Abstract
Background
Prolonged sedentary behavior in workplace settings is associated with increased health risks, including chronic diseases and reduced productivity. While various mobile health (mHealth) interventions exist, most focus on single behaviors such as physical activity (PA) or sedentary time, with limited solutions integrating diet, PA, and sedentary behavior for sedentary employees.
Objective
This study aimed to develop Simple Health, an evidence- and theory-based mHealth web app designed to promote healthy eating, increase PA, and reduce sedentary time among sedentary employees. The study also evaluated the app’s usability.
Methods
The study followed a two-phase approach. In Phase 1, Simple Health was developed by a multidisciplinary team using social cognitive theory and the ecological model as theoretical foundations. Behavior change techniques such as goal-setting, self-monitoring, and personalized feedback were incorporated. In Phase 2, usability testing was conducted with eight sedentary employees. Participants used Simple Health for five days and completed the mHealth app usability questionnaire (MAUQ) to assess ease of use, interface satisfaction, and perceived usefulness. Open-ended feedback was also collected to identify areas for improvement.
Results
Most participants (87.5%) found Simple Health easy to use, with usability scores indicating favorable responses across ease of use (mean: 2.20/7), interface satisfaction (mean: 1.91/7), and usefulness (mean: 1.98/7). Participants valued the simplicity of behavior logging and the actionability of personalized advice. Suggestions for improvement included increasing goal-setting flexibility and refining navigation to enhance user experience.
Conclusions
The development and usability evaluation of Simple Health demonstrate its potential as a workplace mHealth intervention that integrates PA promotion, sedentary behavior reduction, and dietary tracking. While usability feedback was generally positive, refinements such as improved navigation and enhanced goal-setting flexibility could further optimize engagement. Future iterations should explore automatic syncing with wearable devices and expanded implementation in workplace wellness programs to assess long-term adoption and effectiveness.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-22401-3.
Keywords: Mobile health, Usability study, Sedentary behavior, Physical activity, Healthy diet, Workplace wellness
Background
Mobile health (mHealth) technologies have transformed health promotion by providing innovative solutions that encourage healthier lifestyles through mobile devices [1–6]. mHealth, a subset of electronic health (eHealth), refers to the use of mobile devices such as smartphones and tablets to support health-related services [7]. These technologies have demonstrated potential in addressing lifestyle-related health issues such as obesity, physical inactivity, and unhealthy eating. However, most existing mHealth solutions focus on single health behaviors, such as increasing physical activity (PA) or reducing sedentary time, with fewer interventions comprehensively integrating multiple behaviors, particularly in workplace settings [8–12].
Physical activity encompasses any bodily movement produced by skeletal muscles that requires energy expenditure and occurs across various domains, including work, domestic chores, transportation, and leisure time [13]. It includes a spectrum of intensities, ranging from light PA to vigorous exercise, all of which contribute to overall health and well-being [14]. Conversely, sedentary behavior refers to waking time spent sitting or lying down with minimal energy expenditure [14]. It occurs across multiple settings, including the workplace, home, and during transportation. Prolonged sedentary behavior, regardless of PA levels, is associated with increased cardiometabolic disease risk, premature mortality, and reduced workplace productivity [15, 16]. Since many employees accumulate excessive sitting time during work hours, workplace interventions must address both physical inactivity and prolonged sedentary behavior to improve employee health outcomes [17].
Despite the rise of workplace mHealth interventions, most apps focus on a single health behavior, such as promoting PA or reducing sedentary time, while largely neglecting dietary habits [8, 10–12, 18]. Workplace wellness apps such as UPnGO with ParticipACTION and W@W-App encourage movement through step tracking, sit-stand reminders, and gamification features [10, 12]. While effective for short-term engagement, these apps fail to comprehensively integrate multiple health behaviors, limiting their potential for long-term impact.
Some workplace-based apps, such as Health Integrator, offer personalized digital coaching to improve either PA or diet [19]. However, these interventions remain fragmented, addressing behaviors individually rather than considering their interdependent nature. Simple Health was developed to fill this gap by integrating sedentary behavior reduction, PA promotion, and dietary tracking into a single intervention.
For effective mHealth intervention design, two primary theoretical frameworks provide the foundation for behavior change: social cognitive theory [20] and the ecological model [21]. Social cognitive theory emphasizes self-efficacy and self-regulation, positing that an individual’s belief in their ability to perform specific actions is critical for sustained behavior change [20]. By integrating this framework, Simple Health fosters motivation and resilience, enhancing users’ self-regulatory abilities in health-related pursuits [20]. Complementarily, the ecological model considers multiple levels of influence on health behaviors, including intrapersonal, interpersonal, organizational, community, and policy factors [21]. This model ensures that Simple Health not only supports individual behavior change but also fosters a supportive environment within the workplace [22].
Unlike traditional workplace mHealth interventions that focus on a single health behavior, Simple Health integrates multiple lifestyle factors, ensuring a holistic approach to workplace health promotion. Research indicates that multi-component interventions yield greater behavior change and long-term health benefits than single-behavior approaches [23, 24]. Additionally, Simple Health features a personalized and adaptive feedback system that dynamically tailors recommendations based on real-time behavior tracking, utilizing behavior change techniques (BCTs) such as goal-setting, self-monitoring, and reinforcement [22, 25, 26]. This customized intervention model differentiates it from apps with static, one-size-fits-all recommendations.
Whereas some workplace wellness programs (e.g., Health Integrator) require human-led coaching for behavior modification [19], Simple Health utilizes automated, evidence-based coaching to support goal-setting, performance tracking, and behavior reinforcement, making it more scalable, cost-effective, and accessible for workplace implementation. Furthermore, Simple Health incorporates team-based challenges, peer motivation, and workplace social ranking systems, extending beyond individual behavior change by fostering a supportive workplace culture that encourages long-term engagement [21, 22].
The usability of mHealth apps plays a critical role in determining effectiveness and long-term adherence. Poor usability often results in low engagement, early abandonment, and reduced intervention effectiveness [27]. The mHealth app usability questionnaire (MAUQ) is a validated tool for assessing usability, providing quantitative and qualitative insights into ease of use, interface design, and user satisfaction [27]. Previous research emphasizes that user-friendly design and personalized engagement are key factors influencing sustained app adoption [28]. To optimize usability and engagement, this study evaluates Simple Health through real-world testing with sedentary employees, identifying design strengths and areas for refinement to enhance user experience.
This study aims to bridge current gaps by developing Simple Health, an evidence- and theory-based mHealth web app that promotes healthy eating, increased PA, and reduced sedentary behavior among sedentary employees. Additionally, the study seeks to evaluate Simple Health’s usability to ensure adequate user engagement.
The primary research questions guiding this study are: (1) How can an mHealth web app be designed and developed based on theoretical frameworks to promote healthy eating, increase PA, and reduce sedentary behavior among sedentary employees? (2) How do sedentary employees perceive the usability of the developed mHealth web app regarding ease of use, interface quality, and user satisfaction?
Methods
Overview
This study was conducted in two phases. In Phase 1, the primary objective was to design and develop an evidence- and theory-based mHealth web app aimed at promoting healthy eating, increasing PA, and reducing sitting time among sedentary employees. A multidisciplinary team was assembled, including research assistants with dietitian certifications, software engineers, computer programmers, graphic designers, and experts in occupational health, nursing, and nutrition. This diverse expertise ensured the web app was both practical and tailored to the target population. Active collaboration among team members was central to aligning the web app’s features with the specific needs and preferences of sedentary employees. In Phase 2, usability testing was conducted with end users to refine the web app’s design and functionality. Participants were invited to perform a series of tasks within the app, and feedback from these sessions was incorporated into iterative improvements to ensure the app met user needs effectively.
Ethics approval
Ethics approval for this study was obtained from the China Medical University & Hospital Research Ethics Center (CRREC-106-036 [CR-1]).
