Göran B. Klintmalm, MD, PhD
Transplanting organs, replacing old worn-out organs with healthier ones, has long been a dream in medicine. Several attempts were made in 1901 in Vienna, where investigators tried to transplant kidneys in dogs, pigs, goats, and calves. The exercise turned out to be purely technical due to the lack of understanding of vascular surgical techniques, organ preservation, and immunosuppression. In 1902, Dr. Alexis Carrel developed the technique of vascular suturing that in principle is still in practice today. Dr. Carrel developed the technique when, in his attempts at transplanting kidneys to the neck of dogs, he found that the organs thrombosed. Believing that the transplants failed due to a simple technical problem, he developed the vascular surgical technique. Thanks to Dr. Carrel, vascular surgery began to develop, but transplantation still had a long way to go.
In 1933, the first real attempt at transplanting a human kidney to a human patient was done by Dr. YuYu Voronoy in Russia. A kidney was taken from a recently deceased individual and connected to a young woman who was suffering from lead poisoning. No immunosuppression was given. The kidney never functioned. In 1948, Sir Peter Medawar performed experiments that for the first time defined the immunology of transplantation and began to define rejection. For his pioneering work in transplant immunology, Dr. Medawar received the Nobel Prize in Medicine in 1958.
In the early 1950s, Dr. Rene Küss in Paris and Dr. David Hume in Boston began earnest attempts at transplantation. The first recorded event in which a transplanted kidney functioned was in 1951. Dr. Küss transplanted the kidney to the iliac fossa, as is done today. One of the 5 transplanted kidneys worked for 2 months without immunosuppression, when it rejected and thrombosed. In contrast, Dr. Hume placed 6 kidneys subcutaneously in the thigh, with 3 having temporary function. In 1954 at Brigham Hospital in Boston, Dr. Joseph Murray performed the first successful human kidney transplant. A patient with chronic renal failure received a kidney from his identical twin brother. Technically, the transplant was a success, and since the donor was an identical twin, no rejection was seen even though the patient did not receive immunosuppression. This remarkable event proved several things. First, organ replacement could cure a patient; second, organ transplantation was technically feasible; and third, organ transplantation offered a permanent cure of the disease itself. Dr. Joseph Murray and Dr. E. Donnall Thomas received the Nobel Prize for the development of clinical transplantation in 1990.
The immune system presented a formidable obstacle for successful transplantation. In the late 1950s, experiments with irradiation were done to induce allograft tolerance. However, irradiation had acute toxicities, and most of the patients died from the effects of the exposure. In 1959 and 1960, Dr. Roy Calne, a young British surgeon doing a fellowship with Dr. Murray in Boston, used a new compound supplied to him by Burroughs and Wellcome. The drug was azathioprine, an imidazole derivative of 6-mercaptopurine, which was known to be immunosuppressive in kidney transplantation of the dog. Unlike 6-mercaptopurine, which had to be given intravenously, azathioprine could be given orally. Dr. Calne performed experiments that showed that the drug was indeed extremely powerful in dogs and could prevent rejection. With these findings, the foundation for chemical immunosuppression was laid. Shortly after Dr. Calne's return to the United Kingdom, he was appointed chairman and chief of surgery at Cambridge University. Dr. Murray rapidly began to exploit this new drug, which was later to be registered under the name Imuran, but he found that the drug had significant clinical toxicities that limited its use. Very few patients tolerated the doses of Imuran that would prevent organ rejection. When rejection occurred, the grafts were always lost.
The situation changed overnight when a young surgeon by the name of Dr. Thomas E. Starzl in Denver presented to the National Institutes of Health a stack of rolled-up wall charts outlining the astonishing results that he had achieved by using a combination of azathioprine and prednisone. By adding prednisone to the azathioprine, he not only lessened the risk of rejection but could treat any rejection that did occur with large doses of the steroid. The rejection would then abate, and the graft was accepted with long-term function.
The 1963 publication of Dr. Starzl's study in Surgery, Gynecology, and Obstetrics skyrocketed the interest in transplantation. Fearless surgeons and physicians along with brave patients began to experiment with organ transplantation and immunosuppression. New forms of immunosuppression, such as thoracic duct drainage (Franksson, 1964) and antilymphocyte globulin (Starzl, 1967), became adopted in the community of investigators throughout the world. The work presented by Belzer (1968) and Collins (1969) in organ preservation was another milestone. Organs could now be retrieved at one location and transported to the site of the recipient surgery.
With rudimentary but functioning immunosuppression, a rapid evolution ensued. Dr. Starzl did the first liver transplants in humans in 1963, followed by Dr. Calne in 1968 and by Dr. Rudolf Pichlmayr in Hanover in 1971. When Dr. Christiaan Barnard performed the first successful heart transplant in humans in 1967 in South Africa, the public became aware of the potential of organ transplantation. The first attempts at pancreas transplantation were done by Dr. C. Walton Lillehei in Minnesota in 1966. In that same year, Dr. Lillehei performed the first small intestinal transplant.
The early 1970s saw continued efforts with immunosuppression and tissue typing/matching. However, in 1978, immunosuppression was still so poor that the 1-year graft survival rate for cadaveric kidneys in the USA was reported at 47%. That same year, patient mortality was reported at 30%. Maintenance immunosuppression was too weak to prevent rejection. When rejection occurred, the treatment necessary to turn the rejection around brought with it frightful consequences. In 1978, liver transplantation was only practiced with any regularity in 3 centers—Denver, Colorado; Cambridge, UK; and Hanover, Germany—and had an approximate 75% mortality rate. Heart transplantation, which had been started with a worldwide flurry after Dr. Barnard's highly publicized cases, quickly slowed as the patients succumbed. By the late 1970s, few were attempting to do the operation. Dr. Norman Shumway, who initially developed the technique for heart transplantation and who taught Dr. Barnard, continued in his tireless efforts. He was exceeding a 70% 1-year survival. Pancreas transplantation suffered from poorer results with <10% 1-year graft survival with whole organ grafts worldwide. Transplant surgeons were seen as daredevils working at the fringe of science, often working against the advice of less visionary, but highly outspoken, critics. To be a transplant surgeon was something that very few embraced because of the strenuous effort that was required and the discouraging results.
The revolution in transplantation occurred in May 1978 when for the first time Dr. Calne used a new immunosuppressive fungal metabolite discovered by Sandoz. The drug, cyclosporine, changed the history of organ transplantation. In a few short years, aggressive exploratory studies with this drug allowed the pioneers of transplantation to rapidly move forward. Literally overnight, the graft survival rate for kidney transplantation increased to >70% with a mortality rate of ≤10%. The survival rate of liver transplant recipients quickly reached 80%, and so did the survival rate of heart transplant recipients. Pancreas transplantation, which had suffered from almost universal failure, now suddenly began to see consistent survival rates and improving results. In 1982, Dr. Bruce Reitz presented the first series of successful heart-lung transplants using cyclosporine and prednisone. In 1984, the Food and Drug Administration approved the wonder drug under the trade name Sandimmune.
BAYLOR'S INVOLVEMENT
Dr. John Fordtran, who became chairman of the department of medicine at Baylor University Medical Center (BUMC) in 1979, traveled to Denver in 1971 so his son Bill could receive a kidney transplant. After an initial failure, the transplant was successful. Bill later worked at Baylor for many years. A secondary result of Dr. Fordtran's trip to Denver was a close friendship with Dr. Thomas Starzl. As a result of the enthusiastic reports coming not only out of Pittsburgh, where Dr. Starzl moved in 1981, but also from other universities in San Francisco, Minneapolis, and Boston, Dr. Fordtran invited Dr. Starzl to give medical grand rounds at BUMC in November 1983. Dr. Starzl gave an electrifying presentation about the success that was being seen with liver, kidney, heart, and lung transplantation at the University of Pittsburgh. After the presentation, Dr. Starzl told Dr. Fordtran, Dr. Jesse Thompson (chairman of the Department of Surgery), and Boone Powell, Jr., that BUMC should consider starting a transplant program since there was not a liver transplant program in the entire Southwest. Dr. Starzl offered to be a consultant and assist in the recruitment of an elite surgeon for a liver/kidney program. He would also serve as an advisor in setting up the program.
