Abstract
Pneumonia and other lower respiratory tract diseases rank as the fourth leading cause of death worldwide. The objective of this study was to examine pneumonia hospitalization patterns, and trends in total pneumonia hospitalization stratified by age group, by type of hospitalization, and by age group in Australia, England, Wales. This study utilized 3 databases to obtain hospital admissions data: the National Hospital Morbidity Database for Australian hospital admissions data, the Hospital Episode Statistics database (HES) for England hospital admissions data, and the Patient Episode Database for Wales. Pneumonia hospitalization data were extracted utilizing J12 to J18 codes. From 2013 to 2020, there were 4,514,444 cases of pneumonia hospitalizations reported in Australia (646,515 [14.32%]), England (3,668,106 [81.25%]), and Wales (199,823 [4.43%]). The most common type of pneumonia hospitalization in Australia, England, and Wales was “pneumonia, organism unspecified,” accounting for 77.12%, 95.49%, and 95.75% of the total number of pneumonia hospitalizations in each country, respectively. The most common subtype of pneumonia hospitalization in Australia was “pneumonia, unspecified,” accounting for 72.98% of the total number of pneumonia hospitalizations in the country. The most common type of pneumonia hospitalization in England and Wales was “lobar pneumonia, unspecified,” accounting for 59.00% and 56.73% of the total number of pneumonia hospitalizations in each country, respectively. Most pneumonia hospitalizations in Australia, England, and Wales were non-same-day hospitalizations, accounting for 90.78%, 99.91%, and 99.95%, respectively. Pneumonia hospitalizations in Australia, England, and Wales were directly related to age. Males accounted for most pneumonia hospitalizations in Australia, England, and Wales. This study highlighted that hospitalization rate for pneumonia increased during the past decade in Australia, England, and Wales. The age and male gender were clearly contributing factors that affected pneumonia hospitalizations rate. Educational campaign aiming to increase public knowledge of pneumonia, its risk factors, and lifestyle modification should be prioritized to decrease pneumonia episodes.
Keywords: admission, Australia, England, hospitalization, pneumonia, Wales
1. Introduction
Pneumonia is classified by the World Health Organization (WHO) as an acute respiratory illness that impacts the oxygenation and lung parenchyma.[1] Pneumonia and other lower respiratory tract diseases rank as the fourth leading cause of death worldwide.[2] The incidence of pneumonia varies by demographics, health-care settings, and geographic region.[3] Nonetheless, audits conducted by the British Thoracic Society indicated that the 30-day mortality rate has been declining since 2009 in the United Kingdom (UK).[3]
Furthermore, an increase in pneumonia-related hospitalizations have been observed in the Netherlands, Denmark, and the United States and more hospital admissions and bed days are caused by pneumonia than by any other respiratory illness in the UK.[3–8] Besides, pneumonia causes 29,000 deaths annually in the UK, making it the third main cause of lung disease-related deaths, after lung cancer (the leading cause) and chronic obstructive pulmonary disease (COPD), which is the second leading cause.[9] In addition, the UK has the 21st age-standardized pneumonia mortality rate out of 99 countries. Besides, pneumonia has a significant effect on the health-care systems of the UK and Europe since it is linked to high hospital admission and length of stay rates.[9]
There is an absence of comprehensive data regarding the epidemiology of pneumonia in Australia.[10] Over 65,000 patients with this primary diagnosis visit Australian hospitals each year.[11] However, there is a dearth of information regarding the etiology of pneumonia from an Australian perspective, as well as the number of individuals who present to hospitals with the illness but are not later admitted.[11] Previous studies in Australia and the UK examined hospitalization profile due to respiratory diseases and demonstrated rising trends over the past 2 decades.[12–14] There hasn’t been much advancement in the pathogenesis, epidemiology, or treatment of pneumonia.[9] In fact, pneumonia ranked just 20 out of 25 infectious diseases in a study of UK funding for infectious disease research from 1997 to 2013, receiving little investment in relation to its disease burden.[9] Therefore, the objective of this study was to examine pneumonia hospitalization patterns, and trends in total pneumonia hospitalization stratified by age group, by type of hospitalization, and by age group in Australia, England, Wales. Examining hospitalization profile due to pneumonia across these 3 countries provide insights for targeted health interventions and health-care policy developments across countries with different health-care system and policies.
2. Methods
2.1. Data sources
2.1.1. Hospital admissions data
This study utilized 3 databases to obtain hospital admissions data: the National Hospital Morbidity Database (NHMD) for Australian hospital admissions data, the Hospital Episode Statistics database (HES) for England hospital admissions data, and the Patient Episode Database for Wales (PEDW). The NHMD, managed by the Australian Institute of Health and Welfare, contains patient episode-level records from private and public hospitals across Australia.[15,16] HES and PEDW record all hospital admissions at all National Health Service hospitals. The quality of the 3 databases is constantly evaluated to ensure their accuracy and reliability.[17–19] These databases were previously used to examine different health conditions across different age groups.[20–23]
2.1.2. Population data
Population data were collected from 2 official sources: the Australian Bureau of Statistics for the national Australian population[24,25] and the Office for National Statistics for the national England and Wales population.[26] Mid-year population data were collected between 2013 and 2020.
2.2. Study population
This study included all publicly available pneumonia hospitalization data from the 3 databases for the period between 2013 and 2020.[11,27,28] Pneumonia hospitalization data were extracted utilizing J12-J18 ICD-10 codes (“International Statistical Classification of Diseases and Related Health Problems 10th Revision”). The ICD codes used in this study were checked and verified by infectious diseases consultant.
2.3. Statistical analysis
The Statistical Package for Social Science Software (Chicago), version 29 was used to analyze the data for this study. Categorical variables were presented as frequencies and percentages. Hospitalisation rates were presented with 95% CIs. Pearson χ2 test of independence was used to examine the difference in admission rates between 2013 and 2020.
3. Results
3.1. Pneumonia hospitalization patterns
From 2013 to 2020, there were 4,514,444 cases of pneumonia hospitalizations reported in Australia (646,515 [14.32%]), England (3,668,106 [81.25%]), and Wales (199,823 [4.43%]). The most common type of pneumonia hospitalization in Australia, England, and Wales was “pneumonia, organism unspecified,” accounting for 77.12%, 95.49%, and 95.75% of the total number of pneumonia hospitalizations in each country, respectively. The most common subtype of pneumonia hospitalization in Australia was “pneumonia, unspecified,” accounting for 72.98% of the total number of pneumonia hospitalizations in the country. The most common type of pneumonia hospitalization in England and Wales was “lobar pneumonia, unspecified,” accounting for 59.00% and 56.73% of the total number of pneumonia hospitalizations in each country, respectively (Table 1).
Table 1.