Phase 1: design and development of the mHealth web app
Step 1: define purpose, target behaviors, and strategies of the app
Behavior change interventions grounded in behavioral theories are known to be effective in promoting lifestyle modifications [26]. Thus, this study incorporated principles from Bandura’s social cognitive theory [20], which emphasizes self-regulation and self-efficacy, and the ecological model [21], which considers various levels of influence on health behavior, including intrapersonal, organizational, community, and policy factors. These theoretical frameworks were used to structure key behavior change techniques (BCTs), such as goal setting, self-monitoring, and personalized feedback, within the app’s design to enhance users’ dietary habits, PA, and reduce sedentary behavior [8, 22, 25, 26, 29].
The app’s primary features included: (1) Health behavior tracking and monitoring: enables users to engage in self-observation and track their health behaviors over time. (2) Goal setting, recommendations, and performance ranking: helps users establish and assess health goals, supporting self-assessment and motivation. (3) Personalized advice: provides tailored tips and insights designed to reinforce self-regulation and self-efficacy. Advice includes elements such as performance accomplishments, opportunities to observe others’ healthy behaviors (vicarious experience), verbal encouragement, and emotional regulation techniques. (4) Integration of environmental influences: recognizes environmental factors impacting behavior and incorporates them into the advice provided, ensuring a holistic approach to health promotion.
Step 2: platform selection
After defining the app’s structure and goals, the next step was to select the platform—either a native app or a web app. Native apps run directly on the smartphone’s operating system and must be downloaded from app stores such as Google Play or the Apple App Store [30]. In contrast, web apps run on external servers and are accessed through web browsers. Turner-McGrievy et al. recommend choosing a platform based on specific app needs [31]. Native apps are suitable when features like photo capturing, location tracking, touchscreen interaction, on-device processing, or notifications are required. However, a web app is more suitable when the goals include low development cost, platform independence, quick updates, and long-term support [31]. For this intervention, a web app was selected due to its accessibility across devices without requiring installation, allowing users to access it on any device with a browser, increasing usability and reach.
Step 3: program content and tailoring algorithms
The intervention’s content and structure were based on evidence-based guidelines and theoretical models of self-regulation, self-efficacy, and environmental influences. The research team reviewed current PA and dietary guidelines [32–36], as well as empirical studies, to inform the app’s program content and features. The core components developed for the app included:
Health behavior goals
Hourly stand-up goals: Encourages users to log standing frequency every hour, aiming for two instances per hour to promote light PA based on evidence from Pedisic et al. [37] and Diaz et al. [38]. Users track the number of times they stand each hour.
Daily PA goals: Walking is promoted as a simple, accessible PA, with options to track steps via an activity tracker or self-report. Goals are set at 10,000 steps per day [39] or 150–300 min of weekly moderate PA [36]. For users with limited PA, the app starts with 5,000 steps per day, gradually increasing by 10% each week [40]. The app offers incremental targets, such as adding 1,000 steps every two weeks, encouraging self-regulation.
Daily healthy eating goals: The app calculates daily calorie targets (ranging from 1,300 to 2,000 kcal) based on Taiwanese adult height averages [41] and various PA levels, aligning with the guideline [42]. The app also follows MyPlate guidelines [35] for balanced diet proportions, categorizing food into whole grains, proteins, vegetables, and fruits. Nutrient intake follows Taiwan’s dietary guidelines, suggesting 10–20% of calories from protein, 20–30% from fat, and 50–60% from carbohydrates [33]. The app recommends six servings of vegetables for users on the 1,300 and 1,500 kcal plans and nine servings for those on the 1,800 and 2,000 kcal plans, with a consistent recommendation of three servings of fruit across all calorie levels. Table 1 provides the recommended daily servings for each food group across the four calorie plans.
Table 1.
Recommended numbers of servings per day at calorie levels in healthy eating
| Calories, Portion size, Food group | 1300 Kcals | 1500 Kcals | 1800 Kcals | 2000 Kcals |
|---|---|---|---|---|
| Whole grains | 6 | 7.5 | 9 | 12 |
| Proteins | 6 | 7.5 | 9 | 9 |
| Vegetables | 6 | 6 | 9 | 9 |
| Fruits | 3 | 3 | 3 | 3 |
Setting reminders
Users can set personalized reminders, sent via LINE@, at scheduled times to encourage behavior tracking. Reminders such as “stand up and move” and “record my health behaviors” prompt regular engagement, and users receive notifications every 14 days to reset goals. LINE@ was chosen as it is widely used in Asia and allows multimedia communication, supporting text, images, and video. To maximize convenience, the web app is integrated with participants’ personal LINE accounts, linked to the program’s official LINE@ account. This integration allows users to receive timely reminders and personalized updates directly through LINE@, keeping them engaged in the program and providing essential notifications without requiring users to manually access the web app.
Daily logging of behaviors
Stand-up activity: Users specify whether it is a workday, logging standing frequency for work or during morning, afternoon, and evening periods on non-workdays. Research shows employees often engage in prolonged sedentary behavior on both workdays and weekends [43].
Physical activity: The interface adjusts for easy logging based on the user’s selected goal. A guide helps users assess PA intensity, following the Taiwan Health Promotion Administration’s standards [34].
Healthy eating: The app provides tools for logging daily dietary intake using detailed nutritional information, portion sizes, and volume charts [33, 44–51]. Foods are grouped into subcategories based on similarities in appearance, preparation, and portion sizes. When the charts lack specific items, the app allows users to weigh portions using a standard research bowl (250 ml, 10 cm diameter, 5 cm depth) or cup (215 ml). Foods are categorized into four main groups: whole grains, proteins, vegetables, and fruits. To better reflect Taiwan’s dietary habits and enhance tracking, the whole grain category is divided into six subcategories and the protein category into five, with clear serving sizes for each item. The app encourages balanced, healthy eating by dividing meals into 3 main categories: breakfast, lunch, and dinner. Users can also log additional meals or snacks to accommodate individual schedules or eating patterns (e.g., intermittent fasting). This feature enables comprehensive tracking of daily food intake, supporting mindful and balanced eating habits.
Personalized advice
An algorithmic decision-making system was developed to deliver tailored advice based on behavioral performance and goal-setting status (i.e., goal achievement rate). These personalized messages were designed to enhance self-efficacy (via observational learning, scenario simulation, verbal persuasion, and emotional regulation) and self-regulation (via self-monitoring, self-assessment, goal setting, plan development, and positive reinforcement). The advice also highlights the benefits of adopting healthy behaviors while addressing potential barriers users may face. Depending on the user’s progress, the system provides different types of advice, including (1) encouragement to increase a behavior if the target has not been met; (2) reinforcement to maintain the behavior if performance is within the acceptable range [52]; and (3) suggestions to adjust or reduce a behavior if it exceeds the target. Table 2 provides an overview of the tailored advice for each behavior, categorized by achievement rate.
Table 2.