After Dr. Starzl returned to Pittsburgh, the medical staff and administration of BUMC discussed their interest in pursuing transplantation. Discussions had been held previously in 1980 about the possibility of having a kidney transplant program, but at that time the decision was against a program. However, with the revolutionary advancements in drug therapy and with the offer of assistance from the leading transplant surgeon in the USA, all parties felt that BUMC was ready to embark on this journey. A unanimous decision was made that the program should be scientifically based, with a strong academic component. It was also decided that an institutional committee be organized to recruit the lead surgeon, as well as to ensure that the program received the support necessary from the various services. This committee would later become the transplant review committee. The committee quickly focused only on liver and kidney transplantation, as the recruitment for heart transplantation was being pursued separately.
When discussing potential surgeons to fill the critical lead position, the committee turned to Dr. Starzl. Dr. Starzl supplied the committee with two names, Dr. Göran Klintmalm of Stockholm, Sweden, who had trained with him in Denver and followed him to Pittsburgh, and Dr. Roger Jenkins, whom he had also trained, at Harvard Medical School. The key component in the selection process was to find a liver transplant surgeon who could undertake this truly monumental effort. In January 1984, there was still a short list of transplant centers across the USA, including Pittsburgh, the University of California Los Angeles, Memphis, and Minnesota. A new European program had recently been started by one of Dr. Starzl's earlier fellows, Ruud Krom. Thus, the number of potential recruits was small, and the only surgeons that could be considered were those who had previously been trained by the trio of Drs. Starzl, Calne, or Pichlmayr. The plan from the beginning was to have the kidney program be a part of an abdominal transplant program that would be handled by the same surgical team. This was feasible because at the time, all liver transplant surgeons came from a background of kidney transplantation.
In early February 1984 with Baylor's approval, Dr. Starzl called me in Stockholm. The call came around 11:00 PM to my home. When I answered, Dr. Starzl began talking without introducing himself, as had become his custom and privilege. Dr. Starzl bluntly asked if I knew about BUMC, and my answer was that I thought I had heard the name Baylor before. He said, “It is in Dallas, which is in Texas. It is a great institution, and they want to start a transplant program. Are you interested?” When dealing with Dr. Starzl, one is never given much time to make up one's mind, and my response was that I was interested. Within a couple of days, arrangements had been made for my wife and me to travel to Dallas for a site visit.
During my visit, all people with an interest in transplantation, both positive and negative, met me. It was clear that Baylor wanted to have a first-rate program. Specifically, Drs. John Fordtran, Alan Hull, Marty White, Tom Parker, Daniel Polter, Kent Hamilton, Daniel DeMarco, George Race, Weldon Tillery, Herbert Steinbach, Jerome Arndt, Robert Thompson, Michael Ramsay, and Jesse Thompson were extremely supportive and would be key components for a successful endeavor. Dr. Thompson had aligned the support of all the general and vascular surgeons to be available for donor and recipient surgeries. Boone Powell, Jr., and his assistants Robert Hille and Glen Clark looked at the administrative aspects of such a program and offered full and unequivocal support. The president of the Baylor Foundation, Boone Powell, Sr., was also behind the endeavor.
My wife, Tina, was given a similar whirlwind tour. She was taken care of by an equally large and more charming group of wives. She was told in no uncertain terms that you could live very well in Dallas, as there was good housing, you could raise children here, and there were good schools. Mrs. Thompson, Mrs. Lieberman, Mrs. Paulson, Mrs. Stone, and Mrs. Powell played an active part in Tina's visit.
Upon returning to Stockholm, Tina and I had a short but intense discussion about the opportunity presented to us. We decided to accept the offer. With the assistance of lawyers, my Pennsylvania medical license was reciprocated to a Texas medical license, and an immigration visa was obtained. A 1-page letter from Boone Powell, Jr., stating Baylor's position in general terms was sent to me; a contract was never written. In August 1984 on my second site visit to Baylor, Mr. Powell, Jr., and I simply shook hands, thereby sealing the agreement. The outline of the agreement followed the conditions offered to assistant professors recruited to the University of Pittsburgh in 1984. One additional stipulation was that we would also provide fellowship training for Pittsburgh fellows, who could rotate in Dallas.
I returned to Sweden and defended my PhD thesis, “Cyclosporin A Nephrotoxicity in Human Transplant Patients: Clinical, Pharmacological, and Morphological Findings” on September 21. Upon completion of this task, I was free to get my life in order for departure for the USA on December 3, 1984. Tina would not accompany me immediately to the USA, however, as she was pregnant with our second son at the time and would stay in Sweden until his delivery. Since she would be staying for a short time in Sweden, we had to pack some things not only for our new home in the USA, but also for a smaller apartment in Sweden for Tina and our first son. It was quite a busy time for me personally, yet between packing I assisted in planning and performing the first liver transplant in Sweden in November 1984.
On December 4, 1984, I returned to the University of Pittsburgh to learn all of the new developments that had taken place since I left in July 1981. Monumental improvements in the technique of transplantation had been designed, such as the venavena bypass by Denmark in 1982, which made the surgeries much safer. A new immunosuppressant drug, the monoclonal antibody OKT3, was being introduced. This drug gave us a very powerful tool to treat difficult rejections. During my second tenure in Pittsburgh, I made frequent trips to Dallas to complete the immediate preparations for the Baylor program. It was on one of these trips to Dallas that the very first liver transplant was performed, almost as an accident, at BUMC on December 18, 1984.
On January 31, 1985, my wife called me in Pittsburgh telling me that it was time for the delivery of our second son. I took the next flight out on February 1, arriving on a snowy Saturday morning, February 2, in Stockholm. Our second son was born on February 3, 1985. Following his baptism 1 week later, I returned to Pittsburgh, leaving behind my wife and 2 sons. On March 21, 1985, my family joined me in Dallas to begin our new life.
THE BEGINNING
I had traveled to Baylor for a second planning visit to supervise transplant preparations. I met with the head nurse for the operating room and with Dr. Jesse Thompson's scrub nurses to select the instruments we would borrow to make up the trays that would be needed for transplantation. I had long meetings with Dr. Jesse Thompson and Dr. John Preskitt. They organized lists of Baylor vascular and general surgeons who were willing to offer their time to participate and assist with the transplants. Two teams were organized, one headed by Dr. John Anderson and one by Dr. Butch Derrick. Each team was to arrange for 2 of their 10 members to be available at each transplant. One team focused on the donor and the other on the recipient. They would alternate responsibilities. These teams, which were given the name of surgical support group, not only provided surgical manpower for the extremely long transplant operations (then 8 to 15 hours) but also provided the camaraderie and support that I needed as an outsider and foreigner to be able to integrate into the Department of Surgery. The surgical support groups were without question one of the most important factors in the success that Baylor was about to experience. We had the manpower that allowed us to do an unlimited number of transplants when donors became available, even though we had only 1 attending surgeon and a fellow, Dr. Arthur Moore, from Pittsburgh.
