Abstract
If H5N1 influenza viruses become transmissible among humans, vaccination will offer the most effective option to limit their spread. Two human vaccine candidates recently generated by reverse genetics are based on antigenically different hemagglutinin (HA) glycoproteins derived from the A/HK/213/03 (H5N1) and A/Vietnam/1203/04 (H5N1) viruses. Their HA1 amino acid sequences differ at 10 positions, one of which (N154) introduces a potential glycosylation site in A/Vietnam/1203/04 (H5N1). To assess the impact of five amino acids in the putative antigenic sites on immunogenicity and immune protection, we generated a series of whole-virus vaccines that differed only in one or two HA amino acids. Sera from ferrets vaccinated with these inactivated preparations had high virus neutralization titers, but their hemagglutination inhibition (HI) titers were usually low. Interestingly, a recombinant virus in which the HA amino acid S223 (characteristic of 2004 viruses) was converted to N223 (as in A/HK/213/03) resulted in higher HI titers. This observation indicates that specific HA residues, such as N223, increase the sensitivity of the HI assay by altering receptor specificity and/or antibody-antigen binding. Ferrets vaccinated with mutant vaccine viruses were protected against lethal challenge with wild-type A/Vietnam/1203/04 virus. Our results suggest that inclusion of the N223 residue in the HA glycoproteins of diagnostic reference viruses may facilitate the evaluation of vaccine efficacy in humans.
Keywords: reverse genetics, receptor specificity
The recent outbreaks of highly pathogenic H5N1 influenza A viruses in poultry and humans across nine countries in Asia, from Japan in the north to Indonesia in the south, are unprecedented. In 2003, the H5N1 viruses in Southeast Asia comprised different cocirculating genotypes, but in 2004, a single genotype (the “Z-genotype”) became dominant (1). The current evidence suggests that the fatal human cases resulted from direct transmission of virus from birds to humans. The virus also caused disease in cats and was transmitted from cat to cat in experiments (2). This and other evidence of the changing host range and widespread distribution of this virus raised concern that H5N1 viruses may acquire the characteristics that allow transmission from human to human. Humans would have no immunity to such new H5N1 viruses, which could cause catastrophic pandemic influenza (3).
Readily available vaccines would provide the most effective tool against pandemic influenza. After the 1997 H5N1 outbreak in Hong Kong, vaccines produced by two different approaches were tested in humans. Conventional subunit H5 vaccine produced from A/duck/Singapore/3/97 (4) was poorly immunogenic in humans, even against antigenically closely related strains and after multiple vaccination (5). The use of the adjuvant MF59 increased the antibody titer of this H5 vaccine (6). Vaccination with inactivated “split” vaccine derived from nonpathogenic A/duck/HK/836/80 (H3N1) virus and the modified H5 hemagglutinin from A/HK/156/97 (H5N1) virus induced barely detectable titers of neutralizing antibodies in mice (7). Thus, although these H5N1 vaccines were well tolerated, they appeared to be poorly immunogenic.
Serum antibody titers, mainly those determined by hemagglutination inhibition (HI) and virus neutralization assays, are the accepted surrogate measures of immune protection. We used reverse genetics to dissect the antigenic features of the HAs of the H5N1 viruses isolated in 2003 and 2004. Ferrets are considered the best model for evaluating the potential human immune response to influenza virus infection and vaccination. We vaccinated ferrets with inactivated H5 vaccines derived from virus isolated from a fatally infected human patient (A/Vietnam/1203/04) and investigated the contribution of single H5 amino acids to the induction, degree of protection, and detectability of the immune response in the ferret model.
Materials and Methods
Virus Strains and Generation of Recombinant Viruses. Highly pathogenic H5N1 viruses were obtained from World Health Organization-collaborating laboratories in Asia. All work with these viruses was performed in BL3+ facilities at St. Jude Children's Research Hospital. Recombinant viruses rendered nonpathogenic by modification of H5 HA at the cleavage site were generated by DNA transfection as described in ref. 8. Point mutations were inserted into the HA during PCR by using the QuikChange Site-Directed Mutagenesis Kit (Stratagene) and a set of H5 HA-specific primers. Reassortant viruses contained the HA gene or the HA and neuraminidase genes from H5N1 viruses in the genetic background of A/PR/8/34 (H1N1) virus (see Table 1 for viruses generated for this study and their abbreviated names). Allantoic fluid harvested after a single passage in embryonated chicken eggs was frozen at -80°C and used in experiments. The HA genes of the recombinant viruses were amplified by RT-PCR and sequenced to verify that only the designated mutations were present.