Personalized advice for sitting less, moving more, and healthy eating based on achievement rate
| Behavior | Achievement rate | Example of personalized advice |
|---|---|---|
| Sitting less | < 90% (room for improvement) | You need to get up and move more frequently! Try standing up when you drink water or answer the phone! |
| Sitting less | ≥ 90% (good performance) | Great job! Keep up the good work. Regularly standing up and moving can help reduce the risk of non-communicable diseases. |
| Moving more | < 90% (room for improvement) | Try walking a bit more! Regular exercise stimulates brain cells and keeps your mind sharp! |
| Moving more | ≥ 90% (good performance) | Great job! Exercise helps maintain muscle mass and protect cardiovascular health. Keep up your exercise routine! |
| Whole grains | < 90% (below standard, increase intake) | Try adding more whole grains to your diet! Brown rice and whole wheat products contain more dietary fiber, phytochemicals, B vitamins, and minerals compared to white rice and refined starches, helping to prevent chronic diseases! |
| Whole grains | 90–110% (good performance) | Great job! Whole, unrefined foods are rich in fiber, phytochemicals, vitamins, and minerals. Consider adding mixed grains, mung beans, sweet potatoes, pumpkins, potatoes, yams, or lotus root to your meals! |
| Whole grains | > 110% (above standard, reduce intake) | You’re consuming too many whole grains! Research shows that excessive intake of refined carbohydrates (such as white bread and white rice) can lead to chronic high blood sugar levels, which may result in negative metabolic outcomes! |
| Protein | < 90% (below standard, increase intake) | Increase your protein intake! Foods like beans, eggs, seafood, meat, and dairy products are rich in protein, which can slow the rise of blood sugar, maintain muscle mass, and improve strength! |
| Protein | 90–110% (good performance) | Well done! If you had chicken and dairy this meal, try beans, eggs, seafood, or nuts in the next meal to diversify your nutrient intake! |
| Protein | > 110% (above standard, reduce intake) | You’re eating too much protein! Studies show that excessive consumption of processed meat and red meat increases the risk of inflammation, oxidative stress, and exposure to carcinogens, raising overall mortality risk! Opt for natural sources like beans, eggs, fish, meat, dairy, and nuts! |
| Vegetables | < 90% (below standard, increase intake) | You’re not getting enough vegetables. Studies show that people who eat leafy greens have a lower risk of cardiovascular diseases. Try adding spinach or kale to your meals! |
| Vegetables | ≥ 90% (good performance) | Excellent, keep it up! Carotenoids help prevent cardiovascular disease and support eye health. Try incorporating a variety of red, yellow, and green vegetables into your diet! |
| Fruits | < 90% (below standard, increase intake) | Eat more fruits! A serving of fruit is equivalent to one small apple or one orange. |
| Fruits | 90-184.9% (good performance) | Your efforts are paying off! The Mediterranean diet, known to reduce the risk of cardiovascular disease and cancer, emphasizes fruits and vegetables. Keep up the great work! |
| Fruits | ≥ 185% (above standard, reduce intake) | You’re eating too much fruit! Fiber-rich fruits help with portion control by increasing fullness and slowing digestion, which prevents overeating. Stick to fiber-rich options for better balance! |
Health classroom
Educational booklets: The app offers educational booklets that provide practical guidance on increasing PA, maintaining a balanced diet, and reducing sedentary behavior. Six booklets were developed, covering the benefits of PA, tips for staying active, healthy eating basics, practical nutrition advice, safety tips, and simple healthy recipes. Two booklets are released monthly through the app, offering participants easy-to-follow steps to support these health goals.
Motivational booklets. To enhance motivation and commitment, six motivational booklets were designed to address goal setting, overcoming obstacles, avoiding temptations, preventing relapse, maintaining motivation, and sustaining healthy habits [53]. One booklet is provided biweekly through the app, encouraging participants to recognize challenges, stay focused, and continue their progress toward a healthier lifestyle.
Recommended articles and links: To further enrich the participant experience, the app curates articles and videos from reputable health sources. These resources cover reducing sedentary behavior, increasing PA, and adopting healthier eating habits. Additionally, links to trusted websites are provided, allowing users to explore these topics in greater depth and supplement their learning with valuable, credible information.
Health rankings
My performance: Users can track key health metrics—hourly standing frequency, daily step count or minutes of PA, and daily servings of four major food groups—alongside personalized goals. The app calculates an achievement rate by comparing actual performance to target values, supporting users in self-assessing progress. Performance charts reflecting overall PA, workday, and non-workday behavior help users understand patterns, addressing findings that office workers experience prolonged sedentary periods [43].
-
Personal and team rankings: Users can view personal and team-based health performance, fostering individual accountability and group engagement. Rankings are based on three core behaviors: sitting less, moving more, and healthy eating. For each behavior, scores are calculated relative to user-specific goals and aggregated into an overall score. Team scores are derived from the total of individual scores divided by the team size, allowing comparisons across teams.
- “Sitting less score” reflects the frequency of hourly standing, with higher scores for users who stand up more frequently.
- Physical activity levels are converted into a “moving more score” to allow fair comparisons between users with and without activity trackers. Research indicates that 30 min of moderate-intensity PA (approximately 3,800–4,000 steps) [54] aligns with standard daily levels of 6,000–7,000 steps [55]. Based on these estimates, 10,000 daily steps equate to 30 min of moderate-intensity PA. Users earn 100 points by achieving 10,000 steps, 30 min of light or moderate PA, or 20 min of vigorous PA.
- Based on the Healthy Eating Index (HEI) [56], a “healthy eating score” evaluates daily intake of whole grains, proteins, vegetables, and fruits. Each category contributes up to 25 points for a total possible score of 100. Full points are awarded for intake within 90–110% of the target. Vegetables must meet 90% of the goal due to common dietary deficiencies, while fruits earn total points for 90–184.9% of the target; exceeding 185% results in no points, following the DASH diet’s recommendations of 5.2 servings at 2,100 kcal [57]. Food intake is evaluated daily rather than per meal, allowing flexibility. An allowable deviation range is set to encourage consistent healthy eating behaviors [52].
- The “overall score,” 100 points, allocates 34 points for sitting less, 33 for moving more, and 33 for healthy eating, providing a balanced assessment of all behaviors.
Support partners
This feature includes “my team,” “join team,” and a “message board” to help users build a personalized support network within the app. Users can invite colleagues to form teams to collaborate on health goals, share progress, celebrate achievements, and offer mutual encouragement and motivation. This feature fosters interaction and peer support among individuals with similar health objectives. The message board further enhances communication by enabling discussions, sharing challenges, celebrating successes, and creating an engaging, supportive community within the app.
Step 4: web app development and database management
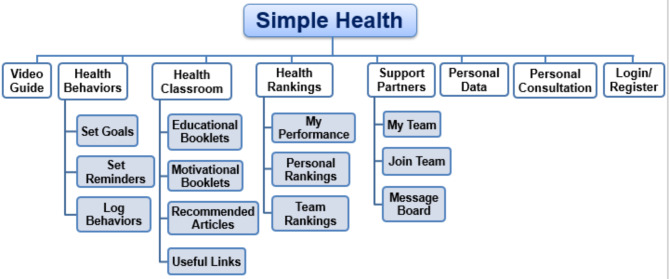
A software development company built the Simple Health web app under the research team’s guidance. The company was responsible for the technical development and app maintenance. To ensure the app’s content and functionality met users’ needs, it was validated by an expert panel and the target population. Figures 1, 2 and 3 display the app’s structure and homepage screenshots in computer and smartphone versions. Flowcharts and screenshots are provided in Additional File 1.
Fig. 1.
Simple Health structure
Fig. 2.
Screenshot of the homepage (computer version)
Fig. 3.
Screenshot of the homepage (smartphone version)
The app was built using the Hypertext Preprocessor (PHP) programming language to facilitate database communication and generate user interfaces. Responsive Web Design (RWD) was implemented using HyperText Markup Language (HTML), Cascading Style Sheets (CSS), JavaScript, JQuery, and Bootstrap, ensuring compatibility across various devices. For data security, MD5 encryption was applied to protect user passwords. Data from the relational database were regularly exported in comma-separated values (CSV) format, allowing easy integration with statistical software for analysis. Several visual assets, including images, were sourced from Shutterstock to avoid copyright issues, maintaining both a professional appearance and legal compliance.
Step 5: post-production quality control
The initial version of the web app underwent multiple rounds of alpha testing to ensure quality control, focusing on identifying and resolving technical and logical issues. Research team members and students tested the app, offering valuable feedback on content accuracy, functionality, editorial consistency, and overall usability. Feedback from external volunteers provided fresh perspectives, highlighting areas where instructions were unclear or specific program features were confusing. Based on this comprehensive feedback, revisions were implemented, and the app underwent an additional round of quality control. Additionally, the program was tested with eight sedentary employees before its full implementation, providing further insights and confirming that the app was user-friendly, effective, and ready for broader use.
Phase 2: usability testing
The usability and acceptability of the prototype Simple Health web app were evaluated through data verification and user assessment. To ensure accuracy, the principal investigator and research assistant cross-checked app data against the relational database by randomly logging dietary and activity behaviors and verifying correct data processing and display.
User perceptions of usability and acceptability were assessed using a Chinese-translated version of the MAUQ. The MAUQ consists of 17 questions covering three domains: ease of use, interface satisfaction, and usefulness [27]. Responses were recorded on a 7-point Likert scale (1 = strongly agree to 7 = strongly disagree), where lower average scores indicate higher usability. The MAUQ has demonstrated strong internal consistency (Cronbach’s alpha = 0.914), with the three subscales showing good to acceptable internal consistency (Cronbach’s alpha range: 0.72–0.91) [27]. Additionally, three open-ended questions gathered qualitative feedback on (1) the most frequently used app features, (2) the time required for daily entries, and (3) suggestions for usability improvements.