Dr. Michael Ramsay took the challenge of anesthesia for the liver transplants. He was recruited in 1976 by Dr. Roy Simpson from London to Baylor. Dr. Ramsay's involvement in transplantation from the very beginning is undoubtedly one of the most important factors in the success we have achieved. His happy, smiling sidekick, Dr. Tom Swygert, who was just completing his residency, was always ready for a challenge and offered to be the number two man on the anesthesia team. Dr. Swygert went to Pittsburgh, where he participated in several transplants before the program was finally launched at Baylor a few months later.
I also met with Drs. Dan Polter, Kent Hamilton, and Dan DeMarco during my second visit at BUMC to discuss the organization of the pretransplant workup. We decided that gastroenterology/hepatology should oversee all workups, with the transplant surgeon providing consultations only. All transplant candidates would be presented to a multidisciplinary selection committee. The purpose was to give every patient a broad review but also to assure the institution that only appropriate patients were being transplanted.
I had important discussions with Drs. Marty White and Tom Parker regarding the kidney transplant selection and immunesuppression regimens. With Dr. George Race and Dr. Weldon Tillery in pathology, we arranged that all chemistry specimens would receive special handling to guarantee the results early in order to detect rejections and thus adjust the immunosuppressive drugs to treat rejections before they became life threatening. Dr. Race and his vision as a pathologist was another reason for the success of the transplant program.
Similar discussions were held with Drs. Herbert Steinbach, Jerome Arndt, and Norman Diamond of radiology. The importance of expeditious radiological examinations, both diagnostic and interventional, was understood since the postoperative events could be quite swift and problematic if not treated promptly.
After 2 busy days, I was ready to return to Pittsburgh on December 22, 1984. I was waiting in Boone Powell's office and chatting with Susan Allen, Judy Williams, and Dr. Fordtran, as Mr. Powell was out buying Christmas presents, when the phone rang. It was Dr. Starzl, and without wasting any time, he said that he had an organ donor in Hamilton, Canada. The intended recipient, Amie Garrison, was a 4-year-old girl who was sitting in an aircraft on the tarmac in Peoria, Illinois, waiting for instructions on where to go. Dr. Starzl said that due to the recent extreme transplant activities in Pittsburgh, there was not a single bed in the intensive care unit (ICU) there that would allow the girl to be admitted before or after the transplant. He had just spoken with Walter Andrews, who had done the first liver transplant at Children's Medical Center in Dallas on October 29, 1984. They didn't have any ICU space either. With Tom's usual tendency to come up with innovative solutions, he quickly concluded that the transplant should be done at BUMC. He said, “This is the girl's only chance. She has just been here with spontaneous bacterial peritonitis, for which she just barely recovered.” Almost as an afterthought he added, “She is quite a special person, you know. She lit the Christmas tree at the White House a couple of weeks ago, and First Lady Nancy Reagan was especially concerned for her and made a personal plea.” He also told me that he would fly to Hamilton, Canada, himself and get the liver to bring it to Dallas. He would bring with him a surgical, anesthesiology, and perfusion team.
This was clearly one of those life-changing decisions. Had I said no, Tom would have lost some of his enthusiasm and hope for Baylor to become a functioning program, and we would have lost some of his support. The high risk of failure brought along with it the risk of adverse publicity, which could even jeopardize the program. Dr. Fordtran quickly called in a select group of physicians. We were unable to reach Mr. Powell, as these were the days before cell phones and pagers that worked outside the hospital. Among those called to come in were Drs. Marvin Stone, Donald Paulson, Marty White, Jesse Thompson, Dan Polter, and Allan Bookatz. The discussion of pros and cons was still waging when a cheerful Mr. Powell came into the office, swinging his Christmas loot. Seeing our group in his office stopped him mid-stride. A very quick discussion was held, and I called Dr. Starzl to verify some of the details, including the team that he would bring with him; I then promised to call him back. The advantages and dangers were intensely discussed, and then Boone turned to me and said, “This must be your decision.” I was fully aware of the threat of the press, having experienced it firsthand in Pittsburgh when we started the transplant program. If we didn't do the transplant, Amie would die, and if we did do it and it failed, at least we tried. We needed to show our faith in Dr. Starzl's judgment in even calling us. It was unanimously agreed upon, and I called Dr. Starzl to tell him that we approved the plan. This entire scene took place in a time span of no more than 20 minutes.
Several events surrounding the transplant now belong to Baylor history. Dr. Starzl went with his team to Hamilton in Canada to procure the liver and then headed for Dallas. When they requested permission to land at Love Field, they were told to go to Dallas/Fort Worth International Airport since it had customs services. In those days, the maximum allowable preservation time for livers was approximately 6 hours or, if you really pushed it, 8 hours. The flight time alone was in excess of 3 hours; thus, to go to DFW and through customs was out of the question. As Dr. Starzl loves to tell the story, “I called the White House, and a subsequent call from the First Lady took care of that problem for us.” A second noteworthy event occurred upon the transplant team's arrival at Love Field. They were met by an entire squad of police cars to clear the roads and by buses to bring the team members with the liver to Baylor. In one of the police cars was Robert Hille, a senior vice president of Baylor. We were in constant radio contact with the team as they traveled to Baylor through Dallas with lights and sirens in the middle of the night. We heard Mr. Hille's voice over the radio saying, “They are slowing down. They are slowing down. They are stopping at a doughnut shop!” As was often his custom, Dr. Starzl was beginning to get hungry and knew that there were several hours of hard work ahead of him, so when he saw his favorite food group, the doughnut, being offered, he simply stopped and got a box of doughnuts and coffee for everyone.
In the meantime, Amie Garrison had arrived with her parents and was admitted. She was brought to the preoperative holding area when the transplant team was on its way to Baylor. Because of my experience in Pittsburgh in 1981, with the press going so far as to steal white lab coats in order to get a picture or interview of the family and the transplant team, we sealed off the central surgical area. The personnel that arrived the next morning were scared to find uniformed police at all stairwells and elevators leading to the surgical area. Many of them thought there had been another presidential incident or some other calamity in Dallas during the night.
Amie was taken to operating room 5 in Truett Hospital, Dr. Thompson's own operating room. This room had every vascular instrument available at Baylor at the time. Dr. Starzl arrived with the team, Amie was anesthetized, and the transplant was done. During the operation, we found a 3-cm abscess behind the caudate lobe that clearly was the source of Amie's previous abdominal sepsis and her possible future demise, just as Dr. Starzl had predicted. During the anhepatic phase, when the old liver had been removed and the new liver was just introduced into the abdomen but had not been sewn into place, we suddenly saw massive blood loss from the upper vena cava. This turned out to be an angled DeBakey clamp from Dr. Thompson's primary vascular set; the jaw had broken. Dr. Thompson profusely apologized for the failure of his instruments.
Otherwise, the transplant went beautifully. Amie Garrison was transported to the ICU in Hoblitzelle Hospital, where we again sealed off the area from any outsiders. She was cared for not only by virtually the entire hospital staff but by the city and nation as well. The morning following the transplant, Dr. Starzl assembled the team that had traveled with him and returned to Pittsburgh, leaving me behind (Figure 1). Amie recovered quickly postoperatively, and the liver functioned immediately. Boone Powell, Jr., personally went out to buy her and her family Spaghettios because that is what she wanted to eat.
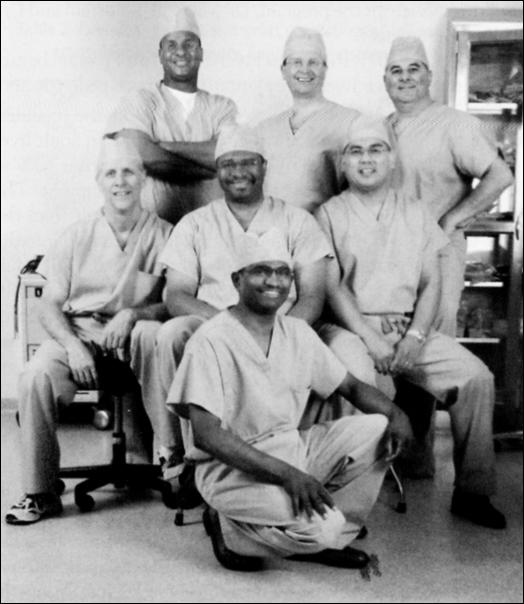
Figure 1.