Pneumonia hospitalization and percentage from total admissions per ICD code.
| ICD code | Description | Total number of pneumonia hospitalizations (% from total) | ||
|---|---|---|---|---|
| Australia | England | Wales | ||
| J12 | Viral pneumonia, not elsewhere classified | 65,263 (10.09) | 27,690 (0.75) | 995 (0.50) |
| J12.0 | Adenoviral pneumonia | 2689 (0.42) | 1405 (0.04) | 49 (0.02) |
| J12.1 | Respiratory syncytial virus pneumonia | 16,102 (2.49) | 8347 (0.23) | 235 (0.12) |
| J12.2 | Parainfluenza virus pneumonia | 4977 (0.77) | 3459 (0.09) | 160 (0.08) |
| J12.3 | Human metapneumovirus pneumonia | 9046 (1.40) | 3765 (0.10) | 178 (0.09) |
| J12.8 | Other viral pneumonia | 10,310 (1.59) | 3680 (0.10) | 95 (0.05) |
| J12.9 | Viral pneumonia, unspecified | 22,139 (3.42) | 7034 (0.19) | 278 (0.14) |
| J13 | Pneumonia due to Streptococcus pneumoniae | 16,036 (2.48) | 48,217 (1.31) | 1940 (0.97) |
| J14 | Pneumonia due to Haemophilus influenzae | 10,800 (1.67) | 15,255 (0.42) | 1253 (0.63) |
| J15 | Bacterial pneumonia, not elsewhere classified | 51,763 (8.01) | 69,114 (1.88) | 3997 (2.00) |
| J15.0 | Pneumonia due to Klebsiella pneumoniae | 1827 (0.28) | 10,494 (0.29) | 487 (0.24) |
| J15.1 | Pneumonia due to Pseudomonas | 8633 (1.34) | 18,866 (0.51) | 830 (0.42) |
| J15.2 | Pneumonia due to Staphylococcus | 4910 (0.76) | 7753 (0.21) | 652 (0.33) |
| J15.3 | Pneumonia due to Streptococcus, group B | 169 (0.03) | 661 (0.02) | 33 (0.02) |
| J15.4 | Pneumonia due to other streptococci | 1959 (0.30) | 8557 (0.23) | 536 (0.27) |
| J15.5 | Pneumonia due to Escherichia coli | 1009 (0.16) | 4979 (0.14) | 317 (0.16) |
| J15.6 | Pneumonia due to other Gram-negative bacteria | 1987 (0.31) | 4102 (0.11) | 271 (0.14) |
| J15.7 | Pneumonia due to Mycoplasma pneumoniae | 9676 (1.50) | 3916 (0.11) | 205 (0.10) |
| J15.8 | Other bacterial pneumonia | 2366 (0.37) | 3047 (0.08) | 253 (0.13) |
| J15.9 | Bacterial pneumonia, unspecified | 19,227 (2.97) | 6739 (0.18) | 413 (0.21) |
| J16 | Pneumonia due to other infectious organisms, not elsewhere classified | 1658 (0.26) | 1045 (0.03) | 78 (0.04) |
| J16.0 | Chlamydial pneumonia | 808 (0.12) | 102 (0.00) | 5 (0.00) |
| J16.8 | Pneumonia due to other specified infectious organisms | 850 (0.13) | 943 (0.03) | 73 (0.04) |
| J17 | Pneumonia in diseases classified elsewhere | 2408 (0.37) | 3986 (0.11) | 228 (0.11) |
| J17.0 | Pneumonia in bacterial diseases classified elsewhere | 408 (0.06) | 512 (0.01) | 55 (0.03) |
| J17.1 | Pneumonia in viral diseases classified elsewhere | 98 (0.02) | 282 (0.01) | 5 (0.00) |
| J17.2 | Pneumonia in mycoses | 798 (0.12) | 2086 (0.06) | 117 (0.06) |
| J17.3 | Pneumonia in parasitic diseases | 1005 (0.16) | 1060 (0.03) | 51 (0.03) |
| J17.8 | Pneumonia in other diseases classified elsewhere | 99 (0.02) | 46 (0.00) | 0 (0.00) |
| J18 | Pneumonia, organism unspecified | 498,587 (77.12) | 3,502,799 (95.49) | 191,332 (95.75) |
| J18.0 | Bronchopneumonia, unspecified | 16,618 (2.57) | 116,405 (3.17) | 7679 (3.84) |
| J18.1 | Lobar pneumonia, unspecified | 4471 (0.69) | 2,164,345 (59.00) | 113,367 (56.73) |
| J18.2 | Hypostatic pneumonia, unspecified | 349 (0.05) | 1269 (0.03) | 72 (0.04) |
| J18.8 | Other pneumonia, organism unspecified | 5294 (0.82) | 2710 (0.07) | 107 (0.05) |
| J18.9 | Pneumonia, unspecified | 471,855 (72.98) | 1,218,070 (33.21) | 70,107 (35.08) |
ICD = International Statistical Classification of Diseases.
3.2. Trends in total pneumonia hospitalization
During the study period, the total number of pneumonia hospitalizations in the 3 countries increased by 52.03%, from 489,855 in 2013 to 744,722 in 2020; raised by 22.43% in Australia (from 76,206 to 93,299), by 59.39% in England (from 389,333 to 620,541), and by 27.00% in Wales (from 24,316 to 30,882). Still, the total pneumonia hospitalization rates in Australia increased by 12.06% from 324.62 (95% CI 322.32–326.92) per 100,000 persons in 2013 to 363.75 (95% CI 361.42–366.08) per 100,000 persons in 2020, (trend test, P < .001). The total pneumonia hospitalization rates in England increased by 53.85% from 716.08 (95% CI 713.84–718.32) per 100,000 persons in 2013 to 1101.70 (95% CI 1098.97–1104.42) in 2020, (trend test, P < .001). The total pneumonia hospitalization rates in Wales increased by 25.75% from 791.08 (95% CI 781.17–800.98) per 100,000 persons in 2013 to 994.76 (95% CI 983.72–1005.79) in 2020 (trend test, P < .001) (Fig. 1).
Figure 1.
Total pneumonia hospitalization rates in Australia, England, and Wales from 2013 to 2020.