The total mean score of the MAUQ was calculated without weighting individual items, as all responses were collected on a 7-point Likert scale. This approach aligns with the validated MAUQ methodology, ensuring consistency with prior studies and preserving the comparability of results. Given the strong internal consistency of the instrument and its uniform response format, weighting was not necessary to maintain interpretability and methodological rigor.
A purposive sample of eight sedentary workers was recruited from an aerospace company in Taichung, Taiwan. Initially, we aimed to recruit five participants, as prior research indicates that usability testing with as few as five users can uncover a substantial proportion of interface issues [58]. However, during recruitment, additional employees expressed interest in participating. To ensure gender balance, we included four males and four females, ultimately expanding the sample to eight participants. While still a small sample, this slight increase allowed us to capture a broader range of user experiences and gather more diverse usability feedback.
Participants were recruited through internal workplace communication channels, with eight individuals voluntarily agreeing to participate. Once a balanced gender distribution was achieved, no further recruitment efforts were made. Eligibility criteria included being a full-time sedentary employee aged 20 or older, having no physical limitations that would hinder participation in PA, and owning a smartphone with Internet access and the LINE app installed. Informed consent was obtained prior to testing.
A “sedentary employee” was defined as an individual who spends more than six hours per workday sitting. This definition aligns with occupational health research [59], which suggests that sitting for approximately 6.4 h or more during the workday represents a substantial portion of work hours spent in a sedentary posture. This threshold is commonly used in workplace health studies to identify individuals at risk of prolonged sedentary behavior and its associated health risks.
Participants engaged with the Simple Health web app while wearing a Fitbit Alta HR activity tracker to monitor their daily step count. Iterative modifications were made following each testing round until users successfully completed 90% of assigned tasks. As an acknowledgment of their time and contribution, each participant received a US$16 incentive.
Results
Phase 1: design and development of the mHealth web app
We developed the Simple Health web app’s content, platform, and structure based on theoretical foundations, a comprehensive literature review, and user feedback. The intervention integrates evidence-based guidelines and behavior change theories focused on enhancing self-regulation and self-efficacy and addressing environmental factors influencing behavior. Table 3 provides a summary of the mHealth program content, including activity tracking, goal setting, reminders, behavior logging, personalized advice, electronic educational booklets, electronic motivational booklets, and individual and team challenges.
Table 3.
Elements of the mHealth intervention and applied behavior change techniques
| Element | Purpose and BCTs used | Frequency | Actions to be taken |
|---|---|---|---|
| Activity tracking |
• The activity tracking feature will enable participants to monitor their progress toward PA goals by providing real-time data on steps taken, calories burned, and distance traveled. This data will help users assess their activity levels and identify areas for improvement. • Activity trackers will play a crucial role in regulating behavior by offering structure, motivation, and feedback, which are essential for adopting and maintaining healthy habits. • BCTs applied: self-monitoring of behavior, prompts/cues, and habit formation. |
Daily, during months 1–3 | • Participants in the intervention group will be provided with activity trackers, which they will wear on their wrists to track their daily step counts and activity levels accurately. |
| Goal setting |
• Goal setting will be a key element of behavioral regulation, providing participants with direction and motivation to manage and adapt their behaviors to achieve desired outcomes. It will empower individuals to take control of their actions and make consistent progress. • Achieving short-term goals will enhance self-efficacy, a critical factor in behavioral regulation. Participants who feel confident in their ability to succeed will be more likely to engage in and sustain behaviors that contribute to reaching their goals • BCTs applied: Behavioral goal setting, self-monitoring of behavior, and habit formation. |
Biweekly, during months 1–3 |
• Participants will set biweekly health behavior goals using the web app. • Before goal setting, they will receive guidance on formulating personal, realistic, and challenging objectives. • Participants will set daily calorie intake targets for healthy eating, specifying appropriate portions from the 4 food groups: whole grains, protein, vegetables, and fruits. • For PA, the goal will be to establish a daily step count. • They will also set stand-up goals to ensure they move around after every hour of sitting. |
| Reminders |
• Reminders will act as cues to prompt specific behaviors at designated times, helping participants remember important tasks or activities and supporting adherence to routines or schedules. • Reminders will be a practical tool for behavioral regulation, providing essential prompts to initiate, maintain, and adjust behaviors in line with personal goals. • BCTs Applied: Prompts/cues, habit formation. |
Daily, during months 1–3 | • Participants will be encouraged to use the web app to set reminders for standing up and logging their behaviors. Notifications for these reminders will be sent through the LINE messaging platform. |
| Behavior logging |
• Behavior logging will be a crucial element of behavioral regulation, providing participants with a structured method to track, understand, and adjust their behaviors. • It will help bridge the gap between intention and action, enabling participants to take control of their habits and systematically work toward achieving their goals. • BCTs applied: Self-monitoring of behavior and habit formation. |
Daily, during months 1–3 |
• Participants will log their daily health behaviors via the web app, including dietary intake, PA, and stand-up occurrences. • The platform will be essential in educating participants about appropriate portion sizes for whole grains, proteins, vegetables, and fruits, helping them track their dietary behaviors more accurately. |
| Personalized advice |
• Personalized advice will offer tailored guidance that aligns with each participant’s unique circumstances and goals. This customization will make the advice more relevant and actionable, increasing the likelihood of adherence. • By delivering tailored, context-specific guidance, the advice will help participants regulate their behavior more effectively while boosting their confidence in achieving their goals. • BCTs applied: Feedback on behavior, behavior substitution, and discrepancy between current behavior and goal. |
Daily, during months 1–3 |
• Advice will be tailored to each participant based on their actual behavior performance and goal-setting status. • After logging their behaviors, participants will receive personalized advice that provides encouragement and positive reinforcement to acknowledge their progress and efforts. |
| Electronic educational booklets |
• The educational booklets will aim to increase participants’ knowledge, develop practical skills, and raise awareness about key health topics, motivating them to initiate and maintain behavior changes. • These booklets will play a critical role in promoting behavioral regulation and self-efficacy by providing the knowledge and skills necessary for participants to effectively manage their behaviors and believe in their ability to achieve their health goals. • BCTs applied: Instruction on how to perform the behavior, problem solving, information about health consequences, demonstration of the behavior, credible source, action planning, and behavior substitution. |
2 booklets will be provided monthly during months 1–3 |
6 educational booklets will be developed and organized into two main themes: “Sit Less, Move More” and “Healthy Eating.” The topics covered in the booklets will include: 1–1 Understanding sitting less and moving more: (1) Benefits of sitting less and moving more; (2) Sedentary behavior and sitting posture; (3) Overview of PA; (4) Recommended amounts for sitting less and moving more; (5) Top 10 tips for staying active during workdays; (6) Strategies for incorporating movement into the workplace. 1–2 Fundamentals of healthy eating: (1) Importance of healthy eating; (2) Various food groups and their nutritional value; (3) Recommendations for healthy eating; (4) Practical advice for healthier food choices when dining out. 2–1 Simplifying “sit less, move more”: (1) Walking for health; (2) Top 10 tips for staying active outdoors and at home; (3) Incorporating movement anytime, anywhere. 2–2 Nutrition at your fingertips: tasty and nutritious: (1) Tips for creating an environment conducive to healthy eating; (2) Simple, healthy recipes. 3–1 Health considerations for standing and PA: (1) Health impacts of prolonged standing and how to mitigate them; (2) Safety considerations for PA; (3) Tips and resources for active leisure. 3–2 Vibrant eating: nutrition and safety: (1) PA and nutrition; (2) Nutrition labels; (3) Food certification labels; (4) Food hygiene and safety. |
| Electronic motivational booklets |