Table 1. Recombinant H5-PR/8/34 viruses generated for use in this study.
| Recombinant virus
|
Amino acid position in HA1
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Full name | Abbreviation* | 36 | 83 | 86 | 120 | 155 | 156 | 189 | 212 | 223 | 263 |
| A/HK/213/03 ΔH5N1 × PR/8/34 | ΔH5N1/03 | T | A | A | N | N | A | R | K | N | A |
| A/Vietnam/1203/04 ΔH5N1 × PR/8/34 | ΔH5N1/04 | K | T | V | S | S | T | K | R | S | T |
| A/Vietnam/1203/04 ΔH5 × PR/8/34 | ΔH5/04 | K | T | V | S | S | T | K | R | S | T |
| A/Vietnam/1203/04 ΔH5S155→N, T156→A × PR/8/34 | ΔH5S155→N, T156→A/04 | T | A | V | S | N | A | K | R | S | T |
| A/Vietnam/1203/04 ΔH5S120→N × PR/8/34 | ΔH5S120→N/04 | T | A | V | N | S | T | K | R | S | T |
| A/Vietnam/1203/04 ΔH5R212→K × PR/8/34 | ΔH5R212→K/04 | T | A | V | S | S | T | K | K | S | T |
| A/Vietnam/1203/04 ΔH5S223→N × PR/8/34 | ΔH5S223→N/04 | T | A | A | S | S | T | K | R | N | A |
| A/Vietnam/1203/04 ΔH5S120→N, S155→N, T156→A × PR/8/34 | ΔH5S120→N, S155→N, T156→A/04 | T | A | A | N | N | A | K | R | S | A |
| A/HK/213/03 ΔH5N223→S × PR/8/34 | ΔH5N223→S/03 | T | A | A | N | N | A | R | K | S | A |
| A/duck/Singapore/3/97 H5 × PR/8/34 | H5/97† | T | D | V | S | N | A | K | E | S | A |
| A/duck/Singapore/3/97 H5S223→N × PR/8/34 | H5S223→N/97 | T | D | V | S | N | A | K | E | N | A |
The amino acids inserted in the HA1 of recombinant H5 viruses are shown in bold.
Δ multibasic amino acids in the H5 were removed by genetic engineering.
Wild-type A/duck/Singapore/3/97 does not have multibasic amino acids.
Preparation of Inactivated Virus for Immunization. Viruses were propagated in the allantoic cavities of 10-day-old embryonated chicken eggs at 35°C for 48 h. Vaccine viruses were inactivated, concentrated, and purified as described in refs. 9 and 10.
Standardization of HA Protein Content of Vaccines. The single radial immunodiffusion technique was used to standardize ΔH5N1/03 (10). The remaining recombinant viruses were separated by 12% SDS/PAGE, the stained gels were analyzed by densitometry on the FUJIFILM Luminescent Image Analyzer LAS-1000plus, and HA was quantified by comparison with a reference protein preparation.
Immunization of Ferrets. Male and female outbred ferrets were obtained through a special breeding program of the Animal Resources Center at St. Jude Children's Research Hospital. Animals were 3-5 months old and were seronegative by HI tests for exposure to currently circulating influenza A H1N1, H3N2, and H5N1 viruses and influenza B viruses. Groups of three ferrets were vaccinated by intramuscular injection of 250 μl of sterile PBS containing 7 μg of HA from inactivated purified viruses. Three control animals were injected with 250 μl of sterile PBS alone. On day 21 after vaccination, serum was collected and a second intramuscular injection of 7 μg of HA was given. Two weeks later, serum was again collected and animals were inoculated with challenge virus.
Challenge Infection of Ferrets. Vaccinated and control animals were inoculated intranasally as previously described with 106 50% egg infective doses (eID50) of A/Vietnam/1203/04 virus (11). Clinical signs of infection, body weight, and temperature were monitored daily for 2 weeks. Ferrets that showed signs of severe disease were killed. To estimate the postinfective immune response, additional groups of ferrets were inoculated with 106 eID50 of the human and avian H5N1 isolates A/HK/213/03, A/Vietnam/3046/04, A/Vietnam/3062/04, A/chicken/Vietnam/39/04, and A/falcon/HK/D0028/04. Sera were collected from the animals on day 28 after inoculation.
Determination of Virus Titers in Upper Respiratory Tract. Specimens were obtained by nasal lavage on days 3, 5, and 7 by methods described in ref. 11. Virus in the samples was titrated in 10-day-old embryonated chicken eggs and expressed as log10 eID50 per 0.1 ml.
mAbs to H5 Hemagglutinin. mAbs CP24, CP46, CP58, and 406/7 to the HA of A/chicken/Pennsylvania/1370/83 (H5N3) virus were produced in the Infectious Diseases Department of St. Jude Children's Research Hospital. mAb VN04-6 to the HA of A/Vietnam/1203/04 virus and mAb HK03-3 to the HA of A/HK/213/03 virus were prepared by a modification of the method described by Kohler and Milstein (12, 13).
Serologic Tests. Sera collected from ferrets were treated overnight with Vibrio cholerae receptor-destroying enzyme (Denka-Seiken, Tokyo), heat inactivated at 56°C for 30 min, and adsorbed with a 0.5% suspension of chicken erythrocytes. Standard HI and virus neutralization tests in Madin Darby canine kidney cells were performed as described in refs. 14 and 15. Four hemagglutinating units (HAUs) of virus were used in each HI assay and 100 50% tissue culture infective doses were used in each neutralization assay.