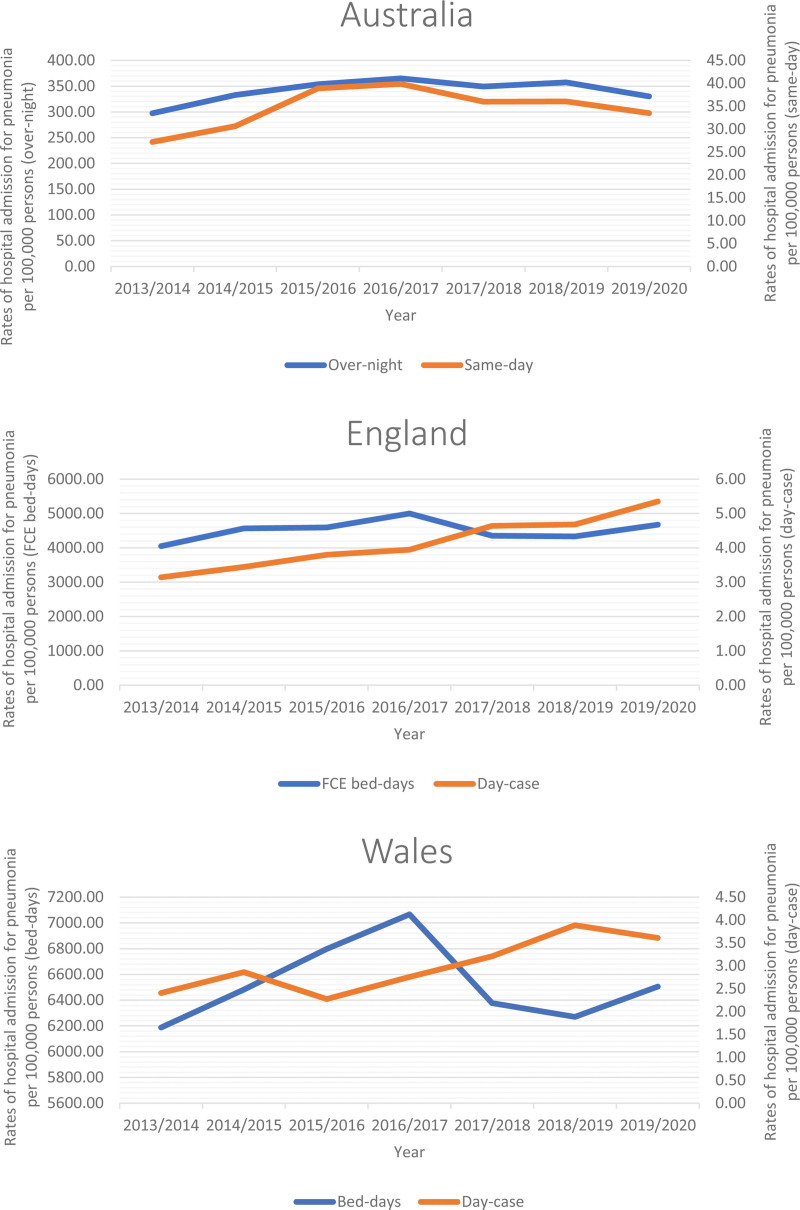
3.3. Trends in total pneumonia hospitalization stratified by hospitalization type
During the study period, most pneumonia hospitalizations in Australia, England, and Wales were non-same-day hospitalizations, accounting for 90.78%, 99.91%, and 99.95%, respectively. The rates of same-day pneumonia hospitalization increased by 23.18%, 70.28%, and 49.85% in Australia, England, and Wales, respectively. On the other hand, the rates of non-same-day pneumonia hospitalization increased by 11.04%, 15.35%, and 5.14% in Australia, England, and Wales, respectively (Table 2 and Fig. 2).
Table 2.
Percentage change in the total pneumonia hospitalization rates from 2013 to 2020 in Australia, England, and Wales stratified by hospitalization type.
| Hospitalization type | Country | Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013 to 2020 |
|---|---|---|---|---|
| Same d | Australia | 27.20 (26.53–27.87) | 33.50 (32.79–34.21) | 23.18 |
| England | 3.14 (2.99–3.29) | 5.35 (5.16–5.54) | 70.28 | |
| Wales | 2.41 (1.86–2.96) | 3.61 (2.94–4.28) | 49.85 | |
| Non-same d | Australia | 297.42 (295.22–299.62) | 330.25 (328.03–332.47) | 11.04 |
| England | 4048.83 (4043.59–4054.07) | 4670.16 (4664.65–4675.67) | 15.35 | |
| Wales | 6187.64 (6160.71–6214.58) | 6505.46 (6478.03–6532.90) | 5.14 |
Figure 2.
Total pneumonia hospitalization rates in Australia, England, and Wales from 2013 to 2020 stratified by hospitalization type.
3.4. Trends in total pneumonia hospitalization stratified by age group
From 2013 to 2020, pneumonia hospitalizations in Australia, England, and Wales were directly related to age. The pneumonia hospitalization rates increased among all age groups in Australia, England, and Wales, except for the age group below 15 years in Wales, where the rate decreased (Table 3 and Fig. 3).
Table 3.
Percentage change in the total pneumonia hospitalization rates from 2013–2020 in Australia, England, and Wales stratified by age group.
| Age group | Country | Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013–2020 |
|---|---|---|---|---|
| Below 15 yr | Australia | 211.57 (207.29–215.84) | 212.37 (208.23–216.50) | 0.38 |
| England | 126.92 (124.68–129.17) | 136.31 (134.01–138.61) | 7.40 | |
| Wales | 141.86 (131.60–152.12) | 113.25 (104.08–122.42) | −20.17 | |
| 15 to 59 yr | Australia | 123.47 (121.65–125.29) | 133.80 (131.97–135.63) | 8.37 |
| England | 170.43 (169.01–171.85) | 287.04 (285.22–288.87) | 68.42 | |
| Wales | 193.50 (187.00–200.00) | 287.84 (279.87–295.82) | 48.76 | |
| 60 to 74 yr | Australia | 533.23 (525.25–541.22) | 574.35 (566.76–581.93) | 7.71 |
| England | 1135.36 (1128.05–1142.68) | 1728.20 (1719.55–1736.85) | 52.22 | |
| Wales | 1169.54 (1140.43–1198.65) | 1419.20 (1388.04–1450.35) | 21.35 | |
| 75 yr and above | Australia | 2124.80 (2101.80–2147.80) | 2253.07 (2231.48–2274.67) | 6.04 |
| England | 5268.87 (5247.88–5289.85) | 7468.76 (7445.23–7492.29) | 41.75 | |
| Wales | 5113.15 (5030.80–5195.51) | 5783.44 (5700.14–5866.75) | 13.11 |
Figure 3.
Total pneumonia hospitalization rates in Australia, England, and Wales from 2013 to 2020 stratified by age group.
3.5. Trends in total pneumonia hospitalization stratified by gender
Over the study period, males accounted for most pneumonia hospitalizations in Australia, England, and Wales. The pneumonia hospitalization rates among males increased by 9.86%, 50.41%, and 24.62% in Australia, England, and Wales, respectively. Similarly, the pneumonia hospitalization rates among females increased by 14.56%, 57.39%, and 26.90% in Australia, England, and Wales, respectively (Table 4 and Fig. 4).
Table 4.