• Motivational booklets will be designed to enhance both intrinsic and extrinsic motivation, encouraging participants to initiate and persist in their efforts to achieve their health goals, even when faced with obstacles. • These booklets will aim to increase participants’ engagement in healthy behaviors by making the process more interesting and rewarding, while reinforcing the importance of their set goals. By reminding participants of the value and benefits of achieving their objectives, the booklets will help align their daily actions with long-term goals. • BCTs applied: Behavioral goal setting, instruction on how to perform the behavior, problem solving, demonstration of the behavior, credible source, action planning, behavior substitution, and self-monitoring of outcomes of behavior |
Biweekly, during months 1–3 |
6 motivational booklets will be created to help participants stay motivated, overcome challenges, and persist in their pursuit of better health. The topics covered will include: 1. Setting goals: Guidance on how to establish realistic and achievable goals for both short-term and long-term healthy behaviors. 2. Overcoming obstacles: Strategies for identifying and overcoming barriers to adopting healthy behaviors. 3. Avoiding temptations: Practical advice for resisting distractions and temptations that may impede progress. 4. Preventing relapse: Techniques for maintaining achievements and preventing setbacks. 5. Maintaining motivation: Strategies for fostering ongoing enthusiasm for an active lifestyle and healthy eating. 6. Sustaining good habits: Approaches for integrating the principles of “sit less, move more, eat healthily” into daily routines. |
| Individual and team challenges |
• The challenges will be designed to boost engagement and motivation by incorporating elements of both competition and cooperation. • These challenges will encourage participants to set specific, short-term goals within a fun and competitive environment. • Challenges support behavioral regulation by providing structured goals and feedback, enhance self-efficacy via achievements and vicarious learning, and offer social support through team-based activities. • BCTs applied: Social support, social comparison, and rewards |
Biweekly, during months 1–3 |
• Within the web app, participants will be able to monitor their progress through the “My Performance” section under the “Health Ranking” feature. This will allow them to compare their rankings with their peers and view their team’s ranking in relation to other groups. • Rankings for both individual and team challenges will be based on performance metrics related to health behaviors (i.e., sitting less, moving more, and healthy eating). The top 3 individual performers and the leading team will receive recognition and awards from the company’s senior management. • The program leveraged a team-based approach and offered incentives, such as prizes, to encourage active participation, setting goals, and achieving these goals. |
Note. BCT = Behavior change techniques; PA = Physical activity
Phase 2: usability testing
Eight sedentary employees (4 males, 4 females) aged 28–61 years (mean = 50.25, SD = 9.81) participated in the five-day usability evaluation (Friday to Tuesday). Participants rated the app across three domains: ease of use, interface satisfaction, and usefulness, using the 7-point Likert scale from 1 (strongly agree) to 7 (strongly disagree) [27]. Lower scores indicated higher usability (Table 4).
Table 4.
Evaluation of the usability and acceptability of the simple health web app (N = 8)
| Mean (SD) | Range | |
|---|---|---|
| Ease of use | 2.20 (1.33) | |
| 1. Simple Health was easy to use. | 2.00 (1.32) | 1–5 |
| 2. It was easy for me to learn to use Simple Health. | 2.00 (0.87) | 1–3 |
| 3. The navigation was consistent when moving between screens. | 2.25 (1.20) | 1–4 |
| 4. The interface of Simple Health allowed me to use all the functions (e.g., setting goals, logging behaviors, viewing health rankings, reading recommended articles) offered by the web app. | 1.88 (1.27) | 1–4 |
| 5. Whenever I made a mistake using Simple Health, I could recover easily and quickly. | 2.88 (1.62) | 1–6 |
| Interface and satisfaction | 1.91 (1.06) | |
| 6. Like the interface of Simple Health. | 2.38 (1.11) | 1–4 |
| 7. The information in Simple Health was well organized, so I could easily find the information I needed. | 2.13 (1.05) | 1–4 |
| 8. Simple Health adequately acknowledged and provided information to let me know the progress of my action. | 2.00 (1.00) | 1–4 |
| 9. I feel comfortable using Simple Health in social settings. | 1.75 (0.83) | 1–3 |
| 10. The amount of time involved in using Simple Health has been fitting for me. | 1.75 (0.83) | 1–3 |
| 11. I would use Simple Health again. | 1.63 (0.99) | 1–4 |
| 12. Overall, I am satisfied with Simple Health. | 1.75 (1.30) | 1–4 |
| Usefulness | 1.98 (1.08) | |
| 13. Simple Health would be useful for my health and well-being. | 1.50 (0.50) | 1–2 |
| 14. Simple Health improved my access to health care services. | 2.00 (1.00) | 1–4 |
| 15. Simple Health helped me manage my health effectively. | 2.00 (1.12) | 1–4 |
| 16. Simple Health has all the functions and capabilities I expected it to have. | 2.50 (1.32) | 1–4 |
| 17. Simple Health provided an acceptable way to receive health care services, such as accessing educational materials, tracking my health behaviors, and viewing my performance. | 1.88 (1.05) | 1–4 |
| How much time do you spend daily logging your stand-up activity, physical activity, and healthy eating? (minutes) | 11.13 (8.05) | 2–30 |
Note. The responses to the statements in the mHealth app usability questionnaire (MAUQ) scale ranged from 1 (strongly agree) to 7 (strongly disagree), with lower average scores indicating higher usability
Ease of use
Most participants (87.5%) reported the app easy to use. The overall mean score for ease of use was 2.20 out of 7 (SD = 1.33). Participants generally found the app user-friendly, with a mean score of 2 for the statement “Simple Health was easy to use,” and a mean score of 2 for “It was easy for me to learn to use Simple Health.” Navigation consistency between screens was rated at 2.25. The app interface’s ability to support the use of all functions, such as setting goals, logging behaviors, and viewing health rankings, was rated at 1.88. Participants generally found it easy to recover from mistakes, as indicated by a score of 2.88, suggesting minor challenges in this area. However, one participant rated this aspect a 6, explaining, “The goal-setting feature currently allows only one entry at a time. It would be better if users could save a new goal each day rather than having the previous one overwritten.”
Interface and satisfaction
Overall satisfaction with the app’s interface scored 1.91 out of 7 (SD = 1.06). Participants generally liked the app’s interface, with a mean score of 2.38 out of 7. They found the information well-organized, scoring it at 2.13, which made it easy to find relevant information. Simple Health adequately acknowledged user progress, scoring 2. Most participants felt comfortable using the app in social settings (mean = 1.75) and found the time spent using the app to be appropriate (mean = 1.75). Participants expressed a willingness to use the app again, with a score of 1.63, and were generally satisfied with their overall experience, as indicated by a score of 1.75.
Usefulness
The perceived usefulness of Simple Health received a mean score of 1.98 out of 7 (SD = 1.08). Participants rated the app’s ability to support their health and well-being with a score of 1.50. The app was considered helpful in improving access to healthcare services, scoring 2 and managing health effectively, also rated at 2. The app’s functions and capabilities met user expectations with a mean score of 2.5. Finally, Simple Health was found to be an acceptable way to receive healthcare services, such as accessing educational materials, tracking behaviors, and viewing health performance, as indicated by a score of 1.88. In addition, all participants expressed satisfaction with the educational content of the intervention, describing it as easy to understand, practical, useful, comprehensive, and engaging.
Time spent logging health behaviors and most frequently used feature
Participants spent an average of 11.13 min daily (SD = 8.05) logging health behaviors, with time ranging from 2 to 30 min. The most frequently used feature was behavior logging, which users valued for several reasons:
Understanding personal health behaviors: Logging helped participants understand their daily habits and health-related activities.
Convenience and ease of use: Participants found the logging feature straightforward and convenient, making it easy to track their behaviors.
Tracking daily diet and activity: The logging feature enabled users to consistently record their daily dietary intake and step count, which is essential for monitoring progress.
Goal achievement: Participants felt that logging activities provided a sense of accountability, helping them work toward achieving their health goals.
Reviewing and adjusting behaviors: Participants appreciated the ability to review and track their daily behaviors, which allowed them to make necessary adjustments, improving their health outcomes over time.
Future self-assessment: Some participants noted that regular logging would aid in future goal setting and self-assessment, keeping them motivated and on track.
Advantages of Simple Health
Participants identified several advantages of the Simple Health web app, contributing to the positive user experience and engagement with Simple Health. The convenience of accessing the app, mainly through a quick link via LINE, was a key benefit. Users also appreciated the well-presented interface, highlighting its clean, single-page design. Simple Health was consistently praised for its ease of use, with participants finding it easy to navigate and interact with the features.