Results
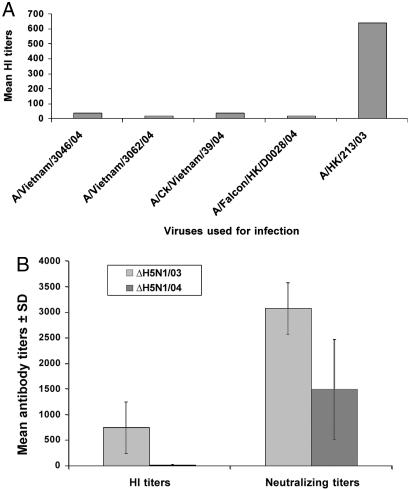
Serum Antibody Titers of Inoculated Ferrets. To compare the immunogenicity of the 2003 influenza viruses of Z genotype, which became dominant in 2004, with that of the 2004 viruses, we inoculated ferrets with the H5N1 virus isolated from a fatal human case (A/HK/213/03) (16) and with four H5N1 viruses isolated from humans, chickens, and falcons in 2004 (Fig. 1A). Serum antibodies were titrated by HI assay with challenge viruses 28 days after inoculation. A/HK/213/03 virus induced high antibody titers (1:640-1:1,280), whereas the four 2004 strains induced very low HI titers (1:20-1:40).
Fig. 1.
HI antibody titers in ferrets inoculated with H5N1 influenza viruses isolated in 2003 and 2004 (A) and HI and virus neutralizing titers in ferrets immunized with ΔH5N1/03 and ΔH5N1/04 viruses (B). (A) Sera were collected on day 28 after inoculation with 106 eID50 of H5N1 viruses and titrated against 4 HAUs of homologous virus. Data are representative values from two or four sera. (B) Sera were collected from ferrets vaccinated twice with 7 μg of HA (see Materials and Methods) of ΔH5N1/03 and ΔH5N1/04 viruses and titrated against 4 HAUs and 100 tissue culture 50% infective dose of homologous virus, respectively.
Virus Neutralization and Sequence Analysis of HA. The relatively low HI titers to the 2004 H5N1 viruses could have been the result of virus-induced general immune suppression. However, the results of vaccination with ΔH5N1-A/PR/8/34 (6 + 2) vaccines that included the HA and neuraminidase of A/HK/213/03 and A/Vietnam/1203/04 indicated that differences in the H5 could be a major contributor to this effect (Fig. 1B). Vaccination with two separate 7-μg doses of ΔH5N1/03 vaccine induced high levels of serum antibodies detectable in both HI and virus neutralization tests (Fig. 1B). After identical vaccination with ΔH5N1/04, very low (≈1:20) titers were detected in the HI test, whereas neutralizing titers were much higher (about half that induced by ΔH5N1/03). Previous studies found that inactivated vaccine derived from A/duck/Singapore/3/97 (H5N3) induced little or no detectable serum antibody (4, 6). Taken together, these results indicate that some H5 isolates may have unusual immunogenic and/or antigenic properties. Alignment of the H5 amino acid sequences revealed that the HAs of A/HK/213/03 and A/Vietnam/1203/04 viruses differ in 10 amino acids in the HA1 region (Table 2). A/Vietnam/1203/04 virus has a potential glycosylation site at asparagine N154 (N*154-S155-T156, N-X-S/T, X≠ P). Sequence comparison revealed three amino acids (S120, K189, and S223) that were present in all of the 2004 viruses but were not present in A/HK/213/03. K212 was characteristic for A/Vietnam/1203/04 virus.
Table 2. Sequence differences in the HA1 protein of H5N1 influenza viruses.
| Amino acid position in HA1
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Virus | 36 | 83 | 86 | 120 | 155 | 156 | 189 | 212 | 223 | 263 |
| A/HK/213/03 | T | A | A | N | N | A | R | K | N | A |
| A/Vietnam/1203/04 | K | T | V | S | S | T | K | R | S | T |
| A/Vietnam/3046/04 | T | A | V | S | S | T | K | R | S | T |
| A/Vietnam/3062/04 | T | A | V | S | S | T | K | R | S | T |
| A/chicken/Vietnam/39/04 | T | A | V | S | S | T | K | R | S | T |
| A/falcon/HK-D0028/04 | T | A | A | S | S | A | K | K | S | A |
| A/duck/Singapore/3/97 | T | D | V | S | N | A | K | E | S | A |
| A/HK/156/97 | T | A | A | S | S | A | K | E | S | T |
Generation and Antigenic Characterization of Recombinant ΔH5-A/PR/8/34 Viruses. To test the impact of the identified amino acids on immunogenicity and protection against virus challenge, we used the 8-plasmid reverse genetics system to generate recombinant viruses with seven gene segments of A/PR/8/34 and the HA gene segment of A/Vietnam/1203/04, containing single point mutations (8). The amino acid change was verified by sequencing the HA segment of the recombinant viruses (Table 1). To evaluate the antigenic properties and diversity of the recombinant HAs, we performed HI assays with a panel of six anti-HA monoclonal antibodies (Table 3). Five mAbs reacted at relatively high titers with the ΔH5N1/03 virus, but only three reacted with ΔH5/04 HA. The reactivity patterns of ΔH5S155→N, T156→A/04, ΔH5S120→N/04, and ΔH5R212→K/04 viruses were similar, in general, to that of ΔH5/04 virus. The reactions of ΔH5S120→N, S155→N, T156→A/04 virus were similar to those of ΔH5N1/03 virus. Four mAbs recognized ΔH5/04 HA with mutation S223→N(ΔH5S223→N/04). The reverse mutation N223→S in the HA of the 2003 virus (ΔH5N223→S/03) resulted in significantly decreased HI titers or the loss of recognition by mAbs.
