Abstract
IFN function is critical for recovery from most primary viral infections, including poxvirus infection. In contrast, very little is known about the requirement for IFN function in mediating recovery from a secondary virus infection. We have used ectromelia virus (ECTV), an orthopoxvirus very closely related to variola virus, to investigate the importance of IFN function in recovery from a secondary infection. Variola virus, the causative agent of smallpox in humans, and ECTV, which causes mousepox in mice, both encode receptor homologs that are thought to interfere with host IFN function. Using a prime-challenge regime, in which avirulent ECTV is used to prime mice deficient in type I/II IFN function or IFN regulatory factor 1 (IRF-1) and then challenging the mice with a virulent strain, we show that IFN function is redundant for virus clearance during a secondary ECTV infection. A neutralizing Ab response is generated in a secondary infection, even in the absence of IFN function, although when present, IFN strongly influences the neutralizing titer and subtype of IgG that is produced. Importantly, the depletion of CD8+ T lymphocytes during a secondary challenge in IFN-deficient mice does not affect their capacity to clear ECTV, indicating that Ab is critical for the control of a secondary infection.
Keywords: antibody, CD8 T cells, ectromelia virus, IFN regulatory factor 1, type I/II IFN
IFN is regarded as part of the first line of defense and is known to play a central role in response to viral infections (reviewed in ref. 1). Type I IFN (IFN-α/β) is secreted early and serves to defend the host by induction of an antiviral state, recruitment of various leukocyte subsets to the site of infection, and induction of a T helper 1-biased inflammatory response. On the other hand, IFN-γ, the only type II IFN, mediates antiviral and immunoregulatory functions in both the innate and the adaptive phases of the immune response (2). The transcription factor IFN regulatory factor 1 (IRF-1) is an important downstream effector molecule for type I/II IFN signaling (reviewed in ref. 3). Mice deficient in IRF-1 have been shown to have defects in IFN responses (4), inducible nitric oxide synthase up-regulation in macrophages (5), CD8+ T cell numbers and survival (6), natural killer cell activity (7), and generation of a T helper 1-type of cytokine response (8), all of which are known to be crucial for recovery from a primary ectromelia virus (ECTV) infection (9-11).
The importance of type I/II IFN for the recovery of mice from a primary ECTV infection has been extensively studied through the use of IFN receptor- or ligand-deficient animals and IFN-depleting Ab (11-13). This importance is further underscored by the fact that the virus, a natural mouse pathogen that has coevolved with the host, itself encodes viral homologs of secreted receptors for IFN-α/β (14) and IFN-γ (15, 16). These molecules are not unique to ECTV, because variola virus (VARV) and several other poxviruses also encode receptor homologs that bind to host IFN and modulate their signaling pathways. Recently, by using vaccinia virus recombinants encoding type III IFN (IFN-λ2 or IFN-λ3), Bartlett et al. (17) have shown that this class of IFN exhibits antiviral activity in mice.
Our understanding of the pathogenesis of smallpox in humans comes from studies in animal models, such as monkeypox and mousepox. The need to rely on animal models is largely due to the fact that smallpox was eradicated before the recent advances in molecular biology, virology, and immunology. However, we are still lacking in our knowledge about the determinants of the immune response that would result in recovery after infection and those that would protect against reinfection or infection after vaccination in humans. Mousepox has been extensively studied and is arguably one of the best available small animal models to examine the immune response to poxvirus infections. Like VARV, ECTV has coevolved with its natural host, encodes various immune-modifying proteins, and is highly virulent, causing disease with high mortality rates.
In contrast to a primary poxvirus infection where IFN is known to play a critical role (12, 13, 18, 19), very little is known about the contribution of IFN in a secondary infection, for example, during reinfection or infection in a vaccinated individual. To investigate the contributions of type I/II IFN and IRF-1 function in control of a secondary ECTV infection, we used a panel of targeted gene knockout (KO) mice where one or more of these molecules were absent. A prime-challenge approach, where groups of mice were first primed with avirulent ECTV 4 weeks before a challenge with virulent ECTV, was used to investigate correlates of protection after a secondary challenge. These responses were compared with a primary infection in which mice received only virulent ECTV. We found that, although mice deficient in type I and II IFN function were highly susceptible to a primary ECTV infection, they were able to control virus effectively and recover from a secondary infection without developing any signs of disease. The capacity of these mice to overcome a secondary infection was associated with their ability to generate neutralizing Ab and was not dependent on CD8+ T lymphocyte function.