The reminders feature was noted as applicable, while the logging function received positive feedback for its intuitive design. Participants found logging dietary information simple and enjoyable, with images of food portions, such as oranges, making portion control more accessible. Additionally, the health classroom feature was valuable for gaining health-related knowledge.
The personalized advice provided through the health rankings feature was particularly appreciated. One participant noted that a specific suggestion, such as incorporating “plum tomatoes” into their diet, was more actionable than general recommendations to eat more fruit. Furthermore, the analysis and feedback feature helped participants reflect on their daily eating habits and make improvements for subsequent meals.
In addition, the educational component was highly valued, as it enriched participants’ learning experiences and facilitated their understanding of health-related topics. The information provided was not only accessible but also actionable, helping participants apply the knowledge gained to improve their health behaviors.
Specific suggestions to improve Simple Health
Participants provided several suggestions for improving the usability of the Simple Health web app:
Menu design: Users recommended simplifying the mobile menu to reduce the number of layers, making navigation easier. Suggestions included displaying multiple options with a single click and adding a “back” button on the “log behaviors” page. Participants also preferred keeping the menu on a single page.
Shortcut design: Participants proposed modifying the mobile shortcut button linked to “set goals” to “log behaviors,” as this feature was used more frequently.
Setting goals: Participants suggested clarifying portions for the “healthy eating goal” feature by indicating whether photos represent a single meal portion. Additionally, they recommended including dates when setting goals for better tracking.
Logging behaviors: Participants wanted to view their logged data directly on the “log behaviors” page, allowing them to compare their records with their health rankings. They also suggested improvements such as more accessible date selection for current logs, filling in missed logs by selecting “unfilled dates,” and including advanced features like automatic syncing with wearable devices. However, manual input is required due to cost constraints.
Support partners: Participants requested the ability to see team members’ names in the “my team” feature to enhance social interaction.
Discussion
Principal results
This study successfully developed Simple Health, an evidence-based and theory-driven mHealth web app designed to promote healthy eating, increase PA, and reduce sitting time among sedentary employees. The usability evaluation provided valuable insights into how the app was received and which features contributed to its success. Notably, 87.5% of participants found the app easy to use, with an overall ease-of-use score of 2.20 out of 7. Key features such as logging health behaviors were described as simple and intuitive, while the personalized advice feature was praised for its relevance and actionability. These findings suggest that Simple Health has the potential to facilitate behavior change through core components such as goal-setting, behavior tracking, and personalized feedback, all of which are essential for promoting sustainable health behavior change among sedentary workers.
The positive reception of Simple Health supports the notion that mHealth interventions can be practical and effective workplace health tools. By integrating social cognitive theory [20] and the ecological model [21] into its design, Simple Health fosters self-efficacy and self-regulation—two critical factors for long-term behavior change—while also considering environmental influences on behavior. The ecological model emphasizes the influence of environmental factors on behavior, which was reflected in the app’s capacity to provide personalized advice that considered users’ unique environments and resources. This feature played a significant role in boosting users’ confidence in their ability to make healthier decisions, a core component of self-efficacy [20, 22]. These findings align with established behavior change theories, highlighting the importance of self-monitoring, goal-setting, feedback, and environmental support in promoting sustainable health behavior change [8, 22, 29].
Although this study focused primarily on development and usability testing, it did not explicitly evaluate the effectiveness of individual BCTs embedded in the app. This contrasts with de Korte et al. [9], who highlighted that many workplace mHealth apps underutilize effective BCT combinations, limiting their potential to drive behavior change. While Simple Health includes essential BCTs such as self-monitoring, goal-setting, and personalized advice—which received positive user feedback—future studies should further examine how each BCT contributes to long-term engagement and behavior change. The favorable reception of these features suggests that they could contribute to effective behavior change, echoing de Korte et al.’s recommendation that apps designed for employees can benefit from incorporating a more substantial evidence base of BCTs tailored to the workplace context to maximize their impact on health behavior change [9].
Strengths of the study
This study has several notable strengths. Simple Health is grounded in social cognitive theory [20] and the ecological model [21], providing a strong theoretical foundation for promoting sustained health behavior change. Unlike many workplace health apps that focus on a single behavior, Simple Health integrates multiple health domains, addressing PA, sedentary behavior, and dietary habits in a single intervention. This multi-component approach ensures that the app is more holistic and comprehensive than existing workplace wellness apps. The app is also designed to be accessible and user-friendly, making it easy for employees with varying levels of technological proficiency to engage with its features. By incorporating personalized feedback, goal setting, and behavior tracking, Simple Health leverages key BCTs known to be effective in fostering long-term engagement. Furthermore, the app goes beyond individual behavior change by integrating team-based challenges, peer motivation, and social ranking systems, which help foster a supportive workplace culture conducive to sustained participation and adherence.
Limitations
This study has several limitations that should be acknowledged. First, the small sample size (n = 8) restricts the generalizability of the findings. While usability testing with a small number of participants is common in mHealth research and can identify major usability issues [58], the results may not fully reflect the experiences of a broader and more diverse population of sedentary employees. Future studies should include larger and more varied participant groups across different workplace environments to enhance the external validity of the findings.
Second, the short duration of usability testing (five days) limits insights into long-term engagement, adherence, and sustained behavior change. Although participants provided valuable feedback on app usability, the study design did not allow for an extended assessment of whether the app effectively promotes sustained improvements in PA, sedentary behavior, and dietary habits. A longer study period would provide more robust data on user retention, engagement trends, and whether the app’s BCTs remain effective over time.
Third, some participants encountered minor usability challenges related to navigation and goal-setting, which may impact user engagement and ease of use. While overall usability scores were favorable, participants suggested simplifying the mobile menu by reducing the number of layers to improve navigation efficiency. Additionally, one participant noted that the goal-setting feature allowed only a single entry at a time, limiting flexibility in tracking multiple goals concurrently. Although these issues did not present major usability barriers, they indicate areas for refinement that could enhance the app’s user experience and functionality in future iterations. Addressing these concerns could further optimize the app’s ability to support sustained behavior change.
Fourth, manual logging of PA rather than automatic syncing with wearable devices may have affected user adherence and engagement. Self-reporting PA can be burdensome for users, potentially leading to underreporting or inconsistencies in data entry. Integrating the app with wearable devices (e.g., Fitbit, Apple Health, or Google Fit) could enhance tracking accuracy, reduce the user burden, and improve long-term adherence. Future iterations of Simple Health should prioritize automatic data synchronization to increase engagement and ease of use.
Despite these limitations, the study provides valuable insights into the usability and potential effectiveness of an evidence-based, multi-behavior workplace mHealth intervention. Addressing these challenges in future iterations will be essential to optimizing the app’s functionality and effectiveness for workplace health promotion.
Lessons learned
The development and usability testing of Simple Health provided several key insights for refining workplace mHealth interventions. One critical takeaway is the need for automated data entry features, such as integration with wearable fitness trackers (e.g., Fitbit, Apple Health, Google Fit), to minimize user burden and enhance engagement. Users also expressed the need for a more flexible goal-setting system that allows multiple goals to be set and tracked simultaneously, which aligns with research highlighting the importance of customizable self-monitoring tools [60]. Navigation and interface simplicity were identified as essential factors for usability, particularly for mobile users. Overly complex menus can hinder engagement, emphasizing the importance of a streamlined and intuitive design. Additionally, gamification elements (e.g., leaderboards and social challenges) embedded in the “health rankings” feature were positively received but could be refined to increase entertainment value and long-term engagement. Lastly, incorporating interactive data visualization and progress-tracking tools may further support sustained behavior change.
Future of the Simple Health web app
Simple Health has the potential to be widely implemented in workplace health promotion initiatives. The app was successfully used in a mobile health intervention study among sedentary employees (manuscript under review), demonstrating feasibility in a real-world setting. While Simple Health was not developed for a specific enterprise, its adaptability suits various industries and employee populations. Future efforts should focus on scaling the app for broader use, improving its functionalities, and integrating additional features to enhance its effectiveness and user experience.
