, T. Kardjito, and J. Ivanyi. 1992. Specificity of antibodies and tuberculin response after occupational exposure to tuberculosis. J. Infect. Dis. 166:182-186. [DOI] [PubMed] [Google Scholar]
- 7.Bothamley, G. H., and R. M. Rudd. 1994. Clinical evaluation of a serological assay using a monoclonal antibody (TB72) to the 38kDa antigen of Mycobacterium tuberculosis. Eur. Respir. J. 7:240-246. [DOI] [PubMed] [Google Scholar]
- 8.Brostoff, J., L. Lenzini, and P. Rottoli. 1981. Immune complexes in the spectrum of tuberculosis. Tubercle 62:169-173. [DOI] [PubMed] [Google Scholar]
- 9.Carr, R. I., A. K. Chakraborty, and M. J. Brundo. 1980. Immune complexes and antibodies to BCG in sera from patients with mycobacterial infections. Clin. Exp. Immunol. 39:562-569. [PMC free article] [PubMed] [Google Scholar]
- 10.Chan, E. D., L. Heifets, and M. D. Iseman. 2000. Immunologic diagnosis of tuberculosis: a review. Tuberc. Lung. Dis. 80:131-140. [DOI] [PubMed] [Google Scholar]
- 11.Chang, Z., T. P. Primm, J. Jakana, I. H. Lee, I. Serysheval, W. Chiu, H. F. Gilbert, and F. A. Quiocho. 1996. Mycobacterium tuberculosis 16kDa antigen (Hsp16.3) functions as an oligomeric structure in vitro to suppress thermal aggregation. J. Biol. Chem. 271:7218-7223. [PubMed] [Google Scholar]
- 12.Daniel, T. M., and P. A. Anderson. 1978. The isolation by immunosorbent affinity chromatography and physicochemical characterization of Mycobacterium tuberculosis antigen 5. Am. Rev. Respir. Dis. 117:533-539. [DOI] [PubMed] [Google Scholar]
- 13.Daniel, T. M., S. M. Debanne, and F. van der Kuyp. 1985. Enzyme-linked immunosorbent assay using Mycobacterium tuberculosis antigen 5 and PPD for the diagnosis of tuberculosis. Chest 88:388-392. [DOI] [PubMed] [Google Scholar]
- 14.Daniel, T. M., and S. Debanne. 1987. The serodiagnosis of tuberculosis and other mycobacterial diseases by enzyme-linked immunosorbent assay. Am. Rev. Respir. Dis. 135:1137-1151. [DOI] [PubMed] [Google Scholar]
- 15.Daniel, T. M., G. L. De Murillo, J. A. Sawyer, A. McLean Griffin, E. Pinto, S. M. Debanne, P. Espinosa, and E. Cespedes. 1986. Field evaluation of enzyme-linked immunosorbent assay for the serodiagnosis of tuberculosis. Am. Rev. Respir. Dis. 134:662-665. [DOI] [PubMed] [Google Scholar]
- 16.Datta, M., P. G. Gopi, B. N. Appegowda, K. R. Bhima Rao, and B. N. Gopalan. 2000. Tuberculosis in North Arcot district of Tamil Nadu—a sample survey. Indian J. Tuberc. 47:147-154. [Google Scholar]
- 17.Enarson, D., and J. Murray. 1996. Global epidemiology of tuberculosis, p. 57-75. In W. N. Rom and S. Garay (ed.), Tuberculosis. Little, Brown and Co., Boston, Mass.8808270
- 18.Garbe, T. R., N. S. Hibler, and V. Deretic. 1999. Response to reactive nitrogen intermediates in Mycobacterium tuberculosis: induction of the 16-kilodaltonα-crystallin homolog by exposure to nitric oxide donors. Infect. Immun. 67:460-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ivanyi, J., G. H. Bothamley, and P. S. Jackett. 1988. Immunodiagnostic assays for tuberculosis and leprosy. Br. Med. Bull. 44:635-649. [DOI] [PubMed] [Google Scholar]
- 20.Jackett, P. S., G. H. Bothamley, H. V. Batra, A. Mistry, B. D. Young, and J. Ivanyi. 1988. Specificity of antibodies to immunodominant mycobacterial antigens in pulmonary tuberculosis. J. Clin. Microbiol. 26:2313-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 22.Lee, B. Y., S. A. Hefta, and P. J. Brennan. 1992. Characterization of the major membrane protein of virulent Mycobacterium tuberculosis. Infect. Immun. 60:2066-2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma, Y., Y. M. Wang, and T. M. Daniel. 1986. Enzyme-linked immunosorbent assay using Mycobacterium tuberculosis antigen 5 for the serodiagnosis of pulmonary tuberculosis in China. Am. Rev. Respir. Dis. 134:1273-1275. [DOI] [PubMed] [Google Scholar]