Materials and Methods
Viruses. Plaque-purified ECTV Moscow (VR 1374, American Type Culture Collection), hereafter referred to as virulent ECTV, was propagated as described in ref. 20 in BS-C-1 cells (CCL26, American Type Culture Collection) and used to infect and challenge mice. The thymidine kinase-deficient strain of ECTV Moscow kindly provided by R. J. Jackson (21), hereafter referred to as avirulent ECTV, also propagated in BS-C-1 cells, was used to prime mice.
Mice. Female, specific pathogen-free mice were used between 8 and 12 weeks of age. The following mice with deficiency in IFN function were used: mice lacking the IFN-α/β receptor (IFN-α/βR), designated IFN-α/βR-/- (22); mice deficient in IFN-γR, designated IFN-γR-/- (23); mice deficient in both IFN-α/βR and IFN-γR, designated IFN-α/β/γR-/- (22); and mice deficient in IRF-1, designated IRF-1-/- (24). Because all of these strains were generated on a 129S7/SvEvBrd (129S7) background, 129S7 mice were used as WT controls. All experiments were performed according to institutional guidelines for animal care and use.
Infection. Groups of mice were primed through the i.p. route with 105 plaque-forming units (pfu) of avirulent ECTV. Priming with this poorly replicating, avirulent virus induced both cell-mediated immunity and neutralizing Ab responses, which peaked at days 8 and 14 after infection, respectively. Both these responses were undetectable by 4 weeks. After 4 weeks, these mice were challenged in the left hind footpad with 103 pfu of virulent ECTV. A highly virulent dose of virus, used for challenge experiments, was determined by infecting groups of mice with a range of doses, as indicated in Table 1. Unprimed, age- and sex-matched animals also were infected with 103 pfu of virulent ECTV in parallel experiments. Before challenge and 2 weeks after challenge, all mice were bled from the tail vein, and sera were collected. Animals were observed for signs of disease, such as ruffled fur and hunched back. For some experiments, mice were killed by cervical dislocation, and sera were collected by means of cardiac puncture 5 days after challenge. Organs were removed aseptically, and virus titers were determined by the virus plaque assay using BS-C-1 cells as described in ref. 20.
Table 1. Mice lacking IFN function are highly susceptible to virulent ECTV infection.
| Virus dose, pfu
|
Mean time to death, days
|
||||
|---|---|---|---|---|---|
| WT | IFN-γR−/− | IFN-α/βR−/− | IFN-α/β/γR−/− | IRF-1−/− | |
| 100 | ND | 23.0 ± 1.8 | 10.2 ± 1.1 | 9.6 ± 1.5 | 10.4 ± 1.9 |
| 101 | ND | 17.2 ± 1.5 | 7.4 ± 0.5 | 7.4 ± 0.9 | 8.2 ± 0.8 |
| 102 | ND | 13.8 ± 1.8 | 6.6 ± 0.5 | 6.8 ± 0.8 | 7.0 ± 0.7 |
| 103 | ND | 9.6 ± 0.9 | 6.2 ± 0.4 | 6.0 ± 0.7 | 6.2 ± 0.4 |
Mice were infected with virulent ECTV at the doses indicated in the hind footpad. Data presented are mean ± SD of five animals per group. ND, no deaths.
In experiments where CD8+ T cells were depleted, groups of mice from each strain were treated with mAb clone 2.43.1 (1 mg per mouse per dose) before and after challenge (on days -1, 1, and 3 after challenge) as described in ref. 10. The efficiency of depletion was assessed by flow cytometric analysis and routinely found to be >99%.
Anti-ECTV Ab Determination. Serum samples that were collected from primed mice before challenge and 2 weeks after challenge were assayed by ELISA for total ECTV-specific IgG and IgG subtypes as described in ref. 11. The ELISA used here predominantly detects Ab directed against the intracellular mature virus. Briefly, U-bottom 96-well plates (Immulon 2, Dynatech) were coated with purified ECTV. Sera from uninfected and infected mice were assayed at various dilutions (ranging from 1:50 to 1:1,000), and ECTV-specific Ab was detected by using horseradish peroxidase-conjugated goat anti-mouse IgM, IgG, or IgG subclasses (Southern Biotechnology Associates), with color developed by using TMB One-Step substrate (DAKO). Based on this titration, a serum dilution of 1:200 was selected for the determination of relative Ab levels.