Percentage change in the total pneumonia hospitalization rates from 2013 to 2020 in Australia, England, and Wales stratified by gender.
| Gender | Country | Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013 to 2020 |
|---|---|---|---|---|
| Males | Australia | 346.77 (343.40–350.15) | 380.95 (377.57–384.34) | 9.86 |
| England | 744.88 (741.62–748.14) | 1120.38 (1116.45–1124.30) | 50.41 | |
| Wales | 817.77 (803.40–832.14) | 1019.11 (1003.15–1035.07) | 24.62 | |
| Females | Australia | 302.72 (299.59–305.86) | 346.79 (343.59–350.00) | 14.56 |
| England | 688.15 (685.07–691.23) | 1083.10 (1079.31–1086.88) | 57.39 | |
| Wales | 765.32 (751.66–778.98) | 971.22 (955.94–986.50) | 26.90 |
Figure 4.
Total pneumonia hospitalization rates in Australia, England, and Wales from 2013 to 2020 stratified by gender.
3.6. Trends in pneumonia hospitalization
The highest change in hospitalization rate in Australia was observed for bacterial pneumonia, not elsewhere classified related hospitalization. However, in England and Wales the highest change in hospitalization rate in was observed for viral pneumonia-related hospitalization. For further details on the change in pneumonia hospitalization rates from 2013 to 2020 in Australia, England, and Wales, refer to Table 5.
Table 5.
Percentage change in pneumonia hospitalization rates from 2013 to 2020 in Australia, England, and Wales per ICD code.
| ICD code | Australia | England | Wales | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013 to 2020 | Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013 to 2020 | Hospitalization rates in 2013 per 100,000 persons (95% CI) | Hospitalization rates in 2020 per 100,000 persons (95% CI) | % change from 2013 to 2020 | |
| J12 | 21.58 (20.99–22.17) | 46.72 (45.88–47.56) | 116.49% | 3.12 (2.98–3.27) | 14.73 (14.42–15.05) | 371.50% | 2.08 (1.57–2.59) | 9.34 (8.27–10.42) | 348.64 |
| J12.0 | 0.86 (0.75–0.98) | 1.32 (1.18–1.46) | 52.84% | 0.18 (0.14–0.22) | 0.65 (0.58–0.72) | 261.49% | 0.03 (−0.03 to 0.10) | 0.90 (0.57–1.24) | 2672.32 |
| J12.1 | 5.29 (5.00–5.59) | 10.39 (10.00–10.79) | 96.31% | 0.49 (0.43–0.55) | 5.97 (5.77–6.17) | 1116.18% | 0.49 (0.24–0.73) | 2.83 (2.24–3.43) | 480.87 |
| J12.2 | 1.32 (1.17–1.46) | 4.51 (4.25–4.77) | 242.70% | 0.45 (0.39–0.50) | 1.55 (1.45–1.65) | 246.39% | 0.23 (0.06–0.40) | 1.39 (0.97–1.80) | 508.21 |
| J12.3 | 2.17 (1.98–2.36) | 6.61 (6.30–6.93) | 204.37% | 0.42 (0.36–0.47) | 1.81 (1.70–1.92) | 334.16% | 0.16 (0.02–0.31) | 1.64 (1.19–2.09) | 909.91 |
| J12.8 | 2.61 (2.40–2.81) | 10.23 (9.84–10.62) | 292.27% | 0.35 (0.30–0.40) | 2.10 (1.98–2.22) | 503.17% | 0.20 (0.04–0.35) | 1.22 (0.83–1.61) | 527.07 |
| J12.9 | 9.32 (8.93–9.72) | 13.65 (13.20–14.11) | 46.42% | 1.24 (1.15–1.34) | 2.65 (2.52–2.79) | 113.65% | 0.98 (0.63–1.33) | 1.35 (0.94–1.76) | 38.62 |
| J13 | 7.98 (7.62–8.34) | 9.74 (9.36–10.12) | 22.07% | 9.81 (9.55–10.07) | 14.65 (14.33–14.96) | 49.28% | 6.96 (6.03–7.89) | 9.24 (8.18–10.31) | 32.79 |
| J14 | 4.96 (4.67–5.24) | 5.10 (4.82–5.38) | 2.85% | 3.44 (3.28–3.60) | 3.85 (3.69–4.02) | 12.07% | 5.30 (4.49–6.12) | 4.61 (3.85–5.36) | −13.14 |
| J15 | 17.99 (17.45–18.54) | 47.71 (46.86–48.55) | 165.13% | 15.14 (14.81–15.46) | 19.20 (18.83–19.56) | 26.81% | 22.42 (20.74–24.09) | 15.59 (14.20–16.98) | −30.45 |
| J15.0 | 1.09 (0.96–1.23) | 0.99 (0.86–1.11) | −9.90% | 2.42 (2.29–2.55) | 2.91 (2.77–3.05) | 20.16% | 3.03 (2.41–3.64) | 2.93 (2.33–3.53) | −3.12 |
| J15.1 | 4.51 (4.24–4.78) | 4.69 (4.42–4.95) | 3.88% | 4.47 (4.29–4.65) | 5.25 (5.06–5.44) | 17.45% | 4.55 (3.80–5.31) | 2.74 (2.16–3.32) | −39.89 |
| J15.2 | 2.90 (2.68–3.11) | 2.28 (2.10–2.47) | −21.26% | 1.99 (1.87–2.10) | 1.81 (1.70–1.92) | −8.92% | 4.20 (3.47–4.92) | 2.16 (1.64–2.67) | −48.58 |
| J15.3 | 0.08 (0.04–0.11) | 0.09 (0.05–0.12) | 11.86% | 0.14 (0.11–0.17) | 0.15 (0.11–0.18) | 6.96% | 0.07 (−0.03 to 0.16) | 0.00 (0.00–0.00) | −100.00 |
| J15.4 | 1.07 (0.94–1.20) | 1.07 (0.94–1.19) | −0.09% | 1.78 (1.67–1.89) | 2.28 (2.15–2.40) | 28.04% | 2.54 (1.97–3.10) | 2.61 (2.04–3.18) | 2.82 |
| J15.5 | 0.59 (0.49–0.69) | 0.51 (0.42–0.60) | −13.12% | 1.11 (1.02–1.19) | 1.24 (1.15–1.33) | 12.43% | 2.18 (1.66–2.70) | 0.68 (0.39–0.97) | −68.97 |
| J15.6 | 0.83 (0.71–0.94) | 1.26 (1.12–1.40) | 52.39% | 0.72 (0.65–0.79) | 1.23 (1.14–1.32) | 71.52% | 0.78 (0.47–1.09) | 1.19 (0.81–1.58) | 52.64 |
| J15.7 | 3.34 (3.11–3.57) | 6.31 (6.00–6.62) | 89.01% | 0.60 (0.54–0.67) | 1.60 (1.50–1.70) | 165.97% | 0.68 (0.39–0.98) | 1.84 (1.36–2.31) | 168.74 |
| J15.8 | 1.08 (0.95–1.22) | 1.31 (1.17–1.45) | 21.43% | 0.80 (0.72–0.87) | 0.58 (0.52–0.65) | −26.83% | 1.53 (1.09–1.97) | 0.74 (0.44–1.04) | −51.55 |
| J15.9 | 2.51 (2.31–2.71) | 29.20 (28.54–29.86) | 1063.89% | 1.12 (1.03–1.21) | 2.15 (2.03–2.27) | 91.32% | 2.86 (2.26–3.46) | 0.71 (0.41–1.00) | −75.25 |
| J16 | 0.93 (0.81–1.06) | 0.00 (0.00–0.00) | −100.00% | 0.22 (0.18–0.25) | 0.42 (0.36–0.47) | 93.06% | 0.33 (0.12–0.53) | 0.48 (0.24–0.73) | 48.52 |
| J16.0 | 0.45 (0.37–0.54) | 0.00 (0.00–0.00) | −100.00% | 0.03 (0.02–0.05) | 0.03 (0.02–0.05) | 7.88% | 0.00 (0.00–0.00) | 0.10 (−0.01 to 0.21) | - |
| J16.8 | 0.48 (0.39–0.57) | 0.00 (0.00–0.00) | −100.00% | 0.18 (0.15–0.22) | 0.38 (0.33–0.43) | 107.54% | 0.33 (0.12–0.53) | 0.39 (0.17–0.61) | 18.81 |
| J17 | 0.98 (0.85–1.10) | 1.98 (1.80–2.15) | 102.64% | 1.01 (0.93–1.10) | 0.94 (0.86–1.02) | −6.81% | 1.27 (0.87–1.67) | 1.06 (0.70–1.43) | −16.22 |
| J17.0 | 0.35 (0.27–0.42) | 0.12 (0.08–0.17) | −63.84% | 0.31 (0.27–0.36) | 0.01 (0.00–0.02) | −95.46% | 0.55 (0.29–0.82) | 0.00 (0.00–0.00) | −100.00 |
| J17.1 | 0.00 (0.00–0.00) | 0.09 (0.05–0.13) | - | 0.09 (0.06–0.11) | 0.05 (0.03–0.07) | −41.68% | 0.03 (−0.03 to 0.10) | 0.00 (0.00–0.00) | −100.00 |
| J17.2 | 0.23 (0.16–0.29) | 1.70 (1.54–1.86) | 651.20% | 0.36 (0.31–0.41) | 0.50 (0.44–0.56) | 36.50% | 0.52 (0.27–0.78) | 0.55 (0.29–0.81) | 5.20 |
| J17.3 | 0.40 (0.32–0.49) | 0.00 (0.00–0.00) | −100.00% | 0.24 (0.20–0.28) | 0.36 (0.31–0.41) | 49.58% | 0.16 (0.02–0.31) | 0.52 (0.26–0.77) | 216.84 |