The team of the first liver transplant at BUMC. Dr. Starzl is in the middle, and Dr. Klintmalm is second from the right.
I experienced one of the most memorable Christmases of my life. Only planning to be here for 2 days, I had brought a small amount of carry-on luggage with me, but Susan and Judy in Mr. Powell, Jr.'s office, along with many others, provided me not only with fresh clothes but also with the Christmas spirit. Dr. John Anderson and Vice President John Carver both invited me into their homes and to attend church with them. During the days between Christmas and the New Year, Amie quickly regained her strength, and I wanted to get Amie to Pittsburgh. Rejections begin to occur in this period, and if the rejection was severe enough, especially in a child, the steroid therapy may not be enough to turn the rejection around. Thus, on December 27, I returned to Pittsburgh on a Lear jet with Amie and her family. She did indeed reject almost immediately upon our arrival in Pittsburgh. A few days later she was started on OKT3, and this reversed her rejection.
Ms. Garrison is still alive and has a child of her own. She currently lives in Jeffersonville, Indiana. She stopped taking immunosuppression on her own accord and dropped out of any follow-up several years ago, but she still stays in contact with us. Thus, this very dramatic transplant not only had a happy ending but also provides us with an example of permanent immune tolerance that developed.
On March 9, 1985, I permanently took up residence in Dallas. Dr. Arthur Moore, a second-year fellow in the Pittsburgh transplant program and a talented surgeon with a great future, traveled with me to Dallas. He was willing and interested in helping set up the program. On April 22, 1985, BUMC performed its first “official” liver transplant on Franklin Findley, who suffered from primary biliary cirrhosis (Figure 2). Mr. Findley had been on the liver transplant waiting list at the University of Pittsburgh and was offered the opportunity to come to Baylor for a transplant by Dr. Starzl. The donor liver was retrieved by one of the teams from Pittsburgh and flown to Dallas. The transplant was a suecess, and over the next 9 weeks, 9 transplants were done. For the first 2 transplants, Dr. Starzl came down with the liver and provided invaluable support. Then we were on our own. By June 1985, the transplant team began to establish a rhythm for the transplant process. The support group system proved its worth time and again, allowing a single transplant surgeon and a single fellow to do 2 transplants in 1 day, which was a huge task back then. Our experience grew rapidly and made each successive transplant faster and easier. Unfortunately, Mr. Findley died 6 weeks after the procedure from a cytomegalovirus infection. No treatment was available for cytomegalovirus in those days, and he succumbed to the disease after having experienced several rejections, even after OKT3 treatment. However, several other successful transplants had been done at the time of his demise, allowing the program to grow despite the setback. On July 1, 1985, Dr. Moore returned to Pittsburgh to begin a training program in cardiac surgery, which was his ultimate goal. Fate had it that Dr. Moore was subsequently killed in a car crash when his small Triumph TR6 was hit by a dump truck that ran a stop sign. He left behind a wife and young son, whom he had seen only twice. There were great expectations of Dr. Moore, who was an exceptionally talented physician and surgeon.
Figure 2.
Intraoperative picture from the first “official” liver transplant, April 22, 1985.
Dr. Andreas Tzakis followed Dr. Moore as the next transplant fellow. Dr. Tzakis had been training in Pittsburgh for 3 years when he was given the opportunity to come to BUMC. He stayed with us until August 1985. During his tenure here he performed his first 3 liver transplants as a surgeon. He then returned to Pittsburgh to become one of the most important surgeons in the Pittsburgh transplant program and subsequently the director of one of the world's leading transplant programs at the University of Miami.
Table 1 shows the fellows who have trained at BUMC. The first 4 were fellows of the joint Pittsburgh/Baylor program. Because of the difficulties of uprooting fellows and their families when the fellows would train in one location for a year and move to the other location for the second year, it was eventually decided to separate the two programs. Since 1986, Baylor has had its own training program in liver and kidney transplant surgery. The table also shows the last known occupation as of July 2001 of the transplant fellows. Many of the fellows are directing their own liver transplant programs and have been quite successful in doing so. Others found that their interests have changed over the years and have taken different paths pursuing successful careers in other fields. To actually perform your first liver transplant as a surgeon was a major event in those days and quite a rare feat. Because of this, we designed a certificate entitled the “I Did It” award that was presented to fellows after completing their first transplant. The ceremony to present the award was always a major affair and was held at one of the upscale restaurants in Dallas with the attending surgeons, surgical fellows, and their spouses participating. We have given out 28 certificates through July 2001.
Table 1.
Fellows trained in transplant surgery at Baylor University Medical Center
| Fellow | Time at BUMC | Current location |
| Andreas Tzakis, MD | 07/1985–08/1985 | University of Miami, Miami, Fla |
| Joseph Nery, MD | 05/1986–12/1987 | University of Miami, Miami, Fla |
| Robert Goldstein, MD | 07/1987–06/1988 | Baylor Regional Transplant Institute, Dallas, Tex |
| Steve Poplawski, MD | 07/1987–06/1989 | West Olive, Mich |
| Joe Cofer, MD | 07/1988–06/1990 | University of Tennessee, Chattanooga |
| Harvey Solomon, MD | 07/1989–06/1991 | St. Louis University Hospital, St. Louis, Mo |
| Eytan Mor, MD | 07/1989–06/1991 | Tel-Aviv University, Beilinson Hospital, Israel |
| Michael Homan, MD | 07/1990–06/1991 | Harrisburg Hospital, Harrisburg, Penn |
| John Gibbs, MD | 07/1990–06/1992 | Roswell Park Cancer Institute, Buffalo, NY |
| Robert McMillan, MD | 07/1991–06/1992 | Louisiana State University, Shreveport |
| Marlon Levy, MD | 07/1991–06/1993 | Baylor Regional Transplant Institute, Fort Worth, Tex |
| Lars Backman, MD, PhD | 07/1991–06/1993 | Sahlgrenska Hospital, Gothenburg, Sweden |
| Caren Eisenstein, MD | 07/1992–06/1993 | Fort Worth, Tex |
| Tom Renard, MD | 07/1992–06/1993 | Dallas, Tex |
| Dale Distant, MD | 07/1992–06/1993 | State University of New York, Brooklyn |
| Marwan Abouljoud, MD | 07/1993–06/1994 | Henry Ford Medical Center, Detroit, Mich |
| David Mulligan, MD | 07/1993–06/1995 | Mayo Clinic Hospital, Scottsdale, Ariz |
| Stig Holmberg, MD, PhD | 07/1994–04/1995 | Molndal Hospital, Molndal, Sweden |
| Mohan Vodapally, MD, PhD | 07/1995–06/1996 | |
| Osman Abbasoglu, MD | 07/1995–06/1997 | Hacettepe University, Ankara, Turkey |
| D. Rohan Jeyarajah, MD | 07/1996–06/1997 | University of Texas Southwestern Medical Center, Dallas |
| Giuliano Testa, MD | 07/1996–06/1998 | University of Illinois at Chicago |
| Ghapjoong Jung, MD | 08/1998–07/2000 | Dong-A University Hospital, Pusan, South Korea |
| Shigeru Marubashi, MD | 04/1999–06/2001 | Osaka, Japan |
| Edmund Sanchez, MD | 07/1999–06/2001 | Baylor Regional Transplant Institute, Dallas, Tex |
| Brian Gogel, MD | 07/2000–06/2001 | Dallas, Tex |
| Mark Thomas, MD | 07/2001–06/2003 | University of Cincinnati, Cincinnati, Ohio |
| Nicholas Onaca, MD | 07/2001–12/2002 | Baylor Regional Transplant Institute, Dallas, Tex |
| Takehisa Ueno, MD | 02/2002–present | |
| Vandad Raofi, MD | 07/2002–08/2003 | Dallas, Tex |
| Patrick Martin, MD | 01/2003–present |
The transplant program rapidly grew. Forty-two liver transplants were done between April 22 and December 31, 1985. This was an incredible volume for a new program. On January 12, 1991, the program performed its 500th liver transplant. Number 1000 came on June 6, 1994; number 1500 on May 14, 1998; and the 2000th liver transplant was performed February 4, 2002 (Figure 3).