Plaque-Reduction Neutralization Test. The plaque-reduction neutralization test, used to determine the virus-neutralizing activity of the Ab present in serum samples, was based on the method used for vaccinia virus (25). Briefly, serum samples were inactivated at 56°C for 30 min, and serial dilutions were made in PBS. Samples were incubated at 37°C for 1 h with 100 pfu of virulent ECTV before being adsorbed for 1 h on BS-C-1 cell monolayers. Overlay media containing 1% methylcellulose and 2.5% FCS in MEM (Invitrogen) was then carefully added. The plates were incubated at 34°C for 4 days, and resulting plaques were visualized by crystal violet staining. Heat-inactivated sera from uninfected mice were used as controls. The neutralization titer was taken as the reciprocal of the dilution of sera that caused a 50% reduction in the number of virus plaques over and above the number of plaques in the samples with sera from naïve mice.
Statistical Analysis. For comparison of viral titers, the nonparametric Mann-Whitney test was used, employing the statistical program prism (GraphPad, San Diego). P < 0.05 was considered significant.
Results
Outcome of a Primary ECTV Infection in the Absence of IFN Function. The WT strain of mice effectively controlled a primary virulent ECTV infection at doses ranging from 100 to 103 pfu (Table 1) with 100% survival. However, mice deficient in one (IFN-α/βR-/- or IFN-γR-/-) or both IFN receptors (IFN-α/β/γR-/-) or in IRF-1 (IRF-1-/-) succumb to infection with doses as low as 1 pfu of virus with 0% survival. Although the mean time to death varies between the KO strains, with IFN-γR-/- animals surviving the longest, it decreases with increasing dose of virus from 100 to 103 pfu (Table 1). Hence, the absence of either type I or type II IFN function resulted in death from a primary ECTV infection.
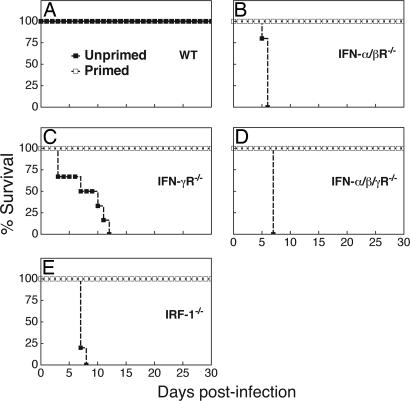
Outcome of a Secondary ECTV Infection in the Absence of IFN Function. To ascertain the role of IFN in a secondary infection, we chose to challenge primed animals with the highest dose of virulent ECTV (103 pfu) used in Table 1. As expected, WT mice survived a virulent ECTV infection with 103 pfu in both unprimed (primary) and primed (secondary) groups (Fig. 1A). Further, as anticipated, mice deficient in IFN-α/βR (Fig. 1B), IFN-γR (Fig. 1C), IFN-α/β/γR (Fig. 1D), or IRF-1 (Fig. 1E) were highly susceptible to primary ECTV infection and exhibited 100% mortality by 6-12 days. Strikingly, and in contrast to the outcome of a primary infection, each one of these gene KO strains was able to survive a virulent secondary infection, with no signs of disease (Fig. 1, open squares).
Fig. 1.
Outcome of primary and secondary ECTV infections in mice lacking IFN function. Groups of five female WT (A), IFN-α/βR-/- (B), IFN-γR-/- (C), IFN-α/β/γR-/- (D), and IRF-1-/- (E) mice were primed i.p. with 105 pfu of avirulent ECTV and 4 weeks later challenged in the hind footpad with 103 pfu of virulent ECTV (□). At the same time, similar age-matched groups of unprimed mice from each strain were infected with 103 pfu of virulent ECTV (▪). Mice were monitored for clinical signs of disease, and survival after challenge was recorded. Data shown are representative of two independent experiments.
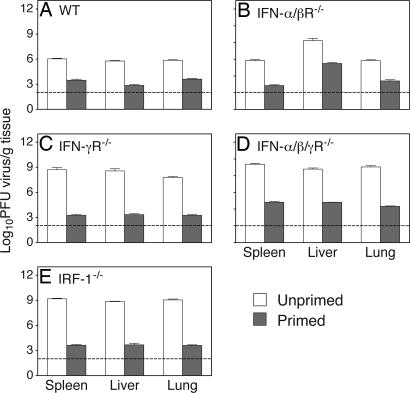
Control of Viral Load in the Absence of IFN Function. To establish that priming allowed recovery from a secondary infection through effective virus control, we determined viral titers in organs from primed ECTV-infected animals and compared these with titers in organs from unprimed animals. Fig. 2 shows that viral titers in most organs from mice lacking one or more IFN functions were several orders of magnitude higher than corresponding titers in organs from WT mice. Notably, viral titers were significantly lower in primed mice, compared with those of unprimed animals of the same strain, for all strains and in all organs tested (Fig. 2). Thus, the effective control of virus in the primed animals deficient in IFN function resulted in survival of the host.