Table 3. H1 analysis of ΔH5 recombinant viruses with anti-H5 monoclonal antibodies.
| Monoclonal antibodies to H5 (H1 titers)
|
||||||
|---|---|---|---|---|---|---|
| Virus | VN04-6* | HK03-3† | CP24‡ | CP46‡ | CP58‡ | 406/7‡ |
| ΔH5N1/03 | 51,200 | 6,400 | 1,600 | 100 | 1,600 | 800 |
| ΔH5/04 | 12,800 | <100 | 800 | <100 | 1,600 | <100 |
| ΔH5S155→N, T156→A/04 | 3,200 | <100 | 800 | <100 | 800 | 100 |
| ΔH5S120→N/04 | 12,800 | 200 | 800 | <100 | 1,600 | <100 |
| ΔH5R212→K/04 | 12,800 | 100 | 1,600 | <100 | 6,400 | <100 |
| ΔH5S223→N/04 | 51,200 | 3,200 | 12,800 | <100 | 25,600 | <100 |
| ΔH5S120→N, S155→N, T156→A/04 | 12,800 | 1,600 | 3,200 | <100 | 1,600 | 200 |
| ΔH5N223→S/03 | 12,800 | 800 | ≤100 | <100 | 200 | ≤100 |
H1 tests were performed in microtiter plates with 0.5% chicken RBCs. Titers are the reciprocal lowest dilutions of mAbs that inhibited hemagglutination caused by 4 HAUs of virus.
Anti-HA mAb to A/Vietnam/1203/04 virus.
Anti-HA mAb to A/HK/213/03 virus.
Anti-HA mAb to A/chicken/Pennsylvania/1370/83 virus.
Another interesting observation was obtained in an HA test with chicken and horse red blood cells (RBCs). Interestingly, recombinant ΔH5S223→N/04 virus was less able to agglutinate 1% horse RBCs but it agglutinated chicken RBCs to a high titer (1:1,024). None of the remaining recombinant viruses differed in their reaction to chicken and horse RBCs to the same extent (data not shown).
Vaccination of Ferrets with H5-Mutant Recombinant Viruses. We assessed the immunogenicity and protective efficacy of the inactivated vaccines by vaccinating groups of three ferrets by intramuscular injection with preparations of ΔH5N1/04, ΔH5/04, ΔH5S155→N, T156→A/04, ΔH5S120→N/04, and ΔH5S223→N/04 virus standardized for HA content. After receiving two injections of 7 μg of HA, each animal was inoculated with A/Vietnam/1203/04 (H5N1) as described in Materials and Methods.
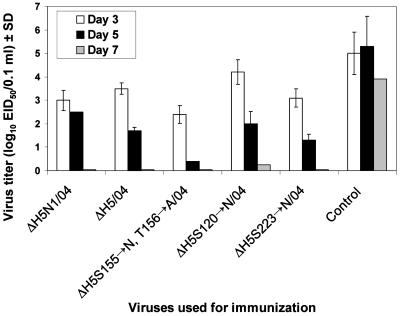
Nasal washes of all vaccinated animals showed virus titers of 2.5-4.5 log10 eID50 on day 3, 0.5-2.5 log10 eID50 on day 5, and 0.25 log10 eID50 or less on day 7 (Fig. 2). Unvaccinated ferrets had a mean titer of 4.0 log10 eID50 1 week after infection. Two of the three control ferrets developed signs of severe disease (massive weight loss and paralysis) and were euthanized and one died of infection. Only one vaccinated ferret became seriously ill. This ferret, vaccinated with ΔH5S120→N/04 virus, showed severe neurological signs and was euthanized on day 7 after inoculation. This ferret had shown severe viral conjunctivitis on day 4 after inoculation, and subsequent virus spread to the brain. It is likely that the virus was transferred to the eyes during the nasal lavage on day 3 and that rapid neuronal spreading to the brain caused encephalitis. The remaining vaccinated ferrets demonstrated decreased activity, loss of body weight, and increased body temperature during the first 3 days after virus challenge. These signs disappeared by day 5, and all animals recovered rapidly. Thus, all vaccine viruses tested protected ferrets from lethal challenge with A/Vietnam/1203/04. Vaccination decreased viral titers in the upper respiratory tract and decreased the duration of virus shedding.