| J17.8 | 0.00 (0.00–0.00) | 0.07 (0.03–0.10) | - | 0.01 (0.00–0.01) | 0.02 (0.01–0.03) | 253.94% | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) | - |
| J18 | 270.20 (268.10–272.30) | 252.51 (250.57–254.45) | −6.55% | 683.34 (681.15–685.53) | 1047.91 (1045.25–1050.57) | 53.35% | 752.72 (743.06–762.38) | 954.43 (943.61–965.24) | 26.80 |
| J18.0 | 11.77 (11.33–12.21) | 6.56 (6.24–6.87) | −44.30% | 31.87 (31.40–32.35) | 26.32 (25.90–26.75) | −17.41% | 42.75 (40.44–45.06) | 25.83 (24.05–27.62) | −39.57 |
| J18.1 | 2.70 (2.49–2.91) | 1.67 (1.51–1.83) | −37.97% | 422.49 (420.77–424.22) | 647.09 (644.99–649.18) | 53.16% | 469.55 (461.91–477.19) | 549.98 (541.75–558.21) | 17.13 |
| J18.2 | 0.29 (0.22–0.36) | 0.11 (0.07–0.15) | −60.97% | 0.37 (0.32–0.42) | 0.30 (0.26–0.35) | −18.76% | 0.39 (0.17–0.61) | 0.58 (0.31–0.85) | 48.52 |
| J18.8 | 3.27 (3.04–3.50) | 2.50 (2.31–2.69) | −23.51% | 0.72 (0.65–0.79) | 0.67 (0.61–0.74) | −6.43% | 0.33 (0.12–0.53) | 0.55 (0.29–0.81) | 68.32 |
| J18.9 | 252.17 (250.14–254.20) | 241.67 (239.77–243.57) | −4.17% | 227.88 (226.61–229.15) | 373.52 (371.93–375.12) | 63.91% | 239.70 (234.24–245.17) | 377.49 (370.66–384.31) | 57.48 |
ICD = International Statistical Classification of Diseases.
4. Discussion
This study aimed to examine pneumonia hospitalization patterns in Australia, England, Wales during the past 2 decades. In this study, the most common type of pneumonia hospitalization in Australia, England, and Wales was “pneumonia, organism unspecified,” accounting for 77.12%, 95.49%, and 95.75% of the total number of pneumonia hospitalizations in each country, respectively. Besides, the most common subtype of pneumonia hospitalization in Australia was “pneumonia, unspecified,” accounting for 72.98% of the total number of pneumonia hospitalizations in the country. The most common type of pneumonia hospitalization in England and Wales was “lobar pneumonia, unspecified,” accounting for 59.00% and 56.73%. In a large study conducted in England using the Hospital Episode Statistics databased on all pneumonia episodes that reported between April 1997 and March 2005, around 42% of pneumonia hospital admissions was related to nonspecific pneumonia, influenza for 10%, H. influenzae for 9%, Bordetella pertussis for 7%, and RSV for 5%.[29] On the other hands, all-cause pneumonia accounted for 791,812 admissions in Australian hospitals between July 1998 and June 2011. Pneumococcal and lobar pneumonia episodes made up 4.3% of the total number of admissions, while other specific causal organism codes accounted for the remaining 10.0%.[30] A basic issue with pneumonia is the inadequate classification of related but heterogeneous diseases and clinical phenotypes due to the lack of generally recognized, widely used, and acceptable definition or definitions. The widespread incapacity to identify the infectious organism or organisms causing lung infections, which calls for empirical antibiotic therapy, is the clearest indication of the severity of this issue.[31,32]
In this study, the total pneumonia hospitalization rates in Australia increased by 12.06% from 324.62 (95% CI 322.32–326.92) per 100,000 persons in 2013 to 363.75 (95% CI 361.42–366.08) per 100,000 persons in 2020, (trend test, P < .001). The total pneumonia hospitalization rates in England increased by 53.85% from 716.08 (95% CI 713.84–718.32) per 100,000 pers persons in 2013 to 1101.70 (95% CI 1098.97–1104.42) in 2020, (trend test, P < .001). The total pneumonia hospitalization rates in Wales increased by 25.75% from 791.08 (95% CI 781.17–800.98) per 100,000 persons in 2013 to 994.76 (95% CI 983.72–1005.79) in 2020 (trend test, P < .001). Early research in the US and Europe found that hospitalizations for pneumonia among adults were on the rise over time with the aging of the population and the rising incidence of underlying diseases being 2 potential risk factors.[4–6] Comorbidities, excessive alcohol consumption, and smoking are other risk factors that increase the possibility of pneumonia hospitalization.[33] The all-cause pneumonia hospitalization rate per 1000 person-years among individuals aged 41 to 64, 65 to 79, and ≥ 80 years rose from 2.92, 14.06, and 31.71 in 1997 to 5.27, 21.32, and 60.38 in 2011, according to a study based on the entire Danish population.[34] The percentage of hospitalized patients with pneumonia who also had underlying illnesses rose from 42.9% to 46.2% according to a previous US study that used data from the National Hospital Discharge Survey. Moreover, the rate of hospitalization for pneumonia among persons aged 65 and older increased by 20% between 1988 and 2002.[4]
Hospitalization, morbidity, and mortality rates can be reduced by identifying risk factors and putting policies in place to limit exposure to modifiable circumstances.[35–40] Age,[35,36] COPD,[35] asthma, diabetes mellitus, congestive heart failure, smoking, malnutrition, and aspiration are risk factors linked to CAP.[35,36,38,40] Additional research indicates that certain types of medication may raise the risk of CAP. According to a nested case-control study, older individuals who take atypical antipsychotic medications had a 2.1-fold increased risk of pneumonia.[39] Proton pump inhibitors dramatically raise the incidence of hospital-acquired pneumonia by 30% and CAP by 50% to 89%.[37] A higher incidence of pneumonia hospitalization was linked to advanced age, male gender, and prior underlying illnesses.[41]