Fig. 2.
Virus load during primary and secondary ECTV infections. Groups of five female WT (A), IFN-α/βR-/- (B), IFN-γR-/- (C), IFN-α/β/γR-/- (D), and IRF-1-/- (E) mice were primed and challenged as in Fig. 1 (shaded column). At the same time, groups of unprimed mice from each strain also were infected as in Fig. 1 (open column). On day 5 after challenge, mice were killed and their organs were collected aseptically for the determination of viral titers, as described in Materials and Methods. The broken line indicates the limit of detection of the assay, which, for these experiments, is 100 pfu. Data shown are mean ± SEM from one of two independent experiments. The differences between primed and unprimed groups for each organ in each strain were analyzed statistically by the Mann-Whitney test and were found to be significant at P < 0.05.
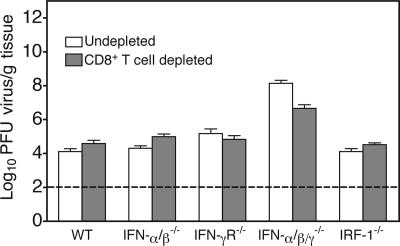
Virus Control in the Absence of Both IFN Function and CD8+ T Cells. Immunological memory and protective immunity against a secondary infection are functions of B and T lymphocyte responses (26). Because CD8+ T cells are known to be critical for recovery from a primary ECTV infection (10), it is possible that this cell subset also contributes to virus control during a secondary infection. To test this, we depleted ECTV-primed WT and KO mice of CD8+ T cells immediately before and after a virulent secondary ECTV infection. The data show that WT and all KO strains of mice are able to control virus load in a secondary infection equally well in the presence or absence of CD8+ T cells (Fig. 3). The infected animals did not exhibit any signs of morbidity in either group for each strain.
Fig. 3.
Effect of CD8+ T cell depletion on virus control during a secondary infection in mice lacking IFN function. Groups of WT, IFN-α/βR-/-, IFN-γR-/-, IFN-α/β/γR-/-, and IRF-1-/- mice were primed as in Fig. 1 and challenged after 4 weeks. Immediately before and after challenge, mice were depleted of CD8+ T cells as described in Materials and Methods. On day 5 after challenge, mice were killed and their organs were collected and used for the determination of viral titers. Data shown here are for lung, as a representative organ, and are mean ± SEM of five individual samples per group. There were no significant differences in virus titers between CD8+ T cell-depleted and nondepleted groups for any strain.
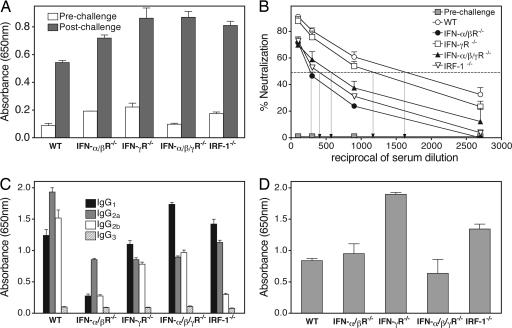
Ab Response in a Secondary ECTV Infection in the Absence of IFN Function. Because virus was controlled effectively in the absence of CD8+ T cells, we therefore investigated the contribution of an antiviral Ab response in recovery from a secondary ECTV infection, in both the presence and the absence of IFN function. Groups of primed mice were bled before and 2 weeks after challenge with virulent ECTV, and sera were assayed for ECTV-specific IgG by ELISA. Fig. 4A shows that WT 129S7 and all KO strains (IFN-α/βR-/-, IFN-γR-/-, IFN-α/β/γR-/-, and IRF-1-/-) produced substantial levels of virus-specific IgG. Further, for each strain, this was significantly higher than the prechallenge levels.
Fig. 4.