Fig. 2.
Virus titers in nasal washes of vaccinated and control ferrets after challenge with A/Vietnam/1203/04 (H5N1). Ferrets vaccinated with ΔH5N1/04 or ΔH5/04 recombinant viruses were inoculated intranasally with 106 eID50 of A/Vietnam/1203/04 virus. Titers are the mean values (log10 eID50/0.1 ml) ± SD determined in the nasal washes of three ferrets.
HI and Neutralization Tests of the Immunogenicity of Recombinant ΔH5-A/PR/8/34 Viruses. Serum from vaccinated ferrets was tested against the recombinant viruses in HI and virus neutralization assays (Tables 4 and 5, respectively). Sera from ferrets vaccinated with the wild-type single-gene reassortant virus (ΔH5/04, reference virus) produced HI titers of 1:20. The construct in which the glycosylation site was removed (ΔH5S155→N; T156→A/04) induced HI titers of 1:10-1:20. Mutant ΔH5 HA S120→N/04 resulted in HI titers of 1:20-1:80. In contrast, vaccination with ΔH5S223→N/04 resulted in an HI titer of 1:640, and the other immune sera tested reacted with ΔH5S223→N/04 virus at high HI titers (1:160 to 1:320). Thus, although the vaccination induced protective immunity, the levels of detectable antibody were different.
Table 4. Immunogenicity of A/Vietnam/1203/04 ΔH5 HA recombinant viruses in ferrets.
| HI titer of sera after immunization with:
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virus | ΔH5/04 | ΔH5S155→N, T156→A/04 | ΔH5S120→N/04 | ΔH5S223→N/04 | ||||||||
| ΔH5N1/03 | 20 | 20 | 10 | 160 | 80 | 160 | 20 | 20 | 10 | 20 | 10 | 10 |
| ΔH5/04 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 |
| ΔH5S155→N, T156→A/04 | 20 | 10 | 20 | |||||||||
| ΔH5S120→N/04 | 80 | 80 | 20 | |||||||||
| ΔH5S223→N/04 | 160 | 320 | 320 | 160 | 320 | 160 | 320 | 320 | 320 | 640 | 640 | 640 |
Eleven-week-old influenza-seronegative ferrets were vaccinated twice at 3-week intervals by intramuscular injection of inactivated, purified, and concentrated virus preparation containing 7 μg of HA in 250 μl of PBS. Data are the HI titers from three ferrets are presented individually. HI tests used 0.5% chicken RBCs. Homologous titers are underlined.
Table 5. Virus-neutralization titers of ferret sera after vaccination with viruses containing the modified HA of A/Vietnam/1203/04 virus.
| Neutralizing antibody titers after immunization with:
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Virus | ΔH5N1/04 | ΔH5/04 | ΔH5S155→N, T156→A/04 | ΔH5S223→N/04 | Mock | ||||||||
| ΔH5N1/03 | 1,280 | 1,280 | 320 | 640 | 320 | 640 | 1,280 | 1,280 | 320 | 640 | 640 | 640 | <80 |
| ΔH5N1/04 | 2,560 | 1,280 | 640 | 1,280 | 640 | 640 | 1,280 | 1,280 | 640 | 640 | 1,280 | 1,280 | <80 |
| ΔH5/04 | 1,280 | 1,280 | 640 | 1,280 | 640 | 640 | 1,280 | 1,280 | 640 | 640 | 1,280 | 1,280 | <80 |
| ΔH5S155→N, T156→A/04 | 1,280 | 1,280 | 640 | 1,280 | 640 | 640 | 1,280 | 1,280 | 640 | 1,280 | 1,280 | 1,280 | <80 |
| ΔH5S223→N/04 | 1,280 | 1,280 | 1,280 | 1,280 | 1,280 | 640 | 1,280 | 1,280 | 320 | 1,280 | 1,280 | 1,280 | <80 |
| ΔH5S223→NN1/04 | 1,280 | 1,280 | 640 | 1,280 | 640 | 640 | 1,280 | 1,280 | 640 | 1,280 | 1,280 | 1,280 | <80 |
Neutralization assay was performed in MDCK cells. Titers are the reciprocal lowest dilutions of sera that completely inhibited 100 TCID50 of virus. Homologous titers are underlined. Values are the neutralizing titers from three ferrets presented individually.
All ΔH5/04 viruses produced high titers of virus-neutralizing antibodies after vaccination (1:320-1:1,280) (Table 5). No substantial differences were observed between homologous and heterologous neutralizing titers. Therefore, the differences observed between the antisera in recognition of the HA did not reflect the ability of the antibodies to neutralize virus.