Figure 3.
Dr. Klintmalm with the first and 2000th liver transplant recipients.
LIVER TRANSPLANTATION
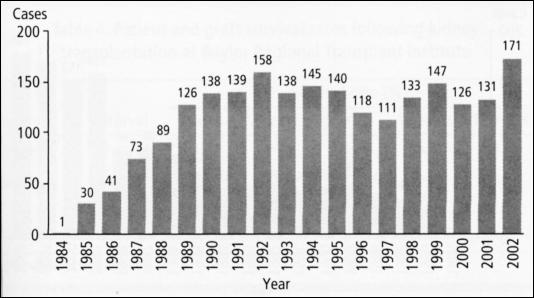
Figure 4 outlines the number of liver transplants performed each year at Baylor. The busiest year was 1992, when 158 liver transplants were done at BUMC. Up until 1992, we had been the only active program in the Southwest, but other programs were established elsewhere and began to utilize the donor supply, which is the growth-limiting factor in transplantation. When the program started, a few days to a few weeks was all that was needed to find a liver for a recipient. In 2001–2002, the average waiting time for a nonurgent patient was 336 days (median, 227 days) compared with 23.9 days (median, 12 days) in 1986–1987. Thus, the patients are in far worse shape going into surgery. The ability of the hepatologists, gastroenterologists, nephrologists, pulmonologists, and other specialists to keep patients alive and in condition has reached previously unattainable levels. Even though sicker patients are transplanted, the mean length of hospital stay as well as the mean length of ICU stay has decreased. The mean length of stay in 1986 was 32.4 days compared with 12.9 in 2000. Most importantly, the patient and graft survival, which was high from the beginning, has continued to improve.
Figure 4.
Annual volume of activity in liver transplantation at Baylor Regional Transplant Institute.
With increased donation awareness and with better knowledge in the selection of marginal donors, the volume of liver transplantation picked up again. In 2002, a total of 171 liver transplants were performed at BUMC in Dallas and Baylor All Saints Medical Center in Fort Worth combined; our limiting factor today continues to be donor availability.
Until May 2003, a total number of 2232 liver transplants were performed at Baylor in adults. Retransplants accounted for 201 adult cases (9%). Combined liver-kidney transplantation was performed in 54 cases and liver-kidney-pancreas in 1 case.
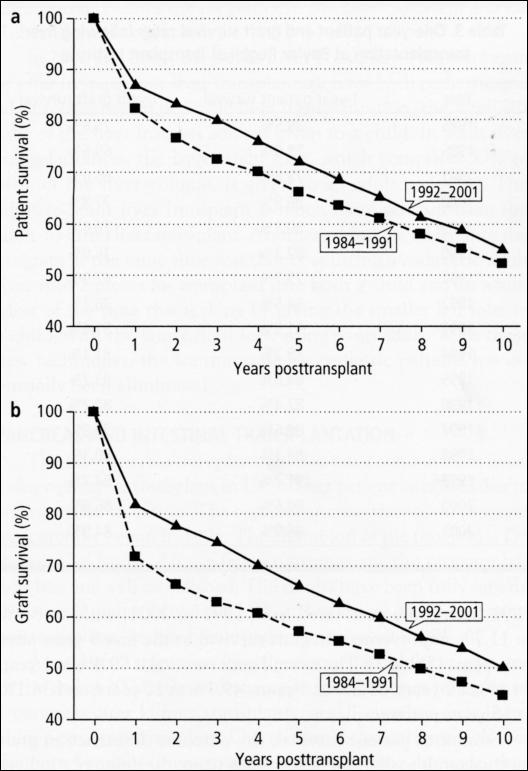
Overall patient survival is 85.8% at 1 year, 81.4% at 2 years, 70.3% at 5 years, 54.7% at 10 years, and 38.3% at 15 years posttransplant. These are the global results. A comparison of survival of cases performed in 1984 to 1991 and 1992 to 2001 shows a 4.7% to 7.7% improvement in the 1- to 5-year survival rates (Table 2), which is statistically significant. In the longer term, the results have not improved quite so much (Figure 5a) due to recurrence of primary diseases such as hepatitis C and hepatocellular carcinoma. The improvement in results occurred despite the change in the spectrum of liver disease etiology through the years. In the 1984-to-1991 period, only 109 out of 637 transplants (17.1%) were performed for chronic hepatitis (B and/or C), while the remainder were performed for cholestatic and other diseases, which carry a better prognosis. In 1992 to 2001, 505 out of 1518 transplants (33.2%) were performed for chronic hepatitis (P < 0.001), and 115 out of 257 transplants in 2000–2001 were in patients with chronic viral hepatitis (C, 102 patients; B, 12 patients; both, 1 patient). Since most of the long-term survival refers to the 1984-to-1991 “era,” this difference in etiologies and their specific outcome might explain the trends in long-term patient survival.
Table 2.
Patient and graft survival rates following transplantation at Baylor Regional Transplant Institute
| Survival rate (%) | ||||||||
| 30 | 90 | 1 | 2 | 5 | 10 | 15 | ||
| Survival | Interval | days | days | year | years | years | years | years |
| Patient | Overall | 96 | 92 | 86 | 81 | 70 | 55 | 38 |
| 1984–1991 | 94 | 90 | 82 | 77 | 66 | 52 | 37 | |
| 1992–2001 | 96 | 93 | 87 | 83 | 72 | 55 | NA | |
| Graft | Overall | 92 | 87 | 79 | 75 | 64 | 49 | 34 |
| 1984–1991 | 87 | 82 | 71 | 66 | 57 | 45 | 31 | |
| 1992–2001 | 93 | 89 | 82 | 78 | 66 | 50 | NA | |
NA indicates not applicable.
Figure 5.
(a) Patient survival and (b) graft survival rates after liver transplantation performed at Baylor Regional Transplant Institute during the periods 1984 to 1991 and 1992 to 2001.
The patient survival was high from the beginning of the program and has further improved over the years (Figure 5a). Of interest is the substantial improvement in graft survival (Figure 5b, Table 3) to the point where graft and patient survival are almost equal. This means a more effective use of the recovered donor livers; i.e., fewer patients need >1 liver graft to be saved.
Table 3.