Anti-ECTV Ab responses generated during a secondary infection in mice lacking IFN function. Groups of female WT, IFN-α/βR-/-, IFN-γR-/-, IFN-α/β/γR-/-, and IRF-1-/- mice were primed and challenged as in Fig. 1. (A-C) Animals were bled before challenge and 2 weeks after challenge, and serum samples were collected for the following determinations. (A) ECTV-specific IgG for individual animals by ELISA. (B) Neutralizing Ab titers of sera by the plaque-reduction neutralization test, where the neutralizing titer is taken to be the reciprocal of the serum dilution at which 50% of the virus is neutralized (represented by the dotted line). (C) IgG subtype by ELISA as described in Materials and Methods. The prechallenge sera for all strains had undetectable neutralizing activity; therefore, for clarity, only the data for WT group are shown (▪, B). Data shown are mean ± SEM of five individual samples and are from one of two separate animal experiments. (D) In a separate group of animals, CD8+ T cells were depleted before and after challenge as described for Fig. 3. On day 5 after challenge, mice were killed and serum was collected for the determination of anti-ECTV IgG levels. Data shown are mean ± SEM of five individual samples per group.
Next, we determined the virus-neutralizing activity of the Ab in serum from the above experiment. Fig. 4B shows that there is no neutralizing activity in sera, of any mouse strain, before the secondary challenge with virulent ECTV virus. Significantly however, 2 weeks after the challenge, neutralizing Ab was produced in all strains tested. Serum from the WT group had the highest neutralizing titer of ≈1,600. The other strains had neutralizing titers that ranged from 300 in the IFN-α/βR-/-, 400 in the IRF-1-/-, 600 in the IFN-α/β/γR-/-, and 1,200 in the IFN-γR-/- groups (Fig. 4B).
Because IFN can influence the composition of IgG subclasses and this may, in turn, affect the neutralizing activity of the Ab, we measured the virus-specific IgG subclasses levels (Fig. 4C). Serum from WT 129S7 animals contained high levels of IgG1, IgG2a, and IgG2b. Levels of IgG2a were reduced to a similar extent in all of the KO strains in the absence of one or more IFN pathways. Although levels of IgG2b also were reduced in all KO groups, these were most notable in sera from IFN-α/βR-/- and IRF-1-/- mice. In contrast, only the IFN-α/βR-/- group showed considerably reduced levels of IgG1. Finally, levels of IgG3 were low and did not change in any of the groups.
The strong correlation between survival from a secondary ECTV infection and an antiviral Ab response suggested that this component of the immune system plays a significant role in virus control, even in the absence of CD8+ T cells. To test this hypothesis, we measured Ab responses during a virulent secondary virus infection in CD8+ T cell-depleted ECTV-primed WT and KO mice. Fig. 4D shows that WT and KO mice generate normal secondary anti-ECTV IgG responses in the absence of CD8+ T cells that are comparable to responses in mice with CD8+ T cells intact. This observation is consistent with effective virus control in secondary ECTV infection by Ab, with or without CD8+ T cells.
Discussion
Data presented here confirm that control of ECTV in a primary infection is highly dependent on the functions of type I/II IFN. Mice deficient in one or more of these cytokines exhibit 100% mortality to primary ECTV infection. In vivo studies have shown the importance of IFN-α/β and IFN-γ in recovery from ECTV in the genetically resistant strains of mice, such as C57BL/6 and 129 (11-13, 27, 28). ECTV-infected C57BL/6 mice treated with anti-IFN-γ Ab showed 100% mortality within 7 days of infection, with the mean time to death approaching that of the highly susceptible BALB/c or A/J strains (11, 12). The latter strains make little or no IFN-γ, respectively. The importance of type I/II IFN in ECTV infection is further highlighted by the fact that the virus itself encodes secreted receptors for IFN-α/β (14) and IFN-γ (15, 16), which bind to and modulate cytokine function. Many other poxviruses adopt similar strategies to counteract the host IFN response, most notably myxoma virus (19), vaccinia virus (16), and VARV (29).
In contrast to a primary infection, we have shown here that mice lacking type I/II IFN function effectively control virus replication (Fig. 2) and survive a secondary infection with virulent ECTV (Fig. 1). Interestingly, this virus control occurred even in the absence of CD8+ T cells (Fig. 3) and strongly correlated with the generation of a virus-neutralizing Ab response (Fig. 4B). Because the role of type III IFN was not tested in this study, we cannot exclude a role for this class of cytokines in response to a secondary infection.
At least two lines of evidence indicate that CD8+ T cells do not play a role in the recovery of mice from a secondary ECTV infection. First, ECTV-primed WT or KO mice depleted of CD8+ T cells immediately before and after a virulent secondary ECTV challenge generate a normal secondary IgG response (Fig. 4D) and control virus effectively (Fig. 3). Second, with the exception of mice lacking IFN-γR, KO strains deficient in IFN-α/βR, IFN-α/β/γR, or IRF-1 do not mount a measurable virus-specific, primary (day 7 after infection), or secondary (day 5 after challenge) cytotoxic T lymphocyte response (unpublished observations). This finding suggests that the priming of naïve and activation of memory CD8+ T responses in mice lacking IFN-α/βR, IFN-α/β/γR, or IRF-1 is defective. Indeed, it also has been reported that IRF-1-/- mice have reduced numbers, as well as defective CD8+ T cell responses (6). Our findings are significant, given the currently held view about the importance of memory CD8+ T cells in protection against secondary viral infections (30).