To further evaluate the reactivity of the recombinant viruses, we used HI assays to test hyperimmune mouse and chicken serum obtained after vaccination with the ΔH5N1/03 and A/HK/213/03 viruses against recombinant viruses with altered HAs (Table 6). The mean HI titers to homologous ΔH5N1/03 virus were 1:2,560. HI titers to ΔH5/04 were 1:160. HI titers against recombinant ΔH5S223→N/04 virus were at least twice the titers against the other mutants.
Table 6. HI testing of antisera to 2003 H5N1 against mutant viruses.
| Polyclonal antiserum to:
|
||
|---|---|---|
| Virus | Vaccine ΔH5N1/03 | A/HK/213/03 (H5N1) |
| ΔH5N1/03 | 2,560 | 2,560 |
| ΔH5/04 | 160 | 160 |
| ΔH5S155→N, T156→A | 80 | 320 |
| ΔH5S120→N/04 | 320 | 320 |
| ΔH5S223→N/04 | 1,280 | 640 |
HI test was performed in microtiter plates with 0.5% chicken RBCs (14). Titers are the reciprocal lowest dilutions of sera that inhibited hemagglutination caused by 4 HAU of virus.
To obtain additional information about the contribution of the amino acid at position 223 to serological reactivity, we generated a recombinant virus in which the H5 was derived from A/HK/213/03, with only the N223→S point mutation (Table 1). This recombinant ΔH5N223→S/03 virus had lower HI titers in chicken and horse RBCs than did the ΔH5N1/03 virus. To further characterize the impact of amino acid 223 on antigen-antibody recognition, we generated recombinant viruses that contained wild-type HA and mutated S223→NHAfromA/duck/Singapore/3/97 (see Table 1). These viruses were tested by HI assay against a panel of anti-H5 antisera and mAbs (Table 7). The S223→N substitution in the HA dramatically increased the HI titers (by a factor of 4 or more). However, this mutation did not significantly alter the reactivity pattern of A/duck/Singapore/3/97 HA, especially in the reactions with mAbs: neither the original nor the mutant HA reacted with mAbs HK03-3 and CP46, and both reacted at a low titer with CP46 (Table 7). These results demonstrate that the S223→N substitution in HA increases the sensitivity of the HI assay.
Table 7. Antigenic analysis of H5/97 and H5S223→N/97 viruses with polyclonal and monoclonal antibodies.
| HI titer of polyclonal antisera
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A/ck/Hida lgo/94
|
A/HK/156/97
|
A/Gs/HK/4 97-4/97
|
A/ck/HK/YU2 2/02
|
A/HK/213/03
|
HI titer of mAbs
|
|||||||
| Virus | ΔH5/03 | VN04-6* | HK03-3† | CP58‡ | CP24‡ | CP46‡ | CP406/7‡ | |||||
| ΔH5/03 | 20 | 320 | 5,120 | 12,800 | 160 | 5,120 | 25,600 | 6,400 | 1,600 | 12,800 | <100 | 1,600 |
| H5/97 | 40 | 640 | 640 | 320 | <10 | 10 | 3,200 | <100 | 3,200 | 1,600 | <100 | 3,200 |
| H5S223→N/97 | 320 | 10,240 | 10,240 | 2,560 | 80 | 1,280 | 25,600 | <100 | 25,600 | 51,200 | 200 | 25,600 |
HI test was performed in microtiter plates with 0.5% chicken RBCs (14). Titers are the reciprocal lowest dilutions of sera that inhibited hemagglutination caused by 4 HAU of virus.
Anti-HA mAb to A/Vietnam/1203/04 virus.
Anti-HA mAb to A/HK/213/03 virus.
Anti-HA mAb to A/chicken/Pennsylvania/1370/83 virus.
Discussion
The H5N1 viruses isolated in 2004 had antigenic properties different from those of the previous isolates and possessed 10 amino acids in the HA1 region that differed from those in A/HK/213/03 virus. Therefore, the World Health Organization-collaborating laboratories recommended that a new reassortant A/PR/8/34 virus with the HA from A/Vietnam/1203/04 (H5N1) be generated by reverse genetics for vaccine studies. In this study, most ferrets vaccinated with A/PR/8/34 single-gene reassortants that differed only in their H5s were protected against a lethal challenge with A/Vietnam/1203/04 virus. These results on cross-protection extend those of previous studies that used a mouse model (17).
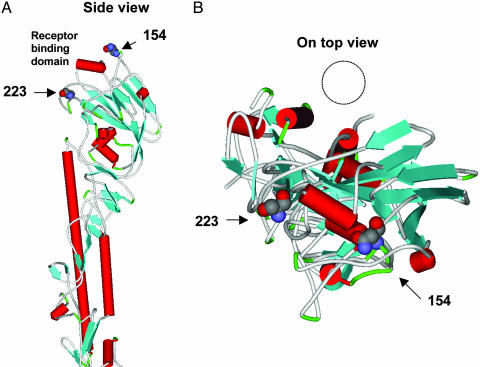
A/Vietnam/1203/04 virus had a previously uncharacterized potential glycosylation site that might mask epitopes of the H5 HA from the previous vaccine candidate. The recombinant virus in which this glycosylation site at the top of the H5 (Fig. 3) was changed completely protected ferrets against virus challenge. These findings are consistent with those of a previous study in BALB/c mice vaccinated with an H5-DNA vaccine derived from the 1997 H5N1 viruses (19). Mice vaccinated with HAs derived from A/HK/156/97 containing single point mutations in the H5 were protected from lethal challenge. Thus, we conclude that the presence or absence of carbohydrate residues at position 154 of H5 is not crucial to the protective efficacy of H5 vaccines.