One-year patient and graft survival rates following liver transplantation at Baylor Regional Transplant Institute
| Year | 1-year patient survival | 1-year graft survival |
| 1985 | 89.5% | 75.6% |
| 1986 | 79.0% | 69.6% |
| 1987 | 78.8% | 66.0% |
| 1988 | 86.8% | 77.8% |
| 1989 | 80.3% | 70.6% |
| 1990 | 82.3% | 75.0% |
| 1991 | 75.7% | 67.9% |
| 1992 | 84.5% | 76.1% |
| 1993 | 91.5% | 81.6% |
| 1994 | 89.2% | 81.1% |
| 1995 | 84.8% | 83.7% |
| 1996 | 82.4% | 80.2% |
| 1997 | 84.6% | 79.8% |
| 1998 | 84.1% | 80.3% |
| 1999 | 91.2% | 84.7% |
| 2000 | 90.6% | 86.6% |
| 2001 | 86.9% | 84.9% |
Graft survival after liver transplantation also tends to improve when comparing data from transplants performed from 1984 to 1991 with those performed from 1992 to 2001, with an 8.9% to 11.7% improvement in graft survival in the first 5 years after transplant (Table 2). The overall graft survival is 79.4% at 1 year, 74.6% at 2 years, 63.8% at 5 years, 49.3% at 10 years, and 34.1% at 15 years posttransplant.
Similar to patient survival, the outcome difference in graft survival tends to diminish long term. Again, the difference in liver disease etiology, as mentioned above, has even more impact in graft survival, graft loss being more frequent with chronic hepatitis C and B than with cholestatic and metabolic liver disease.
Technical improvements have made the surgical procedure less challenging for the patient. The operating room time has decreased from 8 to 9 hours to 4 to 5 hours in “standard” cases. The need for autologous blood transfusion was reduced to 2 to 4 units per case. Massive blood transfusions are extremely rare. Many cases do not necessitate intraoperative blood transfusion.
The improvement in intraoperative care has led to the approach of cases with complex anatomy, which would have been turned down as too risky in the earlier days. The improvement in the perioperative treatment has led to significant shortening in the postoperative ICU stay, as well as the hospital stay in general. The typical patient is admitted to the ICU for <24 hours and has a total hospital stay of 6 to 7 days. The median hospital stay is 9 days, with a mean of 14 days.
The outpatient postoperative follow-up and care is continued in the outpatient clinic by the transplant surgical team for the first 3 months after transplant. This approach allows consistent care, especially in terms of immunosuppression treatment.
KIDNEY TRANSPLANTATION
The first kidney transplant was done in June 1985 as a combined liver-kidney transplant. The regular kidney transplant program began in July 1985, after receiving approval from Medicare.
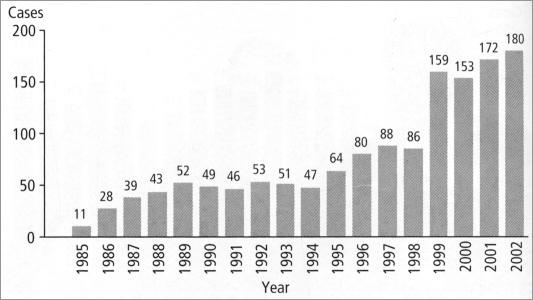
As seen in Figure 6, the volume of kidney transplants remained quite steady until 1996, when the program began to grow. By the end of the decade, we saw an explosion in the growth of the program due in part to the extension of the transplant program to other facilities and to the new laparoscopic technique that could be used to retrieve the kidney of a living donor.
Figure 6.
Annual volume of activity in kidney transplantation at Baylor Regional Transplant Institute.
From 1985 to 2002, the Baylor program performed 1401 kidney transplants. Most of them were done as a solitary procedure; 120 were performed in combination with other solid organ transplants (kidney-pancreas in 58 cases, liver-kidney in 57 cases, heart-kidney in 4 cases, and liver-kidney-pancreas in 1 case). Living donors accounted for 356 cases (23.8%). The use of living donors for kidney transplantation continues to increase. In 2002, a total of 180 kidney transplants were performed, 54 of them from living donors (30%).
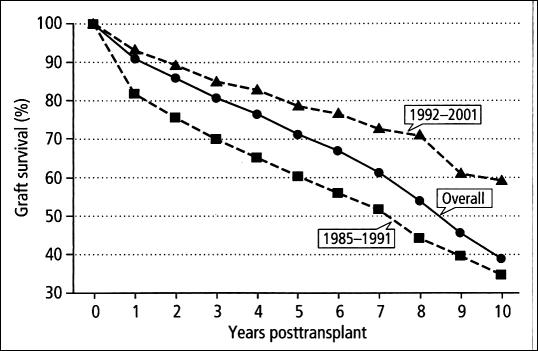
Overall kidney transplant graft survival is 90.8% at 1 year, 85.7% at 2 years, 71.1% at 5 years, 38.7% at 10 years, and 24% at 15 years (Figure 7). A comparison between transplants performed between 1985 and 1991 and between 1992 and 2001 (Table 4) shows an 11.6% to 24.7% improvement in 1- to 10-year graft survival. This is explained mainly by the improvement in surgical technique and immunosuppression, as well as the diligent long-term follow-up in the Dallas Transplant Institute. Overall patient survival is 96.5% at 1 year, 93.7% at 2 years, 86.6% at 5 years, 62.9% at 10 years, and 43.4% at 15 years.
Figure 7.
Graft survival rates after kidney transplantation performed at Baylor Regional Transplant Institute during the periods 1985 to 1991 and 1992 to 2001 and overall.
Table 4.
Patient and graft survival rates following Kidney transplantation at Baylor Regional Transplant Institute
| Survival rate (%) | ||||||
| Survival | Interval | 1 year | 2 years | 5 years | 10 years | 15 years |
| Patient | Overall | 97 | 94 | 87 | 63 | 43 |
| Graft | Overall | 91 | 86 | 71 | 39 | 24 |
| 1985–1991 | 82 | 76 | 60 | 45 | 24 | |
| 1992–2001 | 93 | 89 | 79 | 59 | NA | |
NA indicates not applicable.
The typical postoperative stay includes an overnight stay in the ICU and a total of 4 to 5 days of hospital stay. Care is then transferred to nephrology physicians of Dallas Nephrology Associates.
KIDNEY AND LIVER TRANSPLANTATION AT COMMUNITY MEDICAL CENTERS
In 1999, Baylor Medical Center at Grapevine shouldered the huge responsibility of developing a transplant program. This program was closed in July 2002 when the program in Baylor All Saints was opened. The program at Grapevine performed 136 cadaveric kidney transplants between 1999 and 2001 with results identical to those performed in Dallas.
The Baylor All Saints Transplant Program at Fort Worth was opened in July 2002. Headed by Dr. Marlon Levy, surgical director, and Dr. Natalie Murray, medical director, the program uses the expertise of BUMC and manpower from both medical centers and performs liver and kidney transplantation. The patient care protocols are unified for both the Dallas and Fort Worth programs.
Since its opening, the Baylor All Saints program has performed 29 liver transplants and 44 kidney transplants, all from cadaveric donors. We expect to start living-donor kidney transplantation and pancreas transplantation at this facility.
The extension of the transplant program to Grapevine and subsequently to Fort Worth allowed shortened waiting times for patients on the Baylor waiting list. The opening of the new programs also gave Baylor waiting list candidates access to a donor source, that of Tarrant County, that was unavailable to recipients in Dallas County.
LIVING-DONOR OPERATIONS FOR KIDNEY AND LIVER TRANSPLANTATION
In September 1999, the first living-donor kidney was retrieved laparoscopically at BUMC. A team consisting of Drs. Butch Derrick, Matt Westmoreland, and Michael Seiba began a service offering this very novel approach to living-donor organ donation. This technique results in shorter admissions, and most importantly, it results in a much shorter recuperation time, which allows the donor to return to work in one third to one half the time ordinarily required. Because of these factors and the decreased pain experienced by the donor, the number of individuals willing to become living donors has quadrupled. Less than one third of the living kidney donors are still operated on using the “open” technique. Since 1985, 2 superb urologists fulfill this service for the program, Dr. Michael Goldstein and Dr. Robert Schoenvogel.