Prospective studies have indicated that high levels of neutralizing Ab after vaccination, or after infection in individuals who recovered from smallpox, may be associated with protective immunity (31-33). More recently, it has been shown that serum antiviral Ab levels remained stable up to 75 years after vaccination, whereas antiviral T cell responses declined slowly, with a half-life of up to 15 years (34). Other investigators also have found that B cell memory persists for >50 years after smallpox vaccination and that a robust Ab recall response is elicited upon revaccination (35). Although CD4 and CD8 T lymphocytes may play an important role in a recall response, it should be noted that CD4 T cell memory is maintained for much longer than CD8 memory (36). The persistence of memory CD4 T cells may be important for maintenance of long-term B cell memory and protective recall responses.
Using the mousepox model, we have shown here that virus control and recovery from secondary infection is strongly correlated with the generation of a neutralizing Ab response. In another model of poxvirus infection, macaques immunized with a vaccine strain of vaccinia virus were protected against monkeypox virus challenge with concurrent elevation of both T cell and Ab responses (37). At the time this manuscript was being finalized, an advance online publication by Edghill-Smith et al. (38) showed that in Dryvax (Wyeth Laboratories)-vaccinated macaques, B cell responses are critical for recovery from a high-dose i.v. monkeypox virus challenge. Although the levels of virus-neutralizing Ab were high at the time of challenge, it does support our findings on the critical role for Ab in recovery from a secondary poxvirus infection. The model we have used in the present study affords the advantage that there was no detectable neutralizing Ab present at the time of challenge. As may be the case in the above study (38), our data are not confounded by the possibility that a secondary virus infection is controlled by preexisting neutralizing Ab. Importantly, the dose of virus and route of infection used here more closely resemble a natural infection.
The subclass of IgG generated has a direct effect on the efficiency of virus clearance through its ability to recruit other arms of the immune system, specifically, complement and macrophages. This function of IgG might explain why the subclasses generated after a virulent challenge in mice deficient in IFN function have differing virus-neutralizing activity. Given the ability of IFN-γ to direct the Ab response toward a predominantly IgG2a subclass and IL-4 toward an IgG1 response (39), it is not surprising that, in the absence of IFN-γ function, the secondary ECTV-specific IgG subtype response has a higher contribution from IgG1 in IFN-γR-/-, IFN-α/β/γR-/-, and IRF-1-/- (Fig. 4C) mice, compared with the WT animals. Despite the change in subclass profile, the mice were able to control the infection and fully recover.
ECTV-specific IgG2a concentrations were reduced to similar levels in the absence of different facets of IFN function in primed mice. However, the in vitro neutralizing activity between these groups differed substantially, suggesting that IgG2a alone may not have played a major role in determining the virus-neutralizing activity. In addition, the IgG1 levels in the various KO strains did not correlate with the virus-neutralizing activity. In contrast, the markedly reduced IgG2b levels in the IFN-α/βR-/- and IRF-1-/- mice correlated with the lowest virus-neutralizing activity of sera obtained from these groups. This finding suggested that IgG2b, presumably in combination with IgG2a, plays an important role in determining the neutralizing activity. Importantly, despite the reduction in virus-neutralizing Ab activities when one or more pathways of IFN function were absent, viral titers were still effectively controlled in all of the primed mice, suggesting that the lower neutralizing activity was nevertheless sufficient to control virus.
The Ab response to poxviruses is generated against two forms of infectious particles, the intracellular mature virus and the extracellular enveloped virus. It has been suggested that Ab directed against both these forms is required for maximal protective immunity (40, 41). Although the neutralization assay and the ELISA used in this study detected predominantly intracellular mature virus-specific Ab, it is likely that Ab against both forms of virus are generated. Notwithstanding, we have shown that effective virus control and protection in a secondary infection strongly correlated with the neutralizing Ab response that was measured.