Regarding public availability, Simple Health could be made accessible to a larger audience; however, its sustainability will depend on funding and resource allocation. Additional support will be necessary to further develop and maintain the app, including securing investment for technical improvements, long-term evaluation, and large-scale dissemination. Given the rising demand for digital workplace wellness solutions, Simple Health has the potential to become a scalable, cost-effective intervention for improving employee health.
Next steps and future research directions
To maximize Simple Health’s impact, several research and development directions should be pursued. Expanding integration with wearable devices (e.g., Fitbit, Apple Health, Google Fit) would improve tracking accuracy and reduce manual data entry, thereby enhancing user engagement. Additionally, refining the gamification elements within the “health rankings” feature could increase motivation and participation. While usability testing demonstrated promising results, future research should examine Simple Health’s effectiveness in larger and more diverse employee populations to determine its generalizability and long-term impact. Longitudinal studies assessing sustained behavior change and engagement over time will be essential for evaluating the app’s long-term viability.
Furthermore, collaborations with organizations and corporate wellness programs would provide valuable insights into organizational adoption, employer engagement, and workplace health outcomes. Future research should also explore cost-effectiveness and potential barriers to adoption, ensuring that Simple Health remains a scalable and sustainable intervention for occupational health promotion.
Implications for health promotion practice
The findings of this study highlight the potential role of mHealth interventions in workplace and community health promotion. Occupational health practitioners and wellness program coordinators could incorporate Simple Health into corporate wellness initiatives to encourage PA, promote healthy dietary behaviors, and reduce sedentary time among employees. The app’s personalized feedback and goal-setting features could be used to enhance employee engagement, improve adherence, and facilitate sustained health behavior change.
As sedentary behavior in workplace settings continues to be a public health challenge, Simple Health presents a promising, evidence-based digital health solution to mitigate these risks. By refining and scaling the app, it has the potential to contribute to healthier work environments, ultimately reducing the burden of sedentary-related health risks and enhancing overall employee well-being. Future developments should prioritize scalability, usability refinements, and workplace integration strategies to ensure widespread adoption and long-term impact.
Conclusions
This study successfully developed Simple Health, an evidence-based and theory-driven mHealth web app designed to promote healthy eating, increase PA, and reduce sedentary time among sedentary employees. The development process was guided by social cognitive theory and the ecological model, ensuring a structured approach to fostering self-efficacy, self-regulation, and environmental support for behavior change. The app integrates key BCTs, such as goal-setting, self-monitoring, and personalized feedback, providing users with tools to track and improve their health behaviors. The usability evaluation provided valuable insights into user experience and areas for refinement. While participants found the app generally intuitive and easy to use, feedback highlighted the need for improved navigation, a more flexible goal-setting function, and potential enhancements such as automatic syncing with wearable devices to reduce manual data entry. These findings underscore the importance of iterative improvements to enhance user engagement and functionality. Future research should focus on testing Simple Health in larger and more diverse workplace settings to evaluate its broader applicability and long-term impact on health behavior change. Additionally, further refinements based on user feedback will help optimize the app’s usability and effectiveness, ensuring it remains a practical tool for workplace health promotion.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all participants who participated in this research. YPL acknowledges the support of the National Science and Technology Council (grant numbers MOST 106-2314-B-039-037 and MOST 107-2314-B-039-009), which funded this study.
Abbreviations
- Apps
Applications
- BCTs
Behavior change techniques
- MAUQ
mHealth app usability questionnaire
- mHealth
mobile health
- PA
Physical activity
Author contributions
YPL, KCL, WFM, BSS, WCL, HTY, SHL, and OSH contributed to the conception and design of the study. YPL and BSS designed the intervention content. BSS collected the data. YPL, SHL, OSH, and BSS analyzed and interpreted the data. YPL prepared the manuscript. All authors provided review and edits of the draft manuscript and approval of the final manuscript.
Funding
This study was supported by the National Science and Technology Council (grant numbers MOST 106-2314-B-039-037 and MOST 107-2314-B-039-009). The funder had no role in the study design, data collection, analysis, interpretation, manuscript preparation, or the decision to submit this article for publication.
Data availability
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Ethics approval for this study was obtained from the China Medical University & Hospital Research Ethics Center (CRREC-106-036 [CR-1]). Written informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yun-Ping Lin, Email: yunping@mail.cmu.edu.tw.
Shu-Hua Lu, Email: shuhua@mail.cmu.edu.tw.
References
- 1.Ganesan AN, Louise J, Horsfall M, Bilsborough SA, Hendriks J, McGavigan AD, Selvanayagam JB, Chew DP. International mobile-health intervention on physical activity, sitting, and weight: the stepathlon cardiovascular health study. J Am Coll Cardiol. 2016;67(21):2453–63. 10.1016/j.jacc.2016.03.472. [DOI] [PubMed] [Google Scholar]
- 2.Jung J, Cho I. Promoting physical activity and weight loss with mHealth interventions among workers: systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2022;10(1). 10.2196/30682. [DOI] [PMC free article] [PubMed]
- 3.Lee M, Lee H, Kim Y, Kim J, Cho M, Jang J, Jang H. Mobile app-based health promotion programs: a systematic review of the literature. Int J Environ Res Public Health. 2018;15(12). 10.3390/ijerph15122838. [DOI] [PMC free article] [PubMed]
- 4.Müller AM, Alley S, Schoeppe S, Vandelanotte C. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):109. 10.1186/s12966-016-0434-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Müller AM, Maher CA, Vandelanotte C, Hingle M, Middelweerd A, Lopez ML, DeSmet A, Short CE, Nathan N, Hutchesson MJ, Poppe L, Woods CB, Williams SL, Wark PA. Physical activity, sedentary behavior, and diet-related eHealth and mHealth research: bibliometric analysis. J Med Internet Res. 2018;20(4). 10.2196/jmir.8954. [DOI] [PMC free article] [PubMed]
- 6.Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, Vandelanotte C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):127. 10.1186/s12966-016-0454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Global Observatory for eHealth. mHealth: new horizons for health through mobile technologies: second global survey on eHealth. World Health Organization; 2011. https://iris.who.int/handle/10665/44607.
- 8.Buckingham SA, Williams AJ, Morrissey K, Price L, Harrison J. Mobile health interventions to promote physical activity and reduce sedentary behaviour in the workplace: a systematic review. Digit Health. 2019;5:2055207619839883. 10.1177/2055207619839883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Korte E, Wiezer N, Bakhuys Roozeboom M, Vink P, Kraaij W. Behavior change techniques in mHealth apps for the mental and physical health of employees: systematic assessment. JMIR Mhealth Uhealth. 2018;6(10). 10.2196/mhealth.6363. [DOI] [PMC free article] [PubMed]
- 10.Di Sebastiano KM, Lau EY, Yun L, Faulkner G. An evaluation of a commercialized mHealth intervention to promote physical activity in the workplace. Front Public Health. 2022;10:740350. 10.3389/fpubh.2022.740350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parés-Salomón I, Señé-Mir AM, Martín-Bozas F, Loef B, Coffey A, Dowd KP, Jabardo-Camprubí G, Proper KI, Puig-Ribera A, Bort-Roig J. Effectiveness of workplace interventions with digital elements to reduce sedentary behaviours in office employees: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2024;21(1):41. 10.1186/s12966-024-01595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Wu L, Lange JP, Fadhil A, Reiterer H. Persuasive technology in reducing prolonged sedentary behavior at work: a systematic review. Smart Health 2018 10.1016/J.SMHL.2018.05.002
- 13.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 14.WHO Guidelines on physical activity and sedentary behaviour. World Health Organization; 2020. https://www.who.int/publications/i/item/9789240015128
- 15.Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, Bradley G, Dunstan DW. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med. 2015;49(21):1357–62. 10.1136/bjsports-2015-094618. [DOI] [PubMed] [Google Scholar]
- 16.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardiovasc Risk Rep. 2008;2(4):292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bort-Roig J, Chirveches-Pérez E, Giné-Garriga M, Navarro-Blasco L, Bausà-Peris R, Iturrioz-Rosell P, González-Suárez AM, Martínez-Lemos I, Puigoriol-Juvanteny E, Dowd K, Puig-Ribera A. An mHealth workplace-based sit less, move more program: impact on employees’ sedentary and physical activity patterns at work and away from work. Int J Behav Nutr Phys Act. 2020;17(23):8844. 10.3390/ijerph17238844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonn SE, Löf M, Östenson CG, Trolle Lagerros Y. App-technology to improve lifestyle behaviors among working adults - the health integrator study, a randomized controlled trial. BMC Public Health. 2019;19(1):273. 10.1186/s12889-019-6595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bandura A. Social cognitive theory: an agentic perspective on human nature. 1st ed. John Wiley & Sons; 2023. ISBN: 978-1-394-16146-1.