- 24.Manca, C., K. Lyashchenkoo, H. G. Wiker, D. Usai, R. Colangeli, and M. Gennaro. 1997. Molecular cloning, purification and serological characterization of MPT63, a novel antigen secreted by Mycobacterium tuberculosis. Infect. Immun. 65:16-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.May, J. J., J. Katilus, P. M. Henson, and R. B. Dreisin. 1983. The purification and identification of circulating immune complexes in tuberculosis. Am. Rev. Respir. Dis. 128:920-925. [DOI] [PubMed] [Google Scholar]
- 26.Mehta, P. K., and G. K. Khuller. 1989. Comparative evaluation of the diagnostic significance of circulating immune complexes and antibodies to phosphatidylinositol mannosides in pulmonary tuberculosis by enzyme-linked immunosorbent assay. Med. Microbiol. Immunol. 178:229-233. [DOI] [PubMed] [Google Scholar]
- 27.Oftung, F., E. Borka, and A. S. Mustafa. 1998. Mycobacterium tuberculosis reactive T cell clones from naturally converted PPD-positive healthy subjects: recognition of the M. tuberculosis 16kDa antigen. FEMS Immunol. Med. Microbiol. 20:319-325. [DOI] [PubMed] [Google Scholar]
- 28.Radhakrishan, V. V., A. Mathai, and P. Sundaram. 1992. Diagnostic significance of circulating immune complexes in patients with pulmonary tuberculosis. J. Med. Microbiol. 36:128-131. [DOI] [PubMed] [Google Scholar]
- 29.Raja, A., P. R. Narayanan, R. Mathew, and R. Prabhakar. 1995. Characterization of mycobacterial antigens and antibodies in circulating immune complexes from pulmonary tuberculosis. J. Lab. Clin. Med. 125:581-587. [PubMed] [Google Scholar]
- 30.Raviglione, M. C., D. J. Snider, and A. Kochi. 1995. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA 273:220-226. [PubMed] [Google Scholar]
- 31.Samuel, A. M., M. D. Ashtekar, and R. D. Ganatra. 1984. Significance of circulating immune complexes in pulmonary tuberculosis. Clin. Exp. Immunol. 58:317-324. [PMC free article] [PubMed] [Google Scholar]
- 32.Senthil Kumar, K. S., A. Raja, K. R. Uma Devi, and R. S. Paranjape. 2000. Production and characterization of monoclonal antibodies to Mycobacterium tuberculosis. Indian J. Med. Res. 112:37-46. [PubMed] [Google Scholar]
- 33.Simonney, N., M. L. Molina, M. Molimard, E. Oksenhendler, and P. H. Lagrange. 1997. Circulating immune complexes in human tuberculosis sera: demonstration of specific antibodies against Mycobacterium tuberculosis glycolipid (DAT, PGTb1, LOS) antigens in isolated circulating immune complexes. Eur. J. Clin. Investig. 27:128-134. [DOI] [PubMed] [Google Scholar]
- 34.Uma Devi, K. R., B. Ramalingam, P. J. Brennan, P. R. Narayanan, and A. Raja. 2001. Specific and early detection of IgG, IgA and IgM antibodies to M. tuberculosis 38kDa antigen in pulmonary tuberculosis. Tuberculosis 81:249-253. [DOI] [PubMed] [Google Scholar]
- 35.Verbon, A., R. A. Hartskeerl, A. Schuitema, A. H. J. Kolk, D. B. Young, and R. Lathigra. 1992. The 14,000-molecular-weight antigen of Mycobacterium tuberculosis is related to the α-crystallin family of low-molecular-weight heat shock proteins. J. Bacteriol. 174:1352-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. 1998. Antituberculosis drug resistance worldwide. Wkly. Epidemiol. Rec. 73:249-256. [PubMed] [Google Scholar]
- 37.Yuan, Y., D. D. Crane, and C. E. Barry. 1996. Stationary-phase-associated protein expression in Mycobacterium tuberculosis: function of the mycobacterial α-crystallin homolog. J. Bacteriol. 178:4484-4492. [DOI] [PMC free article] [PubMed] [Google Scholar]