In summary, we have made two pertinent findings in this study. First, IFN function is not necessary for the generation of a secondary neutralizing Ab response. Second, Ab, in the absence of CD8+ T lymphocytes and IFN function, can control virus replication and promote recovery from a secondary infection. These findings have important implications in the engineering of the memory immune response and in vaccine design. These findings also establish that it is feasible to induce protective immunity in the complete absence of IFN function, and hence, it should be possible to vaccinate individuals with defective IFN responses. Efforts to secure safer and more effective vaccines against smallpox that provide broad coverage to include individuals with a variety of immunodeficiencies are of paramount importance.
Acknowledgments
This work was supported by grants from the Howard Hughes Medical Institute (to G.K.) and the National Health and Medical Research Council of Australia (to G.K. and G.C.). G.K. is an International Research Scholar of the Howard Hughes Medical Institute.
Author contributions: V.P., G.C., and G.K. designed research; V.P. and G.K. performed research; and V.P., G.C., and G.K. analyzed data and wrote the paper.
This paper was submitted directly (Track II) to the PNAS office.
Abbreviations: ECTV, ectromelia virus; VARV, variola virus; IRF-1, IFN regulatory factor 1; IFN-α/βR, IFN-α/β receptor; KO, knockout; pfu, plaque-forming units.
References
- 1.Sen, G. C. (2001) Annu. Rev. Microbiol. 55, 255-281. [DOI] [PubMed] [Google Scholar]
- 2.Shtrichman, R. & Samuel, C. E. (2001) Curr. Opin. Microbiol. 4, 251-259. [DOI] [PubMed] [Google Scholar]
- 3.Taniguchi, T. & Takaoka, A. (2002) Curr. Opin. Immunol. 14, 111-116. [DOI] [PubMed] [Google Scholar]
- 4.Salkowski, C. A., Thomas, K. E., Cody, M. J. & Vogel, S. N. (2000) J. Immunol. 165, 3970-3977. [DOI] [PubMed] [Google Scholar]
- 5.Kamijo, R., Harada, H., Matsuyama, T., Bosland, M., Gerecitano, J., Shapiro, D., Le, J., Koh, S. I., Kimura, T., Green, S. J., et al. (1994) Science 263, 1612-1615. [DOI] [PubMed] [Google Scholar]
- 6.Ohteki, T., Maki, C. & Koyasu, S. (2001) J. Immunol. 166, 6509-6513. [DOI] [PubMed] [Google Scholar]
- 7.Duncan, G. S., Mittrucker, H. W., Kagi, D., Matsuyama, T. & Mak, T. W. (1996) J. Exp. Med. 184, 2043-2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lohoff, M., Ferrick, D., Mittrucker, H. W., Duncan, G. S., Bischof, S., Rollinghoff, M. & Mak, T. W. (1997) Immunity 6, 681-689. [DOI] [PubMed] [Google Scholar]
- 9.Karupiah, G., Xie, Q. W., Buller, R. M., Nathan, C., Duarte, C. & MacMicking, J. D. (1993) Science 261, 1445-1448. [DOI] [PubMed] [Google Scholar]
- 10.Karupiah, G., Buller, R. M., Van Rooijen, N., Duarte, C. J. & Chen, J. (1996) J. Virol. 70, 8301-8309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaudhri, G., Panchanathan, V., Buller, R. M., Van Den Eertwegh, A. J., Claassen, E., Zhou, J., De Chazal, R., Laman, J. D. & Karupiah, G. (2004) Proc. Natl. Acad. Sci. USA 101, 9057-9062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karupiah, G., Fredrickson, T. N., Holmes, K. L., Khairallah, L. H. & Buller, R. M. (1993) J. Virol. 67, 4214-4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramshaw, I. A., Ramsay, A. J., Karupiah, G., Rolph, M. S., Mahalingam, S. & Ruby, J. C. (1997) Immunol. Rev. 159, 119-135. [DOI] [PubMed] [Google Scholar]
- 14.Smith, V. P. & Alcami, A. (2002) J. Virol. 76, 1124-1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mossman, K., Upton, C., Buller, R. M. & McFadden, G. (1995) Virology 208, 762-769. [DOI] [PubMed] [Google Scholar]