- 21.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. [DOI] [PubMed] [Google Scholar]
- 22.Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, Michie S. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. 2019;53(8):693–707. 10.1093/abm/kay078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fiedler J, Eckert T, Wunsch K, Woll A. Key facets to build up eHealth and mHealth interventions to enhance physical activity, sedentary behavior and nutrition in healthy subjects - an umbrella review. BMC Public Health. 2020;20(1):1605. 10.1186/s12889-020-09700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spring B, Schneider K, McFadden HG, Vaughn J, Kozak AT, Smith M, Moller AC, Epstein LH, Demott A, Hedeker D, Siddique J, Lloyd-Jones DM. Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology. Arch Intern Med. 2012;172(10):789–96. 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 26.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1). 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed]
- 27.Zhou L, Bao J, Setiawan IMA, Saptono A, Parmanto B. The mHealth app usability questionnaire (MAUQ): development and validation study. JMIR Mhealth Uhealth. 2019;7(4). 10.2196/11500. [DOI] [PMC free article] [PubMed]
- 28.Willms A, Rhodes RE, Liu S. The development of a hypertension prevention and financial-incentive mHealth program using a no-code mobile app builder: development and usability study. JMIR Form Res. 2023;7. 10.2196/43823. [DOI] [PMC free article] [PubMed]
- 29.Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57(4):660–80. 10.1111/j.1464-0597.2008.00341.x. [Google Scholar]
- 30.Hebden L, Cook A, van der Ploeg HP, Allman-Farinelli M. Development of smartphone apps for nutrition and physical activity behavior change. JMIR Res Protoc. 2012;1(2). 10.2196/resprot.2205. [DOI] [PMC free article] [PubMed]
- 31.Turner-McGrievy GM, Hales SB, Schoffman DE, Valafar H, Brazendale K, Weaver RG, McGrievy MJ. Choosing between responsive-design websites versus mobile apps for your mobile behavioral intervention: presenting four case studies. Transl Behav Med. 2017;7(2):224–32. 10.1007/s13142-016-0448-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harvard TH. Chan school of public health. Healthy Eat Plate. 2011. https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/
- 33.Taiwan Health Promotion Administration. Daily dietary guidelines for Taiwanese. 2018. https://health99.hpa.gov.tw/media/public/pdf/21733.pdf
- 34.Taiwan Health Promotion Administration. Physical activity guidelines for Taiwanese. 2018. https://www.hpa.gov.tw/Pages/EBook.aspx?nodeid=1411
- 35.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. 9th ed. Available at DietaryGuidelines.gov. 2020 Dec.
- 36.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. 2018. https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf [DOI] [PubMed]
- 37.Pedisic Z, Bennie JA, Timperio AF, Crawford DA, Dunstan DW, Bauman AE, Salmon J. Workplace sitting breaks questionnaire (SITBRQ): an assessment of concurrent validity and test-retest reliability. BMC Public Health. 2014;14:1249. 10.1186/1471-2458-14-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Safford MM, Hooker SP. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: a National cohort study. Ann Intern Med. 2017;167(7):465–75. 10.7326/m17-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. Pacific Physical Activity Guidelines for Adults. 2008. http://www.who.int/dietphysicalactivity/publications/pacific_pa_guidelines.pdf [PubMed]
- 40.Mintz Y, Aswani A, Kaminsky P, Flowers E, Fukuoka Y. Behavioral analytics for myopic agents. Eur J Oper Res. 2023;310(2):793–811. 10.1016/j.ejor.2023.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pan WH, Report on the results of the National Nutrition and Health Survey. (2013–2016). Health Promotion Administration, Ministry of Health and Welfare. 2017. https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=~/File/Attach/11145/File_12788.pdf
- 42.Taiwan Health Promotion Administration. Let’s move toward a healthy life (p.15). 2014. https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=~/File/Attach/6100/File_5988.pdf
- 43.Smith L, Hamer M, Ucci M, Marmot A, Gardner B, Sawyer A, Fisher A. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office-based workers: the active buildings study. BMC Public Health. 2015;15:9. 10.1186/s12889-014-1338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cancer Care Foundation, Huang CH, Huang SY. The latest food substitution guide: be your own nutritionist. My House; 2019.
- 45.Taiwan Health Bureau, Nantou County Government. Daily dietary guide: food reference atlas. 2018. https://health99.hpa.gov.tw/storage/pdf/materials/21974.pdf
- 46.Taiwan Vegetarian Nutrition Society. Energetic and healthy plant-based diet. 2015. https://www.twvns.org/flyer/nutritionflyer/286-2015-10-14-07-33-54.
- 47.Taiwanese Association of Diabetes Educators. In-depth nutritional analysis of Taiwanese snacks– Southern Taiwan edition. Author; 2011.
- 48.Taiwanese Association of Diabetes Educators. In-depth nutritional analysis of Taiwanese snacks– Northern Taiwan edition. Author; 2015.
- 49.Taiwanese Association of Diabetes Educators. In-depth nutritional analysis of Taiwanese snacks– Central Taiwan edition. Author; 2015.
- 50.Taiwanese Association of Diabetes Educators. Carbohydrate counting: food nutrition atlas. Author; 2016.
- 51.Taiwanese Association of Diabetes Educators. Heart-healthy and brain-boosting recipes. Mediterranean & DASH diets. Author; 2017.
- 52.Op den Akker H, Cabrita M, Op den Akker R, Jones VM, Hermens HJ. Tailored motivational message generation: a model and practical framework for real-time physical activity coaching. J Biomed Inf. 2015;55:104–15. 10.1016/j.jbi.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 53.Dishman RK, DeJoy DM, Wilson MG, Vandenberg RJ. Move to improve: a randomized workplace trial to increase physical activity. Am J Prev Med. 2009;36(2):133–41. 10.1016/j.amepre.2008.09.038. [DOI] [PubMed] [Google Scholar]
- 54.Welk GJ, Differding JA, Thompson RW, Blair SN, Dziura J, Hart P. The utility of the Digi-walker step counter to assess daily physical activity patterns. Med Sci Sports Exerc. 2000;32(9 Suppl). 10.1097/00005768-200009001-00007. [DOI] [PubMed]
- 55.Chou CC, Chan CH. A study on 10,000 steps/day for health promotion. J Phys Educ Sport Sci. 2009;(9):36–45. 10.6634/JPSS-CCU.200912.09.04.
- 56.Kennedy ET, Ohls J, Carlson S, Fleming K. The healthy eating index: design and apps. J Am Diet Assoc. 1995;95(10):1103–8. 10.1016/s0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 57.Svetkey LP, Simons-Morton D, Vollmer WM, Appel LJ, Conlin PR, Ryan DH, for the DASH Research Group. Effects of dietary patterns on blood pressure: subgroup analysis of the dietary approaches to stop hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285–93. 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 58.Nielsen J. How many test users in a usability study? 2012. https://www.nngroup.com/articles/how-many-test-users/
- 59.Bailey DP. Sedentary behaviour in the workplace: prevalence, health implications and interventions. Br Med Bull. 2021;137(1):42–50. 10.1093/bmb/ldaa039. [DOI] [PubMed] [Google Scholar]
- 60.Alshagrawi S, Abidi ST. Efficacy of an mHealth behavior change intervention for promoting physical activity in the workplace: randomized controlled trial. J Med Internet Res. 2023;25:e44108. 10.2196/44108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this study’s findings are available from the corresponding author upon reasonable request.