In 2000 and 2001, the Dallas Liver Transplant Program began to offer living-donor liver transplantation for both pediatric and adult recipients. In pediatric liver transplantation, the small left lobe of the liver from an adult is given to a child. In adult liver transplantation, the larger right lobe, which comprises 50% to 60% of the liver volume, is given to an adult recipient. The adult-to-adult liver transplant is much more difficult than the adult-to-child liver transplant. Another technique added into the program at the same time was that of splitting a cadaveric adult liver into 2 pieces for transplant into both a child and an adult. Most of the time this is done by giving the smaller left lobe to a child, with the larger right lobe going to an adult. With these new techniques, the waiting time for pediatric patients has essentially been eliminated.
PANCREAS AND INTESTINAL TRANSPLANTATION
The first pancreas transplant was done as a combination liver kidney-pancreas transplant in 1989. That patient later died due to an Aspergillus infection. The regular pancreas transplant program was carefully begun in 1995. The champion of the program is Dr. Robert Goldstein. After a few tentative years, the program has now become well established. The results have been truly superb: the overall graft survival is 88.8% at 1 year and 85.7% at 2 years posttransplant, with a 2-year patient survival of 98.4%.
A total of 63 transplants were performed in adult patients until the end of 2002: 60 simultaneous kidney-pancreas transplants, 2 pancreas after kidney transplants, and 1 simultaneous liver kidney-pancreas transplant. Our routine technical approach uses the portal venous drainage and enteric exocrine drainage, thus avoiding systemic complications seen with bladder drainage.
Intestinal transplantation became somewhat popular in the early 1990s. A small bowel transplant was done at Baylor in 1994. The graft worked and allowed partial oral nutrition for 2½ months before it was suddenly rejected and had to be removed. With the rejections of these transplants being so violent, we determined that it was still too early for a clinically based intestinal transplant program. With the advancements in immunosuppression, we are currently moving toward the establishment of a new intestinal transplant program, both for adults and for children.
PEDIATRIC TRANSPLANTATION
The first patient to undergo transplantation at BUMC was a child, Amie Garrison. Over the years, several other children were transplanted on an ad hoc basis. In the early 1990s, it became apparent that BUMC would have to build a pediatric hospital or cease to perform transplants in children. Three months prior to Baylor's first case, Children's Medical Center in Dallas started doing liver transplantation under the direction of Dr. Walter Andrews. In 1992, the program at Children's temporarily closed but was later reopened.
The administration of the University of Texas Southwestern Medical School realized that a freestanding pediatric transplant program was too small and needed the support and feedback of a larger adult program. Discussions began between Southwestern Medical School, Children's Medical Center, and BUMC about the possibility of joining the pediatric program at Children's with the adult liver transplant program at Baylor. From these discussions came the Dallas Liver Transplant Program. With this joint program, we can now provide seamless services for patients at any age, as well as transition patients as they leave childhood and become adults.
A close collaboration between the pediatric and adult divisions is in place. Dr. John Andersen heads the pediatric program. Dr. Walter Andrews, the pioneer and founder of the program, left in 1998 to become chief of pediatric surgery at Children's Mercy Hospital in Kansas City. Dr. Jay Roden, one of the very first fellows at Baylor who also trained at Pittsburgh and later became a pediatric surgeon, joined Dr. Andrews at Children's Medical Center at 1989. With Dr. Roden as the surgical cornerstone, the Baylor surgical team provides additional manpower as needed for the pediatric program, most notably Dr. Ernesto Molmenti and Dr. Carlos Fasola in the past and currently Drs. Edmund Sanchez, Sherfield Dawson, and Henry Randall.
ATTENDING SURGEONS AND KEY MEMBERS OF THE TRANSPLANT TEAM
In September 1985, Dr. Bo S. Husberg joined the program. He was a kidney transplant surgeon from Malmo, Sweden, who had done a fellowship with Dr. Starzl in Denver from 1971 to 1973. Dr. Husberg's main interest was in kidney transplantation and microsurgery. Dr. Husberg eventually left Baylor to return to Scandinavia, where he joined a liver and kidney transplant group in Oslo, Norway, in 1998. In 1988, a third attending surgeon was added, Dr. Robert M. Goldstein, who had completed his liver transplant fellowship at Baylor. Some of Dr. Goldstein's major contributions to the program have been the start-up of the pancreas transplant program and the development of an extremely successful hepatobiliary surgical practice. Dr. Michael Holman joined the program as a fourth attending surgeon in 1990 for 1 year before he moved on to continue his career at Yale. He was followed in 1993 by Dr. Marlon F. Levy. Among Dr. Levy's major contributions to the program have been the research and teaching programs, the unique study of transgenic pig liver extracorporeal support of patients in acute terminal liver failure, and the development of the kidney transplant program at Baylor Grapevine Medical Center and later the transplant program at Baylor All Saints Medical Center in Fort Worth. Dr. Ernesto Molmenti from the University of Pittsburgh fellowship program joined the program in October 1998. Among his many contributions were the revitalization of the pediatric division in the joint Dallas Liver Transplant program and his pursuit of research activities. He left in 2001 to take a position as associate professor at Johns Hopkins. In 1998, Dr. Carlos Fasola joined the program, and most important among his contributions has been his involvement with the donor program and hepatitis C research. He left in July 2002 to join the transplant program at St. John Hospital and Medical Center in Detroit, Michigan. In July 2001, Dr. Edmund Sanchez joined as a new member of the transplant team after completing his liver transplant training at Baylor, followed by Dr. Srinath Chinnakotla, who came in November 2001 from the University of Nebraska. Dr. Sherfield Dawson, who trained at the University of California Los Angeles, came from the program at the University of Virginia in 2002, and Dr. Henry B. Randall, who trained at the University of California San Francisco, came from the University of Kentucky in 2002. The current transplant surgeons at Baylor are pictured in Figure 8.
Figure 8.
Current transplant surgeons at BUMC. Top row: Drs. Sherfield Dawson, Göran Klintmalm, and Marlon Levy. Second row: Drs. Robert Goldstein, Henry Randall, and Edmund Sanchez. Bottom row: Dr. Srinath Chinnakotla.
During the early years, Drs. Dan Polter, Kent Hamilton, and Dan DeMarco provided all the gastroenterology and hepatology services that sustained the program. In 1989, Dr. Harry Sarles joined to further strengthen the already strong gastroenterology program. An important step was taken in 1991 when Dr. Jeffrey Crippin was recruited from the Mayo Clinic, where he had just completed his hepatology fellowship. He was in charge of the liver pretransplant evaluations and was chairman of the selection committee until August 2000, when he left to become the medical director of the transplant program at Washington University in St. Louis. Dr. Jeffrey Weinstein, who had also completed a fellowship in hepatology at the Mayo Clinic, joined Dr. Crippin in 1993 and left in 2003 for a hepatology career elsewhere. In August 2000, Dr. Natalie Murray joined the program as a hepatologist from her previous position as the medical director of liver transplantation at the University of California at Irvine. Drs. Robert McFadden and Sherif Saadeh joined the hepatology team in 2003. The dedication of the gastroenterology/hepatology team to the transplant program and its contribution to the overall success of the liver transplant program cannot be overemphasized. The respect that they command in the world of gastroenterology and hepatology is a major reason for the referrals that Baylor receives. Without their expertise, the program would never have taken off.
The whole spectrum of clinical hepatology and hepatology research changed with the appointment of Dr. Cary Davis as medical director of hepatology and liver transplantation at Baylor. Dr. Davis comes with huge experience and international acclaim in hepatology, especially in chronic hepatitis B and C. We expect an important impetus in the research activity driven by the hepatology service.