- 16.Alcami, A. & Smith, G. L. (1996) Comp. Immunol. Microbiol. Infect. Dis. 19, 305-317. [DOI] [PubMed] [Google Scholar]
- 17.Bartlett, N. W., Buttigieg, K., Kotenko, S. V. & Smith, G. L. (2005) J. Gen. Virol. 86, 1589-1596. [DOI] [PubMed] [Google Scholar]
- 18.Sypulowa, A., Zielinska-Jenczylik, J. & Skurska, Z. (1972) Arch. Immunol. Ther. Exp. (Warsz.) 20, 837-840. [PubMed] [Google Scholar]
- 19.Upton, C., Mossman, K. & McFadden, G. (1992) Science 258, 1369-1372. [DOI] [PubMed] [Google Scholar]
- 20.Scalzo, A. A., Farrell, H. E. & Karupiah, G. (2000) Methods Mol. Biol. 121, 163-177. [DOI] [PubMed] [Google Scholar]
- 21.Jackson, R. J., Maguire, D. J., Hinds, L. A. & Ramshaw, I. A. (1998) Biol. Reprod. 58, 152-159. [DOI] [PubMed] [Google Scholar]
- 22.Muller, U., Steinhoff, U., Reis, L. F., Hemmi, S., Pavlovic, J., Zinkernagel, R. M. & Aguet, M. (1994) Science 264, 1918-1921. [DOI] [PubMed] [Google Scholar]
- 23.Huang, S., Hendriks, W., Althage, A., Hemmi, S., Bluethmann, H., Kamijo, R., Vilcek, J., Zinkernagel, R. M. & Aguet, M. (1993) Science 259, 1742-1745. [DOI] [PubMed] [Google Scholar]
- 24.Reis, L. F., Ruffner, H., Stark, G., Aguet, M. & Weissmann, C. (1994) EMBO J. 13, 4798-4806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez, J. F., Janeczko, R. & Esteban, M. (1985) J. Virol. 56, 482-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Welsh, R. M., Selin, L. K. & Szomolanyi-Tsuda, E. (2004) Annu. Rev. Immunol. 22, 711-743. [DOI] [PubMed] [Google Scholar]
- 27.Jacoby, R. O., Bhatt, P. N. & Brownstein, D. G. (1989) Arch. Virol. 108, 49-58. [DOI] [PubMed] [Google Scholar]
- 28.Karupiah, G. (1998) Vet. Immunol. Immunopathol. 63, 105-109. [DOI] [PubMed] [Google Scholar]
- 29.Shchelkunov, S. N., Blinov, V. M. & Sandakhchiev, L. S. (1993) FEBS Lett. 319, 80-83. [DOI] [PubMed] [Google Scholar]
- 30.Wherry, E. J. & Ahmed, R. (2004) J. Virol. 78, 5535-5545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Downie, A. W. & McCarthy, K. (1958) J. Hyg. 56, 479-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mack, T. M., Noble, J., Jr., & Thomas, D. B. (1972) Am. J. Trop. Med. Hyg. 21, 214-218. [DOI] [PubMed] [Google Scholar]
- 33.Sarkar, J. K., Mitra, A. C. & Chakravarty, M. S. (1972) Trans. R. Soc. Trop. Med. Hyg. 66, 789-792. [DOI] [PubMed] [Google Scholar]
- 34.Hammarlund, E., Lewis, M. W., Hansen, S. G., Strelow, L. I., Nelson, J. A., Sexton, G. J., Hanifin, J. M. & Slifka, M. K. (2003) Nat. Med. 8, 1131-1137. [DOI] [PubMed] [Google Scholar]
- 35.Crotty, S., Felgner, P., Davies, H., Glidewell, J., Villarreal, L. & Ahmed, R. (2003) J. Immunol. 171, 4969-4973. [DOI] [PubMed] [Google Scholar]
- 36.Amara, R. R., Nigam, P., Sharma, S., Liu, J. & Bostik, V. (2004) J. Virol. 78, 3811-3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Earl, P. L., Americo, J. L., Wyatt, L. S., Eller, L. A., Whitbeck, J. C., Cohen, G. H., Eisenberg, R. J., Hartmann, C. J., Jackson, D. L., Kulesh, D. A., et al. (2004) Nature 428, 182-185. [DOI] [PubMed] [Google Scholar]
- 38.Edghill-Smith, Y., Golding, H., Manischewitz, J., King, L. R., Scott, D., Bray, M., Nalca, A., Hooper, J. W., Whitehouse, C. A., Schmitz, J. E., et al. (2005) Nat. Med. 11, 740-747. [DOI] [PubMed] [Google Scholar]
- 39.Stavnezer, J. (1996) Adv. Immunol. 61, 79-146. [DOI] [PubMed] [Google Scholar]
- 40.Law, M., Putz, M. M. & Smith, G. L. (2005) J. Gen. Virol. 86, 991-1000. [DOI] [PubMed] [Google Scholar]
- 41.Viner, K. M. & Isaacs, S. N. (2005) Microbes Infect. 7, 579-583. [DOI] [PubMed] [Google Scholar]