In this study, most pneumonia hospitalizations in Australia, England, and Wales were non-same-day hospitalizations, accounting for 90.78%, 99.91%, and 99.95%, respectively. The rates of same-day pneumonia hospitalization increased by 23.18%, 70.28%, and 49.85% in Australia, England, and Wales, respectively. On the other hand, the rates of non-same-day pneumonia hospitalization increased by 11.04%, 15.35%, and 5.14% in Australia, England, and Wales, respectively. There are multiple factors influencing length of stay in pneumonia patients such as health-care system and hospital management, clinical practice such as (the abilities, expertise, and proficiency of doctors using sound, established clinical recommendations, Early transition from intravenous to oral antibiotic treatment, withdrawal of oxygen when necessary, physicians’ opinions regarding the efficacy of medical interventions), and patient characteristics.[42] Furthermore, a large study included 400,000 adult patients done in (January 1998 to March 1999) in a public acute-care teaching hospital in Valencia (Spain) found that 29% of patients had possibly unnecessary hospitalization due to the “weekend effect” and/or delays in the availability of laboratory test results or chest radiography days.[43] In addition, multiple clinical factors may affect duration of hospitalization like hypoxemia, anemia, neoplastic illness, and complications within 72 hours of admission.[43] A common requirement for hospital admission is hypoxemia, which supports the admission patient to intensive care.[44] It is crucial to note that hospitals with the shortest length of stay did not have higher readmission rates or post-discharge mortality rates among CAP patients.[45,46] These statistics may serve as a helpful standard for doctors and hospitals to lower the length of stay for CAP patients without posing any new risk on the patients.
In this study, males accounted for most pneumonia hospitalizations in Australia, England, and Wales. The pneumonia hospitalization rates among males increased by 9.86%, 50.41%, and 24.62% in Australia, England, and Wales, respectively. Similarly, the pneumonia hospitalization rates among females increased by 14.56%, 57.39%, and 26.90% in Australia, England, and Wales, respectively. This result is consistent with large cohort study conducted in USA during 2006 through 2010, where males exhibited higher rates of at-risk behaviors and comorbidities,[47] which probably contributes significantly to their increased prevalence of pneumonia. Overall, the age of the patients and the study locations may have had an impact on the sex differences observed in these cohorts in addition to other illnesses. It should come as no surprise that delayed hospital presentation for other acute medical conditions has been documented in females,[48] and this may also be a factor in the lower incidence of CAP seen in females, who tend to seek hospital assistance only when clinical conditions worsen (rather than mild cases), which are likely to resolve on their own.[48] Smoking and male gender have previously been shown to be risk factors for pneumonia due to Legionella pneumophila.[49] Immune responses to particular pathogens and sex-specific immune responses interact during the course of an illness an obvious illustration of this link between the incidence and prognosis of influenza virus A infections by sex.[50] The WHO released a paper in 2010 outlining the evidence that gender and sex should be taken into account when assessing influenza virus infection exposure and outcome.[51]
The highest change in hospitalization rate in Australia was observed for bacterial pneumonia, not elsewhere classified related hospitalization. However, in England and Wales the highest change in hospitalization rate in was observed for viral pneumonia-related hospitalization Streptococcus pneumoniae, Hemophilus influenzae (including H. influenzae type b-Hib), Staphylococcus aureus, and other bacteria are the culprits behind pneumonia. Among them include Mycobacterium tuberculosis, Chlamydia, and Mycoplasma.[52] Moreover, influenza continues to be the clinically most important viral cause of adult CAP among viral diseases; other prevalent viral pathogens include Adenovirus, RSV, and parainfluenza viruses (PIV). Human metapneumovirus (HMPV), coronaviruses, and rhinoviruses are among the other viruses found in CAP patients.[53]
It worth mentioning that the COVID-19 pandemic control measures have had an impact on influenza and other respiratory virus transmission. Public health messaging, physical and social separation, national lockdowns, hand cleanliness, facial coverings, and travel limitations were some of these efforts. Some influenza indicators are also directly and indirectly impacted by changes in health-care-seeking behaviors.[54] When interpreting the influenza surveillance indicators presented in this report, these factors remain crucial, particularly when comparing with previous seasons. Even that vaccination is still the most well-known and researched method of preventing pneumonia,[55] it is crucial to understand the modifiable risk factors that contribute to the development of the illness. Malnutrition, which is a significant risk factor for pneumonia.[40] Even in older people, the risk of pneumonia may be reduced by reducing lifestyle-related risk factors like smoking and alcohol use.[52] Pneumonia risk can also be decreased by closely monitoring side effects and carefully reviewing prescription drugs.[37–40] Furthermore, since pathogens were not found in most patients, this likely reflects the relative insensitivity of diagnostic techniques. It is necessary to continue developing new quick diagnostic technologies that can reliably identify and differentiate between possible pneumonia pathogens.[56]
This study has limitations. The study time frame was restricted to examine admissions until 2020. This was due to the fact that COVID-19 pandemic affected the normal pattern of admissions due to different health conditions. This study utilized publicly available data on the population level rather than on the individual level of the patients. This restricted the ability to examine the impact of confounding factors on the estimated hospitalization rates. Overestimation is a common limitation for this type of study as admission rates could include readmission and multiple admissions of the same patient. Therefore, the study findings should be interpreted carefully.