The nephrology service holds a special position in the Baylor way of doing transplants. From the beginning, Drs. Marty White, Michael Emmett, and Tom Parker provided all the nephrology services to the program. These nephrologists with their immense experience in transplantation from the Parkland and Methodist kidney programs had significant expertise in immunosuppression. This knowledge coupled with their nephrology expertise played an important role in the success of BUMC's kidney transplant program. It was quickly recognized that liver transplant recipients frequently face kidney problems as well—problems that could be severe enough to require dialysis, especially posttransplantation. One of the most important additions to the Baylor transplant program was the hiring of Dr. Thomas Gonwa from the University of Iowa, who joined Dallas Nephrology Associates in 1986. With his brilliance, insatiable curiosity, and dedicated work effort, he soon developed into the world's leading nephrologist in the understanding of the post–liver transplant kidney. His scientific output was immense. In July 2001, he left Dallas to take a position as the medical director of the Mayo Kidney Transplant Program in Jacksonville, Florida. After Dr. Gonwa joined the program, Drs. Martin Mai and Larry Melton joined the program in 1988 and 1989, respectively. Dr. Martin Mai left in August 2001 to join Dr. Gonwa in Florida. Dr. Stephen Hays and Dr. Kim Rice joined the group at Baylor in 1994 and 1998, respectively. Dr. Yusri Barri joined the nephrology team in 2002, followed by Dr. Carlos Zayas in 2003.
The BUMC transplant team is unique: everyone involved belongs regardless of specialty. The radiology department has been one of the critical success factors for the transplant program. Both the diagnostic and interventional radiologists have been unwavering in their support of the transplant program. Drs. Norman Diamond, Steve Lee, Chet Rees, Herbert Steinbach, and Mark Hamilton all played a significant role in the development and success of the transplant program at Baylor. Likewise, the pathology department has played a pivotal role in the transplant efforts at Baylor. Drs. Weldon Tillery, David Watkins, and George Netto have provided a service that is second to none in any transplant program. Leading pathologists in the USA have stated that no other institution has such consistent biopsy readings as BUMC. Others such as Drs. Charles Shuey and Robert Black in pulmonology, Dr. William Sutker in infectious disease, and the entire cardiology and neurology groups must not be forgotten. I must finally mention the unsung heroes of transplantation, the anesthesiologists. Dr. Michael Ramsay has built one of the strongest anesthesiology teams in the world in the field of liver transplantation, with Drs. Thomas Swygert, Robert Parks, Peter Walling, Timothy Valek, Victor Ramon, James Pyron, and Thomas Gunning, to mention only the first members of the team. The short surgical times and the low blood loss we experience at Baylor are thanks, in a large degree, to our expert anesthesiologists.
Outside of the physician realm, another critical factor in the Baylor success was the decision to place all transplant patients on the same floor, in the same ICU, and to use the same operating room nurses. The dedication of the nurses has been vital throughout the years. Patients never cease to laud the personnel involved in the transplantation service. The backbone of the transplant program is the transplant coordinators. We have been extremely fortunate in developing a core group of coordinators that remained with the program for many years before they sought new career opportunities. Some coordinators that must be mentioned are Susan Neely, Lori Rippert, Sharon Carden-Hashim, Kathy Manley, Donna Monissey, Pam Fertig, and Sharon Anderson, followed by Helena Roman, Patti Graham, Karen Ochenkoski, Jill Solomon, and Micki Robertson.
One aspect that makes Baylor unique from other institutions is the close tie that exists between the medical team and the hospital administration. The mutual respect established between me and Mr. Powell with the transplant of Amie Garrison set the standard for the working relationship between medicine and administration. Administrators such as Robert Hille, John Carter, Tim Parris, and Joel Allison have all been involved in the intimate dialogue that has taken place between the medical team and administration. For years, Mr. Powell, Dr. Fordtran, and I met frequently in what was jokingly called “scheming sessions.” In these sessions, strategies were proposed and evaluated. The transplant service had its own administrator from the very beginning. Susan Neely, Belinda Tommey, Dorothy Elford, Janet Nelson, and Patti Pickering were all extremely capable administrators that eventually left transplantation for other career opportunities. In 2001, the administrator of transplant was given the title of vice president, indicating the importance of transplantation at Baylor. It is not surprising that Maureen Sweeny was the administrator who achieved this title.
RESEARCH
One of the first decisions made when organizing the Baylor transplant program was that it should have a sound scientific base. In 1984, transplantation was becoming a clinical service that could be offered with a reasonable hope for success. Thus, it was obvious that with aspirations of building a large program, we had to be committed to participate in the development of the science and art of transplantation. Dr. Klintmalm organized the entire program around a scientific core. All patients were expected to provide data for scientific study. If you had data that were good enough to result in good science, you automatically had data for good clinical medicine. However, good clinical medicine does not necessarily result in good research data. Data retrieval was therefore a cornerstone of our research.
In 1987, the first electronic database was established on a mainframe VAX machine. Over the years, as patient material grew and the mainframe became outdated, we finally implemented the second generation of electronic databases, which went live in 1997. The database is now on a server-based personal computer platform. It is partially thanks to this database that Baylor has become one of the large institutions presenting at national and international meetings. A total of 264 papers were published in peer-reviewed medical journals and another 64 in other journals. We published 3 books and wrote 16 book chapters. We published 109 abstracts and had 206 presentations at national and international professional meetings in the field of transplantation, transplant-related science, or hepatobiliary surgery.
The importance of the role of the database cannot be overstated. The database houses all the pretransplant workup data on a patient and follows that patient's data up to and through death. Research nurses, data collectors, quality assurance personnel, master's- and doctoral-level statisticians, and database managers all service this database. This is one of the wonders of the transplant program. Baylor, a private, nonprofit institution, has a clinical research base second to no academic institution in the USA. From the beginning, the only limiting factor has been the availability of time for the attendings and fellows to write papers. Baylor is involved in numerous single- and multicenter trials of immunosuppression medication.
A major research effort is the emerging pancreatic islet cell transplantation program under the direction of Dr. Marlon Levy. This new treatment strategy for type 1 diabetes mellitus has now attracted large interest after recent proof of safety and efficacy with this procedure, which is less invasive than whole organ pancreas transplantation. Major investments are being made to build a state-of-the-art laboratory facility for islet cell isolation, directed by Dr. Bashoo Naziruddin. The laboratory will generate opportunities toward basic research in pancreatic islet physiology and transplant immunology.
THE FUTURE
To quote presidential candidate Dan Quayle, “To make predictions is always difficult, especially about the future.” Where is transplantation going? Today we are in the new millennium, and transplantation has, in a few short and intense years, become one of the most important disciplines at BUMC and thus to the health care system. We have a transplant program at Baylor that can compete with any other program in the world. The success rates that we enjoy today in kidney, liver, pancreas, heart, and lung transplantation are at a level that was unbelievable only 15 years ago. I foresee that transplantation will continue to thrive and expand with the creation of stronger, more specific, and less toxic immunosuppressive drugs. Transplantation will be extended to other organs: already, the first hand transplants have been reported, and this technology will be extended to other extremities as well. Eventually, the limits of transplantation will be set only by our own imagination.
Transplantation was expanded from its base at BUMC to other entities within the health care system: Baylor Medical Center at Grapevine and then Baylor All Saints Medical Genter in Fort Worth. By expanding, we will make transplantation more accessible to the patients. New technology, such as gene therapy, stem cells, and the potential of humanized xenografts, is being developed. One day we will use these and other treatment strategies to induce tolerance and treat underlying disease. Once this happens, medicine as we know it today will fundamentally change. When this change comes, I expect that Baylor Health Care System will have a seat at the table.