Fig. 3.
Location of amino acid at positions 154 and 223 in the 3D structure of H5 HA. (A) The amino acids in the 3D structure of the HA of A/duck/Singapore/3/97 (H5N3) virus (18). The glycosylation site at position 154 is located at the top of the HA molecule. (B) The circle represents the interface between the monomer shown and two other monomers (data not shown) in the trimeric HA. Amino acid at position 223 is located at the surface of the trimer.
In several independent experiments, we found that vaccine viruses containing H5s from 2004 elicited low detectable HI antibody titers. This effect was observed after both intranasal inoculation and intramuscular vaccination. Interestingly, unlike the other three amino acid substitutions, assays using a virus with the S223→N substitution resulted in higher HI titers. The epitopes reported to be important for recognition of H5 HA by mAbs (12) did not include position 223. Alignment of all published H5N1 virus HA sequences shows that all recent isolates in Asia have S223. Some avian H5N1 viruses isolated in Central and South America have a basic amino acid, R223. The basic amino acid N223 is found only in the HA of the human isolate A/HK/213/03 and is located in the 220-loop of the receptor binding domain between Q222 and G224 (Fig. 3). The experimental evidence suggests that the higher HI titers reflect a change in receptor specificity. Indeed, Q222 and G224 bind directly to the sialic acid receptor. Amino acids in the 220 loop or adjacent are important for the conformation of the receptor binding pocket (18). Possibly, substitution of S223 to N223 results in conformational changes and altered receptor specificity. This finding is consistent with the fact that ΔH5S223→N/04 virus did not agglutinate horse RBCs, whose sialic acid receptors have the N-glycosyl sialic acid α 2,3 linkage (20). The sialic acid receptors on chicken RBCs have α 2,3 and α 2,6 linkages. Thus, if ΔH5S223→N/04 virus binds only to sialic acid receptors with α 2,6 linkage, the resultant lower binding on chicken RBCs would require a smaller quantity of antibody to inhibit hemagglutination.
Within the last five years, plasmid-only systems have become powerful tools for generating high-yield influenza viruses of different serotypes (8, 10, 21, 22). To create a new vaccine representing the antigens of a new serotype, a combination of factors must be optimized, such as number of doses, formulation with or without adjuvants, dose range, antigenicity, and antibody testing. The first human vaccine generated by classical reassortment was derived from A/duck/Singapore/3/97 (H5N3) virus and was designed to provide protection against H5N1/97 viruses. This vaccine was reported to be poorly immunogenic in humans, but use of the adjuvant MF59 increased the antibody titer (6). The results of our study and of in vitro assays suggest that genetic engineering of specific residues in the H5 HA may provide an additional means of improving detection of a specific immune response to H5 antigens.
Our results in ferrets suggest that evaluation of postinfection human sera could be improved by genetic engineering of H5 antigens, such as ΔH5-N223. A 2-fold or 4-fold increase in sensitivity could be especially significant in situations in which the endpoints of conventional titration methods are below the limit of detection. The strategy applied here to H5 may be useful in increasing HI titers against other avian HA subtypes, such as H9 and H7. In addition to the use of reference viruses with increased sensitivity in human vaccine clinical trials, those viruses can be used in seroepidimiology studies. The availability of data showing how many humans were infected with H5N1 viruses by rapid and simple detection methods like HI assays would provide important information on the prevalence of H5N1 viruses in humans. This data could be used to asses the probability of H5N1 viruses to spread from human to human.
Acknowledgments
We thank Scott Krauss, David Walker, Patrick Seiler, Jennifer Humberd, and Kelly Jones for excellent technical assistance and Sharon Naron for editorial assistance. These studies were supported by Grant AI95357 from the National Institute of Allergy and Infectious Diseases, Cancer Center Support Grant CA21765 from the National Institutes of Health, and the American Lebanese Syrian Associated Charities.
Author contributions: E.H., A.S.L., R.J.W., E.A.G., and R.G.W. designed research; E.H., A.S.L., R.J.W., E.A.G., and R.G.W. performed research; E.H., A.S.L., R.J.W., E.A.G., and R.G.W. analyzed data; and E.H., A.S.L., R.J.W., E.A.G., and R.G.W. wrote the paper.
Abbreviation: EID50, egg 50% infective dose; HI, hemagglutination inhibition; HAU, hemagglutinating unit; RBC, red blood cell.