5. Conclusion
This study highlighted that hospitalization rate for pneumonia increased during the past decade in Australia, England, and Wales. The most common type of pneumonia hospitalization was “pneumonia, organism unspecified.” Most pneumonia hospitalizations were non-same-day hospitalizations. The age and male gender were clearly contributing factors that affected pneumonia hospitalizations rate. Future studies should identify modifiable risk factors among these population specifically and work on decreasing their impact. Educational campaign aiming to increase public knowledge of pneumonia, its risk factors, and lifestyle modification should be prioritized to decrease pneumonia episodes.
Author contributions
Conceptualization: Mohammed Samannodi.
Data curation: Mohammed Samannodi.
Formal analysis: Mohammed Samannodi.
Funding acquisition: Mohammed Samannodi.
Investigation: Mohammed Samannodi.
Methodology: Mohammed Samannodi.
Project administration: Mohammed Samannodi.
Resources: Mohammed Samannodi.
Software: Mohammed Samannodi.
Supervision: Mohammed Samannodi.
Validation: Mohammed Samannodi.
Visualization: Mohammed Samannodi.
Writing – original draft: Mohammed Samannodi.
Writing – review & editing: Mohammed Samannodi.
Abbreviations:
- ABS
- Australian Bureau of Statistics
- AIHW
- Australian Institute of Health and Welfare
- BTS
- British Thoracic Society
- COPD
- chronic obstructive pulmonary disease
- HES
- hospital episode statistics database
- ICD
- International Statistical Classification of Diseases
- NHMD
- National Hospital Morbidity Database
- NHS
- National Health Service
- ONS
- Office for National Statistics
- WHO
- World Health Organization
This study utilized publicly available data and considered excepted from ethical approval.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Samannodi M. Hospitalization due to pneumonia in Australia, England, and Wales: An ecological cross-sectional study. Medicine 2025;104:15(e42163).
References
- [1].World Health Organization. Pneumonia. 2024. https://www.who.int/news-room/fact-sheets/detail/pneumonia. Accessed December 23, 2024. [Google Scholar]
- [2].World Health Organization. The Top 10 Causes of Death. 2024. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed December 23, 2024. [Google Scholar]
- [3].Daniel P, Woodhead M, Welham S, Mckeever TM, Lim WS; British Thoracic Society. Mortality reduction in adult community-acquired pneumonia in the UK (2009-2014): results from the British Thoracic Society audit programme. Thorax. 2016;71:1061–3. [DOI] [PubMed] [Google Scholar]
- [4].Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. 2005;294:2712–9. [DOI] [PubMed] [Google Scholar]
- [5].Oosterheert JJ, Bonten MJM, Hak E, Lammers JWJ, Schneider MME, Hoepelman IM. The increase in pneumonia-related morbidity and mortality among adults in the Netherlands and possible explanations for it. Ned Tijdschr Geneeskd. 2004;148:1765–9. [PubMed] [Google Scholar]
- [6].Thomsen RW, Riis A, Nørgaard M, et al. Rising incidence and persistently high mortality of hospitalized pneumonia: a 10-year population-based study in Denmark. J Intern Med. 2006;259:410–7. [DOI] [PubMed] [Google Scholar]
- [7].Naser AY, Mansour MM, Alanazi AFR, et al. Hospital admission trends due to respiratory diseases in England and Wales between 1999 and 2019: an ecologic study. BMC Pulm Med. 2021;21:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Alwafi H, Naser AY, Ashoor DS, et al. Trends in hospital admissions and prescribing due to chronic obstructive pulmonary disease and asthma in England and Wales between 1999 and 2020: an ecological study. BMC Pulm Med. 2023;23:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chalmers J, Campling J, Ellsbury G, Hawkey PM, Madhava H, Slack M. Community-acquired pneumonia in the United Kingdom: a call to action. Pneumonia (Nathan) 2017;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ingarfield SL, Celenza A, Jacobs IG, Riley TV. The bacteriology of pneumonia diagnosed in Western Australian emergency departments. Epidemiol Infect. 2007;135:1376–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Australian Institute of Health Welfare. Principal Diagnosis Data Cubes. AIHW; 2024. [Google Scholar]
- [12].Alrajeh A, Naser AY, Aldabayan YS, et al. Hospitalisation patterns for respiratory diseases in Australia: an ecological study. BMJ Open. 2024;14:e084286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Al Rajeh AM, Naser AY, Siraj R, et al. Acute upper respiratory infections admissions in England and Wales. Medicine (Baltim) 2023;102:e33616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Naser AY, Al-Shehri H. Admissions due to perinatal respiratory and cardiovascular disorders in England. J Multidiscip Healthc. 2023;16:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Australian Institute of Health Welfare. National Hospitals Data Collection. 2024. https://www.aihw.gov.au/about-our-data/our-data-collections/national-hospitals-data-collection. Accessed November 13, 2024. [Google Scholar]
- [16].Australian Institute of Health Welfare. About the Data. 2024. https://www.aihw.gov.au/reports-data/myhospitals/content/about-the-data. Accessed November 13, 2024. [Google Scholar]
- [17].Department of Health; State of Western Australia. Hospital Morbidity Data Collection Data Validation Manual. 2024. https://www.health.wa.gov.au/-/media/Corp/Documents/Health-for/PAD/HMDC-Data-Validation-Manual.pdf. Accessed November 13, 2024. [Google Scholar]
- [18].NHS England. Hospital Episode Statistics (HES). 2024. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics. Accessed November 13, 2024. [Google Scholar]
- [19].Service, N.W.I., Data Quality Status Report: Admitted Patient Care Data Set. 2021.
- [20].Naser AY, Wang Q, Wong LYL, et al. Author correction: hospital admissions due to dysglycaemia and prescriptions of antidiabetic medications in England and Wales: an ecological study. Diabetes Ther. 2018;9:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hemmo SI, Naser AY, Alwafi H, et al. Hospital admissions due to ischemic heart diseases and prescriptions of cardiovascular diseases medications in England and Wales in the past two decades. Int J Environ Res Public Health. 2021;18:7041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sweiss K, Naser AY, Samannodi M, Alwafi H. Hospital admissions due to infectious and parasitic diseases in England and Wales between 1999 and 2019: an ecological study. BMC Infect Dis. 2022;22:398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hemmo SI, Naser AY, Taybeh EO. Hospital admission due to hypotension in Australia and in England and Wales. Healthcare (Basel) 2023;11:1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Australian Bureau of Statistics. About the Australian Bureau of Statistics. 2024. https://www.abs.gov.au/about. Accessed November 13, 2024. [Google Scholar]
- [25].Australian Bureau of Statistics. National, State and Territory Population. 2024. https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release#cite-window1. Accessed November 13, 2024. [Google Scholar]
- [26].Office for National Statistics. Estimates of the Population for the UK, England, Wales, Scotland, and Northern Ireland. 2024. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland. Accessed November 13, 2024. [Google Scholar]
- [27].NHS England. Hospital Admitted Patient Care Activity. 2024. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity. Accessed November 13, 2024. [Google Scholar]
- [28].Digital Health and Care Wales. Annual PEDW Data Tables. 2024. https://dhcw.nhs.wales/data/statistical-publications-data-products-and-open-data/annual-pedw-data-tables/. Accessed November 13, 2024. [Google Scholar]
- [29].Trotter CL, Stuart JM, George R, Miller E. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis. 2008;14:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Menzies RI, Jardine A, McIntyre PB. Pneumonia in elderly Australians: reduction in presumptive pneumococcal hospitalizations but no change in all-cause pneumonia hospitalizations following 7-valent pneumococcal conjugate vaccination. Clin Infect Dis. 2015;61:927–33. [DOI] [PubMed] [Google Scholar]
- [31].Mackenzie G. The definition and classification of pneumonia. Pneumonia (Nathan) 2016;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].van der Eerden MM, Vlaspolder F, de Graaff CS, et al. Comparison between pathogen directed antibiotic treatment and empirical broad spectrum antibiotic treatment in patients with community acquired pneumonia: a prospective randomised study. Thorax. 2005;60:672–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Center for Disease Prevention and Control. Risk Factors for Pneumonia. 2025. https://www.cdc.gov/pneumonia/risk-factors/index.html#:~:text=Risk%20Factors%20for%20Pneumonia%201%20About%20risk%20There,Times%20of%20increased%20risk%20...%206%20Resources%20. Accessed March 23, 2025. [Google Scholar]
- [34].Zhang J, Lim Y-H, So R, et al. Long-term exposure to air pollution and risk of acute lower respiratory infections in the Danish nurse cohort. Ann Am Thorac Soc. 2024;21:1129–38. [DOI] [PubMed] [Google Scholar]
- [35].Farr BM, Bartlett CL, Wadsworth J, Miller DL. Risk factors for community-acquired pneumonia diagnosed upon hospital admission. British Thoracic Society Pneumonia Study Group. Respir Med. 2000;94:954–63. [DOI] [PubMed] [Google Scholar]
- [36].Farr BM, Woodhead MA, Macfarlane JT, et al. Risk factors for community-acquired pneumonia diagnosed by general practitioners in the community. Respir Med. 2000;94:422–7. [DOI] [PubMed] [Google Scholar]
- [37].Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA. 2009;301:2120–8. [DOI] [PubMed] [Google Scholar]
- [38].Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39:1642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Knol W, van Marum RJ, Jansen PAF, Souverein PC, Schobben AFAM, Egberts ACG. Antipsychotic drug use and risk of pneumonia in elderly people. J Am Geriatr Soc. 2008;56:661–6. [DOI] [PubMed] [Google Scholar]
- [40].LaCroix AZ, Lipson S, Miles TP, White L. Prospective study of pneumonia hospitalizations and mortality of U.S. older people: the role of chronic conditions, health behaviors, and nutritional status. Public Health Rep. 1989;104:350–60. [PMC free article] [PubMed] [Google Scholar]
- [41].Lin CJ, Chang Y-C, Tsou M-T, Chan H-L, Chen Y-J, Hwang L-C. Factors associated with hospitalization for community-acquired pneumonia in home health care patients in Taiwan. Aging Clin Exp Res. 2020;32:149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Cabre M, Bolivar I, Pera G, Pallares R; Pneumonia Study Collaborative Group. Factors influencing length of hospital stay in community-acquired pneumonia: a study in 27 community hospitals. Epidemiol Infect. 2004;132:821–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Menéndez R, Ferrando D, Vallés JM, Martínez E, Perpiñá M. Initial risk class and length of hospital stay in community-acquired pneumonia. Eur Respir J. 2001;18:151–6. [DOI] [PubMed] [Google Scholar]
- [44].Weingarten SR, Riedinger MS, Varis G, et al. Identification of low-risk hospitalized patients with pneumonia. Implications for early conversion to oral antimicrobial therapy. Chest. 1994;105:1109–15. [DOI] [PubMed] [Google Scholar]
- [45].Baker DW, Einstadter D, Husak SS, Cebul RD. Trends in postdischarge mortality and readmissions: has length of stay declined too far? Arch Intern Med. 2004;164:538–44. [DOI] [PubMed] [Google Scholar]
- [46].McCormick D, Fine MJ, Coley CM, et al. Variation in length of hospital stay in patients with community-acquired pneumonia: are shorter stays associated with worse medical outcomes? Am J Med. 1999;107:5–12. [DOI] [PubMed] [Google Scholar]
- [47].Corica B, Tartaglia F, D’Amico T, Romiti GF, Cangemi R. Sex and gender differences in community-acquired pneumonia. Intern Emerg Med. 2022;17:1575–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Siegel SJ, Weiser JN. Mechanisms of bacterial colonization of the respiratory tract. Annu Rev Microbiol. 2015;69:425–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Bagaitkar J, Demuth DR, Scott DA. Tobacco use increases susceptibility to bacterial infection. Tob Induc Dis. 2008;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Torres A, Cillóniz C. Epidemiology, etiology, and risk factors of bacterial pneumonia. In: Torres A. and Cillóniz C., eds. Clinical Management of Bacterial Pneumonia. Springer International Publishing; 2015:7–28. [Google Scholar]
- [51].Klein SL, Passaretti C, Anker M, Olukoya P, Pekosz A. The impact of sex, gender and pregnancy on 2009 H1N1 disease. Biol Sex Differ. 2010;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Brooks WA. Hunter’s Tropical Medicine and Emerging Infectious Diseases. Elsevier; 2020. [Google Scholar]
- [53].Dandachi D, Rodriguez-Barradas MC. Viral pneumonia: etiologies and treatment. J Investig Med. 2018;66:957–65. [DOI] [PubMed] [Google Scholar]
- [54].Groves HE, Piché-Renaud P-P, Peci A, et al. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: a population-based study. Lancet Reg Health Am. 2021;1:100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Jain S, Self WH, Wunderink RG, et al. ; CDC EPIC Study Team. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373:415–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Caliendo AM, Gilbert DN, Ginocchio CC, et al. ; Infectious Diseases Society of America (IDSA). Better tests, better care: improved diagnostics for infectious diseases. Clin Infect Dis. 2013;57(Suppl 3):S139–70. [DOI] [PMC free article] [PubMed] [Google Scholar]