References
- 1.Li, K. S., Guan, Y., Wang, J., Smith, G. J., Xu, K. M., Duan, L., Rahardjo, A. P., Puthavathana, P., Buranathai, C., Nguyen, T. D., et al. (2004) Nature 430, 209-213. [DOI] [PubMed] [Google Scholar]
- 2.Kuiken, T., Rimmelzwaan, G., van Riel, D., van Amerongen, G., Baars, M., Fouchier, R. & Osterhaus, A. (2004) Science 306, 241. [DOI] [PubMed] [Google Scholar]
- 3.Fouchier, R., Kuiken, T., Rimmelzwaan, G. & Osterhaus, A. (2005) Nature 435, 419-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicholson, K. G., Colegate, A. E., Podda, A., Stephenson, I., Wood, J., Ypma, E. & Zambon, M. C. (2001) Lancet 357, 1937-1943. [DOI] [PubMed] [Google Scholar]
- 5.Stephenson, I., Bugarini, R., Nicholson, K. G., Podda, A., Wood, J. M., Zambon, M. C. & Katz, J. M. (2005) J. Infect. Dis. 191, 1210-1215. [DOI] [PubMed] [Google Scholar]
- 6.Stephenson, I., Nicholson, K. G., Colegate, A., Podda, A., Wood, J., Ypma, E. & Zambon, M. (2003) Vaccine 21, 1687-1693. [DOI] [PubMed] [Google Scholar]
- 7.Takada, A., Kuboki, N., Okazaki, K., Ninomiya, A., Tanaka, H., Ozaki, H., Itamura, S., Nishimura, H., Enami, M., Tashiro, M., Shortridge, K. F. & Kida, H. (1999) J. Virol. 73, 8303-8307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann, E., Krauss, S., Perez, D., Webby, R. & Webster, R. G. (2002) Vaccine 20, 3165-3170. [DOI] [PubMed] [Google Scholar]
- 9.Liu, M., Wood, J. M., Ellis, T., Krauss, S., Seiler, P., Johnson, C., Hoffmann, E., Humberd, J., Hulse, D., Zhang, Y., et al. (2003) Virology 314, 580-590. [DOI] [PubMed] [Google Scholar]
- 10.Webby, R. J., Perez, D. R., Coleman, J. S., Guan, Y., Knight, J. H., Govorkova, E. A., McClain-Moss, L. R., Peiris, J. S., Rehg, J. E., Tuomanen, E. I. & Webster, R. G. (2004) Lancet 363, 1099-1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Govorkova, E. A., Rehg, J. E., Krauss, S., Yen, H. L., Guan, Y., Peiris, M., Nguyen, T. D., Hanh, T. H., Puthavathana, P., Long, H. T., et al. (2005) J. Virol. 79, 2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaverin, N. V., Rudneva, I. A., Ilyushina, N. A., Lipatov, A. S., Krauss, S. & Webster, R. G. (2004) J. Virol. 78, 240-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohler, G. & Milstein, C. (1976) Eur. J. Immunol. 6, 511-519. [DOI] [PubMed] [Google Scholar]
- 14.Palmer, D. F., Dowdle, M. T. Coleman, M. T. & Schild, G. C. (1975) Advanced Laboratory Techniques for Influenza Diagnosis. U.S. Department of Health, Education and Welfare Immunology Series 6 (U.S. Dept. of Health, Education, and Welfare, Washington, DC).
- 15.Kida, H., Brown, L. E. & Webster, R. G. (1982) Virology 122, 38-47. [DOI] [PubMed] [Google Scholar]
- 16.Guan, Y., Poon, L. L., Cheung, C. Y., Ellis, T. M., Lim, W., Lipatov, A. S., Chan, K. H., Sturm-Ramirez, K. M., Cheung, C. L., Leung, Y. H., et al. (2004) Proc. Natl. Acad. Sci. USA 101, 8156-8161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipatov, A. S., Webby, R. J., Govorkova, E. A., Krauss, S. & Webster, R. G. (2005) J. Infect. Dis. 191, 1216-1220. [DOI] [PubMed] [Google Scholar]
- 18.Ha, Y., Stevens, D. J., Skehel, J. J. & Wiley, D. C. (2001) Proc. Natl. Acad. Sci. USA 98, 11181-11186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bright, R. A., Ross, T. M., Subbarao, K., Robinson, H. L. & Katz, J. M. (2003) Virology 308, 270-278. [DOI] [PubMed] [Google Scholar]
- 20.Ito, T., Suzuki, Y., Mitnaul, L., Vines, A., Kida, H. & Kawaoka, Y. (1997) Virology 227, 493-499. [DOI] [PubMed] [Google Scholar]
- 21.Subbarao, K., Chen, H., Swayne, D., Mingay, L., Fodor, E., Brownlee, G., Xu, X., Lu, X., Katz, J., Cox, N. & Matsuoka, Y. (2003) Virology 305, 192-200. [DOI] [PubMed] [Google Scholar]
- 22.Nicolson, C., Major, D., Wood, J. M. & Robertson, J. S. (2005) Vaccine 23, 2943-2952. [DOI] [PubMed] [Google Scholar]